Abstract
Objective:
Aimed at reducing surgical deaths, several recent initiatives have attempted to establish volume-based referral strategies in high-risk surgery. Although payers are leading the most visible of these efforts, it is unknown whether volume standards will also reduce resource use.
Methods:
We studied postoperative length of stay and 30-day readmission rate after 14 cardiovascular and cancer procedures using the 1994-1999 national Medicare database (total n = 2.5 million). We used regression techniques to examine the relationship between length of stay, 30-day readmission, and hospital volume, adjusting for age, gender, race, comorbidity score, admission acuity, and mean social security income.
Results:
Mean postoperative length of stay ranged from 3.4 days (carotid endarterectomy) to 19.6 days (esophagectomy). There was no consistent relationship between volume and mean length of stay; it significantly increased across volume strata for 7 of the 14 procedures and significantly decreased across volume strata for the other 7. Mean length of stay at very-low-volume and very-high-volume hospitals differed by more than 1 day for 6 procedures. Of these, the mean length of stay was shorter in high-volume hospitals for 3 procedures (pancreatic resection, esophagectomy, cystectomy), but longer for other procedures (aortic and mitral valve replacement, gastrectomy). The 30-day readmission rate also varied widely by procedure, ranging from 9.9% (nephrectomy) to 22.2% (mitral valve replacement). However, volume was not related to 30-day readmission rate with any procedure.
Conclusion:
Although hospital volume may be an important predictor of operative mortality, it is not associated with resource use as reflected by length of stay or readmission rates.
In this study based on the national Medicare population, we examined length of stay and 30-day readmission rates with 14 cardiovascular and cancer procedures. Hospital procedure volume was not consistently related to either measure.
As evidence mounts that high-volume hospitals have better outcomes in selected surgical procedures,1-4 interest in volume-based referral initiatives is growing. Among the most visible of these, the Leapfrog group, a coalition of public and private payers representing more than 30 million patients, is encouraging patients to undergo surgery at hospitals meeting minimum volume standards for 5 high-risk procedures.5 Although the primary impetus for these efforts is reducing mortality, many also assume that high-volume hospitals will provide surgery less expensively than low-volume hospitals as a function of lower complication rates and better economies of scale.6-10
However, this assumption has not been well tested. Although prior studies have examined relationships between hospital volume and costs,7,11-25 most studies have relied on hospital charges (adjusted with cost-charge ratios), a notoriously poor surrogate for resource use.26 Their findings have varied widely, perhaps because of the heterogeneity in the procedures and populations on which these studies were based. Several studies have examined relationships between volume and length of stay, a popular surrogate for hospital costs. Although most suggested shorter length of stay at high-volume hospitals, many of these studies were based on relatively old data or information from individual states, which may not be broadly generalizable.13,21-25
To address this issue systematically, we studied length of stay and 30-day readmission rates with 14 cardiovascular and cancer procedures using the national Medicare database. In earlier work, we used this database to describe relationships between hospital volume and mortality.1 In this analysis, we used similar methods to determine whether hospital volume is related to 2 important components of hospital cost.
METHODS
Databases
Utilizing data from the Medicare claims database, we used 100% national samples from the Health Care Financing Administration’s MEDPAR and denominator files for years 1994-1999. This file contains hospital discharge abstracts for acute care hospitalizations of all U.S. Medicare recipients under the hospital (Part A) insurance program. Only patients in fee-for-service arrangements are included in the MEDPAR file; thus, our sample excludes Medicare patients enrolled in risk-bearing health maintenance organizations (less than 10%) during this time period. We excluded patients under age 65 or over age 99.
Patients and Procedures
Admissions for each of the 6 cardiovascular and 8 major cancer procedures in our analysis were identified using appropriate procedure codes from the International Classification of Diseases, version 9 (ICD-9).27 Patients undergoing abdominal aortic aneurysm (AAA) repair were excluded if their discharge abstracts contained diagnosis or procedure codes suggesting aneurysm rupture and/or thoracoabdominal aneurysms. We also excluded patients with end-stage renal disease (determined from the denominator file) from our lower extremity bypass cohort, to reduce potential contamination with upper extremity shunts and bypass procedures performed for dialysis access (ICD-9 codes do not distinguish upper from lower extremity bypass). We excluded from our coronary artery bypass grafting cohort patients undergoing simultaneous valve replacement. Finally, for the 8 major cancer resections, our cohort was restricted to patients who also had a diagnosis code for the malignancy associated with the operation (eg, patients undergoing colectomy were also required to have a diagnosis code for colon cancer).
Outcome Measures
Our primary outcome measures were postoperative length of stay and 30-day readmission rate. Length of stay was defined as the period from the index procedure to hospital discharge for the index admission. Readmission to any hospital within 30 days of discharge after the index procedure was designated as a 30-day readmission.
Hospital Volume
Methods for establishing volume categories have been described in detail elsewhere.1 In brief, volume was measured at the hospital level, expressed as the average numbers of procedures per year. Although volume was evaluated as a continuous variable, for presentation purposes we also created categorical variables. For each procedure, the hospitals were ranked in order of increasing total hospital volume, and then 5 volume groups were defined by the selections of whole number cutoff points for annual volume that most closely sorted the patients into 5 groups of equal size (quintiles). To reflect most accurately the overall institutional experience with each type of operation, we combined the replacement of aortic and mitral valves into the single category of heart-valve replacement and lobectomy and pneumonectomy into the category of lung resection in determining hospital volume. However, length of stay and readmission rates for these procedures were assessed separately.
We used linear regression to examine the relationship between hospital volume and length of stay (a continuous variable) and logistic regression to examine hospital volume and readmission rate (a binary variable). In preliminary analysis, we noted that patients with very long lengths of stay substantially skewed the distribution of this variable, thus violating the normality assumption of our regression model. For this reason, we performed logarithmic transformation of this variable in our analysis.28 To account for potential confounding by patient characteristics, we used multiple logistic regression techniques to adjust for the following variables: age, gender, race (black or nonblack), comorbidities (as defined by Charlson score,29,30) admission acuity (elective, urgent, or emergency), and mean Social Security income. However, because our results were only negligibly affected by adjustment, we present only observed length of stay and readmission rates here. All tests of significance are at the P < 0.05 level, and all P values are two-tailed. The institutional review board at Dartmouth Medical School approved our study protocol.
RESULTS
Patient Characteristics
During the study period of 1994-1999, approximately 2.5 million Medicare patients underwent 1 of the 14 high-risk surgical procedures. As described in our previous report,1 patient age and sex did not differ consistently across hospital volume strata. For most procedures, black patients were more likely to undergo surgery at lower-volume hospitals, but Charlson comorbidity scores tended to be slightly higher at high-volume hospitals. Patients at low-volume hospitals, particularly those undergoing cancer resections, were more likely to be admitted nonelectively.
Length of Stay
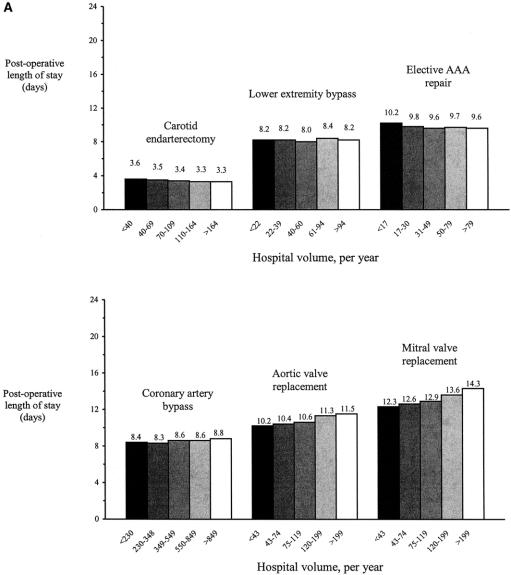
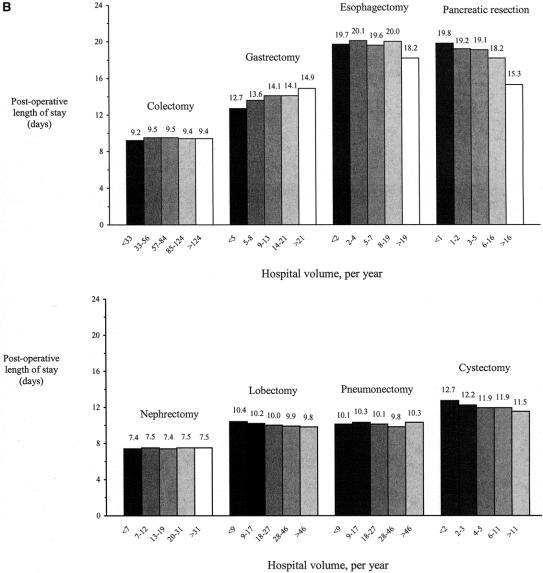
Postoperative length of stay varied widely across procedures (Fig. 1a and b). Mean length of stay was shortest in carotid endarterectomy (3.4 days), and longest for esophagectomy (19.6 days). In general, patients undergoing cancer resections had longer mean lengths of stay than those undergoing cardiovascular procedures. Several cancer resections were associated with mean lengths of stay in excess of 10 days (cystectomy, gastrectomy, esophagectomy, and pancreatic resection).
FIGURE 1. (a) Mean postoperative length of stay for 6 cardiovascular procedures, based on data from the national Medicare population (1994–1999). P < 0.05 for all differences across volume strata. (b) Mean postoperative length of stay for 8 cancer resections, based on data from the national Medicare population (1994–1999). P < 0.05 for all differences across volume strata.
Because of very large sample sizes, there were statistically significant associations between volume and length of stay for all 14 procedures. However, there was no consistent direction for this effect. Mean postoperative length of stay increased across volume strata for 7 of the 14 procedures and decreased across volume strata for the other 7.
Volume was associated with meaningful differences in length of stay for only a limited number of procedures. The largest difference occurred in pancreatic resection; mean postoperative length of stay was 4.5 days shorter in very-high-volume hospitals (compared with very-low-volume hospitals). Mean postoperative length of stay at very-low-volume and very-high-volume hospitals differed by more than 1 day for 6 procedures. Of these, length of stay was shorter in high-volume hospitals for 3 procedures (pancreatic resection, esophagectomy, cystectomy), but longer in high-volume hospitals for 3 other procedures (aortic and mitral valve replacement, and gastrectomy). Differences in length of stay of less than 1 day were observed for the remaining 8 procedures.
30-Day Readmission Rate
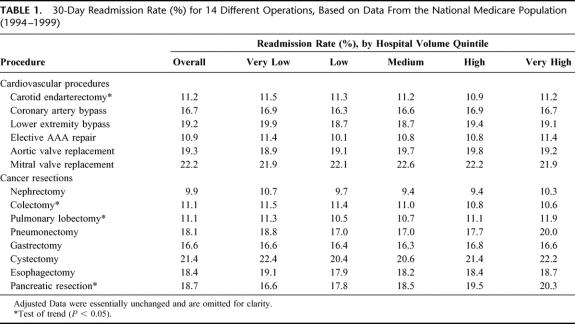
The 30-day readmission rate also varied widely across procedures (Table 1). The lowest readmission rate was 9.9% (nephrectomy), and the highest was 22.2% (mitral valve replacement). Statistically significant changes across volume strata were noted for only 4 of the 14 procedures. Readmission rates increased with volume for 2 procedures (pulmonary lobectomy and pancreatic resection) and decreased with volume for 2 procedures (carotid endarterectomy and colectomy). Although these differences were statistically significant, none were large enough to be considered clinically meaningful.
TABLE 1. 30-Day Readmission Rate (%) for 14 Different Operations, Based on Data From the National Medicare Population (1994–1999)
DISCUSSION
Using a large, national database, we examined the association between hospital volume and resource utilization by studying length of stay and 30-day readmission rate for 14 high-risk surgical procedures. Hospital volume was not consistently related to length of stay or 30-day readmission rates. Rather, the nature of the procedures themselves was a more important determinant of length of stay and 30-day readmission rate.
Although our study is the first to examine the association between readmission and volume, others have examined relationships between hospital volume and length of stay. In contrast to our findings, prior studies have reported shorter lengths of stay in higher volume hospitals.13,17,21,22,24,25 There may be several reasons for these differing conclusions. First, most of these studies were often limited to a single state or region. Since practice varies widely, their findings may not be generalizable to other parts of the country. Second, many of the prior studies were performed using data from more than a decade ago. Because length of stay has decreased over time for most procedures, volume may be a less important determinant of length of stay than it was 10 years ago. Lastly, publication bias may explain the lack of studies showing no association between volume and length of stay. It is well known that studies with negative results are less likely to be published.31-33
Our study has several limitations. First, because our study was limited to the Medicare population, our results may not be generalizable to patients less than 65 years of age. However, it is important to note that the Medicare population comprises approximately 60% of all patients undergoing these procedures.1 Second, we may not have fully accounted for differences in case-mix across volume strata, because the limits of administrative data for risk adjustment are well known.34-39 Thus, it may be possible that our study would have detected shorter length of stay at high-volume hospitals with better data for risk adjustment. However, this could only occur if patients in high-volume hospitals were systematically older and sicker, a premise not supported in the volume-outcome literature.4
Length of stay and 30-day readmission rates are imperfect proxies for hospital-based costs because they do not reflect intensity of hospital care. In other words, hospitals with similar lengths of stay may differ in how resources are used during hospitalization. Intensity of care is known to differ between teaching and nonteaching hospitals.40-46 In general, patients at teaching hospitals tend to receive more diagnostic tests and spend more time in the intensive care unit. However, it remains unknown whether similar differences in intensity of care are present between high-volume and low-volume hospitals.
A full accounting of the economic effects of volume-based referral initiatives would need to consider other potential costs.47 These include administrative costs associated with the referral process (eg, transfer of medical information). Another potential cost may be duplication of services, including specialist consultations and preoperative imaging.
A full accounting of resource use must also consider what happens to patients after discharge. In many of the procedures studied here, intermediate care facilities are used as a resource for nonacute care and rehabilitation, allowing a shorter length of stay during the “acute” hospitalization.48 How often these intermediate care facilities are used, across different procedures and volume categories, is unknown. It is also important to consider the use of home health services, which has also increased dramatically in recent years.49-51 At this time, however, it is not known whether use of home health services varies by hospital volume.
Lastly, it is important to consider how volume-based referral initiatives might affect the total number of procedures performed, at least for discretionary procedures. Emphasis on procedure volume as a quality indicator creates incentives for hospitals and surgeons to operate more often. Because of the subjective nature of clinical decision making for conditions such as lifestyle-limiting coronary disease, small aortic aneurysms, and asymptomatic carotid stenosis, the use of surgery could be increased without overtly “inappropriate” procedures.52,53 Also, geographic regions with the highest procedure rates tend to be dominated by high-volume surgeons, a phenomenon labeled the “enthusiasm hypothesis” by Chassin.54 Thus, efforts to concentrate care in high-volume centers might drive patients toward surgeons with lower thresholds to operate, further increasing the number of procedures performed.
Although not a true resource cost, policy makers must also consider the indirect effects of redistributing surgical revenue.47 Because surgery is a well-known profit center at most hospitals, loss of caseloads could threaten the viability of some low-volume hospitals. It could also adversely affect their ability to recruit and retain surgeons. These indirect effects could threaten patient access to basic surgical care. To avoid this problem, the Leapfrog group has exempted hospitals in rural areas from their evidence-based referral initiative. Advocates for other volume-based initiatives should take similar caution.
Clearly, a full accounting of the likely effects of volume-based referral initiatives on resource use is difficult given the data currently available. However, to the extent that length of stay and readmission rates reflect overall costs, volume-based referral initiatives seem more likely to decrease mortality than the cost of delivering high-risk surgery.
Footnotes
Reprints: Philip P. Goodney, MD, V.A. Outcomes Group (111B), Department of Veteran Affairs Medical Center, White River Junction, VT, 05009. E-mail: philip.goodney@hitchcock.org.
Supported by a grant from the Agency for Healthcare Research & Quality (R01 HS10141-01). Dr. Birkmeyer was also supported by a Career Development Award from the VA Health Services Research & Development program. The views expressed herein do not necessarily represent the views of the Department of Veterans Affairs or the United States Government.
REFERENCES
- 1.Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States: 1994-1999. N Engl J Med. 2002;346:1128–1137. [DOI] [PubMed] [Google Scholar]
- 2.Begg CB, Cramer LD, Hoskins WJ, et al. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280:1747–1751. [DOI] [PubMed] [Google Scholar]
- 3.Dudley RA, Johansen KL, Brand R, et al. Selective referral to high volume hospitals: estimating the potential impact on hospital mortality. JAMA. 2000;283:1159–1166. [DOI] [PubMed] [Google Scholar]
- 4.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002; 137(6):I52. [DOI] [PubMed]
- 5.Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001;130:415–422. [DOI] [PubMed] [Google Scholar]
- 6.Phillips KA, Luft HS. The policy implications of using hospital and physician volumes as “indicators” of quality of care in a changing health care environment. Int J Quality Health Care. 1997;9:341–348. [DOI] [PubMed] [Google Scholar]
- 7.Norton EC, Garfinkel SA, McQuay LJ, et al. The effect of hospital volume on the in-hospital complication rate in knee replacement patients. Health Serv Res. 1998;33(5 Pt 1):1191–1210. [PMC free article] [PubMed] [Google Scholar]
- 8.Glasgow RE, Mulvihill SJ. Hospital volume influences outcome in patients undergoing pancreatic resection for cancer. West J Med. 1996;165:294–300. [PMC free article] [PubMed] [Google Scholar]
- 9.Birkmeyer JD, Lucas FL, Wennberg DE. Potential benefits of regionalizing major surgery in Medicare patients. Eff Clin Prac. 1999;2:277–283. [PubMed] [Google Scholar]
- 10.Finkler SA. Cost effectiveness of regionalization-further results for heart surgery. Health Serv Res. 1981;16:325–333. [PMC free article] [PubMed] [Google Scholar]
- 11.Ellison LM, Heaney JA, Birkmeyer JD. The effect of hospital volume on mortality and resource use after radical prostatectomy. J Urol. 2000;163:867–869. [PubMed] [Google Scholar]
- 12.George EL, Large AA. Reducing length of stay in patients undergoing open heart surgery: the University of Pittsburgh experience. AACN Clin Issues. 1995;6:482–488. [DOI] [PubMed] [Google Scholar]
- 13.Gordon TA, Burleyson GP, Tielsch JM, et al. The effects of regionalization on cost and outcome for one general high-risk surgical procedure. Ann Surg. 1995;221:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harmon JW, Tang DG, Gordon TA, et al. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann Surg 1999;230:404–411; discussion 411-413. [DOI] [PMC free article] [PubMed]
- 15.Lavernia CJ, Guzman JF. Relationship of surgical volume to short-term mortality, morbidity, and hospital charges in arthroplasty. J Arthroplasty. 1995;10:133–140. [DOI] [PubMed] [Google Scholar]
- 16.Nallamothu BK, Saint S, Ramsey SD, et al. The role of hospital volume in coronary artery bypass grafting: is more always better? J Am Coll Cardiol. 2001;38:1923–19230. [DOI] [PubMed] [Google Scholar]
- 17.Perler BA, Dardik A, Burleyson GP, et al. Influence of age and hospital volume on the results of carotid endarterectomy: a statewide analysis of 9918 cases. J Vasc Surg 1998;27:25–31; discussion 31-33. [DOI] [PubMed]
- 18.Shahian DM, Heatley GJ, Westcott GA. Relationship of hospital size, case volume, and cost for coronary artery bypass surgery: analysis of 12, 774 patients operated on in Massachusetts during fiscal years 1995 and 1996. J Thorac Cardiovasc Surg. 2001;122:53–64. [DOI] [PubMed] [Google Scholar]
- 19.Urschel JD, Urschel DM. The hospital volume-outcome relationship in general thoracic surgery. Is the surgeon the critical determinant? J Cardiovasc Surg. 2000;41:153–155. [PubMed] [Google Scholar]
- 20.Wen SW, Simunovic M, Williams JI, et al. Hospital volume, calendar age, and short term outcomes in patients undergoing repair of abdominal aortic aneurysms: the Ontario experience, 1988-92. J Epidemiol Commun Health. 1996;50:207–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Swisher SG, Deford L, Merriman KW, et al. Effect of operative volume on morbidity, mortality, and hospital use after esophagectomy for cancer. J Thorac Cardiovasc Surg. 2000;119:1126–1132. [DOI] [PubMed] [Google Scholar]
- 22.Sosa JA, Bowman HM, Gordon TA, et al. Importance of hospital volume in the overall management of pancreatic cancer. Ann Surg. 1998;228:429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sosa JA, Bowman HM, Tielsch JM, et al. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228:320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gordon TA, Bowman HM, Bass EB, et al. Complex gastrointestinal surgery: impact of provider experience on clinical and economic outcomes. J Am Coll Surg. 1999;189:46–56. [DOI] [PubMed] [Google Scholar]
- 25.Balcom JH, Rattner DW, Warshaw AL, et al. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001;136:391–398. [DOI] [PubMed] [Google Scholar]
- 26.Finkler SA. The distinction between cost and charges. Ann Intern Med. 1982;96:102–109. [DOI] [PubMed] [Google Scholar]
- 27.The International Classification of Diseases, 9th revision, Clinical Modification: ICD-9. Washington, DC: Government Printing Office, 1998.
- 28.Hennekens CH, Buring JE. Epidemiology in Medicine. Toronto, Canada: Little, Brown, and Company, 1987.
- 29.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 30.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data:differing perspectives. J Clin Epidemiol 1993;46:1075–1079; discussion 1081-1090. [DOI] [PubMed]
- 31.Callaham ML, Wears RL, Weber EJ, et al. Positive-outcome bias and other limitations in the outcome of research abstracts submitted to a scientific meeting. JAMA. 1998;280:254–257. [DOI] [PubMed] [Google Scholar]
- 32.Begg CB, Berlin JA. Publication bias and dissemination of clinical research. J Natl Cancer Inst. 1989;81:107–115. [DOI] [PubMed] [Google Scholar]
- 33.Dickersin K, Chan S, Chalmers TC, et al. Publication bias and clinical trials. Control Clin Trails. 1987;8:343–353. [DOI] [PubMed] [Google Scholar]
- 34.Fisher ES, Whaley FS, Krushat WM, et al. The accuracy of Medicare’s hospital claims data: progress, but problems remain. Am J Public Health. 1992;82:243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fisher ES, Baron JA, Malenka DJ, et al. Overcoming potential pitfalls in the use of Medicare data for epidemiologic research. Am J Public Health. 1990;80:1487–1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iezzoni LI, Ash AS, Shwartz M, et al. Predicting who dies depends on how severity measured: Implications for evaluating patient outcomes. Ann Int Med. 1995;123:763–770. [DOI] [PubMed] [Google Scholar]
- 37.Iezzoni LI. The risks of risk adjustment. JAMA. 1997;278:1600–1607. [DOI] [PubMed] [Google Scholar]
- 38.Iezzoni LI. Risk adjustment and current health policy initiatives. Risk adjustment for measuring healthcare outcomes. Chicago: Health Administration Press, 1997.
- 39.Iezzoni LI, Foley SM, Daley J, et al. Comorbidities, complications, and coding bias. Does the number of diagnosis codes matter in predicting in-hospital mortality? JAMA. 1992;267:2238–2239. [DOI] [PubMed] [Google Scholar]
- 40.Taylor DH Jr, Whellan DJ, Sloan FA. Effects of admission to a teaching hospital on the cost and quality of care for Medicare beneficiaries. N Engl J Med. 1999;340:293–299. [DOI] [PubMed] [Google Scholar]
- 41.Rosenthal GE, Harper DL, Quinn LM, et al. Severity-adjusted mortality and length of stay in teaching and nonteaching hospitals. Results of a regional study. JAMA. 1997;278:485–490. [PubMed] [Google Scholar]
- 42.Keeler EB, Rubenstein LV, Kahn KL, et al. Hospital characteristics and quality of care. JAMA. 1992;268:1709–1714. [PubMed] [Google Scholar]
- 43.Iezzoni LI, Shwartz M, Moskowitz MA, et al. Illness severity and costs of admissions at teaching and nonteaching hospitals. JAMA. 1990;264:1426–1431. [PubMed] [Google Scholar]
- 44.Sloan FA, Feldman RD, Steinwald AB. Effects of teaching on hospital costs. J Health Economics. 1983;2:1–28. [DOI] [PubMed] [Google Scholar]
- 45.Sloan FA, Valvona J. Uncovering the high costs of teaching hospitals. Health Aff (Millwood). 1986;5:68–85. [DOI] [PubMed] [Google Scholar]
- 46.Josephson MA, Agger WA, Bennett CL, et al. Performance measurement in pneumonia care: beyond report cards. Mayo Clin Proc. 1998;73:5–9. [DOI] [PubMed] [Google Scholar]
- 47.Birkmeyer JD, Skinner JS, Wennberg DE. Will volume-based referral strategies reduce costs, or just save lives? Health Aff (Millwood) 2002; 21:234–241. [DOI] [PubMed]
- 48.Crouch DS, McLafferty RB, Karch LA, et al. A prospective study of discharge disposition after vascular surgery. J Vasc Surg. 2001;34:62–68. [DOI] [PubMed] [Google Scholar]
- 49.Cut inpatient utilization in half with proper use of home health services. Public Sector Contracting Rep. 1999;5:93-95. [PubMed]
- 50.Benjamin AE. State variations in home health expenditures and utilization under Medicare and Medicaid. Home Health Care Serv Q. 1986;7:5–28. [DOI] [PubMed] [Google Scholar]
- 51.Picone G, Wilson RM. Medicare home health agency utilization, 1984-1994. Inquiry. 1999;36:291–303. [PubMed] [Google Scholar]
- 52.Leape LL, Park RE, Solomon DH, et al. Does inappropriate use explain small-area variations in the use of health care services? [see comments.]. JAMA. 1990;263:669–672. [PubMed] [Google Scholar]
- 53.Leape LL, Park RE, Solomon DH, et al. Relation between surgeons’ practice volumes and geographic variation in the rate of carotid endarterectomy. N Engl J Med. 1989;321:653–657. [DOI] [PubMed] [Google Scholar]
- 54.Chassin MR. Explaining geographic variations. The enthusiasm hypothesis. Med Care. 1993;31(5 Suppl):YS37-44. [DOI] [PubMed]