Abstract
Objective:
To document functional results in patients treated with an ileal pouch anal anastomosis (IPAA).
Summary Background Data:
The restorative proctocolectomy with IPAA has become the procedure of choice for patients with ulcerative colitis, yet the long-term functional results are not well known.
Methods:
We performed this prospective observational study in 391 consecutive patients (56% male; mean age, 33.7 ± 10.8 years; range, 12-66 years) who underwent an IPAA between 1987 and 2002 (mean follow-up, 33.6 months; range, 0 to 180 months).
Results:
The majority of patients underwent the procedure under elective circumstances with a hand-sewn ileal pouch anal anastomosis and a protective ileostomy. In 25 patients (6.4%), the procedure was performed under urgent conditions; in 137 patients (35%), the temporary ileostomy was omitted; in 117 patients (29.9%), the ileal pouch anal anastomosis was stapled. There was 1 hospital mortality (0.25%) and 1 30-day mortality. Mean length of stay was 9.2 ± 5.6 days (3-68 days; median, 8 days) and was increased by the occurrence of septic complications (8.9 versus 13.6 days; P < 0.02) and by the omission of a temporary ileostomy (8.3 versus 10.4 days; P = 0.005). Complications included pelvic abscess (1.3%), anastomotic dehiscence (6.4%), bowel obstruction (11.7%), and anastomotic stenosis in need of mechanical dilatation (10.7%). Patients were asked to record their functional results on a questionnaire for 1 week at 3, 6, 9, 12, 18, and 24 months after the IPAA and yearly thereafter. Our data to 10 years show that median number of bowel movements (bms) was 6 bm/24 hours at all time intervals. The average number of bms increased by 0.3 bm/decade of life (P < 0.001). Throughout the entire follow-up, more than 75% of patients had at least 1 bm most nights, although fewer than 40% found it necessary to alter the time of their meals to avoid bms at inappropriate times. Depending on the time interval, between 57% and 78% of patients were always able to postpone a bm until convenient, and this ability was similar in patients with a stapled or hand-sewn ileoanal anastomosis; only up to 18% were able to always distinguish between flatus and stools, and this ability was similar in patients with a stapled or hand-sewn ileoanal anastomosis. Complete daytime and nighttime continence was achieved by 53-76% of patients depending on the time interval. The percentage of fully continent patients was higher following the stapled rather than the hand-sewn technique (P < 0.001), and this difference persisted over time. When patients experienced incontinence, its occurrence ameliorated over time (P < 0.001), and the occurrence of perianal rash and itching as well as the use of protective pads decreased over time (P < 0.008). At 5 years, patients judged quality of life as much better or better in 81.4% and overall satisfaction and overall adjustment as excellent or good in 96.3% and 97.5%, respectively.
Conclusions:
We conclude that the IPAA confers a good quality of life. The majority of patients are fully continent, have 6 bms/d on average, and can defer a bm until convenient. When present, incontinence improves over time.
The long-term functional results obtained with a restorative proctocolectomy with ileal pouch anal anastomosis show that this procedure confers a good quality of life to patients in need of surgical treatment for ulcerative colitis. The majority of patients are fully continent, have 6 bowel movements per day on average, and can defer a bowel movement until convenient. When present, incontinence improves over time.
The restorative proctocolectomy with ileal pouch anal anastomosis has become the procedure of choice for the surgical treatment of patients with ulcerative colitis. This procedure shares the goal of removing the affected colon and rectum with the traditional proctocolectomy and adds the additional goal of maintaining gastrointestinal continuity and transanal defecation.
Over the past 2 decades, several studies have looked at short-term and long-term functional results obtained with this procedure. Although many have concluded that the short-term functional results are very satisfactory and remain constant, others have suggested that functional results deteriorate over time.
The present study was conducted to evaluate long-term functional outcome in a large cohort of patients who underwent an IPAA for ulcerative or indeterminate colitis between August 1987 and May 2002. To avoid physician subjectivity and to minimize patient inaccuracies when evaluating functional outcome, the functional results were evaluated prospectively with a previously used and validated data collection questionnaire1 that enabled patients to record daily observations over 1 week at specific time points after reconstitution of the gastrointestinal continuity. This article details the results of this study.
MATERIALS AND METHODS
Patients and Operative Technique
Three hundred ninety-one consecutive patients who underwent an ileal pouch anal restorative proctocolectomy (IPAA) for ulcerative or indeterminate colitis were entered in a prospective database between August 1987 and May 2002. All IPAAs were performed by the 2 senior authors (FM and RDH). The majority of patients underwent the procedure under elective circumstances according to the technique previously described.1-2 Specifically, if a hand-sewn anastomosis had been selected, the anorectal mucosectomy was performed starting at the dentate line. The IPAA was then fashioned with 1 layer of interrupted 4-0 polyglactin 910 (Vicryl) stitches. If a stapled anastomosis had been selected, it was performed according to the double staple line technique after insertion of a 31-mm circular EEA through the anus. A protecting loop ileostomy was fashioned in the majority of patients, usually in the right lower quadrant, and was matured over a red rubber catheter as soon as the abdominal wall and skin incision had been closed. Perioperative data were accrued in a prospective database.
Questionnaire
The questionnaire consisted of 2 parts and was mailed to patients at 3, 6, 9, 12, 18, and 24 months after the surgical procedure and yearly thereafter. Part I consisted of a list of questions aimed at assessing the use of pharmacological aids and diet restrictions to reduce bowel movement (bm) frequency, and quality of continence (ability to distinguish flatus from stool and to defer a bm, use of protective pads, incidence of perineal rash, and pruritus). Part I also contained questions aimed at assessing patient’s quality of life. Part II consisted of 7 sheets to record oral intake, sleep pattern, bowel activity, and daily continence over 1 week. Following a detailed legend, patients were able to chart the consistency of each bm and grade the severity of eventual episodes of fecal incontinence over a 24-hour period (Fig. 1).
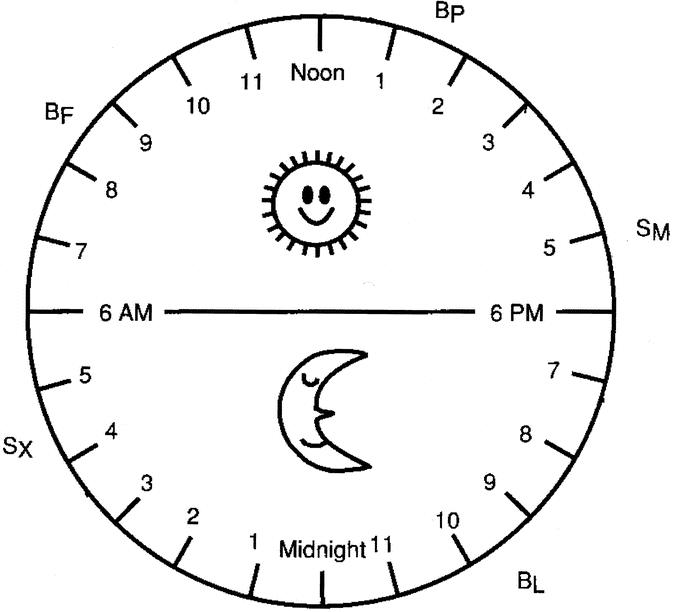
FIGURE 1. Representation of part II of questionnaire to assess bowel activity and continence over 1 week. A bowel movement (bm) was recorded as BL, BP, or BF (liquid, pasty, or formed, respectively); in the event of fecal leakage, a minor episode of leakage that could be cleaned with toilet paper or a tissue was recorded as SM, and loss of solid stool as SX.
Two to three weeks after receiving the questionnaire, patients came to our outpatient clinic, where the questionnaire was evaluated. Answers that appeared to be unclear or inconsistent with previous answers were clarified, although not changed; bowel activities and episodes of incontinence were averaged over 7 days and expressed with daytime, nighttime, and 24-hour mean values. Diet and medications were reviewed; suggestions were made to improve functional results. A complete physical examination was performed with particular attention given to a digital examination aimed at assessing the status of the IPAA, anal canal, pouch, and sphincter mechanism. This was complemented by a pouchoscopy if there was a suspicion of pouchitis. A rigid anoscopy with 4 quadrant biopsies of the anal transitional zone was performed annually in patients in whom the anastomosis had been fashioned according to the stapled technique. Data on occurrence of ileoanal stenosis in need of mechanical dilatation and conversion to Crohn disease were entered in each patient’s protocol.
Statistical Analysis
The study was approved by the Institutional Review Board of the Division of Biologic Sciences of the University of Chicago (Protocol #11767, approved on July 15, 2002). For the analysis of baseline and demographic variables, 2 sample t tests were used for comparison of continuous variables and Pearson χ2 test for categorical variables. Fisher exact test was used when only few observations were available. Multiple regression and multiple logistic regression models were fit to examine the relationship between operative technique and early outcomes, such as length of hospital stay, occurrence of anastomotic dehiscence, and stenosis. For the analysis of functional results at the prescribed time points since completion of the procedure, GEE (Generalized Estimating Equation) regression models were used.3 To assess changes over time, we used univariate and multivariate models. Measures with more than 2 categories on the questionnaire were dichotomized according to specified rules. For example, an indicator of continence function such as rectal itching, which had 4 categories (none = 0, occasionally = 1, sometimes = 2, and often = 3), was dichotomized into occurrence of rectal itching or not (≥1 versus 0). A logit link was employed in the GEE model to evaluate the odds of occurrence of rectal itching as a function of time and other predictor variables. Number of bms was treated as a continuous variable and an identity link was used to model the mean number of bms over time. Number of leakage episodes was treated as both a continuous variable and as a binary variable (incontinent versus continent).
RESULTS
In the 15-year period between August 1987 and May 2002, 391 consecutive patients (mean age, 33.7 ± 10.8 years; range, 12-66 years; 218 male patients) underwent an ileal J-pouch anal restorative proctocolectomy for a preoperative diagnosis of ulcerative colitis (n = 378) or indeterminate colitis (n = 13). The majority of patients underwent the procedure under elective circumstances with a hand-sewn ileal pouch anal anastomosis and a protective ileostomy; in 25 patients (6.4%) the procedure was performed under urgent conditions; in 117 patients (29.9%), the ileal pouch anal anastomosis was stapled; in 137 patients (35%), the temporary ileostomy was omitted (40.2% in the stapled group and 32.8% in the hand-sewn group). No temporary ileostomy was omitted prior to 1992 and no anastomosis was stapled prior to 1993. Between 33 and 455 days after pouch construction, patients with a temporary ileostomy underwent closure of the stoma (mean, 111 ± 61 days; median, 94 days). Closure of the temporary stoma was always preceded by a digital and radiographic examination of the ileoanal anastomosis and the pouch to assess patency and integrity.
There was 1 hospital mortality (0.25%) and 1 30-day mortality. Twenty-five patients (6.4%) experienced a postoperative anastomotic dehiscence, and 5 patients (1.3%) developed a postoperative pelvic abscess. Forty-three patients developed 1 or more episodes of small bowel obstruction: 23 patients (6%) developed a mechanical small bowel obstruction in the immediate postoperative period; 20 patients (5.2%) developed a mechanical small bowel obstruction after discharge from the hospital; 2 patients (0.5%) had an episode of mechanical obstruction during the immediate postoperative period and 1 episode prior to closure of the ileostomy. Forty-two patients (10.7%) developed an anastomotic stricture in need of at least 1 mechanical dilatation under anesthesia.
Mean postoperative hospital stay (± standard deviation) was 9.2 ± 5.6 days (3-68 days; median, 8 days). Length of stay was not influenced by whether the anastomosis was hand-sewn or stapled, but it was significantly affected by the occurrence of septic complications (8.9 ± 5.4 versus 13.6 ± 7.3 days; P < 0.02) and by the omission of a temporary ileostomy (8.4 ± 4.3 days versus 10.4 ± 6.9 days, respectively; P = 0.005). Even after adjusting for other covariates (age, gender, anastomotic technique), the omission of a temporary ileostomy had a significant effect on length of hospital stay; avoiding the temporary ileostomy, with all other things being equal, lengthened hospital stay by more than 2 days, and this difference was statistically significant (P = 0.002).
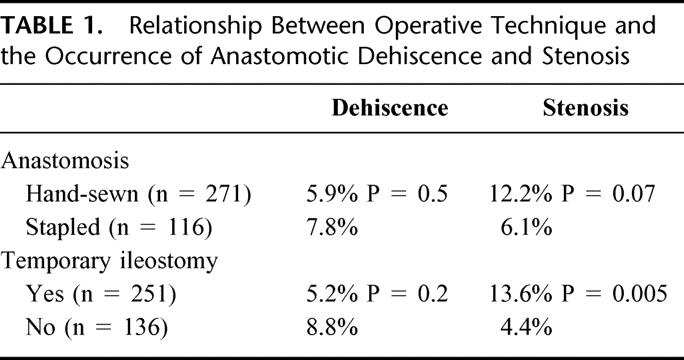
Table 1 correlates operative technique (hand-sewn versus stapled anastomosis or presence or omission of a temporary ileostomy) with the occurrence of anastomotic dehiscence and stenosis. The occurrence of an anastomotic dehiscence was similar whether the ileoanal anastomosis was hand-sewn or stapled (5.9% versus 7.8%, respectively; P = 0.5) or whether a temporary ileostomy was used or omitted (5.2% versus 8.8%, respectively; P = 0.2); yet the incidence of postoperative anastomotic stenosis was statistically significantly higher if a temporary ileostomy was used (13.6% versus 4.4%, respectively; P = 0.005). Twice as many patients with a hand-sewn anastomosis had a stenosis (12.2% versus 6.1%, respectively; P = 0.07), indicating a marginally significant association between the technique used and the development of an anastomotic stenosis. The results from multivariate logistic regression models suggest that the presence of a temporary ileostomy had a significant effect on the odds of developing an anastomotic stenosis (3.1 times the odds of a patient without a temporary ileostomy). Also, while not statistically significant, the odds of developing an anastomotic stenosis following a stapled technique are about 0.5 times that after a hand-sewn technique.
TABLE 1. Relationship Between Operative Technique and the Occurrence of Anastomotic Dehiscence and Stenosis
Long-term follow-up information is available on 353 of 391 patients (90.3%; mean, 37.2 months; median, 24 months; range, 0-180 months). It should be noted that 12 patients have had their pouch removed for various reasons (poor functional results, 4; Crohn disease, 3; chronic pouchitis, 5).
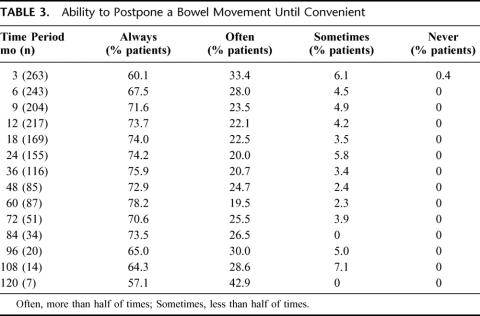
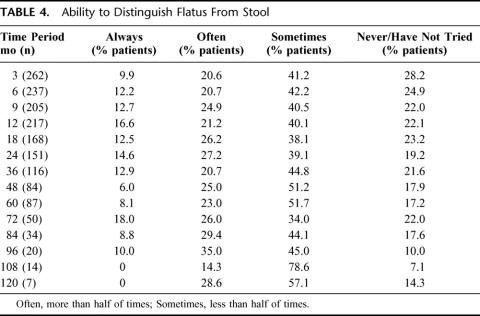
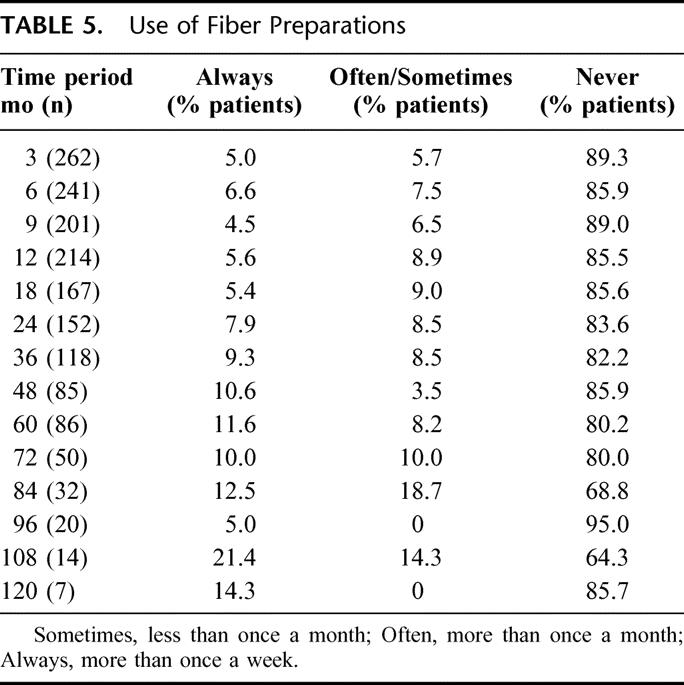
Frequency of bms at different intervals from reestablishment of gastrointestinal continuity is detailed in Figure 2. Median number of bms was 6 bms/24 hours at all time intervals. All patients defecated spontaneously. The average number of bms increased by 0.3 bm/decade of life (P < 0.001). Although the majority of patients had at least 1 bm most nights (Table 2), few took antimotility drugs to alter stool frequency (Fig. 3), and this use declined noticeably over time (P = 0.011). Table 2 also shows the percentage of patients who found it necessary to alter the time of their meals to avoid bms at inappropriate times (nighttime, commuting, social activities). The ability to defer a bm until convenient and to distinguish flatus from stool are quantitated in Tables 3 and 4. The former was similar in patients with a stapled or a hand-sewn ileoanal anastomosis. These characteristics did not change significantly over time. Consistency of bms remained stable at each time interval, with patients reporting that the majority of bms were pasty (between 40% and 56%) or formed (between 19% and 37%), although only a minority of patients took fiber preparations to affect stool consistency (Table 5).
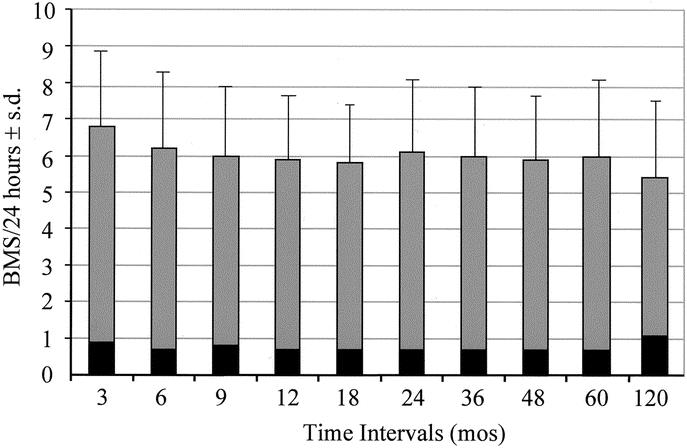
FIGURE 2. Frequency (mean ± SD) of bms per 24 hours. Black bars, nighttime; gray bars, daytime.
TABLE 2. Occurrence of Bowel Movement at Night and Need to Alter Time of Meals to Avoid Bowel Movements at Inappropriate Times
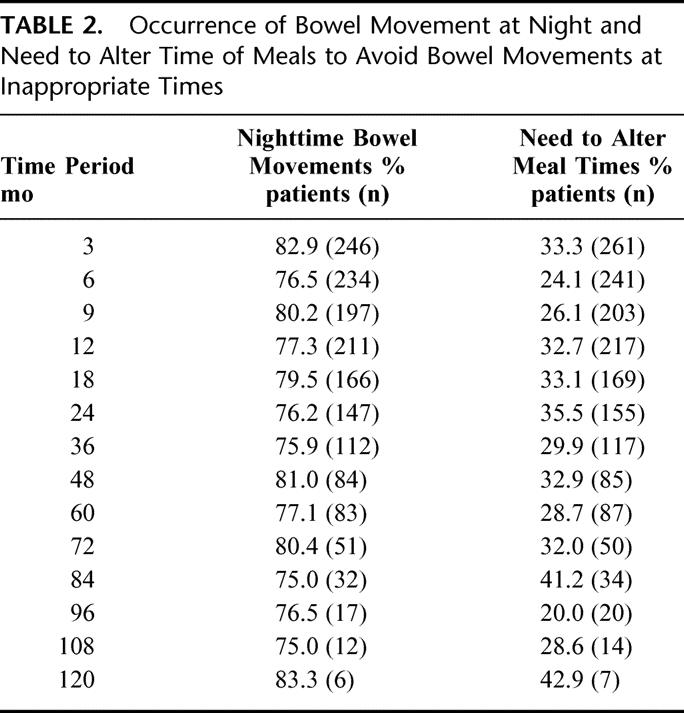
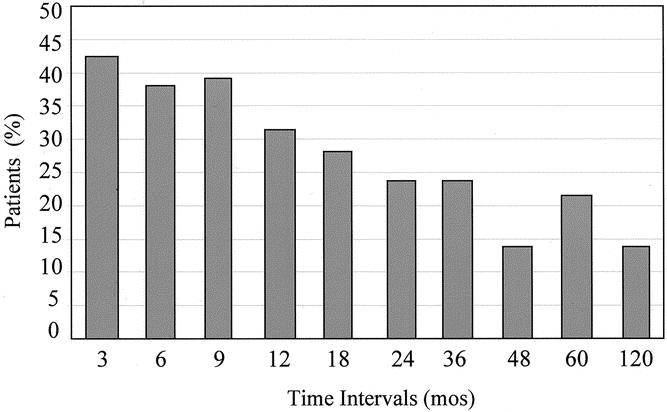
FIGURE 3. Percentage of patients using antimotility drugs to decrease the number of bms per 24 hours.
TABLE 3. Ability to Postpone a Bowel Movement Until Convenient
TABLE 4. Ability to Distinguish Flatus From Stool
TABLE 5. Use of Fiber Preparations
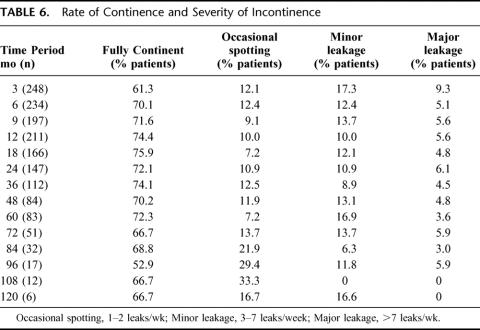
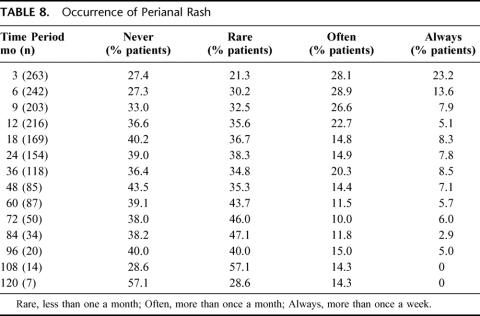
The rate of continence over time is listed in Table 6. The percentage of fully continent patients (Fig. 4) and the percentage of patients’ continent during daytime or nighttime (Table 7) were higher for the stapled rather than the hand-sewn technique (P < 0.001), and this difference persisted over time. An examination of trends over time suggests that when a patient is continent immediately after re-establishment of gastrointestinal continuity, continence will be maintained over time unless other factors such as pouchitis or strip anusitis occur. By the same token, when incontinence is experienced, its severity tends to ameliorate over time (P < 0.001), as suggested by the decrease in the percentage of patients with major leakage (Table 6), constant perianal rash (Table 8), or perianal irritation (Table 9), and use of daytime and nighttime protective pad (Fig. 5). Each 1 of these parameters declined noticeably over time (P < 0.01). It should be noticed that, depending on the time period, protective pads were used by up to 8.7% of the patients during the day and by up to 11.8% during the night in the absence of fecal incontinence (Fig. 5). Although there was no difference in the rate of male and female patients experiencing incontinence, the odds of ever using a protective pad were greater for female patients (odds ratio = 2.28; P < 0.001), and this relationship did not change over time. In general, the odds of ever using a protective pad did decline over time (P = 0.01).
TABLE 6. Rate of Continence and Severity of Incontinence
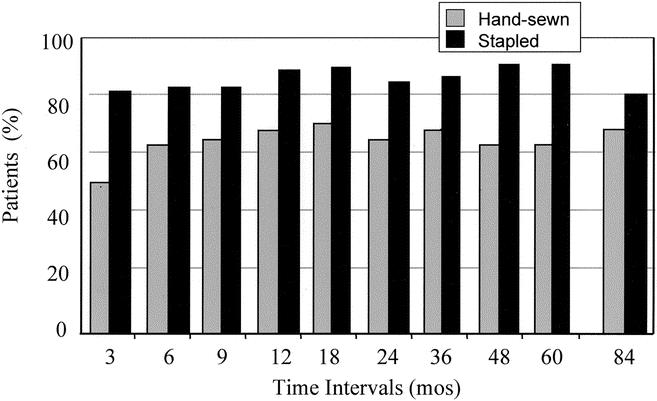
FIGURE 4. Percentage of patients experiencing full continence (daytime and nighttime) according to surgical technique.
TABLE 7. Daytime and Nighttime Continence Rate for Patients With Stapled (S) and Hand-Sewn (H) Anastomosis
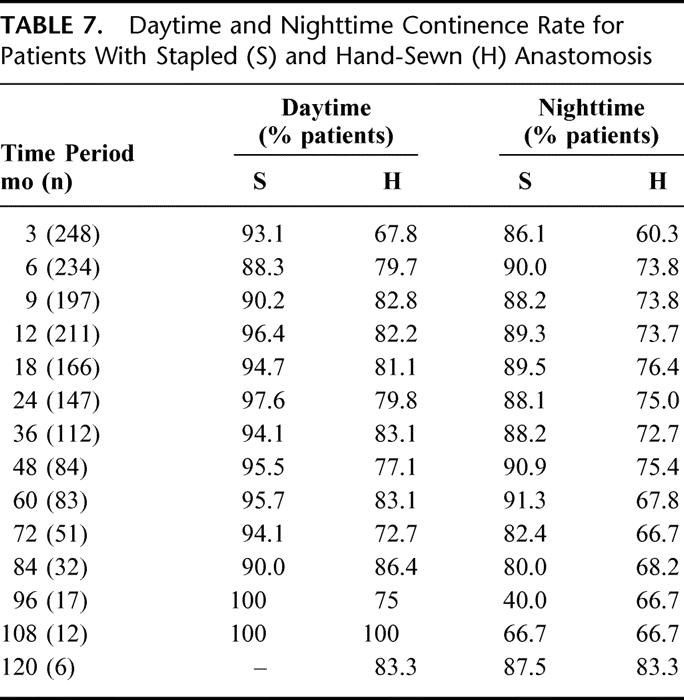
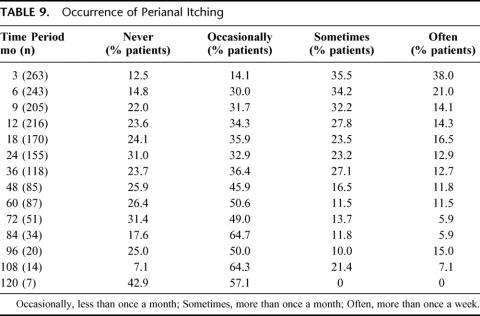
TABLE 8. Occurrence of Perianal Rash
TABLE 9. Occurrence of Perianal Itching
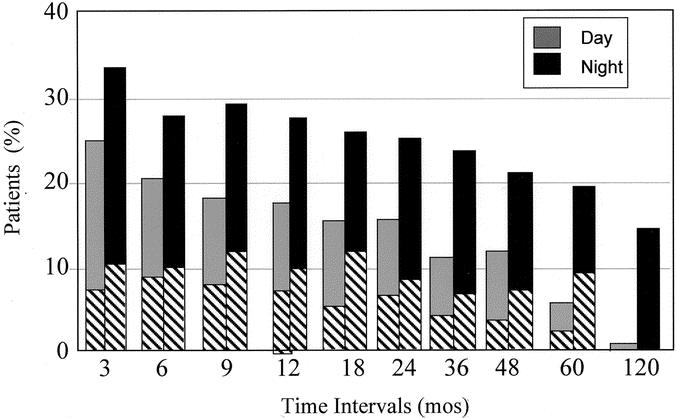
FIGURE 5. Daytime and nighttime protective pad usage. Bottom shaded bars indicate usage by continent patients.
Analysis of continence at 5 years shows that 72.3% of patients are fully continent during daytime and nighttime and that only 27.7% have some fecal incontinence (Table 6). The severity and the temporal occurrence of their incontinence at 60 months is depicted in Figure 6, where patients are divided into 3 groups according to the frequency of their incontinence: patients with 1-2 episodes of incontinence per week (occasional spotting, 7.2%), 3-7 per week (minor leakage, 16.9%), or more than 7 per week (major leakage, 3.6%). Within each bar, their incontinence is expressed according to the severity (minor stain versus loss of solid stool) and whether it occurred during the day or night. Eighty to eighty-five percent of all episodes of leakage in patients with occasional spotting or minor leakage occurred at night, and loss of solid stools occurred infrequently during the day only in the minor leakage group. Patients in the major leakage group had an almost equal number of episodes of incontinence during the day and night, and 11.4% of leakage episodes experienced in this group were loss of solid stool during the day. Protective pad usage for all patients with incontinence was 3.4% during daytime and 10.3% during nighttime. Analysis of severity of incontinence at 60 months according to surgical technique reveals that only 8.7% of patients with a stapled anastomosis were incontinent, with an equal proportion of patients in the minor (3-7 leaks/wk) and the major (>7 leaks/wk) incontinence group. By the same analysis, 35.6% of patients with a hand-sewn anastomosis experienced some incontinence: 10.2% in the occasional spotting group; 22% in the minor incontinence group; 3.4% in the major incontinence group.
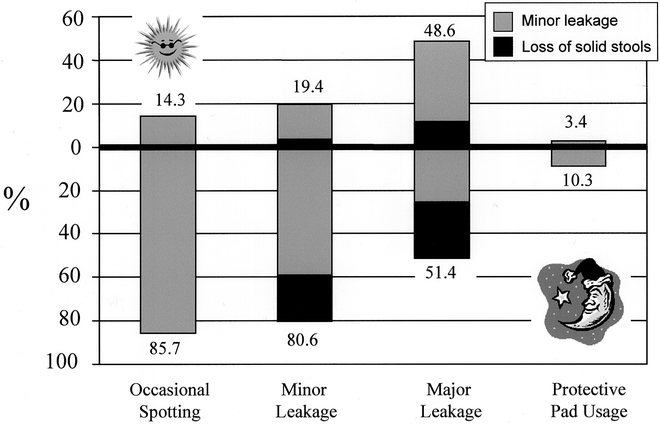
FIGURE 6. Degree of incontinence during the day and night for patients with occasional spotting (1-2 leaks/wk), minor leakage (3-7 leaks/wk), and major leakage (>7 leaks/wk). Top of figure above zero line indicate awake hours; bottom, sleeping hours. Within each bar, open area indicates percentage of episodes of minor leakage; solid area, percentage of episodes of loss of solid stool. Diurnal and nocturnal use of protective pads is tabulated by the bar on the right side of the graph.
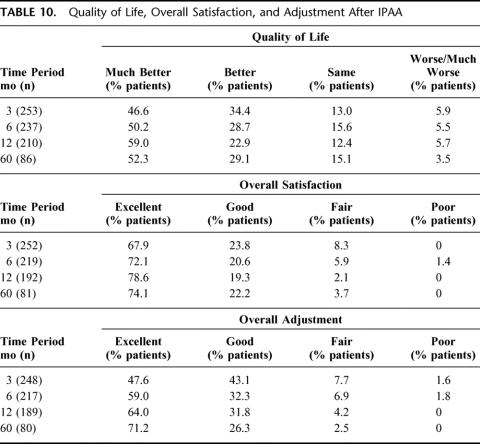
Patients’ subjective assessment of their quality of life showed overall satisfaction and adjustment with the lifestyle imposed by the procedure; at 5 years, patients judged quality of life as much better or better in 81.1% and overall satisfaction and adjustment as excellent or good in 96.3% and 97.5%, respectively (Table 10).
TABLE 10. Quality of Life, Overall Satisfaction, and Adjustment After IPAA
DISCUSSION
With this study, we describe the long-term functional results following a restorative proctocolectomy with J-pouch ileoanal anastomosis for ulcerative or indeterminate colitis. The data were obtained in a prospective fashion using patient-completed questionnaires and daily diaries. The questionnaire was designed to assess less frequently occurring adverse outcomes, such as perianal itching and rash, and the daily diary was designed to measure the timing and consistency of bms, as well as the occurrence, timing, and degree of incontinence. We used this previously validated tool in an effort to more systematically collect data that are accurate and free from recollection bias of the patient and subjective bias of the surgeon.
The restorative proctocolectomy with J-pouch ileoanal anastomosis is a safe procedure with minimal perioperative mortality and acceptable morbidity. As familiarity and experience with the performance of this operation has increased, the incidence of anastomotic dehiscence, pelvic sepsis, and small bowel obstruction have decreased. Interestingly, the occurrence of an anastomotic stricture was higher in patients in whom a temporary ileostomy was fashioned. Although tension on the ileoanal anastomosis might very well have been the reason for the temporary diversion and the cause of the anastomotic stricture, it is tempting to speculate that the lack of stool passage through the freshly fashioned anastomosis may have contributed to the occurrence of the stenosis.
Our data on frequency of bms show that stool frequency remain constant in the first decade after the surgical procedure. These data are in agreement with those reported by others. McIntyre et al4 noticed that median stool frequency was 7 in a 24-hour period at both 1 year and 10 years. Seven bms in 24 hours was also the mean value reported by Bullard et al5 over an 8-year span. Our patients’ mean stool frequency of 6 bms/24 hours at 1 and 10 years compares favorably with the 2 previous reports and confirms that number of bms per 24 hours remains stable over the first decade after the surgical procedure. It is interesting that these results were obtained despite the fact that the majority of patients were following no specific dietary restrictions and that the use of drugs to alter stool frequency decreased over time. This observation is in agreement with Bullard et al;5 in their experience, the percentage of patients using antidiarrheals decreased from 34% to 19% over the course of 8 years.
Complete fecal continence improved drastically in the first 12 months and remained stable in the first 5 years. Our rate of 70-75% of perfect continence is in agreement with the functional results reported by others.4 Most importantly, the ability to always postpone a bm until convenient increased during the first year from 60% to 74% and was 78% at 5 years. As the majority of patients failing medical treatment of ulcerative colitis suffer from urgency, the ability to postpone a bm until convenient is one of the most rewarding quality of life improvements that they experience. Although there was no element of randomization in this study with regard to surgical technique, and therefore, comparison of functional results in patients with a hand-sewn versus a stapled anastomosis may be confounded by other factors, it should be noticed that patients who underwent a stapled ileoanal anastomosis showed a statistically significantly higher rate of day-time and night-time and complete fecal continence in comparison to patients who underwent a hand-sewn anastomosis, an observation that is in complete agreement with others.6,7 On the other hand, there was no difference between the 2 techniques in terms of the ability to distinguish flatus from stools.
When incontinence was present, it improved over time. The improvement was most significant during the first 12-18 months, suggesting that it parallels the disappearance of the local response to the trauma of surgery on the anal sphincter and the patient’s adaptation to the procedure. Our prospective patient completed protocol allowed us to quantitate the increase in the number of daytime, nighttime, and fully continent patients and the decrease in the number of patients with major leakage, perineal rash and itching, and in the daytime and nighttime usage of protective pads.
Several authors have suggested that continence may worsen with longer follow-up from the procedure.5 We cannot substantiate this observation. Although our rate of fully continent patients decreased slightly after 5 years, the apparently worse functional outcome can be explained by the larger contribution of patients with hand-sewn anastomosis to the later time intervals.
In conclusion, the restorative proctocolectomy with ileoanal pouch anastomosis confers good long-term functional results to patients with ulcerative colitis in need of surgical treatment. After an initial period of adjustment lasting 12-18 months, bowel frequency stabilizes at 6 bms per day, with the majority of patients fully continent and able to postpone a bm until convenient. The stapled technique confers a higher rate of continence. Subjective assessment of quality of life, overall satisfaction, and adjustment are very high.
ACKNOWLEDGMENTS
The authors wish to thank Mr. Jon Mills and Mr. and Mrs. Jim Abrams for their generous contributions toward the study.
Discussions
Dr. John H. Pemberton (Rochester, Minnesota): Thank you for allowing me to discuss the paper and thank you, Dr. Michelassi, for sending me the manuscript in a timely fashion.
As you can all guess, after listening to this presentation and the previous 1 from the Cleveland Group, ileoanal anastomosis has become a very popular operation among patients requiring ileostomy for ulcerative colitis and familial polyposis. Although other less complex operations exist and some patients are not candidates for this procedure, ileoanal has become the procedure of choice at this time.
Our data set, Dr. Michelassi, nearly mimics yours identically. Among the 2,317 patients we have followed from 1981 until 2001, the mean follow-up has been 9 years and the longest just over 20. At 1 year, about 98% of our patients had a functioning pouch; at 5 years, 95%; at 10 years, 92%. Among the 409 patients followed as a cohort out to 15 years, that success rate is 91%. And of 44 patients followed 20-plus years, the success rate remains 90%. Thus the ileoanal operation appears to be indeed durable, 90% of patients having a functioning operation at the end of 20 years.
Dr. Michelassi’s data together with ours and those of the Cleveland Group all point to the same conclusion; namely, this operation has evolved and matured into a really good one, 1 which achieves its goals of eliminating disease and preserving fecal continence. To be sure, the operation is not perfect. The stool frequency reported here of about 6 during the day and 2 at night needs to be lower.
The incidence of pouchitis in our study population is fully 60% by 20 years. We still don’t understand the etiology of pouchitis but do know that only a very small fraction, less than 10% of that 60% that get pouchitis, have a chronic ongoing problem with it.
Complications with diverting ileostomies continue to occur and dishearteningly, patients originally diagnosed at the time of their ileoanal anastomosis as having ulcerative colitis continue to develop changes in the pouch and the anal canal which for all the world appear to be Crohn’s disease.
Fecal continence is imperfect as well. Dr. Michelassi interestingly observed that continence was significantly better in those patients who were stapled compared with those in whom a hand-sewn anastomosis was performed. We had looked at this question In a randomized study and were unable to find a difference, but I am heartened by Dr. Michelassi’s observations.
Pelvic sepsis, abdominal sepsis, stricture, fistula, all of these have not been eliminated even as our experience has grown. And of course some patients, because of their body habitus and their age, continue to not be candidates for the operation. Of interest, we have also noted that the mean age of our patients has increased from 31 to 36 years.
Dr. Michelassi, a couple of questions:
How can we improve the operation?
Should we do a one-stage procedure on nearly all of our patients thus eliminating the comorbidity of an ileostomy? What experience do you have with complications of the ileostomy? Should we only operate on younger patients and eliminate the problem of fecal incontinence in older patients? Should we staple all of our anastomoses? And should we, in an attempt to control the problem of pouchitis, treat our patients prophylactically with Flagyl or Cipro to minimize the occurrence of pouchitis over time?
With regards to indeterminate colitis, what is your definition of indeterminate colitis and do you offer your IC patients this operation?
What is the incidence of symptomatic anal transition zone inflammation in your pouch population what can we do to keep that minimized?
Although only 1 study in the literature has shown a problem with dysplasia occurring in the pouch after operation, do you look for this in your patients and how do you follow that?
Lastly, do you treat patients with ulcerative colitis and either colonic or rectal cancer differently?
Thanks to the Association for the privilege of discussing the paper and congratulations on a great presentation.
Dr. Fabrizio Michelassi (Chicago, Illinois): Thank you, Dr. Pemberton. Let me first thank you for your comprehensive discussion and also knowledge your contribution and the contribution of the Mayo Clinic to the surgical treatment of ulcerative colitis.
You asked how we can improve on the operation. There are 2 ways to do the anastomosis; 1 is with a hand-sewn technique after a full mucosectomy and the second 1 is with a stapled technique.
There is no question that the stapled anastomosis is technically easier and there are data, such as ours, suggesting that it may confer better function. The drawback of the procedure is that it leaves some native rectal transitional zone in place which is at risk for further complications such as dysplasia and cancer and possibly persistent inflammation.
A way to improve on the current surgical procedure could be to find a way that combines the ease of performance and the superiority of the functional results of the stapled technique with the completeness of the mucosectomy of the hand-sewn technique. Whether new instrumentation or new techniques could allow that, it is something to be assessed.
You asked to elaborate on the morbidity of the temporary ileostomy and whether we should migrate towards a one-stage procedure. There is no question that the temporary ileostomy confers morbidity, and, even in the absence of morbidity, it requires a second procedure for its closure with its attendant additional morbidity.
Yet, I don’t think that we should avoid the temporary ileostomy in all patients. In our experience, we have omitted the temporary ileostomy when the anastomosis appeared intact and under no tension, the procedure was not complicated by excessive bleeding or other technical difficulties, the terminal ileum was not affected by backwash ileitis and the patients were not on high dose of oral steroids prior to the surgery. I think that these are safe guidelines for placement of a temporary ileostomy which protects against the pelvic septic complications of an anastomotic dehiscence.
You asked whether we should have an age limit for patients to be candidates for this procedure. Our oldest patient in this study was 66 years. I think that we should select patients based on absence of comorbidities rather than chronological age.
Should we do a stapled anastomosis on all patients for better functional outcome? No, we don’t staple all anastomosis. We certainly do not staple patients with familial polyposis or patients with colorectal dysplasia or cancer. We also avoid stapling patients with severe disease at the ano-rectal transitional zone and with secondary manifestations of ulcerative colitis which may benefit from total removal of the diseased mucosa.
We have reported on the incidence of pouchitis in a previous study. In that study, 1 of 2 patients had at least 1 episode of acute pouchitis in the first 5 years from the procedure: 10% of these patients converted to chronic pouchitis as defined by continuous pouchitis or at least 6 episodes of recurrent acute pouchitis per year. Chronic pouchitis is difficult to treat: it requires antibiotic treatment, which is very effective in the acute episode but, at best, limits the adverse symptomatology in the chronic state.
Dr. David A. Rothenberger (Minneapolis, Minnesota): Just a quick question about the anal strictures you discussed. Are those short-term problems or long-term problems? During the interval of the time that the patient has a temporary ileostomy, are you digitalizing the anal anastomosis or do you just let it go until the takedown?
Thank you for providing me with your manuscript. I enjoyed the opportunity to review it.
Dr. Fabrizio Michelassi (Chicago, Illinois): Thank you, Dr. Rothenberger. Allow me first to acknowledge your contributions and the contributions of your group to this subject.
Strictures are usually a short-term problem because they can be dilated satisfactorily in the majority of cases, although patients may require up to 3 or 4 mechanical dilatations prior to having a stable nonstenotic anastomosis. In our practice, we digitalize patients with a temporary ileostomy within 6 weeks of the procedure, and if we find that there is a stricture we dilate that prior to doing a dynamic proctography and closing the temporary ileostomy.
My bias, although I do not have data, is that the strictures following a stapled anastomosis are more difficult to dilate permanently than the ones after a hand-sewn anastomosis.
Dr. Victor W. Fazio (Cleveland, Ohio): First of all, I want to thank Dr. Michelassi for letting me look at the manuscript and congratulate him on an excellent paper.
One of the issues about following up patients like this with questionnaires is the assurance of anonymity of the respondent to the surgeon involved. This at least has been 1 of the issues we have in our pouch database. And I wondered if you could comment on the compliance with the respondents as well as how they can be assured somewhat of an anonymity - they are not doing quite as well as what we would like to think they do.
The other question I have is, did you use a quality of life instrument? If so, what domains were examined in that? Different patients will put up with significant pleuritis, et cetera, but still rate their quality of life as being quite high, somewhat of a disconnect between our perceptions of surgeons and that of the patients themselves.
Finally, did you find that the pouch loss rate increased through time? We have found at the ten-year mark that seemed to cumulatively increase, although our individual rates of success, if you like, at 1 year and 2 years seemed to have dropped.
Thank you for allowing me to comment.
Dr. Fabrizio Michelassi (Chicago, Illinois): Thank you, Dr. Fazio. And again, let me acknowledge your contributions and the Cleveland Clinic contributions to this procedure.
We have removed 12 pouches over the course of 15 years: 5 of them for poor function, 3 of them for Crohn’s disease, and 4 of them for chronic pouchitis. Twelve of 400 is a pouch loss of 3%, but this incidence is bound to get higher with longer follow-up.
We mailed the questionnaire at home. We felt that patients would be more accurate to chart their functional data in the privacy of their home, over the course of a week. There was unfortunately no chance to maintain anonymity. These patients are well-known to us. They came back to the clinic with the questionnaire. But, certainly we did not change any of their answers, and therefore, we believe that we have avoided physician and surgeon biases in the reporting of the functional results.
Dr. Bruce A. Harms (Madison, Wisconsin): I too would like to congratulate you. A great report and good results in the difficult work of following 90%-plus patients. Just 1 quick comment.
Looking at your continence rate, if anything, it may be even better if you took out the 10% of patients with chronic pouchitis. One thing that was difficult for me to sort out is of the patients with major nighttime incontinence, how many of those fell into the category of chronic pouchitis patients?
As you know, with some patients, even though they may not have significant symptoms if you actually look at it you will see a low-grade pouchitis in a high percentage of patients, and if in fact you looked at that, would that have brought your overall continence rate up for the patients who did not have significant pouchitis.
Additionally, in relationship to your stricture rates, you commented that you may have had a higher stricture rate in those patients who were diverted. I question that a little bit from what you just said with a little selection bias. Do you have any manometric data to support that? Is it something you are looking at in your series of patients? And should you keep following this group of patients? Because even longer-term studies are going to be needed in the future. I would appreciate your comments.
Dr. Fabrizio Michelassi (Chicago, Illinois): Dr. Harms, thank you very much.
Our intent was to give an overall view of the entire group without selecting patient subgroups. We have already reported on patients with pouchitis and their functional results, in absolute terms, are worse than the ones obtained by patients without chronic pouchitis.
You are absolutely right in terms of the fact that this was a prospective observational study, not a randomized study. So, the higher incidence of anastomotic strictures in patients with an ileostomy probably indicates that these are the patients in whom the anastomosis was technically more difficult and probably under more tension, therefore resulting in a greater incidence of anastomotic strictures.
Yet it is interesting to postulate that the immediate transanal passage of fecal material may also have a protective effect on the anastomosis. It is my observation that patients with an ileostomy have more strictures even in the absence of undue tension on the anastomosis.
Dr. James M. Becker (Boston, Massachusetts): Neither of the studies today really addressed the issue of pouchitis, although you have alluded to that as an important factor. I wonder if you could comment further on pouchitis and any thoughts you have about how to treat this difficult condition, since that really is the single long-term problem associated with this otherwise wonderful operation.
I would agree that there may be a significant selection bias in regards to the decision to employ a diverting ileostomy. Could you comment more specifically on your criteria for applying an ileostomy or not applying it?
If you look at your length of stay data, your overall length of stay was over 9 days for the patients without an ileostomy and about 2 days less than that for patients with an ileostomy. The length of stay in many centers is quite a bit shorter than that. In my own experience, for those patients that have a routine diverting ileostomy, it is about 6 days and then 3 days for the ileostomy closure. Thus, the total length of stay really is no different than that reported today for patients that had no ileostomy but were in the hospital much longer the first time.
Dr. Fabrizio Michelassi (Chicago, Illinois): Dr. Becker, thank you very much.
As you know, pouchitis is the Achilles heel of this procedure. And as I already mentioned, at least 50% of our patients had at least 1 episode of acute pouchitis over the course of the study in the first 5 years and 10% of those patients converted to chronic pouchitis.
Acute pouchitis is easy to treat with 48 to 72 hours of antibiotics by mouth, but chronic pouchitis is difficult to treat and some of these patients will eventually lose the pouch because of unmanageable chronic pouchitis.
We follow patients with chronic pouchitis is with a flexible pouchoscopy every 3 to 6 months. At the time of the pouchoscopy we obtain biopsies to rule out the presence of dysplasia. We have found none so far.
We offer the option of a J-pouch ileo-anal procedure to patients with indeterminate colitis, although we caution them that the incidence of pouchitis and development of Crohn’s is higher than patients with ulcerative colitis.
I don’t call the decision to place or avoid a temporary ileostomy a selection bias; I call it surgical judgment. I did not randomize these patients. At the time of surgery if things were absolutely fantastic, there was no tension on the anastomosis, and I felt reassured about the technique and the overall condition of the patient, I felt that avoiding the morbidity of the temporary ileostomy was the right thing to do.
These patients stay in the hospital 2 days longer, an average of 9 days. Our average length of stay for patients with a temporary ileostomy is 7 days. We have a surgical practice that attracts patients from a distance. We don’t have any local facility to discharge patients to and still feel confident that they are within reach of the hospital. This explains our conservative attitude toward discharging patients and our average seven-day length of stay.
Dr. Eric W. Fonkalsrud (Los Angeles, California): I would also like to congratulate Dr. Michelassi for this excellent presentation on the indicators of pouch function. In our experience, the ability of the patient to urinate without having a bowel movement is an indicator of good coordinated pouch function. The ability to pass flatus without a movement is another good indicator. Lastly, we have found that females with ileoanal pouches for colitis often have some difficulty inbecoming pregnant compared with the normal female population. We have also observed a correlation between the presence of large ovarian cysts and the inability of females with pouches to have a pregnancy. Could you comment on some of these points.
Dr. Fabrizio Michelassi (Chicago, Illinois): Thank you, Dr. Fonkalsrud. You are absolutely on the mark by suggesting that these additional parameters really reflect quality of life. Many of our patients, indeed all male patients, are able to urinate without passing bowel movements. Female patients going to the bathroom to pass urine also take the opportunity to empty their pouch at the same time.
Another shortcoming of this procedure is that the majority of patients are not able to distinguish flatus from bowel movements. In our cohort of patients, only about 15% of all patients were able to always distinguish flatus from bowel movements.
There is increasing data suggesting that the fertility rate and pregnancy rate is much decreased in the female population. Data from Norway indicate that the fertility rate may be decreased to as low as 30% of the normal population. To go back to Dr. Pemberton’s question, another way to improve the procedure would be to figure out a way to do the procedure without decreasing the fertility rate in young female patients.
Footnotes
Reprints: Fabrizio Michelassi, MD, Professor and Vice Chairman, Chief, Section of General Surgery, Department of Surgery, The University of Chicago, 5841 South Maryland Avenue (MC 5094), Chicago, Illinois 60637. E-mail: fmichela@surgery.bsd.uchicago.edu.
REFERENCES
- 1.Michelassi F, Stella M, Block GE. Prospective assessment of functional results after ileal J pouch—anal restorative proctocolectomy. Arch Surg. 1993;128:889-895. [DOI] [PubMed] [Google Scholar]
- 2.Michelassi F, Block GE. A simplified technique for ileal J-pouch construction. Surg Gynecol Obstet. 1993;176:290-294. [PubMed] [Google Scholar]
- 3.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121-130. [PubMed] [Google Scholar]
- 4.McIntyre PB, Pemberton JH, Wolff BG, et al. Comparing functional results one year and ten years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Dis Colon Rectum. 1994;37:303-307. [DOI] [PubMed] [Google Scholar]
- 5.Bullard KM, Madoff RD, Gemlo BT. Is ileoanal pouch function stable with time? Dis Colon Rectum. 2002;45:299-304. [DOI] [PubMed] [Google Scholar]
- 6.Gemlo BT, Belmonte C, Witz O, et al. Functional assessment of ileal pouch-anal anastomotic technique. Am J Surg. 1995;169:137-142. [DOI] [PubMed] [Google Scholar]
- 7.Fazio VW, Ziv Y, Church JM, et al. Ileal pouch-anal anastomosis complications and function in 1005 patients. Ann Surg. 1995;222:120-127. [DOI] [PMC free article] [PubMed] [Google Scholar]