Abstract
Objective:
Comparison of outcome and costs after laparoscopic and open colectomy.
Summary Background Data:
Previous studies comparing laparoscopic and open colectomy report conflicting results with regard to clinical outcome and costs.
Methods:
Laparoscopic colectomy patients from a prospective database were matched for age, gender, and disease-related grouping to patients who underwent the same operation by the open approach over the same period (2000 to 2001). Data for the latter group was gathered by retrospective analysis and the 2 groups were compared for outcome and direct costs.
Results:
Laparoscopic colectomy patients (n = 150) were compared with the same number of open colectomy patients. American Society of Anesthesiologists classification (P = 0.09), body mass index (P = 0.17), diagnosis (P = 0.12), complications (P = 0.14), and rate of readmission within 30 days (P = 0.44) were similar for both groups. Operating room costs were significantly higher after laparoscopic colectomy (P < 0.0001), but length of hospital stay was significantly lower (P < 0.0001). This resulted in significantly lower total costs (P = 0.0007) owing to lower pharmacy (P < 0.0001), laboratory (P <0.0001), and ward nursing costs (P = 0.0004).
Conclusions:
Laparoscopic colectomy results in significantly lower direct costs compared with open colectomy for carefully matched patients.
The laparoscopic approach to colectomy is slowly gaining acceptance for the management of colorectal pathology. It has proved itself useful for many benign conditions, including diverticulitis, Crohn’s disease, and rectal prolapse. The cost-effectiveness and long-term outcomes with laparoscopic colectomy (LAC) for malignancy are less well accepted. Smaller incision size leads to improved cosmesis and reduced postoperative pain. The laparoscopic approach is also associated with less postoperative ileus and earlier tolerance of diet. These factors contribute to earlier recovery of the patient with a reduced hospital stay and earlier return to normal activity.
Initial concerns with laparoscopic colorectal surgery related to technical difficulty, steeper learning curves, a need for specialized instrumentation, and longer operating times. Secondary concerns have developed, including increased hospital costs, questions about real improvements in outcome, and concerns regarding safety in neoplastic disease. These factors have led to the slower dissemination of the technique compared with other advanced laparoscopic procedures, like Nissen fundoplication or splenectomy. Recent reports of “fast-track” care for colectomy patients has further blurred the distinctions between outcome of laparoscopic and open colectomy because of the perception that length of stay can be dramatically reduced with open surgery.1-3 Therefore, it is prudent to compare the clinical outcome and relative cost structures of open and laparoscopic colon resection in a large group of patients managed with similar perioperative care plans. This may ascertain whether laparoscopic operating room costs are balanced by postoperative care savings.
Studies comparing costs from colectomy by the laparoscopic and open approaches report conflicting results. Although some4,5 report costs for LAC to be greater than for open surgery, others found results to be equivocal,6-9 Some have reported that LAC leads to reduced costs compared with open colectomy,10-16 Most of these studies compared costs for laparoscopic and open colectomy for a single procedure or diagnosis. Other reports of costs comparison after different operations for benign and malignant disease only compared small numbers of patients undergoing LAC.7,8,13,17 This study compares the direct costs and clinical outcome for patients undergoing operations by the laparoscopic approach for benign and malignant colorectal disorders over a 2-year period (2000 to 2001) with the costs of open procedures over the same period.
MATERIALS AND METHODS
All patients undergoing surgery by the laparoscopic approach for colorectal disorders at this institution are currently entered prospectively into an institutional review board approved database. Details include age, gender, body mass index (BMI), diagnosis, American Society of Anesthesiologists classification, operation procedure, operating time, estimated blood loss, complication, and length of stay in hospital. The hospital coding system differentiates patients undergoing bowel resection into those with and without comorbidity by disease-related grouping (DRG).
Patients who underwent laparoscopic procedures between January 2000 and December 2001 were identified from the laparoscopic database and were compared with patients with the same hospital code (DRG) undergoing the same surgical procedure by the open approach during that period. The 2 groups were also matched for age (within 10 years) and gender. In addition to the variables that were entered into the database for the laparoscopic group, details of previous abdominal operations were recorded for the open group by retrospective chart review. Patients who underwent previous open abdominal surgery (other than cholecystectomy, hysterectomy, salpingo-oophorectomy, appendectomy, or tubal ligation) that might have been considered an exclusion criterion for laparoscopic surgery were excluded from this group. LAC patients who underwent conversion to the open technique remained in the laparoscopic group for the purpose of comparison by intention to treat principles.
Both groups were compared for American Society of Anesthesiologists classification, BMI, duration of stay in hospital, operating time, and complications. Direct costs (hospital expenses, rather than billed costs) for the 2 groups were calculated by using the Stanford’s integrated hospital cost management system and decision software (Transition Systems Inc. Boston, MA). This software provided direct cost per case for hospitalization, operating room (OR), radiology, anesthesia, pharmacy, laboratory, intensive care unit, and nursing care. Professional costs were not included in the study and billed costs were not calculated. Parametric data is presented as mean ± SD and nonparametric data as median and interquartile range. Values were compared by Wilcoxon matched pairs test, Fisher exact test tests, or χ2 test as appropriate. Significance level for all analysis was P < 0.05 and GraphPad InStat version 3.05, 32 bit for Windows 95/NT (GraphPad Software, San Diego, CA, USA; www.graphpad.com) was used for analysis.
RESULTS
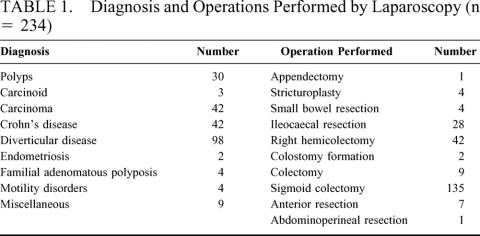
Patients (n = 234) underwent colorectal surgery by the laparoscopic approach during the study period. Patient demographics, diagnosis, operative procedure performed, and complications are detailed in Tables 1 and 2. During the same period, 2293 patients underwent open surgery.
TABLE 1. Diagnosis and Operations Performed by Laparoscopy (n = 234)
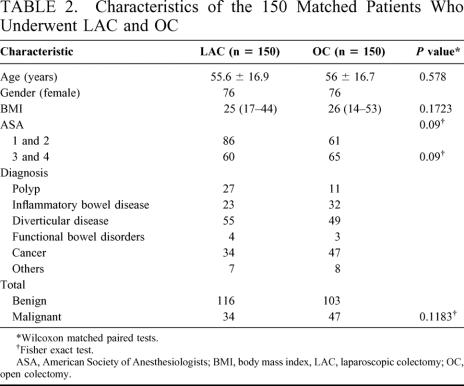
TABLE 2. Characteristics of the 150 Matched Patients Who Underwent LAC and OC
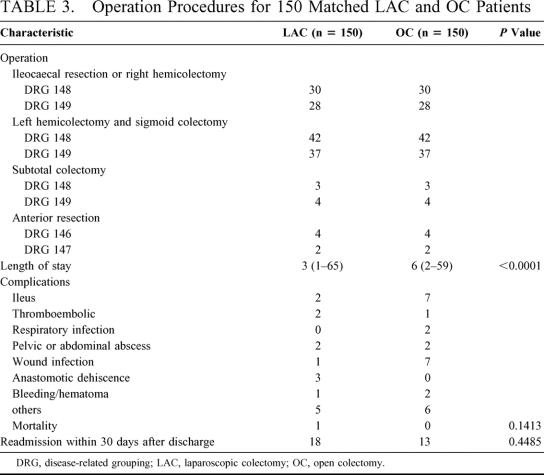
Patients (n = 150) from the laparoscopic database (LAC) could be matched with the same number of patients undergoing surgery by the open approach (OC) for age, gender, DRG, and operation procedure. The characteristics of patients in the 2 groups and the factors compared are outlined in Table 3. There was no significant difference in BMI, diagnosis (benign and malignant), and complications, including readmission rate. LAC had significantly shorter operating time and LOS compared with OC. One patient in LAC died on the first postoperative day as a result of cardiac arrest.
TABLE 3. Operation Procedures for 150 Matched LAC and OC Patients
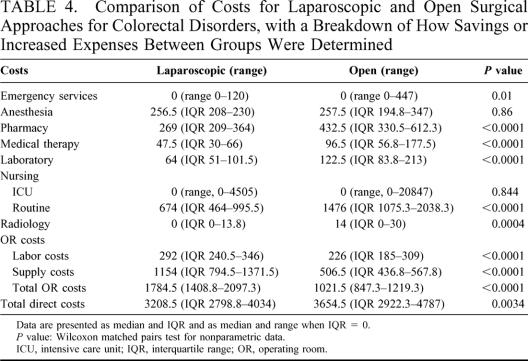
Direct costs for the 2 groups of patients and the distribution of costs are presented in Table 4. LAC had significantly lower total direct costs than OC (P = 0.003). Because this probably relates to the significantly shorter stay in hospital for this group of patients, not only were costs related to bed and nursing utilization reduced as might be expected but pharmacy, laboratory, radiology, and ward nursing costs were also significantly lower for this group of patients. Costs related to input by other departments, such as physiotherapy, respiratory therapy, and so on, were also significantly lower for LAC compared with OC. In contrast, costs in the OR, including supply costs (for equipment and consumables) and labor costs were significantly lower for the open group leading to significantly lower costs in the OR. Anesthesia and intensive care unit nursing costs for both groups were similar.
TABLE 4. Comparison of Costs for Laparoscopic and Open Surgical Approaches for Colorectal Disorders, with a Breakdown of How Savings or Increased Expenses Between Groups Were Determined
DISCUSSION
The care of patients undergoing colorectal surgery is associated with a variety of direct costs, which include hospitalization and nursing costs, costs towards operating equipment and consumables, anesthesia, laboratory, radiology, and pharmacy. Taheri et al18 described the fact that decreasing 1 or 2 days at the end of the length of stay has minimal impact on the overall cost of care compared with reducing resources in the OR or earlier in the course of care. Therefore, if LAC requires greater OR costs because of longer operating time or more expensive equipment for laparoscopic procedures, these costs must be balanced by reduced analgesia requirements, earlier return of bowel function, and reduced length of stay when compared with open procedures. This will be particularly challenging as more aggressive postoperative care plans further reduce the length of stay for open colectomy.
Most studies have reported a shorter duration of stay after LAC.19-23 Others,24-26 however, report a similar length of stay for patients undergoing surgery by the 2 approaches, although this may be related to differing length of stay in different cultural environments and less experience with the technique in some reports. There is also variability in the reporting of duration of ileus after laparoscopic and open colorectal procedures. Although most authors found a shorter duration of postoperative ileus and earlier intake of food in LAC patient6,10,20-24,27,28 others report similar recovery of bowel function after both procedures.5,25 Complication rates for LAC are generally similar6,12,13,19,21,27 or less than12 for open colorectal procedures depending on the study, with rare exceptions to this.25 Although most studies6,10,12,27 report a reduced need for pain medication, Bokey et al5 did not find a significant difference in analgesic requirements after laparoscopic when compared with open surgery. Reports on comparative operating times between the 2 procedures are also equivocal.
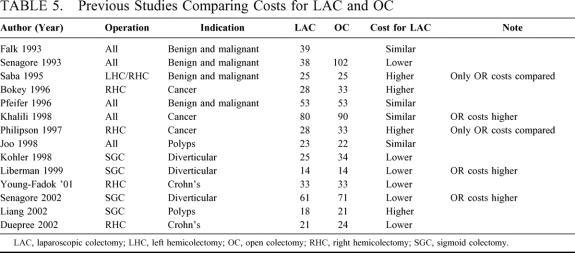
This variability has resulted in conflicting reports on the relative costs of laparoscopic and open colectomy. Falk et al7 published data on cost comparison between laparoscopic and open colectomy in 1993 in which they reported no difference between the 2 groups as the shorter duration of stay in hospital for laparoscopic patients in their study compensated for the increased operating room costs. Studies since that time have either confirmed or refuted this initial finding (Table 5). Most studies compare costs for a single procedure performed by the laparoscopic or open approach for either benign or malignant disease conditions. Studies7,8,13,17 that compare costs for a mixed group of patients with both benign and malignant disease undergoing different surgical procedures also report conflicting results. A review29 found that patients undergoing LAC had fewer complications, decreased mortality, less postoperative pain and shorter length of stay compared with open surgery with similar total costs while another30 reported greater costs.
TABLE 5. Previous Studies Comparing Costs for LAC and OC
In this study we report a reduction in total direct costs of $450 per case. Analysis of the source of hospital costs demonstrates that these cost reductions are derived from a reduction in the cost of nursing care, pharmacy and laboratory costs, which more than compensate for the increased operating room expenses incurred by laparoscopy. This cost reduction is measured in direct costs to the institution and may reflect a reduction of several times more in billed costs. Additional financial benefits to the institution will vary depending on whether the hospital is operating at its maximum capacity or not. In those operating at maximum capacity, additional bed-days will become available allowing new patients to be admitted and treated without any increase in fixed costs. In systems operating at lower capacity, nursing requirements will be reduced allowing for closure of bed spaces and reductions in staffing requirements.
Previous abdominal surgery with the possibility of adhesions could significantly increase operating time and costs for patients undergoing open surgery but most studies have not taken this fact into consideration during comparison with the open technique. We have avoided this confounding factor by excluding such patients from the open group. Comparison between laparoscopic and open surgery may not be appropriate in centers where the procedure is performed by a multitude of surgeons with varying degrees of expertise in laparoscopy. The greater variation in laparoscopic skills as when compared with open surgery would tend to skew the results towards greater operating room and overall costs for the laparoscopic group. Two experienced laparoscopic surgeons (AJS and CPD) performed all laparoscopic procedures included in the database at this institution over this time period. This fact avoids the negative effect of reduced skills in laparoscopic surgery that could result if more surgeons with varying degrees of experience performed the procedure. The steep learning curve for the laparoscopic technique leads to longer operating times and chance for complications, both factors that influence overall costs. This study hence compares the 2 techniques performed by surgeons with equivalent technical expertise for the 2 procedures.
This study evaluates patients undergoing a broad variety of operations for differing pathology. Patients undergoing LAC had significantly lower length of stay and hospital costs than those having open surgical procedures using groups of carefully matched patients. LAC was associated with greater OR costs as a result of consumables and equipment. Although the postoperative complication rate is comparable, the overall utilization of laboratory, radiologic, pharmacy, and nursing services are significantly lower. This reflects the reduction in length of stay but is also contributed by a reduced need for postoperative nursing care, medication and investigations. This results in significantly lower direct costs when compared with open surgery.
Footnotes
Reprints: Conor P. Delaney, Department of Colorectal Surgery/A-30, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, OH 44195. E-mail: delanec@ccf.org.
REFERENCES
- 1.Basse L, Hjort Jakobsen D, et al. A clinical pathway to accelerate recovery after colonic resection. Ann Surg. 2000;232:51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kehlet H, Mogensen T. Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg. 1999;86:227–230. [DOI] [PubMed] [Google Scholar]
- 3.Delaney CP, Fazio VW, Senagore AJ, et al. ’Fast track’ postoperative management protocol for patients with high co-morbidity undergoing complex abdominal and pelvic colorectal surgery. Br J Surg. 2001;88:1533–1538. [DOI] [PubMed] [Google Scholar]
- 4.Philipson BM, Bokey EL, Moore JW, et al. Cost of open versus laparoscopically assisted right hemicolectomy for cancer. World J Surg. 1997;21:214–217. [DOI] [PubMed] [Google Scholar]
- 5.Bokey EL, Moore JW, Chapuis PH, et al. Morbidity and mortality following laparoscopic-assisted right hemicolectomy for cancer. Dis Colon Rectum. 1996;39(10 Suppl):S24–S28. [DOI] [PubMed] [Google Scholar]
- 6.Joo JS, Amarnath L, Wexner SD. Is laparoscopic resection of colorectal polyps beneficial? Surg Endosc. 1998;12:1341–1344. [DOI] [PubMed] [Google Scholar]
- 7.Falk PM, Beart RW Jr, Wexner SD, et al. Laparoscopic colectomy: a critical appraisal. Dis Colon Rectum. 1993;36:28–34. [DOI] [PubMed] [Google Scholar]
- 8.Pfeifer J, Wexner SD, Reissman P, et al. Laparoscopic vs open colon surgery. Costs and outcome. Surg Endosc. 1995;9:1322–1326. [PubMed] [Google Scholar]
- 9.Bergamaschi R, Arnaud JP. Immediately recognizable benefits and drawbacks after laparoscopic colon resection for benign disease. Surg Endosc. 1997;11:802–804. [DOI] [PubMed] [Google Scholar]
- 10.Young-Fadok TM, HallLong K, McConnell EJ, et al. Advantages of laparoscopic resection for ileocolic Crohn’s disease. Improved outcomes and reduced costs. Surg Endosc. 2001;15:450–454. [DOI] [PubMed] [Google Scholar]
- 11.Liberman MA, Phillips EH, Carroll BJ, et al. Laparoscopic colectomy vs traditional colectomy for diverticulitis. Outcome and costs. Surg Endosc. 1996;10:15–18. [DOI] [PubMed] [Google Scholar]
- 12.Kohler L, Rixen D, Troidl H. Laparoscopic colorectal resection for diverticulitis. Int J Colorectal Dis. 1998;13:43–47. [DOI] [PubMed] [Google Scholar]
- 13.Senagore AJ, Luchtefeld MA, Mackeigan JM, et al. Open colectomy versus laparoscopic colectomy: are there differences? Am Surg. 1993;59:549–553; discussion 553-554. [PubMed] [Google Scholar]
- 14.Senagore AJ, Duepree HJ, Delaney CP, et al. Cost structure of laparoscopic and open sigmoid colectomy for diverticular disease: similarities and differences. Dis Colon Rectum. 2002;45:485–490. [DOI] [PubMed] [Google Scholar]
- 15.Larach S, Ferrera A. Cost Analysis. In: Jager R, Wexner SD, eds. Laparoscopic Colorectal Surgery. New York: Churchill-Livingstone; 1996. [Google Scholar]
- 16.Duepree HJ, Senagore AJ, Delaney CP, et al. Advantages of laparoscopic resection for ileocecal Crohn’s disease. Dis Colon Rectum. 2002;45:605–610. [DOI] [PubMed] [Google Scholar]
- 17.Saba AK, Kerlakian GM, Kasper GC, et al. Laparoscopic assisted colectomies versus open colectomy. J Laparoendosc Surg. 1995;5:1–6. [DOI] [PubMed] [Google Scholar]
- 18.Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg. 2000;191:123–130. [DOI] [PubMed] [Google Scholar]
- 19.Bemelman WA, Slors JF, Dunker MS, et al. Laparoscopic-assisted vs open ileocolic resection for Crohn’s disease. A comparative study. Surg Endosc. 2000;14:721–725. [DOI] [PubMed] [Google Scholar]
- 20.Young-Fadok TM, Radice E, Nelson H, et al. Benefits of laparoscopic-assisted colectomy for colon polyps: a case-matched series. Mayo Clin Proc. 2000 Apr;75:344–348. [DOI] [PubMed] [Google Scholar]
- 21.Muckleroy SK, Ratzer ER, Fenoglio ME. Laparoscopic colon surgery for benign disease: a comparison to open surgery. JSLS. 1999;3:33–37. [PMC free article] [PubMed] [Google Scholar]
- 22.Kakisako K, Sato K, Adachi Y, et al. Laparoscopic colectomy for Dukes A colon cancer. Surg Laparosc Endosc Percutan Tech. 2000;10:66–70. [PubMed] [Google Scholar]
- 23.Franklin ME Jr, Rosenthal D, Abrego-Medina D, et al. Prospective comparison of open vs. laparoscopic colon surgery for carcinoma. Five-year results. Dis Colon Rectum. 1996;39(10 Suppl):S35–S46. [DOI] [PubMed] [Google Scholar]
- 24.Khalili TM, Fleshner PR, Hiatt JR, et al. Colorectal cancer: comparison of laparoscopic with open approaches. Dis Colon Rectum. 1998;41:832–838. [DOI] [PubMed] [Google Scholar]
- 25.Ho YH, Tan M, Eu KW, et al. Laparoscopic-assisted compared with open total colectomy in treating slow transit constipation. Aust N Z J Surg. 1997;67:562–565. [DOI] [PubMed] [Google Scholar]
- 26.Milsom JW, Hammerhofer KA, Bohm B, et al. Prospective, randomized trial comparing laparoscopic vs. conventional surgery for refractory ileocolic Crohn’s disease. Dis Colon Rectum. 2001;44:1–8; discussion 8-9. [DOI] [PubMed] [Google Scholar]
- 27.Marubashi S, Yano H, Monden T, et al. The usefulness, indications, and complications of laparoscopy-assisted colectomy in comparison with those of open colectomy for colorectal carcinoma. Surg Today. 2000;30:491–496. [DOI] [PubMed] [Google Scholar]
- 28.Marcello PW, Milsom JW, Wong SK, et al. Laparoscopic restorative proctocolectomy: case-matched comparative study with open restorative proctocolectomy. Did Colon Rectum. 2000;43:604–608. [DOI] [PubMed] [Google Scholar]
- 29.Ballantyne GH. Laparoscopic-assisted colorectal surgery: review of results in 752 patients. Gastroenterologist. 1995;3:75–89. [PubMed] [Google Scholar]
- 30.Chapman AE, Levitt MD, Hewett P, et al. Laparoscopic-assisted resection of colorectal malignancies: a systematic review. Ann Surg. 2001;234:590–606 [DOI] [PMC free article] [PubMed] [Google Scholar]