Abstract
Objective:
To evaluate how age affects functional outcome and quality of life after ileal pouch anal anastomosis (IPAA).
Summary Background Data:
Because of the limited number of older patients undergoing IPAA, it has been difficult to assess functional outcome and quality of life stratified by age.
Methods:
IPAA was performed in 1895 patients. Patients were stratified by age into <45 (n = 1410), 46–55 (n = 289), 56–65 (n = 154), and more than 65 years (n = 42). Outcome was assessed prospectively. Results are presented at 1, 3, 5, and 10 years after surgery.
Results:
Patients were followed for 4.6 ± 3.7 years (maximum, 17 years). Pouch failure occurred in 4.1% (pouch excision or permanent diversion). Incontinence and night time seepage were more common in older patients. There were minor differences in the quality of life, health, energy and happiness between age groups, with a slight benefit for those under 45 years. Fourteen percent or fewer patients experienced social, sexual or work restrictions. Overall, 96% of patients were happy to have undergone their surgery, and 98% recommended it to others. Although the respective figures were 89% and 96% in the over-65 age group, the difference was not significant.
Conclusions:
These data provide a unique assessment of outcome after IPAA at multiple time points. Although functional outcome after IPAA is not as good in older patients, appropriate case selection confers acceptable function and quality of life to patients of all ages.
One thousand eight hundred and ninety five patients who underwent ileal pouch-anal anastomosis since 1983 were grouped by age and analyzed after 1, 3, 5 and 10 years. Although functional outcome was not as good in those over 65 years, quality of life was similar at all ages and over 96% of patients were happy with the results of their surgery. Appropriate case selection confers acceptable outcome for all patients.
Proctocolectomy and reconstruction with an ileal pouch-anal anastomosis (IPAA) has become the operation of choice for patients with ulcerative colitis and familial polyposis.1–6 The procedure is a particularly good option for patients with ulcerative colitis who can be offered an excellent quality of life while avoiding a permanent ostomy.7–9 Many studies have reported the relative benefits of IPAA, but these have concentrated on younger patient populations or have presented data across a range of ages.2,10
The complexity of IPAA leads surgeons to perform this procedure on “ideal” candidates who were young and in good health apart from their intestinal disease. Complications, such as pelvic sepsis, high stool frequency, fecal incontinence, evacuation disorders, and overall pouch failure rates lead some authors to suggest that IPAA should not be performed in patients over 50 years of age.11 Alterations in surgical technique over the last decade, including the double-stapled pouch-anal anastomosis without anal canal mucosectomy, have been suggested to improve outcome in these patients.12–14
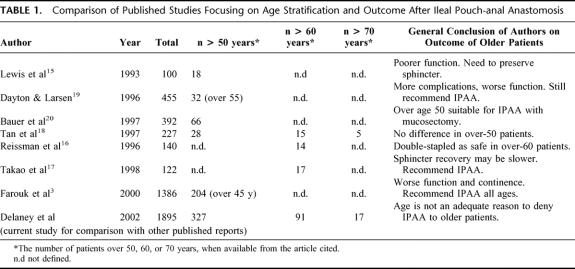
Although there is no defined age cut-off for patients having IPAA, many would suggest 60 or 65 years as the upper limit. Little evidence supports this recommendation, but the relative infrequency of IPAA in older patients has made it difficult to stratify patients by age while maintaining adequate numbers for analysis. Several studies have compared the outcome of IPAA in different age groups of patients.15–20 However, the small number of patients in these series has prevented an accurate assessment of the complications and functional outcome of IPAA, particularly in the older age groups. Furthermore, the evaluation in all published series to date has been made at 1 time point only after IPAA, and has not included an evaluation of quality of life after surgery.
In this study, we prospectively evaluated the functional outcome and quality of life in 1895 patients who had undergone IPAA and who had at least 6 months postoperative follow-up at the time of this study. Patients were stratified by age at the time of surgery into those younger than 45 years, those between 46 and 55 years, 56 and 65 years, and more than 65 years. Functional outcome and quality of life data are presented for multiple points, namely 1, 3, 5, and 10 years of follow-up. This provides a unique perspective of the outcome of IPAA surgery over a long period of time, which in turn permits an accurate, focused discussion to be had with patients of all ages who are candidates for proctocolectomy and IPAA.
MATERIALS AND METHODS
Between 1983 and 1999, 1895 patients underwent IPAA and had at least 6 months postoperative follow-up. Patients were stratified by their age at the time of undergoing IPAA surgery. Stratification was into those less than 45 years of age at the time of surgery; those from 46 to 55 years at surgery; those from 56 to 65 years at surgery; and those 65 years or older at the time of surgery. Surgery involved formation of an ileo-anal J pouch with two 20-cm limbs or an ileo-anal S-pouch with three 15-cm limbs.
Functional Outcome and Complications
Functional outcome, pouch salvage rates and quality of life parameters were obtained from a prospectively maintained database for all available follow-up visits, as previously described and validated.21 Patients were asked to complete a self-administered, structured questionnaire at each return visit to the office. If the patient did not attend for over 1 year, the information was requested by means of the same questionnaire delivered by mail.
Patients completed questions on the number of bowel motions during daytime and at night. The presence of urgency was defined as the inability to defer defecation for more than 30 minutes. Incontinence was defined by the patient themselves, and they classified their own incontinence as never, rarely, sometimes, mostly or always. Also assessed were the requirements for pad usage and the presence of fecal seepage.
Quality of Life and Satisfaction with Surgery
Quality of life was assessed by using the Cleveland Global Quality of Life (CGQL) score, as described and validated recently.21 This scale determines global QOL on a serial basis after IPAA. Patients were asked to score 3 items: current quality of life, current quality of and health, and current level of energy. Each was graded on a scale of 0–10, where 0 was worst and 10 was the best possible score. The final CGQL score was then calculated by dividing the total by 30.
Overall happiness with surgery was graded by the patients from 1 to 10, with 10 representing complete satisfaction with the procedure. Patients were also asked at each office visit whether they would undergo the same operation again if it was needed, and whether they would recommend the operation to someone else with the same diagnosis.
Pouch Failure
Pouch failure was defined as excision of the ileo-anal pouch, permanent diversion with a proximal diverting loop ileostomy, or long-term nonclosure of the defunctioning stoma. Whether patients underwent a repeat reconstruction with a revised IPAA, or continent ileostomy at the time of pouch failure, they were still classed as pouch failure for the purpose of this study.
Statistical Analysis
Data were analyzed for follow-up at 1, 3, 5 and 10 years after surgery. As patients could return more than 1 time over each time period, data from the closest visit to each time point was chosen, with a cut-off of ± 6 or 12 months. Data for 1 year follow-up included all patients who returned between 6 and 18 months after surgery, whereas data for 3, 5, and 10 years included anyone returning within a 1-year period from each data point. Thus, visits more than 12 months away from 1, 3, 5, and 10 years were censored. The closest visit was used for each patient; for example, if a patient had follow-up at 33 and 41 months, the event at 33 months would be used.
The tables summarize categorical variables in terms of frequencies and percentages, within age categories. Quantitative data are summarized within terms of mean ± and also as the median with 25th and 75th percentiles. Overall and pair-wise age group comparisons were performed by using the Fisher exact test or χ2 test with respect to categorical variables. Multivariable logistic regression models were used to compare age groups while adjusting for effects of gender, type of pouch, type of anastomosis, and final pathologic diagnosis. The Bonferroni correction was applied to the pairwise tests, maintaining overall significance at 0.05. Overall comparisons with respect to quantitative data were performed by the Kruskal–Wallis test. Pairwise age group comparisons for the quantitative variables were performed by using Dunn’s test, which also preserved overall 0.05 significance levels. Adjustments for gender, pouch type, anastomosis type, and final diagnosis were made by using analysis of covariance with Scheffe pairwise comparisons of age groups. The particular pairwise comparisons that yielded significance are designated by footnotes. Data were analyzed by using SPSS software (SPSS Inc., Chicago, IL), and P < 0.05 was accepted as a significant result.
RESULTS
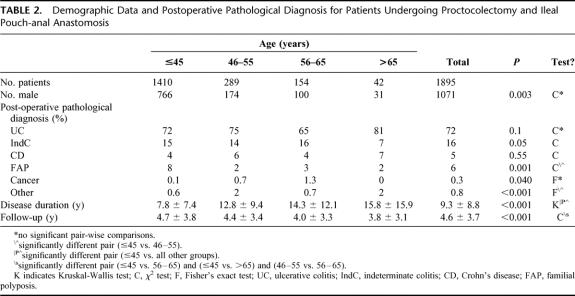
Patients were stratified by age at multiple time points, and 435 patients were over the age of 50 years at the time of surgery, whereas 485 were over 45 years (Tables 1 and 2). There was an overall significant difference in male/female ratios between age groups, but none reached significance in pairwise comparison.
TABLE 1. Comparison of Published Studies Focusing on Age Stratification and Outcome After Ileal Pouch-anal Anastomosis
TABLE 2. Demographic Data and Postoperative Pathological Diagnosis for Patients Undergoing Proctocolectomy and Ileal Pouch-anal Anastomosis
When the indication for surgery was analyzed (as defined by pathologic diagnosis from the surgical specimen), there was a significant age-related difference in indication for surgery for ulcerative colitis (most frequent in patients more than 65 year of age), familial polyposis (most frequent in patients less than 45 years), and cancer (most frequent in patients 56-65 years), as described in Table 2. There was also a difference in the disease duration before surgery, with the youngest subgroup having the shortest disease duration before surgery. Follow-up was 4.6 ± 3.7 years overall, with the oldest patients having shortest follow-up.
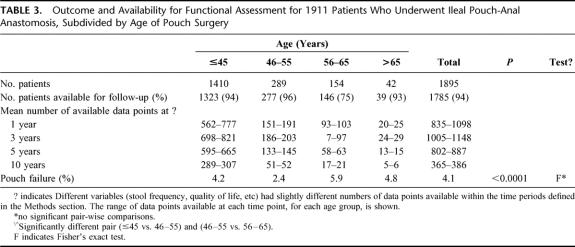
Availability for Assessment and Pouch Failure Rates
Peri-operative data were available for all patients from the database. Long-term follow-up data (regarding quality of life and functional outcome) were available for 94% of patients. Many of these patients had multiple follow-up visits, and had completed pouch database questionnaires at more than 1 visit. Thus, there were a total of 6247 follow-up points available for 1785 patients for functional and quality of life analysis.
Pouch failure (Table 3) occurred in 4.1% of cases, with no significant difference between subgroups when divided by age. Failure occurred least frequently in those less than 56 years of age at the time of surgery. Eight of the patients with failure had a continent ileostomy (Kock pouch) fashioned at the time of pouch excision. Five further patients underwent revision of their IPAA.
TABLE 3. Outcome and Availability for Functional Assessment for 1911 Patients Who Underwent Ileal Pouch-Anal Anastomosis, Subdivided by Age of Pouch Surgery
Operative Details
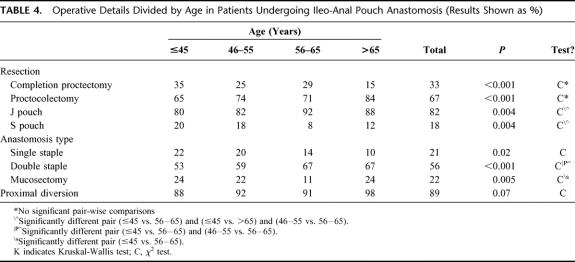
Subtotal colectomy with end ileostomy or ileo-rectal anastomosis was performed as a staged procedure prior to proctectomy and IPAA in a greater percentage of younger patients (generally for familial polyposis), but there was no significant difference between groups in pairwise comparison (Table 4). Older patients were more likely to undergo removal of the colon and rectum at the same time as IPAA.
TABLE 4. Operative Details Divided by Age in Patients Undergoing Ileo-Anal Pouch Anastomosis (Results Shown as %)
The ileal pouch was formed most frequently with a ‘J’ configuration, with an increased frequency in the older patients. The ileal pouch-anal anastomosis was fashioned most frequently with the double stapled technique, particularly in the older age groups. Mucosectomy (with hand-sewn anastomosis) was the next most common technique of anastomosis, although it was performed slightly less frequently in the 56–65 age group. The single-stapled technique was performed less frequently, particularly in recent years.
Temporary proximal diversion was performed by making a loop ileostomy 30 to 60 cm above the ileal pouch at the time of surgery. These temporary stomas were left in position for 3 months in routine cases, and somewhat longer in patients with postoperative anastomosis-related complications. A loop ileostomy was used in 89% of patients. Although there were no significant differences between groups, a loop ileostomy was used in 98% of patients over 65 years of age.
Functional Outcome at 1, 3, 5, and 10 Years After IPAA
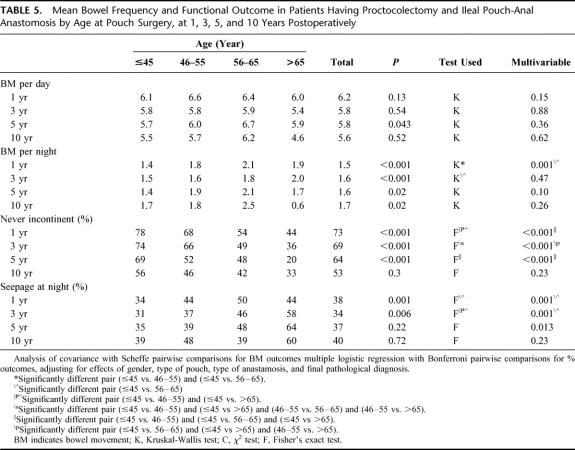
There was no major difference in day-time stool frequency between groups (Table 5). Mean stool frequency was 6.2 motions per day, falling to 5.6 motions at 10 years. Stool frequency was increased to 6.7 in 56–65 year olds at 5 years, but this is of uncertain clinical significance. Nighttime stool frequency was between 1.3 and 1.8, with the lowest frequency in those under 45 years. Although, this overall difference between groups was maintained at all times, the significant difference between subgroups was absent after 1 year using multivariate analysis.
TABLE 5. Mean Bowel Frequency and Functional Outcome in Patients Having Proctocolectomy and Ileal Pouch-Anal Anastomosis by Age at Pouch Surgery, at 1, 3, 5, and 10 Years Postoperatively
The percentage of those who had perfect continence (“never incontinent”) was highest in patients who underwent surgery when they were less than 45 or 55 years of age. This difference was maintained at 1, 3, and 5 years but was lost at 10 years of follow-up. Some patients had minor seepage at night. Many patients did not classify this as incontinence. The incidence of night time seepage was lowest in patients under 45 years of age, however this primarily reached statistical significance when comparing those under 45 years to older cohorts. Overall, approximately 35–40% of patients had some night-time seepage over the 10 years of follow-up.
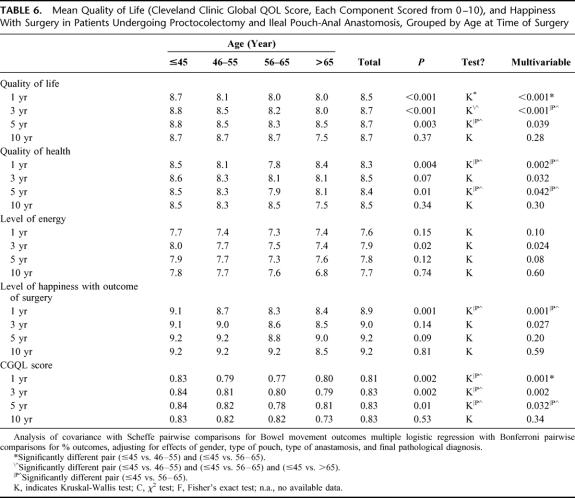
Quality of Life and Health and Level of Happiness with Surgery at 1, 3, 5, and 10 Years After IPAA
Quality of life and health, and level of energy and happiness were each scored on a scale of 0 (worst) to 10 (best) for each parameter (Table 6). Quality of life was scored as 8.5–8.7 of 10 during the course of the study. After 1, 3, and 5 years of follow-up, this was very slightly higher for those having surgery under 45 years of age, when compared with older patients. Quality of health and level of energy tended to be better at 1, 3, and 5 years for patients less than 45 years undergoing IPAA, reaching statistical significance by univariate and multivariate analysis. Except for a slight reduction in the level of happiness with the outcome of surgery at 1 year (lowest in the over 56 cohort, but no significant difference between groups after 1 year postoperative), there was no difference in level of happiness with surgery at 1, 3, 5, or 10 years of follow-up. CGQL scores also tended to be better in patients under 45 years of age at 1, 3, and 5 years of follow-up.
TABLE 6. Mean Quality of Life (Cleveland Clinic Global QOL Score, Each Component Scored from 0–10), and Happiness With Surgery in Patients Undergoing Proctocolectomy and Ileal Pouch-Anal Anastomosis, Grouped by Age at Time of Surgery
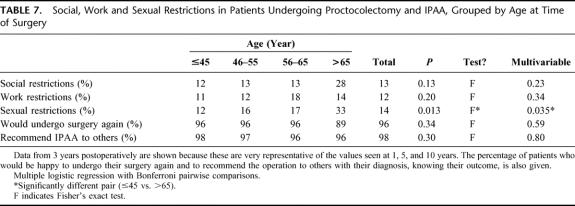
Patients were also asked whether they experienced any social, work or sexual restrictions (Table 7). At 1 year of follow-up, there was a smaller risk of social (8.5%), work (12.1%), and sexual (8.8%) restrictions in those patients less 45 years at surgery when compared with those in older age groups (approximately 20% social restrictions, 20% work restrictions, and 20% sexual restrictions). These differences between groups were not present at 3 years of follow-up, except for sexual function between patients <45 and >65 years. Sexual restrictions increased over time in those who were aged under 45 at the time of surgery, reaching 11.4% at 10 years. The data at 3 years of follow-up are extremely representative of those found at 5 and 10 years of follow-up and are therefore shown in Table 7.
TABLE 7. Social, Work and Sexual Restrictions in Patients Undergoing Proctocolectomy and IPAA, Grouped by Age at Time of Surgery
Finally, patients were asked whether they would undergo their surgery again, and also whether they would recommend IPAA to someone else with the same diagnosis (Table 7). There were no significant differences between groups at any time point. At 1 year of follow-up, between 95% and 98% of all groups would recommend their surgery to others, and 95% to 97% would undergo their surgery again. After 3 years of follow-up, 96% of patients would undergo IPAA again, rising slightly to 98% at 10 years. In contrast, 98% of patients would recommend their experience to others at 3, 5, and 10 years.
DISCUSSION
Ileal pouch-anal anastomosis was described in the late 1970s as a new alternative to nonrestorative proctocolectomy, the continent ileostomy, or ileo-rectal anastomosis.1 Because of the complexity of the operation, the indications for this type of surgery were initially conservative. Thus, only “ideal” candidates were selected for IPAA because of concerns, including high rates of pelvic sepsis, evacuation disorders, stool frequency rates, and incontinence, and a failure rate of up to 10%. As a result, the centers doing the highest volume of this surgery arbitrarily chose upper age limits of 50, 55, or 60 years to be as safe as possible, publishing series as portrayed in Table 1. The subsequent decade provided a number of surgical advances that have helped reduce the complications of surgery and have lead to improved functional outcome and quality of life. Techniques, such as preservation of the anal transitional zone, using a circular stapler to perform the ileo-anal anastomosis without requiring dilating retractors to place sutures by hand, and avoiding a long muscular cuff after mucosal proctectomy, have all helped to reduce pelvic sepsis rates and contribute to a better functional outcome.12–14 With these improvements in the surgical approach, and increasing experience with the technique, consideration was given to whether selection criteria for IPAA were too strict. Were patients who should be offered an ileal pouch7 denied surgery because of unnecessary concerns about poor functional outcome related to their age?
In this work we presented a univariate and multivariate analysis of data on the functional outcome and quality of life in 1895 patients who underwent IPAA for the indications in Table 2. To address our primary concern of outcome related to age at the time of surgery, patients were stratified into 4 groups, and evaluated at multiple time points. As the functional outcome and quality of life can change with time postoperatively, data are presented at 4 individual follow-up times: 1, 3, 5, and 10 years postoperatively. The perioperative details and technique used for fashioning the IPAA was similar between groups (Table 4). As an increasing number of older patients underwent IPAA in recent years, they tended to have a double-stapled J-pouch, with preservation of the anal transitional zone and minimal sphincter dilation.
Because IPAA has been performed more frequently in recent years, mean follow-up was 4.6 ± 3.7 years, however some patients had follow-up since 1983 when the first IPAA was performed at this institution. Only 4.1% of patients developed failure of their IPAA for long-term complications of surgery or poor function.
Functional results were not as good in patients in the older groups. This was manifested by a slight reduction in the percentage with perfect continence, and a slight increase in the number with seepage of stool at night, although many patients did not classify this as incontinence. Daytime and nighttime stool frequencies were generally similar between groups (Table 5).
Although as physicians we might perceive this reduction in continence as a poor outcome, the patients were not as disappointed. There were slight differences between groups for quality of life outcome criteria (Table 6), some of which reached statistical significance. These were apparent as trends to higher scores for quality of life and health, and levels of energy and happiness in patients under 45 years at the time of surgery, however it was impossible to find significant differences between older age groups, with either univariate or multivariate analysis.
The problem is that quality of life scores may not directly equate to the desire of the patient to keep the IPAA. Even using the Cleveland Global Quality of Life score,21 the only validated score after IPAA surgery, it is difficult to gauge whether a drop in quality of life from 0.83 to 0.79 should equate with performing, or not performing IPAA surgery. Indeed, this is the problem with most quality of life systems, which tend to show minimal differences in quality of life between permanent ileostomy and IPAA, and yet maintenance of continence is the primary concern of colitis patients being considered for surgery.
As a consequence, we feel that the most important questions to address when talking to patients after IPAA is whether they would be happy to undergo their surgery again, and whether they would recommend it to others. Between 95% and 100% of patients under 65 would undergo their surgery again, and 96-100% would recommend it to others. It is hard to imagine improving on these figures. For patients more than 65 years of age at the time of surgery, 89-100% would undergo their surgery again, whereas 93-100% would be happy to recommend it to others at different times of follow-up. The specific complications that patients over 70 years of age experienced and their functional and manometric outcome are the subject of another report by these authors.22 Because the large majority of patients more than 65 years, and indeed those over 70 years, experienced a good result and were happy to recommend it to others, we feel that these patients should be offered IPAA, but that discussion of the risks and benefits of surgery is particularly important for this age group. Furthermore, it is critical to have a highly motivated group of patients who are otherwise in excellent health prior to construction of an IPAA.
In conclusion, IPAA provides a very satisfactory quality of life and functional outcome in patients who require proctocolectomy for their disease. Patients under 45 years of age at the time of surgery experience the best functional result. Careful discussion of the procedure and outcome with individual patients allows prudent case selection, yielding a high percentage of patients of all ages who are happy with their postoperative outcome, and who are happy to recommend it to other patients with the same diagnosis.
Footnotes
Reprints: Victor W. Fazio, MB, MS, FRACS, FRACS(Hon), Department of Colorectal Surgery, A-30, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, OH 44195. E-mail: faziov@ccf.org.
REFERENCES
- 1.Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. Br Med J. 1978;ii:85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fazio VW, Ziv Y, Church JM, et al. Ileal pouch-anal anastomoses complications and function in 1005 patients. Ann Surg. 1995;222:120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farouk R, Pemberton JH, Wolff BG, et al. Functional outcomes after ileal pouch-anal anastomosis for chronic ulcerative colitis. Ann Surg. 2000;231:919–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Provenzale D, Shearin M, Phillips-Bute BG, et al. Health-related quality of life after ileoanal pull-through evaluation and assessment of new health status measures. Gastroenterology. 1997;113:7–14. [DOI] [PubMed] [Google Scholar]
- 5.Pemberton JH, Phillips SF, Ready RR, et al. Quality of life after Brooke ileostomy and ieal pouch anal anastomosis. Ann Surg. 1989;209:620–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcello PW, Roberts PL, Schoetz DJ, et al. Long-term results of the ileo-anal pouch procedure. Arch Surg. 1993;128:500–504. [DOI] [PubMed] [Google Scholar]
- 7.Sagar PM, Lewis W, Holdsworth PJ, et al. Quality of life after restorative proctocolectomy with a pelvic ileal reservoir compares favorably with that of patients with medically treated colitis. Dis Colon Rectum. 1993;36:584–592. [DOI] [PubMed] [Google Scholar]
- 8.McLeod RS, Churchill DN, Lock AM, et al. Quality of life of patients with ulcerative colitis preoperatively and postoperatively. Gastroenterology. 1991;101:1307–1313. [DOI] [PubMed] [Google Scholar]
- 9.Kelly KA. Anal sphincter-saving operations for chronic ulcerative colitis. Am J Surg. 1992;163:5–11. [DOI] [PubMed] [Google Scholar]
- 10.Bauer JJ, Gorfine SR, Gelernt IM, et al. Restorative proctocolectomy in patients older than fifty years. Dis Colon Rectum. 1997;40:562–565. [DOI] [PubMed] [Google Scholar]
- 11.Setti-Carraro P, Ritchie JK, Wilkinson KH, et al. The first 10 years’ experience of restorative proctocolectomy for ulcerative colitis. Gut. 1994;35:1070–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lavery IC, Tuckson WB, Easley KA. Internal anal sphincter function after total abdominal colectomy and stapled ileal pouch anal anastomosis without mucosal proctectomy. Dis Colon Rectum. 1989;32:950–953. [DOI] [PubMed] [Google Scholar]
- 13.Tuckson WB, Lavery IC, Fazio VW, et al. Manometric and functional comparison of ileal pouch anal anastomosis with and without anal manipulation. Am J Surg. 1991;161:90–96. [DOI] [PubMed] [Google Scholar]
- 14.Ziv Y, Fazio VW, Church J, et al. Stapled ileal pouch anal anastomoses are safer than handsewn anastomoses in patients with ulcerative colitis. Am J Surg. 1996;171:320–323. [DOI] [PubMed] [Google Scholar]
- 15.Lewis WG, Sagar PM, Holdsworth PJ, et al. Restorative proctocolectomy with end to end pouch-anal anastomosis in patients over the age of fifty. Gut. 1993;34:948–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reissman P, Teoh TA, Weiss EG, et al. Functional outcome of the double stapled ileoanal reservoir in patients more than 60 years of age. Am Surg. 1996;62:178–183. [PubMed] [Google Scholar]
- 17.Takao Y, Gilliland R, Nogueras JJ, et al. Is age relevant to functional outcome after restorative proctocolectomy for ulcerative colitis: prospective assessment of 122 cases. Ann Surg. 1998;227:187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan HT, Connolly AB, Morton D, et al. Results of restorative proctocolectomy in the elderly. Int J Colorectal Dis. 1997;12:319–322. [DOI] [PubMed] [Google Scholar]
- 19.Dayton MT, Larsen KR. Should older patients undergo ileal pouch-anal anastomosis? Am J Surg. 1996;172:444–448. [DOI] [PubMed] [Google Scholar]
- 20.Bauer JJ, Gorfine SR, Gelernt IM, et al. Restorative proctocolectomy in patients older than fifty years. Dis Colon Rectum. 1997;40:562–565. [DOI] [PubMed] [Google Scholar]
- 21.Fazio VW, O’Riordain MG, Lavery IC, et al. Long term function and quality of life after stapled restorative proctocolectomy. Ann Surg. 1999;230:575–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Delaney CP, Dadvand B, Remzi FH, et al. Functional outcome, quality of life, and complications after ileal pouch-anal anastomosis in septuagenarians. Dis Colon Rectum. 2002;45:890–894. [DOI] [PubMed] [Google Scholar]