Abstract
Objective:
This study was conducted to examine the long-term prognosis of after treatment of patients with choledocholithiasis, including the recurrence of lithiasis, and to thereby determine the best treatment modality for choledocholithiasis based on its pathological entity.
Summary Background Data:
Choledocholithiasis can be caused by either primary bile duct stones that originate in the bile duct or by secondary bile duct stones that have fallen out of the gallbladder. The recurrence rates vary depending on the type of choledocholithiasis.
Methods:
Two-hundred thirteen outpatients who were treated for choledocholithiasis from 1982 to 1996 were selected as subjects and monitored for a period ranging from 5 to 19 years (mean, 9.6 years). The 213 patients were divided into 3 groups: 87 patients who had undergone choledocholithotomy and T-tube drainage (including the use of the laparoscopic method), 44 patients who had undergone choledochoduodenostomy, and 82 patients whose stones were removed by endoscopic sphincterotomy (EST). Recurrence of lithiasis was examined for each type of treatment modality.
Results:
Choledochoduodenostomy was performed in 44 cases for the purpose of preventing any recurrence. The recurrent rate was analyzed in 169 cases. Choledocholithiasis recurred in 17 of the 169 cases (10.1%). The remaining 152 patients that showed no recurrence of lithiasis were examined and compared. The diameter of the common bile duct measured during the initial treatment was more dilated in patients with recurrent lithiasis (16.6 ± 5.9 mm) than in patients without any recurrence (9.8 ± 4.9 mm; P < 0.05). Peripapillary diverticula were observed in 10 of the 17 patients with recurrent lithiasis (58.8%), and in 34 of the 152 nonrecurrent patients (22.3%), showing that diverticula were more common in recurrent cases (P < 0.05). Furthermore, while primary bile duct stones were found in 11 of the 17 cases with recurrent lithiasis (64.7%), primary stones were found in only 37 of the 152 nonrecurrent patients (24.3%), showing primary bile duct stones were also more common in recurrent patients (P < 0.05). The recurrent patients were examined by surgical procedure. Nine patients with choledocholithotomy and T-tube drainage had a recurrence (10.3%), and 8 patients in the EST group had a recurrence (9.8%). The recurrence rates for these procedures were higher than for cases with choledochoduodenostomy (recurrence rate: 0%, P < 0.05). In particular, lithiasis recurred in 5 of the 12 patients with T-tube drainage for primary bile duct stones (41.7%).
Conclusion:
Although choledocholithotomy and T-tube drainage, including open and laparoscopic surgery, is presently a common procedure for choledocholithiasis, this procedure will not necessarily prevent a recurrence of the disease. For older patients with primary bile duct stones, choledochoduodenostomy or EST is recommended.
In recent years, in addition to nonoperative treatment methods, including endoscopic sphincterotomy (EST), endoscopic papillary balloon dilatation (EPBD), and extracorporeal shock-wave lithotripsy (ESWL),1–3 minimally invasive surgeries, including laparoscopic choledocholithotomy, are becoming popular.4–6 However, because the recurrence rate after treatment ranges from 6.4 to 18%,7–9 it is desirable to select treatment methods that have no recurrence. Choledocholithiasis can be caused by either primary bile duct stones that originate in the bile duct or by secondary bile duct stones that have fallen out of the gallbladder, and the recurrence rates vary depending on the type of choledocholithiasis.10 However, many surgeons select surgical procedures based on their experience rather than the disease’s pathogenesis. Therefore, in this report, the recurrence of lithiasis was analyzed by type of treatment modality. The goal was to determine the best treatment method to prevent recurrence in each type of choledocholithiasis.
PATIENTS AND METHODS
One-thousand sixty-two patients with cholelithiasis were treated at Wakayama Medical University Hospital between 1982 and 1996; 807 patients with cholecystolithiasis, 213 with choledocholithiasis (20.1%), and 42 with hepatolithiasis. Of these patients, 213 with choledocholithiasis were treated between 1982 and 1996, and monitored at the outpatient clinic for a period ranging from 5 to 19 years (mean, 9.6 years). The recurrence rate for lithiasis and the incidence of other digestive diseases was examined.
Primary bile duct stones were classified with the definition proposed by Saharia et al10: 1) previous cholecystectomy without bile duct exploration, 2) detection of bile duct stones at least 2 years after cholecystectomy, and 3) no evidence of biliary stricture prior to surgery. In addition, the following stones were classified as primary bile duct stones: 1) brown pigment stones found in the common bile duct even when there are no stones in the gallbladder and 2) brown pigment stones found in the common bile duct when there are cholesterol stones in the gallbladder and the diameter of the common bile duct is no less than 15 mm. The components of all stones were analyzed by infrared absorption spectrometry, and brown pigment stones were defined as stones whose cross sections appear macroscopically laminar and when stone analysis shows that the stone contains at least 60% of bilirubin calcium.11 As a result, the population was divided into a group of 90 patients with primary bile duct stones and a group of 123 cases with secondary bile duct stones.
Cases followed up for over 5 years were treated by choledocholithotomy and T-tube drainage in 87 patients, choledochoduodenostomy in 44 patients, and EST in 82 patients. T-tube drainage was performed by open laparotomy in 80 of the 87 cases, using the laparoscopic method in the other 7 cases. In all cases, a 1.5- to 3-cm longitudinal incision was made along the bile duct after cholecystectomy. After the stones had been removed, a cholangioscope was used to check for residual stones. A T-tube was then inserted, and the interrupted sutures were inserted at 2-mm intervals at the incised section using 4-o or 5-o absorbable suture.
Choledochoduodenostomy was performed by side-to-side anastomosis in 6 of the 44 patients, including 3 cases in which the patients were over 80 years of age and 3 cases with poor risk (a case undergoing dialysis, a case with liver cirrhosis, and a case with severe diabetes mellitus). End-to-side anastomosis was performed in the remaining 38 patients to avoid sump syndrome. The bile duct was ablated all around the duct, and a transverse incision was made in the anterior wall facing the duodenum and the stones were then removed. The bile duct was closed on the side facing the duodenum by continuous sutures using 4-o absorbable suture.
Choledochoduodenostomy was performed by interrupted end-to-side anastomosis of all layers of the end of the bile duct and the duodenal bulbus on the side of the lesser curvature of stomach, 3 to 4 cm caudal from the pylorus, using a control-release atraumatic needle with 4-o absorbable suture.
The common bile duct stones were removed through EST alone in all 82 cases that had undergone EST in the study. Cholecystectomy had already been performed in 18 of the 82 cases, and open cholecystectomy or laparoscopic cholecystectomy was performed in 56 of the 64 cases after EST. Cholecystectomy was not performed in 8 patients because of advanced age and high surgical risk. EST was performed using a pull-type papillotome, and small-to-medium incisions were made. Retrieval balloons or baskets were used to remove stones no more than 1 cm in diameter, and a endoscopic mechanical lithotripter was used to perform lithotripsy for stones more than 1 cm in diameter. When stones could not be removed, an endoscopic nasobiliary drainage tube was inserted. When stones were removed, endoscopic retrograde cholangiography (ERC) was performed a week later to verify the absence of residual stones.
ERC was performed in all 213 choledocholithiasis patients. Peripapillary diverticulum was defined as a diverticulum that was located within 2 cm of the papilla of Vater. The number of stones and the maximum diameter (mm) of the common bile duct were measured during the operation in patients with T-tube drainage or choledochoduodenostomy, and in patients with EST measured from ERC X-ray films before the stones were removed.
All data are expressed as mean ± standard deviation. Statistical analysis was performed with the χ2 test and Student’s t test. Probability differences of 0.05 or less were considered to be significant.
RESULTS
Background of Patients with Choledocholithiasis during the Initial Treatment
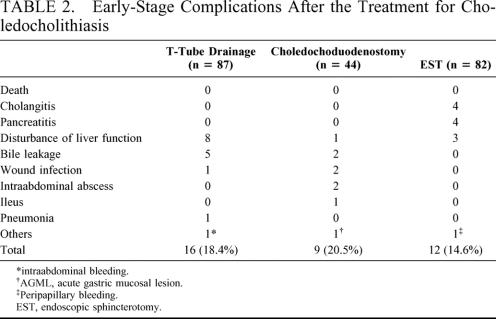
The mean age of patients with choledochoduodenostomy was 71.8 ± 11.8 years, whereas those with T-tube drainage was 64.5 ± 13.3 years (P = 0.025). The presence of biliary treatment history was found in 10 of the 77 patients with T-tube drainage (13.0%), and 18 of the 64 patients with EST (28.1%) (P = 0.029, Table 1). Complications within 1 month, such as liver disturbance and bile leakage, were observed in 16 of the 87 patients with T-tube drainage (18.4%), in 9 of the 44 with choledochoduodenostomy (20.5%), and in 12 of the 82 patients with EST (14.6%) (Table 2). None of the complications were life-threatening, and all of them improved with conservative treatment.
TABLE 1. Background of Patients During the Treatment for Choledocholithiasis
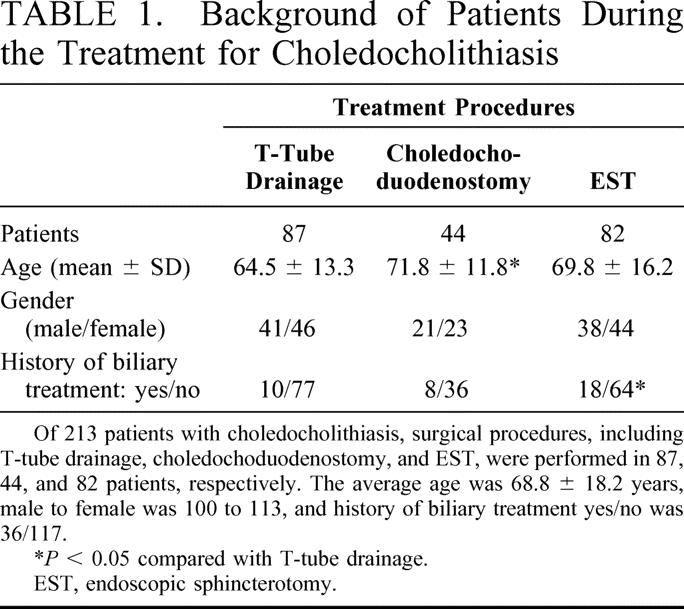
TABLE 2. Early-Stage Complications After the Treatment for Choledocholithiasis
Characteristics of Patients with Recurrent Stones after Treatment of Choledocholithiasis
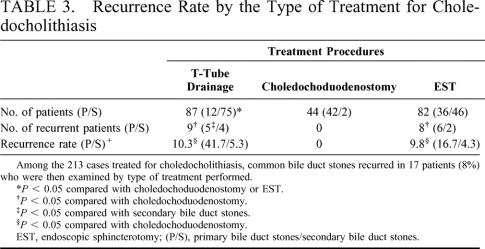
The patients treated with T-tube drainage had more secondary bile duct stones compared with the choledochoduodenostomy or EST groups (P < 0.0001). Secondary bile duct stones were more common (46 cases) than primary bile duct stones (36 cases) among cases with EST, and a significant difference was observed between EST and choledochoduodenostomy (P = 0.0001, Table 3). Common bile duct stones recurred in 9 of the 87 patients with T-tube drainage (10.3%), and a significant difference was observed when compared with nonrecurrent patients with choledochoduodenostomy (P = 0.03). Stones also recurred in 8 of the 82 patients with EST (9.8%), and a significant difference was observed when compared with nonrecurrent cases with choledochoduodenostomy (P = 0.03, Table 3). Moreover, stones recurred in 5 of 12 patients with primary bile duct stones (41.7%), whereas they recurred only in 4 of 75 cases with secondary bile duct stones (5.3%) (P = 0.0001). Among patients with EST, common bile duct stones recurred in 6 of the 36 patients with primary bile duct stones (16.7%), and 2 of the 46 patients with secondary bile duct stones (4.3%) (P = 0.06, Table 3).
TABLE 3. Recurrence Rate by the Type of Treatment for Choledocholithiasis
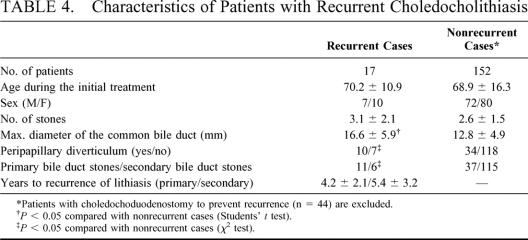
The 152 patients without recurrence of common bile duct stones, excluding 44 patients with choledochoduodenostomy to prevent recurrence were examined and compared to 17 patients with recurrent disease (Table 4). The maximum diameter of the common bile duct was 16.6 ± 5.9 mm in recurrent cases and 12.8 ± 4.9 mm in nonrecurrent cases, showing a significant difference between the 2 groups (P = 0.003). Although peripapillary diverticula was found in 10 of the 17 patients with recurrent cases (58.8%), it was observed in 34 of the 152 nonrecurrent cases (22.4%; P = 0.001). In addition, although primary bile duct stones were found in 11 of the 17 recurrent patients (64.7%), primary bile duct stones were found in 37 of the 152 nonrecurrent patients (24.3%) (P = 0.0005). The period of recurrence in recurrent cases was 4.2 ± 2.1 years for primary bile duct stones and 5.4 ± 3.2 years for secondary bile duct stones.
TABLE 4. Characteristics of Patients with Recurrent Choledocholithiasis
Digestive Disease after the Initial Treatment for Choledocholithiasis
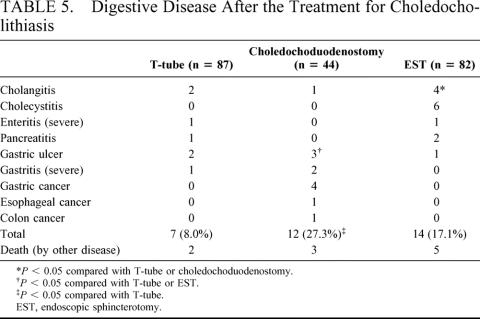
Digestive diseases that occurred during the follow-up and lasted at least 5 years from the time of treatment are shown in Table 5. Digestive diseases were found in 7 of the 87 patients with T-tube drainage (8.0%) and in 12 patients with choledochoduodenostomy (27.3%) (P = 0.03). Four patients with cholangitis were observed after EST, and the patients with preserved gallbladders had cholecystitis. Therefore, the incidence of post-EST biliary infection was higher than that of the patients with T-tube drainage (P = 0.01) or choledochoduodenostomy (P = 0.03). In the 9 patients with choledochoduodenostomy, gastric lesions were observed, including 3 patients with gastric ulcers requiring treatment with proton-pomp inhibitors, 2 patients with severe gastritis, and 4 patients with gastric cancer. They all showed a higher incidence of gastric lesions when compared to the patients with T-tube drainage (P = 0.001) or EST (P = 0.0005, Table 5).
TABLE 5. Digestive Disease After the Treatment for Choledocholithiasis
DISCUSSION
The incidence of choledocholithiasis is higher in Japan compared with Western countries. Between 1993 and 1995, 19,465 of the 105,062 patients treated for cholelithiasis in Japan had choledocholithiasis (18.5%).11 Choledocholithotomy and T-tube drainage, including the use of the laparoscopic method, have been performed in 78.3% of the patients treated for choledocholithiasis, and in only 9.5% of those treated for choledochoduodenostomy (or choledochojejunostomy). Papilloplasty was used widely in the past, but has now been replaced by EST.11 Although choledocholithotripsy (and T-tube drainage) is the most standard technique, laparoscopic method has become an increasingly more common procedure in many institutions.4–6 Although a secondary bile duct stone is a good indication of choledochotomy and sutures that use the laparoscopic method,4 some institutions attempt the transcystic approach because the diameter of the bile duct without any dilation is usually no more than 10 mm, making procedures, such as T-tube insertion and bile duct sutures, very difficult to perform (unless the surgeon is technically experienced).6 The transcystic approach is used to dilate the cystic duct with a balloon so that stones can be removed with the help of a cholangioscope, unfortunately this increases the risk of residual stones.6 It has been reported that the recurrence rate is high when only choledochotomy and T-tube drainage are performed, because the unchanged biliary structure keeps the environment of the common bile duct prone to lithogenesis.12 Indeed, the recurrence rate for choledocholithiasis was 41.7% when T-tube drainage was performed for primary bile duct stones in this study. This rate was significantly higher than the 5.3% recurrence rate seen when T-tube drainage was performed for secondary bile duct stones, suggesting that a simple T-tube drainage should be avoided for primary bile duct stones.
There are 2 types of choledochoenterostomy for choledocholithiasis: choledochojejunostomy with Roux-enY reconstruction and choledochoduodenostomy. Choledochojejunostomy is not commonly selected as a treatment option for choledocholithiasis as a result of the following reasons: 1) endoscopic extension cannot be performed when postoperative anastomotic stenosis has occurred; 2) the recurrent stone is a very intractable type of hepatolithiasis; and 3) the surgical techniques are complicated.13 To prevent recurrence, choledochojejunostomy is considered to be a good choice for patients with primary bile duct stones, cholangiectasis 15 mm or greater,14,15 or peripapillary diverticula.16 Recent reports on laparoscopic choledochoduodenostomy have suggested “side-to-side” anastomosis.17,18 Using this side-to-side anastomosis, the longitudinal incision in the anterior wall of the bile duct can be anastomosed with the incision in the anterior wall of the duodenal bulbus on the side of the lesser curvature of the stomach without the necessity of having to completely ablate the bile duct. The procedure is also easy to perform and can be used for high-risk patients.19 However, side-to-side anastomosis of the bile duct and the duodenum can cause foreign bodies to enter into the residual bile duct after surgery, triggering the onset of intractable and recurrent cholangitis and liver abscess, which is defined as sump syndrome.20,21 End-to-side anastomosis should be performed to prevent this intractable syndrome.
We performed end-to-side anastomosis for 38 patients. Although this procedure reduced the incidence of biliary infection, there were many unidentified complaints, such as gastric discomfort, when compared with patients who had T-tube drainage. These complications may be attributed to alkaline reflux gastritis associated with gastropyloric insufficiency.22 We reported 4 patients with gastric cancer during the 8 to 11 years after choledochoduodenostomy, which we suspect to be caused by the stimulation of bile acids such as chenodeoxycholic acid or cholic acid. It is important to monitor these patients very carefully after surgery, with special attention to the occurrence of upper digestive tract malignancies. We suggest that choledochojejunostomy may be the treatment of choice for younger patients with primary stones because it may avoid a long-term gastric problem.
When EST was first introduced in 1974, it was primarily used for bile duct stones that could not be removed through cholecystectomy.23 However, in a growing number of facilities, laparoscopic cholecystectomy is widely performed, with the combined use of laparoscopic cholecystectomy and EST regarded as the first-choice treatment for choledocholithiasis complicated by cholecystolithiasis from the standpoint of “minimum surgery”.24–26 Early-stage complications after EST have been reported at 6.4 to 15.8%, including hemorrhage, pancreatitis, and perforation of the digestive tract.24–27 With respect to long-term post-EST complications, cholangitis occurred in 4 of the 82 patients that were followed up for at least 5 years, and cholecystitis occurred in 6 of the 8 patients whose gallbladder had not been extirpated during EST as the result of a poor prognosis. The incidence of such biliary infections was significantly higher when compared with patients with T-tube drainage or choledochoduodenostomy. These observations were congruent with many reports,28,30 and an effort has been made to perform laparoscopic cholecystectomy after EST. In our hospital, the recurrence of choledocholithiasis after EST was 2.8% in cases with secondary bile duct stones and 12.2% with primary bile duct stones. According to Kim et al, stones recur in 21.3% of patients with primary bile duct stones. The reason for such a high incidence has been attributed to the presence of peripapillary diverticula and a dilated common bile duct.31
The primary cause of post-EST cholangitis might be dysfunction of the sphincter of Oddi caused by EST. This does not conflict with the report that the incidence of cholangitis and the incidence of recurrent lithiasis increase with age when EST is performed, especially in young patients.32 Based on such findings, many institutions are beginning to perform EPBD, particularly in young patients, to protect and maintain the function of the papillary muscle.1,33 Currently, EPBD is the first-choice treatment at our institution for patients 60 years of age or younger with secondary bile duct stones. One of the best treatments for causing a minimum amount of discomfort in patients is ESWL. According to our survey in Japan, stones were completely removed by ESWL alone in 44.6% of patients nationwide.34 This is related to the fact that most choledocholiths are bilirubin calcium stones and not the cholesterol stones that are the targets for ESWL, especially for poor-risk patients with secondary cholesterol stones.2,34
Although the basic principle for treatment of choledocholithiasis is to determine how to best remove the stones by choosing among the many treatment modalities, there has been no report showing the precise statistics concerning the recurrence rate for choledocholithiasis based on the type of treatment.
Footnotes
Reprints: Hiroki Yamaue, MD, Second Department of Surgery, Wakayama Medical University, School of Medicine, 811-1 Kimiidera, Wakayama 641-8510, Japan. E-mail: yamaue-h@wakayama-med.ac.jp.
REFERENCES
- 1.Bhasin DK, Sinha SK. Comparing the treatment outcomes of endoscopic papillary dilation and endoscopic sphincterotomy for removal of bile duct stones. Gastrointest Endosc. 1999;50:886–888. [PubMed] [Google Scholar]
- 2.Meyenberger C, Meierhofer U, Michel-Harder C, et al. Long-term follow-up after treatment of common bile duct stones by extracorporeal shock-wave lithotripsy. Endoscopy. 1996;28:411–417. [DOI] [PubMed] [Google Scholar]
- 3.Sugiyama M, Atomi Y. Medium-term effects of endoscopic papillary balloon dilation on gallbladder motility. Gastrointest Endosc. 2001;54:459–463. [DOI] [PubMed] [Google Scholar]
- 4.Lauter DM, Froines EJ. Laparoscopic common duct exploration in the management of choledocholithiasis. Am J Surg. 2000;179:372–374. [DOI] [PubMed] [Google Scholar]
- 5.Uchiyama K, Takifuji K, Tani M, et al. Effectiveness of the clinical pathway to decrease length of stay and cost for laparoscopic surgery. Surg Endosc. 2002;16:1594–1597. [DOI] [PubMed] [Google Scholar]
- 6.Fitzgibbons RJ Jr, Gardner GC. Laparoscopic surgery and the common bile duct. World J Surg. 2001;25:1317–1324. [DOI] [PubMed] [Google Scholar]
- 7.Tanaka M, Takahata S, Konomi H, et al. Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc. 1998;48:465–469. [DOI] [PubMed] [Google Scholar]
- 8.Bergman JJ, van de Mey S, Rauws EA, et al. Long-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc. 1996;44:643–649. [DOI] [PubMed] [Google Scholar]
- 9.Hammarstrom LE, Stridbeck H, Ihse I. Long-term follow-up after endoscopic treatment of bile duct calculi in cholecystectomized patients. World J Surg. 1996;20:272–276. [DOI] [PubMed] [Google Scholar]
- 10.Saharia PC, Zuidema GD, Cameron JL. Primary common duct stones. Ann Surg. 1977;185:598–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uchiyama K, Tanimura H, Ishimoto K. Hepatolithiasis in Japan. Arch Jpn Chir. 1996;65:145–157. [PubMed] [Google Scholar]
- 12.Lygidakis NJ. Surgical approaches to recurrent choledocholithiasis. Choledochoduodenostomy versus T-tube drainage after choledochotomy. Am J Surg. 1983;145:636–639. [DOI] [PubMed] [Google Scholar]
- 13.Uchiyama K, Onishi H, Tani M, et al. Indication and procedure for treatment of hepatolithiasis. Arch Surg. 2002;137:149–153. [DOI] [PubMed] [Google Scholar]
- 14.Parrilla P, Ramirez P, Sanchez Bueno F, et al. Long-term results of choledochoduodenostomy in the treatment of choledocholithiasis: assessment of 225 cases. Br J Surg. 1991;78:470–472. [DOI] [PubMed] [Google Scholar]
- 15.Deutsch AA, Nudelman I, Gutman H, Reiss R. Choledochoduo-denostomy an important surgical tool in the management of common bile duct stones. A review of 126 cases. Eur J Surg. 1991;157:531–533. [PubMed] [Google Scholar]
- 16.Miyazawa Y, Okinaga K, Nishida K, et al. Recurrent common bile duct stones associated with periampullary duodenal diverticula and calcium bilirubinate stones. Int Surg. 1995;80:120–124. [PubMed] [Google Scholar]
- 17.Tinoco R, El-Kadre L, Tinoco A. Laparoscopic choledochoduodenostomy. J Laparoendosc Adv Surg Tech A. 1999;9:123–126. [DOI] [PubMed] [Google Scholar]
- 18.Gurbuz AT, Watson D, Fenoglio ME. Laparoscopic choledochoduodenostomy. Am Surg. 1999;65:212–214. [PubMed] [Google Scholar]
- 19.Aramaki M, Ikeda M, Kawanaka H, et al. Choledochoduodenostomy: simple side-to-side anastomosis. J Hepatobiliary Pancreat Surg. 2000;7:486–488. [DOI] [PubMed] [Google Scholar]
- 20.Hiura A, Kim EC, Ikehara T, et al. Hepatic abscess as a complication of the sump syndrome. J Hepatobiliary Pancreat Surg. 2000;7:231–235. [DOI] [PubMed] [Google Scholar]
- 21.Khan TF, Sherazi ZA, Muniandy S, et al. Recurrent pyogenic cholangitis: ‘sump syndrome’ following choledochoduodenostomy. Trop Doct. 1997;27:51–52. [DOI] [PubMed] [Google Scholar]
- 22.Mihmanli M, Isgor A, Erzurumlu K, et al. Long-term results of choledochoduodenostomy and T-tube drainage. Hepatogastroenterology. 1996;43:1480–1483. [PubMed] [Google Scholar]
- 23.Kawai K, Akasaka Y, Murakami K, et al. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20:148–151. [DOI] [PubMed] [Google Scholar]
- 24.Pereira-Lima JC, Rynkowski CB, Rhoden EL. Endoscopic treatment of choledocholithiasis in the era of laparoscopic cholecystectomy: prospective analysis of 386 patients. Hepatogastroenterology. 2001;48:1271–1274. [PubMed] [Google Scholar]
- 25.Contractor QQ, Dubian MK, Boujemla M, et al. Endoscopic therapy after laparoscopic cholecystectomy. J Clin Gastroenterol. 2001;33:218–222. [DOI] [PubMed] [Google Scholar]
- 26.Ganci-Cerrud G, Chan C, Bobadilla J, et al. Management of choledocholithiasis found during laparoscopic cholecystectomy: a strategy based on the use of postoperative endoscopic retrograde cholangiography and sphincterotomy. Rev Invest Clin. 2001;53:17–20. [PubMed] [Google Scholar]
- 27.Binmoeller KF, Schafer TW. Endoscopic management of bile duct stones. J Clin Gastroenterol. 2001;32:106–118. [DOI] [PubMed] [Google Scholar]
- 28.Yi SY. Recurrence of biliary symptoms after endoscopic sphincterotomy for choledocholithiasis in patients with gall bladder stones. J Gastroenterol Hepatol. 2000;15:661–664. [DOI] [PubMed] [Google Scholar]
- 29.Pereira-Lima JC, Jakobs R, Winter UH, et al. Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998;48:457–464. [DOI] [PubMed] [Google Scholar]
- 30.Coppola R, Riccioni ME, Ciletti S, et al. Analysis of complications of endoscopic sphincterotomy for biliary stones in a consecutive series of 546 patients. Surg Endosc. 1997;11:129–132. [DOI] [PubMed] [Google Scholar]
- 31.Kim DI, Kim MH, Lee SK, et al. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001;54:42–48. [DOI] [PubMed] [Google Scholar]
- 32.Bergman JJ, van der Mey S, Rauws EA, et al. Long-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc. 1996;44:643–649. [DOI] [PubMed] [Google Scholar]
- 33.Yasuda I, Tomita E, Enya M, et al. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001;49:686–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Uchiyama K, Tanimura H, Ishimoto K, et al. Extra-corporeal shock wave lithotripsy (ESWL) for biliary stones; A nation wide survey in Japan. Arch Jpn Chir. 1994;63:199–207. [PubMed] [Google Scholar]