Abstract
Objective:
The aim of the study was to compare the efficacy and mechanical consequences of 2 partial fundoplications performed laparoscopically under the framework of a randomized, controlled clinical trial.
Summary Background Data:
Although laparoscopic total fundoplication procedures have proven their effectiveness in the control of gastroesophageal reflux, problems remain with the functional consequences after a supra-competent gastric cardia high-pressure zone. Partial fundoplications have been found to be associated with fewer mechanical side effects.
Patients and Methods:
During a 2-year period, 95 patients with gastroesophageal reflux disease were enrolled into a randomized, controlled single-institution clinical trial comparing a partial posterior (Toupét, n = 48) fundoplication and an anterior partial wrap (Watson, n = 47). All patients were assessed postoperatively at predefined time points, and the 12-month follow-up data are presented in terms of clinical results and 24-hour pH monitoring variables.
Results:
Both patient groups were strictly comparable at the time of randomization. All operations were completed laparoscopically, and no serious complications were encountered. During the first postoperative year, a difference regarding the control of reflux symptoms was observed in favor of the posterior fundoplication. Esophageal acid exposure (% time pH <4) was substantially reduced by both operations but to a significantly lower level after a Toupét compared with the Watson partial fundoplication (1.0 ± 0.3 vs. 5.6 ± 1.1 mean ± SEM; p < 0.001). Postfundoplication symptoms were infrequently recorded with no difference between the groups.
Conclusions:
When performing a laparoscopic partial fundoplication, the posterior modification (Toupét) offers advantages in terms of better reflux control compared with an anterior type (Watson).
To evaluate the functional consequences of a laparoscopic anterior as compared to posterior partial fundolplication, 95 patients were prospectively evaluated pre- and postoperatively by symptom assessment and 24 pH-monitoring. At the one year follow up a significant difference with regard to the control of reflux symptoms and acid exposure was observed in favor of the posterior fundoplication (n = 48).
There has been increasing interest in the surgical management of gastroesophageal reflux disease, particularly after the introduction of minimal invasive techniques in 1991.1 To master the laparoscopic fundoplication technique, each surgeon has to “climb up” along a definitive learning curve that strongly endorses the significance of centralizing these procedures to high-volume, high-quality centers and also on the supervision of the surgical practice by an experienced surgeon.2,3 Despite these measures taken, some problems with failure and side effects of these operations remain. The most frequent postfundoplication symptoms are dysphagia, inability to belch and vomit, postprandial fullness, bloating and pain, and socially embarrassing rectal flatus.4,5 The frequencies by which these postfundoplication symptoms are reported vary considerably. A recent randomized clinical trial suggested that laparoscopic total fundoplications were associated with more obstructive complaints in the early postoperative period than after open procedures.6 However, other similar trials have not been able to confirm these potential hazards with the laparoscopic technique.7-11 At any rate, prevention is mandatory because we lack effective treatment of established severe postfundoplication symptoms. A large randomized trial with open antireflux surgery has reported that posterior partial fundoplications are associated with less troublesome complaints of gas–bloat/rectal flatus.12 In addition, a recent trial comparing a total with a partial anterior fundoplication performed laparoscopically suggested similar advantages with this partial fundoplication.13 It has been argued that some partial fundoplication procedures augment various constituents of the valvuloplasty components of the competence in the gastroesophageal junction and as a consequence were associated with a very low incidence of mechanical complications.14 To further optimize the design and function of antireflux surgery, the question then arises: Which type of partial fundoplication that maintains clinical efficacy in terms of reflux control with a concomitant minimization of post fundoplication complaints?
METHODS
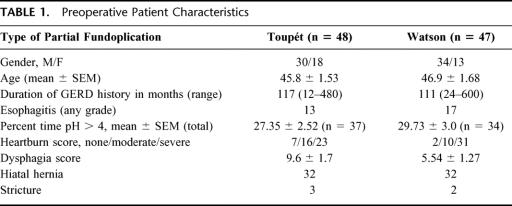
Ninety-five consecutive patients with chronic gastroesophageal reflux disease who were referred to our institution for antireflux surgery were enrolled into the trial. These patients had not previously had any major abdominal open surgical procedure. All patients underwent a complete preoperative evaluation, including esophageal manometry, 24-hour pH monitoring, endoscopy, and symptom assessment. At the time of endoscopy, many patients had, however, been treated with antisecretory drugs, which might jeopardize a valid assessment of the original severity of the esophagitis. Demographic data and reflux disease characteristics in the 2 study groups are presented in Table 1, demonstrating a similarity between the 2 study groups. The esophageal acid reflux was of the same magnitude in both study groups when studied preoperatively. Acid reflux variables were lacking in 13 Watson and 11 Toupét patients because of technical failures and missing values.
TABLE 1. Preoperative Patient Characteristics
Laparoscopic fundoplications were performed using standard operative techniques. The procedure began with dissection of the hiatal pillars followed by full esophageal mobilization, and a posterior crural repair was always performed by the use of nonabsorbable sutures. The proximal part of the gastric fundus was dissected, and the short gastric vessels were divided by the use of an ultrasound scalpel (Ultra Cision, Ethicon Endo-Surgery, Cincinnati, OH). The division began at the level of the hilus of the spleen, and in patients randomized to a Toupét fundoplication,15 the fundus was wrapped behind the esophagus to encircle 180-200° of the esophageal circumference and the proximal sutures on each side also fixed the fundus to the crura and the lateral margins of the esophagus. The right suture row was then continued distally with 2-3 stitches between the fundus and the right margin of the esophageal wall. The right posterior part of the fundoplication was fixed to the right crus with 2-3 separate nonabsorbable sutures. The left part of the fundoplication was fixed to the left crus by at the most 2 sutures, where after the left posterior part of the fundoplication was fixed in the same manner as the right side, making the length of the fundus cuff 2-3 cm.
In patients randomized to an anterior fundoplication according to Watson,16,17 the distal esophagus was mobilized to enable reduction of the hiatal hernia and allow a mobilization of 4-6 cm of the intraabdominal esophagus. The intraabdominal segment was then retracted anteriorly. The crural sling was repaired with interrupted, unabsorbable sutures placed posterior to the esophagus. The intraabdominal segment of the esophagus was fixed to the crural repair by suturing the posterior lateral aspect of the muscular layer of esophagus to the crural sling repair, avoiding the retracted posterior vagus nerve. The angle of His was reconstituted by placing interrupted unabsorbable sutures between the seromuscular layer of the superomedial aspect of the fundus of the stomach and the inferior surface of the diaphragm. A 120° anterior lateral fundoplication was thus performed between the medial aspect of the gastric fundus and the anterior aspect of the muscle layer of the esophagus, taking care to avoid branches of the anterior vagus nerve.
All operations were performed or supervised by a well-trained surgeon familiar with a variety of different fundoplication procedures. Before embarking on the current trial, a pilot series of cases with the anterior partial fundoplication (Watson) was completed to ensure a high-quality technical performance.
Clinical Assessment
Each patient was interviewed preoperatively and then at regular intervals during the first 12 months after the operations. Gastroesophageal reflux symptoms as well as those specifically related to the postfundoplication procedure were recorded. At each assessment, the patients were evaluated by an independent observer. Unless otherwise stated, each symptom was scored from 1 to 3 (1, no symptoms; 2, mild-to-moderate symptoms; 3, severe symptoms). Dysphagia was scored by several methods. One used a visual analogue scale (0-45; 0 = no dysphagia to 45 = total dysphagia) that was independently applied for solids and liquids and also a previously validated dysphagia score.18 This composite score combines information about difficulties in swallowing 9 types of liquids and solids. Endoscopic investigation of the esophagus and the upper gastrointestinal tract was performed preoperatively and postoperatively only at the discretion of the investigator.
Manometry was performed before the operation and at 6 months postoperatively. The pressure characteristics of the gastroesophageal junction were assessed by a water-perfused multiple lumen pressure catheter to which was connected a sleeve sensor straddling the gastroesophageal junction. The catheter was connected to a transducer assembly placed at the esophageal level of the subject in the supine position. Each channel was perfused with 0.5 mL of water per minute via a low-compliance capillary system (Arndorfer Medical Specialities, Greendale, WI). The probe was introduced through the nose in subjects being fasted overnight. Ambulatory 24-hour pH monitoring was performed before the operation and at 6 months after the operation. A monocrystalline antimony pH electrode was passed through and secured to the nose with the electrode placed 5 cm above the high-pressure zone, as located by the manometric examination. A reference electrode was attached to the skin of the chest. The patients were ambulatory throughout all recordings and were instructed to follow their usual pattern of living. Reflux symptoms, meals, including drinking or smoking, and resting periods were recorded in a diary by the patients. The pH data and information given in the diary were evaluated manually as well as by computer (Metronics, Stockholm, Sweden).
Statistics and Ethics
Informed consent was obtained from all patients participating in the study, and the study protocol was approved by the Ethic Committee of the Medical Faculty, University of Gothenburg. Data are given as either medians or mean values (± SEM) depending on a normal distribution was verified or not. Statistical evaluation was obtained by use of Fisher’s nonparametric permutation test for matched pairs. P < 0.05 was considered to be significant.
RESULTS
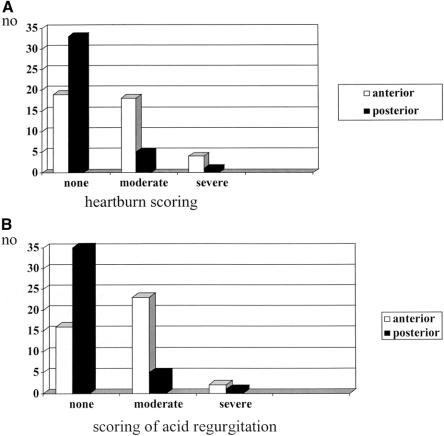
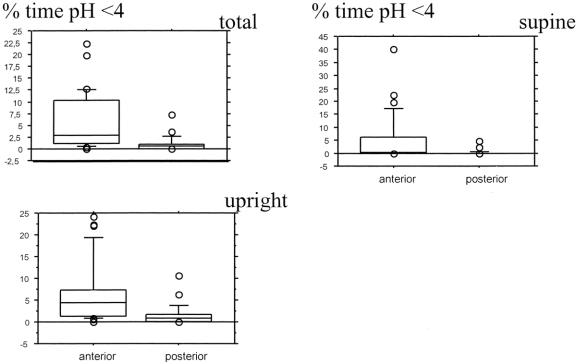
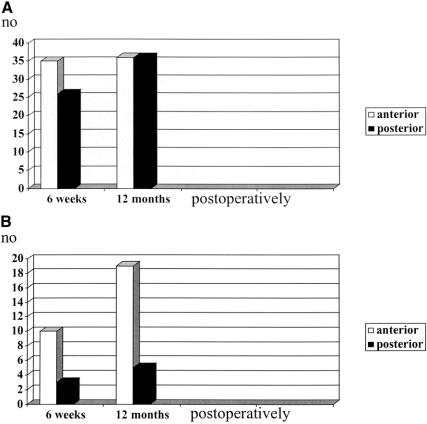
Both operations were effective in reducing reflux-associated symptoms, as illustrated in Figure 1a and b, but we observed a significant difference (P < 0.001) among the groups with fewer patients complaining of heartburn and acid regurgitation after a posterior partial fundoplication. Only 2% of patients receiving the Toupét procedure complained of remaining severe acid regurgitation. These differences in symptom control were paralleled by differences in 24-hour pH monitoring variables (Fig. 2). Although both operations reduced acid exposure, normal levels were reached only in the Toupét group (P < 0.001). From the same figure, it also can be deducted that the largest differences between the two procedures were observed during daytime recordings.
FIGURE 1. Scores for heartburn (a) and acid regurgitation (b) 12 months after an anterior or a posterior partial fundoplication.
FIGURE 2. Ambulatory 24-hour pH monitoring 6 months after either an anterior (Watson) or a posterior (Toupét) partial fundoplication. The box plot incorporates median values, 75 and 95% interquartile ranges. Data were acquired from 27 patients receiving the Watson procedure and 26 patients receiving the Toupét procedure.
We encountered difficulties in the acceptance rates for the postoperative 24-hour pH-monitoring (27 Watson vs. 26 Toupét), which might reflect the reluctance to perform a test in a patient without symptoms. To evaluate whether the anterior fundoplication was better in patients with less score reflux, we separated the material into 2 groups, ie, those with percentage time esophageal pH <4 more or less than 10% at the preoperative setting. By doing this, we found that the Toupét procedure was followed by the same low acid reflux values at 6 months after the operation: 0.4 ± 0.1 (n = 11) and 0.9 ± 0.3 (n = 15), respectively. In the anterior partial fundoplication group, the corresponding figures were 8.6 ± 2.6 (n = 9) and 2.7 ± 0.7 (n = 18). Thus, a statistical significance remained between the 2 procedures (P = 0.009, P = 0.019) irrespective of the magnitude of the preoperative acid reflux variables.
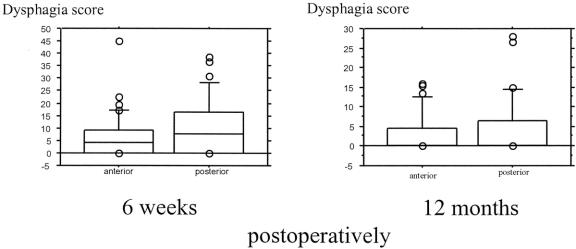
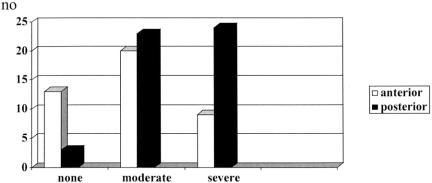
In terms of postfundoplication complaints, we observed no differences between the 2 procedures when patients with any level of obstruction was considered, as indicated by the composite score for dysphagia (Fig. 3). As expected, we found an improvement in dysphagia scores from 6 weeks to 12 months postoperatively. We recorded no difference between the 2 study groups regarding self-reported ability to belch, whereas more patients reported an ability to vomit after the anterior partial fundoplication (Fig. 4a and b). The patients general dyspeptic symptomatology did not change from the pre- to the postoperative situation, but some patients complained of rectal flatus, as seen in Figure 5. It can be noted that more patients in the posterior fundoplication group suffered from socially embarrassing rectal flatus (P < 0.02).
FIGURE 3. Box plot incorporating dysphagia composite scoring at 6 weeks and 12 months after an anterior an a posterior partial fundoplication.
FIGURE 4. Ability to belch (a) and vomit (b) (yes or no) after either an anterior or a posterior laparoscopic partial fundoplication.
FIGURE 5. Postfundoplication complaints of rectal flatus at 12 months after an anterior or a posterior partial fundoplication.
DISCUSSION
Laparoscopic antireflux surgery is not without complications, and the management of these may negate the proposed cost benefit for surgery over long-term medical therapy.19-22 This is of importance because the perception that laparoscopic antireflux surgery has its obvious advantages is ultimately dependent on the surgical community being able to achieve consistently excellent results after fundoplication with a low incidence of side effects. One of the most troublesome complication is persistent dysphagia. Some patients experience preoperative dysphagia, which is fairly common early postoperative complaint, whereas persistent difficulties affect only 5-10% of the patients.22 Patients and referring physicians may consider the risk of adverse outcomes, such as persistent dysphagia and gas-related symptoms, of special importance when deciding whether surgery is an appropriate treatment option or not. These problems have led to the investigation of a range of modifications of Nissen’s original procedure, which seek to improve outcome in patients after antireflux surgery.
Division of the short gastric vessels have failed to improve the overall outcome for patients undergoing a total fundoplication.13,23,24 For a long time, the use of a large bougie in the esophagus has been advocated to avoid the construction of a too-tight total wrap. Objective data have now been attained to support the use of a similar indwelling device to reduce obstructive side effects.25 Recently, the results of a trial comparing a laparoscopic anterior partial fundoplication with a Nissen total fundoplication showed a reduced incidence of dysphagia and gas-related problems in the former group13 yet equivalent control of reflux in both at 6 months follow-up. A subsequent longer follow-up of patients having a similar anterior partial fundoplication suggested reassuring outcomes.26 Findings from such a controlled trial would thus support the conclusions drawn from an uncontrolled, single-institution trial evaluating an open approach to the anterior partial repair.27 We have recently reported the long term (median follow-up of 12 years) of an open trial comparing a posterior partial with a total fundoplication showing equal levels of reflux control in the 2 groups but with a maintained difference in favor of the partial fundoplication with less gas–bloat/flatus complaints.28 The debate, however, continues whether some of the mechanical side effects of a total fundoplication can be avoided by doing a partial fundoplication without jeopardizing the efficacy by which reflux is controlled.29-31 In our patients having a laparoscopic partial posterior fundoplication, we found a normalization of acid reflux also in the subgroup of patients alleged to have severe reflux (>10% of time with pH <4).
The present randomized, controlled clinical trial addressed the question of whether there are important differences between the anterior and the posterior partial fundoplication in terms of reflux control and side effects. The trial incorporated 95 GERD patients, but the follow-up was limited to only 12 months. We found significant differences in favor of the posterior fundoplication regarding the level of reflux control. In fact, when daytime acid exposure was objectively assessed, the outcome after the laparoscopic anterior partial fundoplication was found to be poor. We were unable to demonstrate any differences in obstructive complaints between the 2 partial fundoplications, but interestingly enough, significantly more patients reported an ability to vomit after the anterior fundoplication. This observation probably reflects the efficacy of the respective repair. Of some interest is that somewhat more patients reported flatus complaints in the Toupét group. Flatulence is associated with, if not merely caused, by the ability to vent air from the stomach in the postoperative situation.32-34 It seems as if it is difficult to maintain an intact, normal ability to vent air from the stomach without efficacy with the assurance of reflux control.
Why should an anterior partial fundoplication function differently from a posterior one? The extent of the esophageal circumference that is encircled by the actual wrap varied somewhat between our study groups. Therefore, it can be argued that the buttressing effect of respective wrap might differ. The posterior fundoplication elevates the abdominal portion of the esophagus from its native bed in the hiatus and by necessity angulates the gastroesophageal junction. The significance of this has to be clarified but, if anything, this angulation might have the potential to cause some esophageal outflow obstruction. This we could not verify when quite-sophisticated questionnaires were used to assess eventual obstructive symptoms.
Are there other explanatory factors behind the discrepancies found in our short-term postoperative observation period and that of other published short- and median long-term follow-up studies in patients having an anterior partial fundoplications? The anterior partial fundoplication, performed and recently validated by Watson and coworkers,13,35 differed somewhat from that originally described16 and presently applied. There might, however, be some differences in outcomes when specific procedures are performed laparoscopically. Some studies have presented data to suggest inferior results after a laparoscopic Toupét fundoplication31,36,37 as compared with what we have presently recorded and also previously described when using the open technique.12,38 In the present study, all operations where performed by/or supervised by an experienced surgeon to ensure optimal technical quality, and we consider ourselves to have reached a plateau on the learning curve for the respective procedures. Furthermore, we adhered strictly to the operative procedure previously described and published when performing both an open and a laparoscopic anterior partial fundoplications. The only technical difference that could be envisaged was that we the mobilized at the fundus by division of the short gastric vessels to the same extent in both study groups. This deviation from the original description was urged by other methodological reasons to allow us to do appropriate manometric and physiological observations during the subsequent postoperative follow-up period. However, it is hard to believe that this marginal modification should explain the inferiority of the laparoscopic anterior procedure.
CONCLUSION
A posterior partial fundoplication (Toupét) performed laparoscopically was followed by adequate reflux control assessed both objectively and subjectively but an anterior partial fundoplication gave unacceptable results both in terms of reflux control and esophageal acid reflux variables.
Footnotes
Reprints: Cecilia Hagedorn, Department of Surgery, Sahlgrenska University Hospital, S-413 45 Gothenburg, Sweden. E-mail: cecilia.hagedorn@vgregion.se.
REFERENCES
- 1.Dallemagne B, Weerts JM, Jehaes C, et al. Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc. 1991;1:138–143. [PubMed] [Google Scholar]
- 2.Watson DI, Jamieson GG, Baigrie RJ, et al. Laparoscopic surgery for gastro-oesophageal reflux: beyond the learning curve. Br J Surg. 1996;223:1284–1287. [PubMed] [Google Scholar]
- 3.Watson DI, Jamieson GG. Antireflux surgery in the laparoscopic era. Br J Surg. 1998;85:1173–1184. [DOI] [PubMed] [Google Scholar]
- 4.Lundell L, Miettinen P, Myrvold HE, et al. Continued (5 year) follow up of a randomised clinical study comparing antireflux surgery and omeprazole in gastroesophageal reflux disease. J Am Coll Surg. 2001;192:172–179. [DOI] [PubMed] [Google Scholar]
- 5.Hinder A, Smith SL, Klinger PJ, et al. Laparoscopic antireflux surgery—it’s a wrap. Dig Surg. 1999;16:7–11. [DOI] [PubMed] [Google Scholar]
- 6.Bais JE, Bartelsman JF, Bonjer HJ, et al. Laparoscopic or conventional Nissen fundoplication for gastro-oesophageal reflux disease: randomised clinical trial. Lancet. 2000;355:170–174. [DOI] [PubMed] [Google Scholar]
- 7.Franzen T, Anderberg B, Tibbling L, et al. A report from a randomized study of open vs laparoscopic 360° fundoplication [abstract]. Surg Endosc. 1996;10;582. [Google Scholar]
- 8.Heikkinen TJ, Haukipuro K, Koivukangas P, et al. Comparison of costs between laparoscopic and open Nissen fundoplication: a prospective randomized study with a 3-month follow up. J Am Coll Surg. 1999;188:368–376. [DOI] [PubMed] [Google Scholar]
- 9.Laine S, Rantala A, Gullichsen R, et al. Laparoscopic vs conventional Nissen fundoplication. A prospective randomized study. Surg Endoscopic. 1997;11:441–444. [DOI] [PubMed] [Google Scholar]
- 10.Nilsson G, Larsson S, Johnsson F. Randomized clinical trial of laparoscopic versus open fundoplication: blind evaluation of recovery and discharge period. Br J Surg. 2000;87:873–878. [DOI] [PubMed] [Google Scholar]
- 11.Watson DI, Gourlay R, Globe J, et al. Prospective randomised trial of laparoscopic (LNF) versus open (ONF) Nissen fundoplication [abstract]. Gut. 1994;35(suppl 2):S15.7911442 [Google Scholar]
- 12.Lundell L, Abrahamsson H, Ruth M, et al. Long term results of a prospective randomized comparison of total fundic wrap (Nissen-Rossetti) or semifundoplication (Toupet) for gastro-oesophageal reflux. Br J Surg. 1996;83:830–835. [DOI] [PubMed] [Google Scholar]
- 13.Watson DI, Jamieson GG, Pike GK, et al. Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg. 1999;86:123–130. [DOI] [PubMed] [Google Scholar]
- 14.Watson A. Update: total versus partial laparoscopic fundoplication. Dig Surg. 1998;15:172–180. [DOI] [PubMed] [Google Scholar]
- 15.Toupét A. Technique d’oesophago-gastroplastie avec phreno-gastropexie appliquee dans la cure radicale des hernies hiatales et comme complement de l’operation d Heller dans les cardiospasmes. Mem Acad Chir. 1963;89:394–399. [Google Scholar]
- 16.Watson A, Jenkinson LR, Ball CS, et al. A more physiological alternative to total fundoplication for the surgical correction of resistant gastro-oesophageal reflux. Br J Surg. 1991;78:1088–1094. [DOI] [PubMed] [Google Scholar]
- 17.Watson A, Spychal RT, Brown MG, et al. Laparoscopic “physiological” antireflux procedure: Preliminary results of a prospective symptomatic and objective study. Br J Surg. 1995;82:651–656. [DOI] [PubMed] [Google Scholar]
- 18.Watson DI, Pike GK, Baigrie RJ, et al. Prospective double blind randomised trial of laparoscopic Nissen fundoplication with division and without division of short gastric vessels. Ann Surg. 1997;226:642–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeMeester TR, Stein HJ. Minimizing the side effects of antireflux surgery. World J Surg. 1992;16:335–336. [DOI] [PubMed] [Google Scholar]
- 20.de Beaux AC, Watson DI, O’Boyle C, et al. Role of fundoplication in patient symptomatology after laparoscopic antireflux surgery. Br J Surg. 2001;88:1117–1121. [DOI] [PubMed] [Google Scholar]
- 21.Perdikis G, Hinder RA, Lund RJ, et al. Laparoscopic Nissen fundoplication: where do we stand? Surg Laparosc Endosc Percutan Tech. 1997;7:17–21. [PubMed] [Google Scholar]
- 22.Wills VL, Hunt DR. Dysphagia after antireflux surgery. Br J Surg. 2002;88:486–499. [DOI] [PubMed] [Google Scholar]
- 23.Blomqvist A, Dalenbäck J, Hagedorn C, et al. Impact of complete gastric fundus mobilisation on outcome after laparoscopic total fundoplication. J Gastrointest Surg. 2000;4:493–500. [DOI] [PubMed] [Google Scholar]
- 24.Luostarinen ME, Isolauri JO. Randomized trial to study the effect of fundic mobilization on long term results of Nissen fundoplication. Br J Surg. 1999;86:614–618. [DOI] [PubMed] [Google Scholar]
- 25.Patterson EJ, Herron DM, Hansen PD, et al. Effect on an esophageal bougie on the incidence of dysphagia following Nissen fundoplication. Arch Surg. 2000;135:1055–1062. [DOI] [PubMed] [Google Scholar]
- 26.Watson DI, Liu J, Devitt PG, et al. Outcome of laparoscopic anterior 180° partial fundoplication for gastroesophageal reflux disease. J Gastrointest Surg. 2000;4:486–492. [DOI] [PubMed] [Google Scholar]
- 27.Cambell KL, Munro A. Efficacy and incidence of post-fundoplication symptoms at a median of 5 years following open Watson fundoplication. Br J Surg. 1998;85:(suppl 1):8. [Google Scholar]
- 28.Hagedorn C, Lönroth H, Rydberg L, et al. Long-term efficacy of a total (Nissen-Rosetti) and a posterior partial fundoplication (Toupét). Results of a randomised, clinical trial. J Gastroenterol Surg. In press. [DOI] [PubMed]
- 29.Franzen T, Boström J, Tibbling Grahn L, et al. Prospective study of symptoms and gastro-oesophageal reflux 10 years after posterior partial fundoplication. Br J Surg. 1999;86:56–60. [DOI] [PubMed] [Google Scholar]
- 30.Hunter JH, Trus TL, Branum GD, et al. A physiologic approach to laparoscopic fundoplication for gastroesophageal reflux disease. Ann Surg. 1996;223:673–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Horwath KD, Jobe BA, Herron DM, et al. Laparoscopic Toupét fundoplication is an inadequate procedure for patients with severe reflux disease. J Gastrointest Surg. 1999;3:583–591. [DOI] [PubMed] [Google Scholar]
- 32.Johnsson F, Holloway RH, Ireland AC, et al. Effect of fundoplication on transient lower oesophageal sphincter relaxation and gas reflux. Br J Surg. 1997;84:686–689. [PubMed] [Google Scholar]
- 33.Rydberg L, Ruth M, Lundell L. Mechanism of action of antireflux procedures. Br J Surg. 1999;86:405–410. [DOI] [PubMed] [Google Scholar]
- 34.Tew S, Ackroyd R, Jamieson GG, et al. Belching and bloating:facts and fantasy after antireflux surgery. Br J Surg. 2000;87:477–481. [DOI] [PubMed] [Google Scholar]
- 35.Watson DI, Mathew G, Pike GK, et al. Efficacy of anterior, posterior and total fundoplication in an experimental model. Br J Surg. 1998;85:1006–1009. [DOI] [PubMed] [Google Scholar]
- 36.Jobe BA, Wallace J, Hansen PD, et al. Evaluation of laparoscopic Toupét fundoplication as a primary repair for all patients with medically resistant gastroesophageal reflux. Surg Endosc. 1997;11:1080–1083. [DOI] [PubMed] [Google Scholar]
- 37.O’Reilly MJ, Mullins SG, Saye WB, et al. Laparoscopic posterior partial fundoplication: analysis of 100 consecutive cases. J Laparoendosc Surg. 1996;6:141–150. [DOI] [PubMed] [Google Scholar]
- 38.Laws HL, Clements RH, Swillie CM. A randomised, prospective comparison of the Nissen fundoplication versus the Toupet fundoplication for gastroesophageal reflux disease. Ann Surg. 1997;225:647–654. [DOI] [PMC free article] [PubMed] [Google Scholar]