Abstract
The health care quality chasm is better described as a gulf for certain segments of the population, such as racial and ethnic minority groups, given the gap between actual care received and ideal or best care quality. The landmark Institute of Medicine report Crossing the Quality Chasm: A New Health System for the 21st Century challenges all health care organizations to pursue six major aims of health care improvement: safety, timeliness, effectiveness, efficiency, equity, and patient-centeredness. “Equity” aims to ensure that quality care is available to all and that the quality of care provided does not differ by race, ethnicity, or other personal characteristics unrelated to a patient's reason for seeking care. Baylor Health Care System is in the unique position of being able to examine the current state of equity in a typical health care delivery system and to lead the way in health equity research. Its organizational vision, “culture of quality,” and involved leadership bode well for achieving equitable best care. However, inequities in access, use, and outcomes of health care must be scrutinized; the moral, ethical, and economic issues they raise and the critical injustice they create must be remedied if this goal is to be achieved. Eliminating any observed inequities in health care must be synergistically integrated with quality improvement. Quality performance indicators currently collected and evaluated indicate that Baylor Health Care System often performs better than the national average. However, there are significant variations in care by age, gender, race/ethnicity, and socioeconomic status that indicate the many remaining challenges in achieving “best care” for all.
There is a significant gap between the quality of care the US health care system is capable of achieving and the quality of care it currently delivers. Rather than being the consequence of individual providers' actions or inadequacies, gaps in the quality of care are largely due to the failure of health care organizations to incorporate known improvement measures into the process of care. The 2001 Institute of Medicine (IOM) report Crossing the Quality Chasm: A New Health System for the 21st Century (1) asserts that the health care safety and quality problems exist because of limited infrastructure and outmoded care systems, which result in a cycle of suboptimal care being repeated throughout the many levels of care.
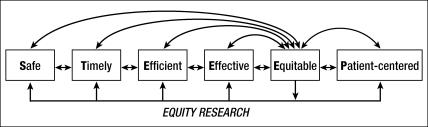
Crossing the Quality Chasm also issued a challenge for health care system improvement in recommending that all health care organizations, as well as professional groups and purchasers of health care, pursue six major aims of health care:
Safety: avoid injuries to patients from care that is intended to help them.
Timeliness: reduce waits and sometimes harmful delays for both those who receive care and those who give care.
Effectiveness: provide services based on scientific knowledge to all who could benefit and refrain from providing services to those not likely to benefit (avoid underuse and overuse, respectively).
Efficiency: avoid waste, including waste of equipment, supplies, ideas, and energy.
Equity: provide care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status (SES).
Patient-centeredness: provide care that is respectful of and responsive to individual patient preferences, needs, and values, ensuring that patient values guide all clinical decisions (1). Substantial improvements are achievable in all six dimensions of health care quality. The aim of equity is to ensure quality care benefits for all, based on individual need, and to ensure that quality of care does not differ because of race, ethnicity, or other personal characteristics unrelated to the patient's condition or reason for seeking care.
Baylor Health Care System (BHCS) has trademarked these six aims with the acronym STEEEP as a means of communicating both the dimensions and the magnitude of the challenge in the health care quality improvement journey (2). While achieving improvement in each of these six dimensions has not been officially prioritized, it is evident from the literature that achieving equitable care typically receives less attention in the quality arena. The reasons for this are likely manifold: providers may not be aware of the health disparities that exist within their patient populations, or may not have the data collection processes in place to examine them, or may assume that by addressing the other five dimensions of quality, equitable care will naturally follow. BHCS is in the unique position of being able to examine the current state of equity in a typical health care delivery system and to lead the way in health equity research.
BHCS is a not-for-profit integrated health care delivery system in Dallas–Fort Worth, Texas, including 14 owned or leased hospitals; >60 primary care, specialty care, and senior health centers; >400 physicians employed in the HealthTexas Provider Network (HTPN); and >3000 affiliated physicians. HTPN has approximately 850,000 annual ambulatory visits, and hospital admissions and emergency department visits totaled approximately 96,000 and 247,000, respectively, in 2004. BHCS does not own or operate a health plan nor participate in capitated care. It therefore represents a very different health care environment from staff-model health plans like Kaiser Permanente, private and public managed care organizations, and health plans that have a longer history of formalized quality improvement and health equity initiatives.
BHCS'S VISION OF “BEST CARE” EMBRACES EQUITY
BHCS has a long-standing commitment to quality in general and equity in particular. The first hospital in the system was founded in 1903 by Dr. George W. Truett, pastor of the First Baptist Church of Dallas, as “a great humanitarian hospital, one to which people of all creeds and those of none may come with equal confidence.” Today, BHCS outlines its commitment to quality in its five core values: quality, meeting the needs and striving to exceed the expectations of those we serve through continuous improvement; integrity, maintaining an ethical and respectful manner; servanthood, serving with an attitude of unselfish concern; innovation, consistently exploring, studying, and researching new concepts and opportunities; and stewardship, managing resources in a responsible manner. Its commitment to quality is also evident in its organizational vision, “to be trusted as the best place to give and receive safe, quality, compassionate health care,” and in its mission, “Founded as a Christian ministry of healing, Baylor Health Care System exists to serve all people through exemplary health care, education, research, and community service.” BHCS's business objectives are to deliver safe, quality, patient-centered care, supported by education and research; to be a leader in serving our communities; to be responsible financial stewards; and to be the best place to work and care for patients.
In addition to the “culture of quality” evident in the values, mission, and business objectives, BHCS has a formalized quality improvement system in place. The history of the development of this system has been detailed previously (2). Central to quality improvement at BHCS is the Best Care Committee. Established in 2001, the committee is a dedicated entity focusing on systemwide implementation of health care improvement initiatives, responsible for developing project concepts, designs, and budgets; coordinating the implementation of quality improvement projects throughout BHCS; and reporting results to accountable leaders. The primary vehicle for measuring, reporting, and tracking quality of care is the monthly Best Care Report produced by the Best Care Committee. A total of 60 clinical indicators focused on measures of health care underuse, overuse, and misuse are tracked through the Best Care Report, under the six STEEEP dimensions. Safety measures are based on the adverse event reporting system housed in MIDAS (a certified Joint Commission for the Accreditation of Healthcare Organizations [JCAHO] core measures vendor) and used in all BHCS hospitals. Timeliness measures look at the delivery of time-sensitive therapies—such as surgical infection prophylaxis and the first dose of antibiotics for pneumonia. Effectiveness measures include the JCAHO core measure for in-hospital quality (collected in MIDAS at all BHCS hospitals) and delivery of 11 clinical preventive services for ambulatory care practices (based on semiannual chart review). Efficiency measures assess the median time to delivery of time-sensitive therapies, and patient-centered measures are a subset of the questions included on the patient satisfaction survey questionnaires given to BHCS inpatients, outpatients, and primary care HTPN patients. Equity, rather than being examined through dedicated indicators, is reported in the Best Care Report by stratifying safety, timeliness, efficiency, effectiveness, and patient-centeredness performance indicators by age (<65 vs ≥65 years), gender, race (Black [used interchangeably with African American here], White, Hispanic, other), payer type (insured vs uninsured), and SES (based on the Claritas ZQ score (3) calculated based on the patient's ZIP code) for inpatient JCAHO core measure indicators and by age, gender, and SES for HTPN clinical preventive services indicators.
IMPLICATIONS OF EQUITY FOR BHCS OPERATIONS
Arguably, a health care system cannot claim to provide “best care”—or hope to achieve it—if subgroups of the population are receiving suboptimal care or care that does not meet the health care system's promulgated standards. For any organization to pride itself on providing “best care,” inequities in access, use, and outcomes of health care must be scrutinized and the critical injustice they create remedied. The cumulative evidence of racial/ethnic differences nationally is overwhelming, and the persistent disparities gap raises questions about equity and fairness in health care delivery.
Inequities in health care raise moral, ethical, economic and, perhaps, legal issues for health care system operations. In a constantly changing health care environment, inequities in health care pose moral and ethical issues for providers who are sworn and obligated to provide the best care possible but who also struggle with time constraints, coordination of care, and a limited clinical support system, oftentimes resulting in care outcomes that are less than personally desirable and satisfying. Bias and discrimination claims and violations of civil rights and patient protection regulations could have enormous legal ramifications.
Persistent health care inequities also raise concerns regarding the overall quality of health care and may have significant implications for overall health care expenditures. Greater equity and accountability of the health care system is important to a growing constituency of payers, providers, and individual consumers. Businesses, who sponsor and pay for employees' health insurance, are becoming increasingly concerned about the quality of care their employees receive given the rising health expenditures and the negative impact poor-quality care has on workers' productivity, attendance, and health care costs.
Although they have lower health care expenditures and receive fewer health care resources, particularly for high-end procedures such as catheterization, African Americans, Hispanics, and Native Americans have a higher burden of chronic disease, disease complications, and disabilities. Racial and ethnic minorities, persons of low SES, and other vulnerable groups also enter the health care system at more advanced stages of disease and with higher uncontrolled rates of treatable chronic conditions, such as hypertension (4) and diabetes (5). Furthermore, racial and ethnic minorities have greater rates of rehospitalization for very costly conditions, such as congestive heart failure (CHF) (6, 7), and are more likely to be hospitalized for preventable conditions (8). African Americans have nearly twice the rate of premature births as Whites (9) and thus a greater need for neonatal intensive care. All the above examples relate to health care system resource allocations and suggest opportunities for reducing unnecessary expenditures. Furthermore, better glycemic control, prevention of CHF rehospitalization due to uncontrolled hypertension, and higher rates of full-term births lead to enormous medical cost savings.
In addition to affecting resource allocation, reducing unnecessary expenditures, and potentially leading to medical care cost savings, equity impacts patient satisfaction, which speaks to the bottom line of health care. As in any business, satisfaction in health care is a factor of perceived quality, competency of providers, and personal respect and treatment received during visits. High patient satisfaction is related to return visits, compliance with medical treatment, adherence to mutually agreed goals of self-management, and, possibly, reduced hospital readmissions. It is also intuitive that poor public perception of a health care system is associated with poor community visibility and community relations, and it severely limits marketability of services and the ability to expand to select community markets.
To the extent that inequities in the health care system—especially those relating to the underuse of recommended and needed services—result in use of more costly services at a later stage of illness, poorer outcomes, and lost productivity, there are health and social costs beyond the individual or specific population group. The greater societal “added” value in eliminating health care inequities is consistent with BHCS's vision of compassionate and equitable best care. Perhaps equally important, proactive efforts to address inequities in health care identify opportunities for appropriate interventions to improve overall care quality.
THE GOALS OF HEALTH EQUITY
The many dimensions of inequities in health care include race, ethnicity, age, gender, social class, culture, and ability to pay. The persistent and unacceptable gap in health care access, use, and outcomes by race and ethnicity raises many questions about equity, fairness, and social justice given the history of discrimination in this country and society's struggle to rid itself of vestiges of legal and de facto segregation. The racial/ethnic gap in care quality is also a challenge and an affront to our abilities to achieve “best care.” BHCS has several goals related to equity:
To increase awareness of the importance of equity in clinical operations, provider practices, and in achieving best care
To create a cultural transformation in which equity is an essential element of clinical transformation
To integrate the concept of equity throughout health care operations and all other STEEEP dimensions of quality improvement and health care practices
To eliminate health care inequities
BHCS's current efforts and commitment to improve care quality and achieve best practices bode well for the organization to become a national leader in achieving equitable best care.
THE NEED FOR A COMPREHENSIVE STRATEGY FOR EQUITABLE BEST CARE
Views vary considerably on specific strategies to eliminate inequities in health care. However, a general consensus is emerging that a comprehensive, multidimensional strategy is needed to address this problem. Furthermore, it is becoming evident that local health care system problems need local health care system solutions. BHCS has a distinctive history and differs from other health care systems in its organizational structures, policies, and operations. These characteristics present unique opportunities to identify any inequities in health care, better understand the complex nature and causes of inequities within BHCS, and use appropriate BHCS data to design and implement activities aimed at ensuring equitable delivery of health care services. Nevertheless, the growing body of research and quality improvement initiatives as well as the unique characteristics of BHCS and its current efforts suggest a comprehensive strategy in advancing the equity dimension of STEEEP (Table 1)
Table 1.
A comprehensive strategy for equitable care in the Baylor Health Care System
| • Increase awareness among providers and decision makers of the importance of equity in “achieving best care” |
| •Ensure equitable access to preventive and curative health care services |
| • Reduce uncertainty in clinical decisions through real-time patient medical record and clinical laboratory information, evidence-based guidelines, and recommended standards of best care |
| •Improve efficiency and coordination of all aspects of primary care, ambulatory care, specialty care, and hospital care |
| •Eliminate variations in health care that may be due to unconscious and conscious cost considerations, reimbursements, and patient insurance coverage or perceived ability to pay |
| •Increase the knowledge base to better understand the nature and causes of health care inequities and appropriate interventions to eliminate them |
| •Create a culturally competent health care system capable of delivering the highest-quality and safest care available to every patient regardless of race, ethnicity, social class, culture, ability to pay, or language proficiency |
| •Ensure health system accountability in equitable care quality by tracking, monitoring, and reporting equity quality measures |
| •Integrate the elimination of inequities with quality improvement |
If efforts elsewhere are any indication, confronting racial and ethnic inequities at BHCS may be politically challenging. The contentious history of race relations, continuing significant controversy over whether racial/ethnic inequities exist within the system of care, and, to date, the lack of a clear, articulated strategy for eliminating them present challenges. However, these challenges are not insurmountable. With strong leadership, willingness to engage key stakeholders, and the continued involvement of clinical leaders and staff in the process of transformation, health care equity can be improved.
The senior leaders at BHCS have demonstrated their commitment to and direct participation in quality improvement initiatives. For example, the HTPN quality initiative that improved delivery of adult clinical preventive services to eligible patients from 37% in 1999 to 92% in 2005 was largely driven by Carl Couch, MD, MMM, chairman of the HTPN board, and David Winter, MD, MSc, chairman of the HTPN Quality Committee. Similarly, Bill Aston, chairman of the Baylor University Medical Center board, participated in a project to reduce time to first antibiotics for patients admitted with community-acquired pneumonia, and David Ballard, MD, PhD, senior vice president and chief quality officer for BHCS, participated in a project to reduce readmissions for heart failure as part of the Intermountain Healthcare Mini–Advanced Training Program in Health Care Delivery Improvement. BHCS modeled the Accelerating Best Care at Baylor (ABC Baylor) program after the Intermountain Healthcare program, educating physicians and nursing and administrative leaders on the tools and techniques of quality improvement. Senior leaders are involved in the ABC Baylor program in many ways—including serving on the steering committee and designing and teaching the classes. Joel Allison, BHCS president and chief executive officer, not only addresses each ABC Baylor class at the opening session but was one of the first graduates of the program. Extending this model of direct participation and involvement of senior leaders to equity initiatives will be instrumental to their success. The existence of the model is an aspect of BHCS that uniquely suits it to tackling the challenge of achieving health care equity.
Increasing awareness
The general public has a marginal awareness of the nature of racial/ethnic disparities and equity issues. Health care providers likewise have misperceptions of the nature of racial and ethnic inequities. In a recent national survey, two thirds (67%) of Whites indicated they believe that African Americans get the same quality of care as Whites, and over half (59%) of Whites indicated they believe Hispanics get the same quality of care as they do (10). In contrast, 64% of African Americans and 56% of Hispanics in this survey believed they received lower quality of care than Whites.
When physicians were asked about the unfair treatment of patients, less than a third of physicians (29%) indicated they believe the health care system “very often or somewhat often” treats people unfairly based on their racial/ethnic background.
Most often, physicians believed that insurance, education, and patient preferences were the reason for health care inequities. If misperceptions about the existence and nature of inequities are common, it is not only difficult to change practice behavior and institutional policies but also difficult to allocate resources to address the problem.
Collecting race/ethnicity data to identify inequities and plan interventions
Collecting accurate race/ethnicity data is a prerequisite for a comprehensive strategy to address inequities in health care. Not unlike BHCS, managed care plans, integrated health care systems, and hospitals around the country are taking this first step to identify inequities and are using race/ethnicity data as the foundation for clinical interventions to improve the quality of health care for racial and ethnic populations.
Managed care plans, particularly Medicare and Medicaid plans, have taken the lead in addressing health care inequities, often through federally funded collaborations. State Medicaid programs are required by the Centers for Medicare and Medicaid Services to provide data on enrollees' race/ethnicity and primary language to managed care plans, allowing plans to identify inequities in care quality and develop programs in culturally competent and linguistic services. Medicare managed care plans are under similar requirements to conduct at least one quality improvement project in the areas of culturally competent and linguistic services or “disparities” (11). Commercial, Medicare, and Medicaid managed care plans have conducted externally funded demonstration projects to collect data on race/ethnicity directly or use geocoding and surnames to prepare Health Plan Employer Data and Information Set (HEDIS) reports stratified by race/ethnicity.
Aetna, a major private insurer, is considered an industry leader in its effort to reduce or eliminate racial/ethnic disparities. Its chair and chief executive officer authorized the collection of race and ethnicity data in 2001. Data collection started with its health maintenance organization product in 13 states and the District of Columbia; in 2 years, it had expanded to 47 states and multiple product lines. Data collection is the cornerstone of Aetna's quality of care initiative and is being used to target members who are likely to benefit from its special programs and services (12). Aetna is also collecting data on race, ethnicity, and languages spoken by network physicians.
Since 2004, several of the largest health insurance plans and organizations (including Aetna, CIGNA, HealthPartners, Kaiser Permanente, and UnitedHealth Group) have partnered with the Agency for Healthcare Research and Quality (AHRQ) in the National Health Plan Learning Collaborative to Reduce Disparities and Improve Quality to test ways to improve the collection and analysis of race and ethnicity data, to match these data to HEDIS quality measures, and to develop replicable quality improvement interventions to close gaps in care that are identified in this process (13).
The Health Research and Educational Trust, an affiliate of the American Hospital Association, has developed a toolkit for collecting race, ethnicity, and primary language data in hospitals (14). Initially funded by the Commonwealth Fund, a consortium of six leading hospitals and health systems (Henry Ford Health Systems, Kaiser Permanente, Massachusetts General Hospital, Northwestern Memorial Hospital, Parkland Memorial Hospital, and the University of Pittsburgh Medical Center Health System) participated in developing this toolkit. The toolkit will guide quality improvement activities internally as well as promote similar efforts by other hospitals and health systems to assess quality and identify disparities in clinical diagnosis, treatment, and outcomes.
Using race/ethnicity data to target interventions
Commercial and Medicaid managed care organizations have been active in developing programs to reflect the cultural and ethnic needs of members. The programs emphasize preventive care, community and member health education, case management and disease management tracking, and the use of sophisticated technology to analyze and coordinate services.
Medicare, Medicaid, and commercial managed care plans have been funded by the Health Resources and Services Administration (HRSA) to analyze HEDIS and the Consumer Assessment of Health Plans Survey data and subsequently conduct quality improvement demonstration projects to reduce or eliminate inequities. Some progress toward these goals was noted in a relatively short 1-year period (11).
Health Disparity Collaboratives, established by HRSA's Bureau of Primary Health Care among regional networks of community health centers to improve quality of care for traditionally underserved populations, are being evaluated to determine their impact on chronic conditions such as diabetes, hypertension, asthma, and depression. The critical components of these collaboratives are support for patient self-management, support for collaborative decision making, clinical information system upgrades, delivery system redesign, health care system reorganization to include senior partnerships and clinical champions on teams, and the development of community partnerships. Quality improvement projects require that the teams plan, implement, review, and then integrate change into health care systems (i.e., the rapid-cycle change model of plan, do, study, and act).
Integrating efforts to improve quality and reduce inequities
Reducing inequities in health care must be synergistically integrated with quality improvement. General efforts at the national, regional, or local level that bring attention to racial/ethnic inequities in health care are not expected to eliminate the inequity gap. As in the case of high-cost surgical procedures among elderly Medicare beneficiaries, no evidence was found that Black-White differences in the receipt of coronary artery bypass grafting, carotid endarterectomy, hip and knee replacements, and five other surgical procedures changed in the 10-year period examined (15). On the other hand, the Black-White gap narrowed significantly in seven of nine clinical performance measures, and clinical performance improved in all measures, for elderly Medicare beneficiaries in managed care plans in a 7-year period as a result of local plans collecting race/ethnicity data and having to publicly report quality-of-care measures for breast cancer screening, diabetes care, and cardiovascular care (16).
In a Medicare-funded quality improvement initiative on the adequacy of hemodialysis, implemented by local dialysis centers and clinicians, a twofold improvement for all patients was observed and was accompanied by a significant reduction in the Black-White gap (from a 10% difference in 1993 to a 3% difference in 2000) and a significant reduction in the male-female gap (23% to 9% in the same time period) (17). The 8-year multimodal intervention included numerical reporting of quality, regular feedback of results to dialysis sites, and workshops and direct supervision for poorly performing sites. This is the first study to demonstrate concurrent longitudinal improvement in quality and racial inequities (18).
Improving access to health care
Persons having a usual source of care are more likely to obtain preventive, primary, and specialty care services. Certainly, insurance coverage must be part of a comprehensive strategy to reduce inequities in health care (10). Insurance is the single largest contributor to Hispanic-White differences (23%–33%) and African American–White differences (24%–42%) in having a usual source of care (19). Asian Americans, Hispanics, Native Americans, and African Americans make up 52% of the uninsured in the USA. Beyond insurance, other financial constraints, limited availability of providers in some locales, long waits for appointments, and limited culturally appropriate services result in vulnerable groups in rural and urban settings having a reduced level of care.
Public hospitals, community providers, and private and public managed care organizations have taken on the challenges of reducing barriers to care. Several hospitals are meeting their goals of timely appointments for any outpatient (within 3 days of initial call) and streamlining visits and waiting times such that a patient can complete the visit in 45 minutes or less (20). Reducing language barriers and hiring patient navigators to assist patients within the health care system hold promise.
Developing alliances with local community and faith-based organizations and local health departments is increasingly recognized as an essential element in improving access to care. Partnerships between community organizations and local health departments, for example, have led to the elimination of significant disparities in breast cancer and cervical cancer screening rates between Whites and African Americans and a substantial reduction in disparities in breast cancer screening rates between Whites and Hispanics. Health care organizations often have informal and formal relationships with local community groups through participation in community screenings, health fairs, health awareness campaigns, speakers bureaus, and community forums. As health care facilities around the country become actively engaged with the community, they develop into pivotal resources—improving access to care, enhancing ongoing community-based activities, and addressing other aspects of health care inequities. Financial incentives or payment structures for providers to reduce barriers and increase access to care for minority patients is a practical element of a comprehensive strategy for equitable care (21).
Developing broader approaches to reduce or eliminate inequities
Private health care systems are also entering the arena for reducing/eliminating health disparities. For example, the Henry Ford Health System has established an Institute on Multicultural Health (formerly known as the Center for Medical Treatment Effectiveness Programs in Diverse Populations) to improve health-related treatment outcomes and quality of life for racial and ethnic populations within the Henry Ford Health System and the wider community. The institute undertakes both research and practical initiatives, facilitating the delivery of quality care, providing community-based services and technical assistance to increase health awareness, increasing providers' understanding of culturally appropriate care, and identifying strategies to further establish and implement culturally appropriate care to improve outcomes and patient satisfaction (22). Current projects include the African American Initiative for Male Health Improvement (AIMHI) Network Chronic Disease Project, which includes health screening, education, referral and follow-up, nutrition counseling, fitness assessments and training, and ongoing support groups for persons with diabetes and cardiovascular diseases, and the Racial and Ethnic Approaches to Community Health (REACH) Partnership, which is designed to reduce disparities in diabetes and its complications in the African American and Hispanic communities using four interventions: community, the family, social support systems, and the health care system (22). The AIMHI project is funded by the Department of Health and Human Services, Office of Minority Health, and the REACH partnership is funded by the Centers for Disease Control and Prevention.
Adventist HealthCare, based in Rockville, Maryland, is in the process of establishing a Center for Health Disparities as part of the expanded vision for Washington Adventist Hospital. The community-based center will focus on improving access to care for underserved populations, combining clinical care, research, and health careers training (23).
In the managed care arena, Kaiser Permanente is a leader in the field of health equity initiatives. It has several active programs aimed at reducing health disparities:
The Kaiser Permanente Community Health Fund, established in 2004 at the Northwest Health Foundation, which aims to improve access to health care for vulnerable and uninsured populations, reduce health disparities, and promote intercultural health in the Northwest (24).
The Institute for Culturally Competent Care, which provides training, develops tools, and supports large-scale initiatives aimed at eliminating health care disparities and inequities. The institute further supports Centers of Excellence that develop innovative models of care for Kaiser Permanente's diverse membership. The first six such centers targeted the African American population, Armenian population, Hispanic population, members with disabilities, linguistic services, and women's health (25).
- Health disparities research projects, including
- – African Americans and breast cancer: what works?
- – Cancer screening, managed care, and the underserved
- – Cross-cultural communication in colorectal cancer screening
- – Educational disparities in diabetes complications
- – Ethnic disparities in childhood stroke
- – Ethnic disparities in perinatal outcomes
- – Patient-clinician factors influencing racial/ethnic variation in the treatment of coronary disease: the REMOVE CHD study
- – Differences in alcohol and drug treatment outcomes for various cultural groups (26)
As shown, health care organizations around the country are in the early stages of addressing inequities in health care. The larger effort to reduce or eliminate racial/ethnic inequities is led by the federal government primarily through its Medicare and Medicaid programs. These federal agency–led quality initiatives and funded collaborations are beginning to demonstrate, in a few examples from the national aggregate of data, a reduction in racial/ethnic inequities in the provision of health care, as indicated by selected quality performance measures.
However, health care is delivered locally, and system-level initiatives for local health care systems are necessary to better understand the contextual nature of inequities and to implement local solutions to suboptimal quality throughout the integrated system of local practice settings. A focused, comprehensive, and system-level quality improvement strategy at BHCS can demonstrate that equitable best care is achievable.
EQUITY RESEARCH AT BHCS
The “problem”
The problems to be addressed by equity research at BHCS are inherent in the “quality chasm.” We begin the research inquiry with the premise that health care quality is less than is achievable, desirable, expected, and, often, needed for all. Nationally, adult Americans may receive only about 55% of the recommended medical care for most major illness (27). For BHCS, quality performance indicators currently collected and evaluated indicate that the health care organization often performs better than the national average. For acute myocardial infarction (AMI) care, for example, BHCS hospitals continue to improve on benchmark measures, often exceeding the national average in five key quality care indicators (2). However, there are significant opportunities at BHCS for quality improvement.
The health care gap indicates that the quality chasm is far more severe for certain segments of the patient population who suffer from a relatively higher burden of disease, disease complications, disabilities, and premature deaths. Equity research recognizes that overall quality of care is less than optimal for all and focuses on the gap in health care access, use, and outcomes between racial/ethnic minorities and Whites. Regarding opportunities for improvement and racial/ethnic inequities, only 52% of African Americans and Whites and a relatively lower proportion of Hispanics (44%) meet the benchmark measure of percutaneous transluminal coronary angioplasty (PTCA) within 90 minutes of hospital arrival following an AMI, an opportunity for improvement for all and particularly for Hispanics (28).
A second premise that guides equity research is that system-level quality improvement, ongoing at BHCS, can yield desirable results and concurrently reduce racial/ethnic inequities in health care. For example, as a result of quality improvement efforts at BHCS, comparable rates for beta-blocker administration within 24 hours of hospital admission for AMI are observed for all racial/ethnic groups (94%–97%) (27). Smoking cessation counseling following an AMI is 98% to 100% for all racial/ethnic groups (28). For preventive services related to and impacting high-burden conditions for racial/ethnic minorities (hypertension-related conditions, cervical cancer incidence and mortality, and breast cancer mortality), BHCS has exceeded agreed-upon benchmarks.
A focus on racial/ethnic inequities does not exclude attention to other personal characteristics that are known to determine access, use, and outcomes of health care. Extensive research shows that inequities related to race, ethnicity, and SES pervade the health care system across all dimensions of quality, including patient safety, effectiveness, timeliness, and patient-centeredness (29). Within many subpopulations, including women, the elderly, inner-city residents, and residents of socially disadvantaged areas of limited social, civic, and health resources, significant inequities are observed in all aspects of health care. Equity research is intentionally interdisciplinary and seeks to better understand the interrelatedness of determinants of inequities within its scope of working to improve health care quality and equity.
The goal of equity research at BHCS is to facilitate equity in best health care delivery and outcomes through evidence-based research, translation of research into practice, policy assessment, dissemination of findings, and advocacy. Specifically, equity research will explore, monitor, understand, and explain racial/ ethnic and other inequities in health care; identify intervention opportunities; and demonstrate, through research, appropriate interventions to achieve equity in best health care delivery and outcomes.
Equity research objectives
Specific objectives for equity research at BHCS are as follows:
Plan and conduct interdisciplinary research that explores, identifies, monitors, and explains inequities in health care and identifies intervention opportunities and appropriate interventions for improving equity in best health care access, utilization, and outcomes
Integrate equity research throughout all other dimensions of best care research and quality improvement (Figure 1)
Develop, implement, and evaluate the effectiveness of health care interventions that eliminate inequities in health care and demonstrate equity in best health care processes (i.e., access, utilization, and delivery) and outcomes
Disseminate research findings to health care providers, policy makers, and consumers to promote equitable best care
Figure 1.
Integrating equity research into “STEEEP” best care research and practice.
Published research demonstrates that racial and ethnic inequities in access, use, and outcomes of health care are irrefutably consistent in certain areas (e.g., invasive cardiac care), require careful interpretation in other areas (e.g., cancer treatment), and are muddled in some areas (e.g., mental health) (30). Furthermore, racial/ethnic inequities are not limited to low-income, uninsured, or governmentally insured groups but are also observed among privately insured patients (30, 31). It must also be noted that racial/ethnic inequities persist when SES and other important determinants (e.g., age, gender, and insurance status) are accounted for (30). These findings indicate clearly that SES, insurance coverage, health status, disease severity, and patient preferences do not adequately explain racial/ethnic health care inequities. Some interpersonal factors may offer a partial explanation (e.g., culture, cultural perception, patient-provider communication, provider bias, and intentional and unintentional racism). System-level characteristics (care coordination, inefficiencies, lack of evidence-based clinical decisions, and uncertainty in clinical decisions) may prove to offer the best explanation and opportunities for achieving equity in health care access, use, and outcomes.
The nature of observed inequities is complicated by the fact that race and ethnicity are correlated with economic status, insurance coverage, health-seeking behavior, and preexisting disease burden. Disentangling these correlations to examine racial/ethnic inequities is more complex than is often recognized. In some cases, e.g., cardiac care, putative factors such as lack of insurance may widen the inequities gap (30, 32). Or as in the case of emergency care, for example for long-bone fracture, a combination of insurance coverage, personal characteristics, and injury severity may exacerbate inequities in care quality to a remarkable magnitude (33). Yet racial/ethnic inequities in access to medical treatment may be reduced or even absent under more universally accessible health care systems with more apparent uniformity in care, such as the Department of Defense, Veterans Health Administration (34–36), or private managed care organizations.
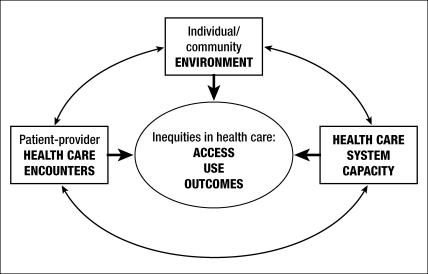
The theoretical framework of equity research
Three dimensions of health care inequities will frame interdisciplinary research development (Figure 2). Research in the individual/community environment dimension will examine such factors as sociocultural norms and values, social network and cohesion, and individual health promotion and care-seeking behaviors. Community-based participatory research, an important dimension of equity research, will appropriately engage community-based partners and key stakeholders to ensure the community/consumer/patient perspective and the origin of ideas in identifying determinants of inequities in access, use, and outcomes of health care.
Figure 2.
Theoretical model: dimensions of health care inequities.
The patient-provider dimension of equity research will focus on the nature and content of the health care encounter, patient-provider communication, and other interpersonal factors (such as trust, respect, and patient participation in clinical decisions; ability to navigate the health care system; and health literacy). Aligned with ongoing care improvement initiatives at BHCS, interventional research will address or evaluate the capacity of BHCS to deliver equitable best care (i.e., care coordination, inefficiencies, timeliness, accuracy of clinical data, and appropriateness of clinical decisions). These system-level interventions will be developed and implemented in the context of known determinants of health care access, utilization, and care outcomes (e.g., personal characteristics and economic, social, behavioral, cultural, interpersonal, and clinical factors). Several basic guiding questions will be used: Are there inequities in patient safety, timeliness of care, efficiency of care delivery, effectiveness of care provided, and patient-centeredness, particularly patient satisfaction with care received? What are the appropriate actions, based on the evidence, to reduce or eliminate observed inequities? Were actions taken effective in achieving equity?
BHCS QUALITY PERFORMANCE INDICATORS TO GUIDE EQUITY RESEARCH
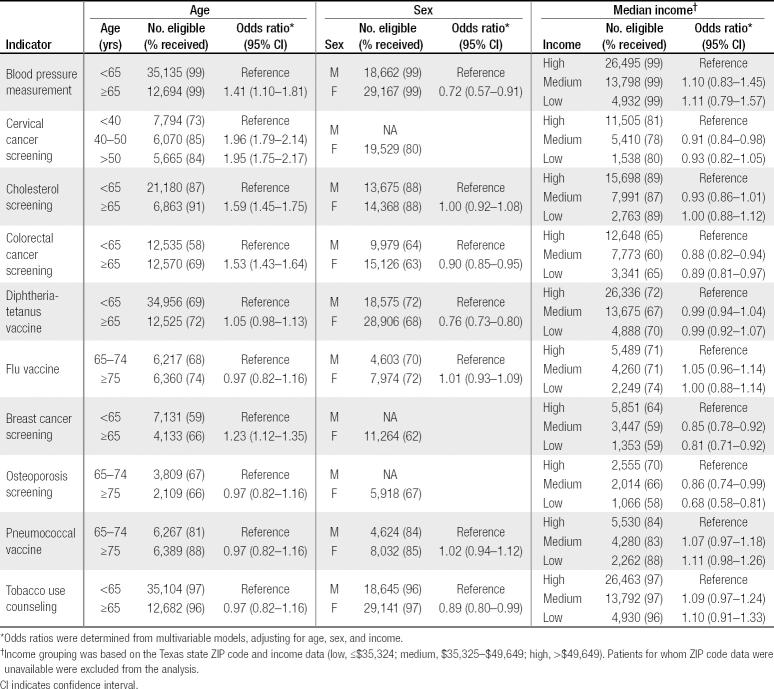
As an initial effort to identify opportunities around equity research within BHCS, exploratory analyses of the HTPN and BHCS quality indicator data, as well as the BHCS claims-based acute care mortality data, were conducted. The HTPN and BHCS data contained visits and discharges from July 2003 to June 2005. The acute care mortality data contained encounters from calendar year 2004. The objectives of these analyses were to estimate the effect of patient characteristics on both the odds of receiving indicated services in the ambulatory care and inpatient settings and the odds of dying during an acute care stay. The quality measures and related eligibility criteria used in the equity analyses are shown in Tables 2 and 3. Clinical preventive services indicators and definitions were chosen by the HTPN Quality Committee, based on the second edition of the US Preventive Services Task Force's Guide to Clinical Preventive Services (37).
Table 2.
Definitions of and patient eligibility criteria for clinical preventive services indicators tracked by HealthTexas Provider Network
| Clinical preventive service | Eligibility |
| Blood pressure: measured on each visit 1 year retrospective to most recent visit | All patients |
| Cervical cancer screening: Pap smear 3 years retrospective to most recent visit | Women 18–65 years |
| Cholesterol screening: 5 years retrospective to most recent visit | Men 35–75 years |
| Colorectal cancer screening: barium enema or flexible sigmoidoscopy 5 years retrospective to most recent visit, Colonoscopy 10 years retrospective to most recent visit, or fecal occult blood testing with 3 results within 1 year of the most recent visit | Women 45–75 years |
| Diphtheria-tetanus vaccine: 10 years retrospective to most recent visit Influenza vaccine: 1 year retrospective to most recent visit | ≥50 years |
| Breast cancer screening: mammogram 1 year retrospective to most recent visit | All patients |
| Osteoporosis screening: ever, over the age of 55 years | ≥65 years |
| Pneumococcus vaccine: ever | Women 50–75 years |
| Tobacco use counseling | Documented tobacco user |
Table 3.
Inpatient quality indicators tracked at Baylor Health Care System acute care hospitals: the 13 core measures of the Joint Commission for the Accreditation of Healthcare Organizations
| Clinical area | Indicator |
| Indicator | |
| Aspirin at admission | |
| Aspirin at discharge | |
| Acute myocardial infarction | Beta-blockers at admission |
| Beta-blockers at discharge | |
| ACE inhibitors for LVSD | |
| Antibiotics within 4 hours | |
| Community-acquired pneumonia | Oxygenation assessment |
| Pneumococcal vaccination | |
| Assessment of left ventricular function | |
| Congestive heart failure | ACE inhibitors for LVSD |
| Surgical infection prevention | |
| Antibiotic received within 1 hour prior to surgical incision | |
| Antibiotic selection for surgical patients | |
| Antibiotic discontinued within 24 hours of surgery end time |
ACE indicates angiotensin-converting enzyme; LVSD, left ventricular systolic dysfunction.
Inpatient quality measures are the 13 JCAHO core measures in the clinical areas of AMI, CHF, community-acquired pneumonia, and surgical infection prevention. Although it's not part of the core measures set, an additional AMI measure—PTCA within 90 minutes—was included in the analysis, as there was previous evidence of racial disparity with this indicator. Acute care mortality was calculated as the proportion of patients with an acute care encounter who died during the stay. Measure-specific multivariable models were developed for both the HTPN clinical preventive services and BHCS in-hospital measurement sets plus the acute care mortality measure. Descriptive statistics and adjusted odds ratios were calculated for each measure across the patient characteristics of interest.
Clinical preventive service indicator models contained a dichotomized age variable, gender, and median income of the patient's ZIP code as a proxy for SES, as these are the only characteristics currently available for these measures. To account for within-physician clustering, generalized estimating equations were used to derive adjusted odds ratios related to receiving an indicated preventive service. Logistic regression was used to model the BHCS in-hospital quality measures. In addition to age, gender, and ZIP code median income, the inpatient core measure logistic models included race/ethnicity and payer type. To reduce collinearity with payer type—which included Medicare as a category—age was treated as continuous. Furthermore, hospital, specified as a fixed effect, was included as a confounder. Logistic regression was also used to analyze the BHCS acute care mortality data. As with the in-hospital quality indicator models, the mortality model included age (continuous), gender, race/ethnicity, payer type, and ZIP code median income. Risk of mortality and hospital were included as confounders. Risk of mortality was calculated, using 2004 Texas administrative data, as the state death rate in the patient's all-patient-refined diagnosis-related group (APR-DRG, 3M Corp, Minneapolis, MN) risk of mortality subclass.
Table 4 indicates the variation in clinical preventive services by age, gender, and SES for HTPN. Of the quality indicators evaluated, significant variations by age were observed for five: blood pressure, cholesterol, cervical cancer, breast cancer, and colorectal cancer screening. Adults older than 65 years were consistently more likely to have had the blood pressure, cholesterol, and colorectal and breast cancer screenings than adults younger than 65 years. Women over 50 years had comparable cervical cancer screening rates to women between the ages of 40 and 50 years and were nearly twice as likely as women under 40 years of age to be screened for cervical cancer as recommended. Accounting for age and income, the results indicated that women were less likely than men to have been screened as recommended for high blood pressure (odds ratio [OR], 0.72; 95% confidence interval [CI], 0.57–0.91) and colorectal cancer (OR, 0.90; 95% CI, 0.85–0.95), less likely to have had a diphtheria-tetanus vaccine (OR, 0.76; 95% CI, 0.73–0.80), and marginally less likely to receive tobacco use counseling. Although not seen for the other clinical preventive services, women in the lower-income groups were significantly less likely to have had the recommended breast cancer screening (OR, 0.81; 95% CI, 0.71–0.92) and osteoporosis screening (OR, 0.68; 95% CI, 0.58–0.81) relative to women in the highest-income group.
Table 4.
Delivery of adult clinical preventive services by patient age, sex, and socioeconomic status by HealthTexas Provider Network physicians, July 2003 to June 2005
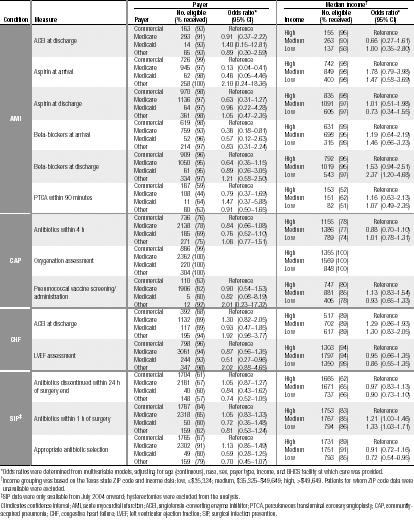
Variation in JCAHO core measures for in-hospital quality of care by patient demographic characteristics is shown in Tables 5 and 6. While the results indicate that the rate of aspirin prescription at discharge for AMI patients was similar for Blacks and Whites, Hispanics were significantly less likely to receive aspirin at discharge as a preventive measure (OR, 0.34;95% CI, 0.16–0.71). In contrast, Blacks were significantly less likely to receive PTCA within 90 minutes of hospitalization for AMI compared with Whites (OR, 0.29; 95% CI, 0.12–0.68). Hispanics were significantly more likely to receive angiotensin-converting enzyme inhibitors at hospital discharge for CHF (OR, 10.31; 95% CI, 1.41–75.50). On the other hand, Whites and Hispanics were less likely than Blacks to have a left ventricular ejection fraction assessment when hospitalized for CHF (White vs Black OR, 1.39; 95% CI, 0.90–2.13; White vs Hispanic OR, 0.70; 95% CI, 0.41–1.20). The results also indicated that Blacks and Hispanics were less likely to have antibiotics discontinued within 24 hours of surgery end time and that Hispanics were less likely to receive appropriate antibiotics for surgical infection prevention. When accounting for other personal characteristics (age, race/ethnicity, payer, and income), the results indicated that women were significantly less likely than men to receive PTCA within 90 minutes of arrival for AMI (OR, 0.56; 95% CI, 0.33–0.95). Regarding payer type, Medicare-insured patients were less likely to receive aspirin and beta-blockers at arrival for AMI, as were Medicaid patients to receive left ventricular ejection fraction assessment for CHF. No other variations in hospital quality by payer type were observed. No significant variation in hospital care quality was observed for the census track indicator of patients' income.
Table 5.
Delivery of Joint Commission for the Accreditation of Healthcare Organizations core measures for in-hospital quality of care by race/ethnicity, sex, and age for Baylor Health Care System hospitals, July 2003 to June 2005
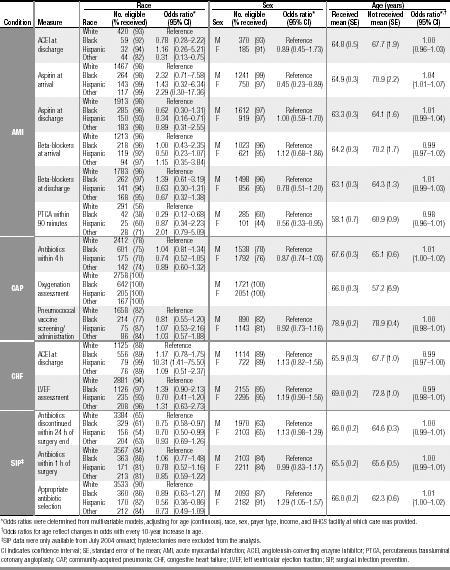
Table 6.
Delivery of Joint Commission for the Accreditation of Healthcare Organizations core measures for in hospital quality of care to eligible patients by median income and payer type for Baylor Health Care System hospitals, July 2003 to June 2005
Tables 7 and 8 show results of the acute care mortality analyses. Mortality rates for Blacks and Hispanics were similar to the rates for Whites. Inpatient mortality rates were significantly lower for women compared with men. The likelihood of acute care mortality increased with increasing age and was higher for Medicare-insured patients and patients with “other” insurance payers, compared with commercially insured patients. Patient income was not observed to be related to acute care mortality.
Table 7.
Acute care inpatient mortality by race/ethnicity, sex, and age for Baylor Health Care System hospitals, July 2003 to June 2005
| Race | Sex | Age (years) | |||||||
| Measure | Race | Discharges (% died) | Odds ratio∗ (95% CI) | Sex | Discharges (% died) | Odds ratio∗ (95% CI) | Died mean (SE) | Survived mean (SE) | Odds ratio∗,† (95% CI) |
| White | 43,820 (3) | Reference | |||||||
| Acute care | Black | 9,943 (3) | 0.86 (0.72–1.03) | M | 26,617 (3) | Reference | 67.6 (0.4) | 56.7 (0.1) | 1.03 (1.03–1.04) |
| mortality | Hispanic | 4,448 (3) | 1.07 (0.84–1.37) | F | 34,647 (2) | 0.85 (0.76–0.96) | |||
| Other | 3,053 (2) | 0.67 (0.49–0.92) | |||||||
∗Odds ratios were determined from multivariable models, adjusting for age (continuous), race, sex, payer type, income, diagnosis-related group, and BHCS facility at which care was provided.
†Odds ratios for age reflect changes in odds with every 10-year increase in age.
CI indicates confidence interval; SE, standard error of the mean.
Table 8.
Acute care inpatient mortality by payer type and median income for Baylor Health Care System hospitals, July 2003 to June 2005
| Payer | Median income† | |||||
| Measure | Payer | Discharges (% died) | Odds ratio∗ (95% CI) | Income | Discharges (% died) | Odds ratio∗ (95% CI) |
| Commercial | 26,674 (1.3) | Reference | ||||
| Medicare | 25,683 (4.1) | 0.95 (0.79–1.13) | High | 24,190 (2.2) | Reference | |
| Acute care mortality | Medicaid | 3,431 (3.2) | 1.57 (1.20–2.06) | Medium | 23,845 (2.7) | 1.06 (0.91–1.23) |
| Other | 5,476 (2.1) | 1.42 (1.09–1.84) | Low | 13,229 (3.4) | 1.03 (0.86–1.23) | |
∗Odds ratios were determined from multivariable models, adjusting for age (continuous), race, sex, payer type, income, diagnosis-related group, and BHCS facility at which care was provided.
†Income grouping was based on the Texas state ZIP code and income data: low, ≤$35,324; medium, $35,325–49,649; high, >$49,649. Patients for whom ZIP code data were unavailable were excluded from the analysis.
CI indicates confidence interval.
WHERE DO WE GO FROM HERE?
Equity refers to differences that are unnecessary or reducible and are unfair and unjust. The concept of fairness obviously involves a moral judgment and is, therefore, intrinsically difficult. As in the case with health outcomes, similarly the inequities in health determinants are those that should not exist. Every person should, in terms of equity, have the opportunity to access those sanitary and social measures necessary to protect, promote and maintain or recover health.
—Sir George Alleyne (38)
BHCS has some distinctive attributes—its founding philosophy, well-coordinated care, involved senior leadership, long-term commitment to providing quality health care, system for reporting quality performance to the board of directors and senior leaders, programs training physicians as quality leaders, and public reporting of quality performance data—that both contribute to the lack of inequities seen above and provide a unique opportunity to identify and target those areas where equity is still to be achieved. Significant financial investment in clinical transformation throughout BHCS, allowing new technologies to bring real-time patient care data and decision support to improve patient care, is also a major attribute. Such tools should aid improvement in areas where inequities are observed and/or areas where improvement impacts inequities: coordinating care (i.e., real-time linkage of primary, specialty, and hospital patient care data), providing evidence-based guidelines to facilitate clinical decisions, and reducing uncertainties and thus variation.
However, the scope of quality measures and thus health care equity assessment is limited and therefore reflects neither the quality of the comprehensive services BHCS offers nor some critical areas in which inequities are likely to exist. Furthermore, with the exception of acute care mortality, the quality indicators are all process of care measures. Outcomes of care (i.e., post-diagnosis or posthospitalization disease or health status, quality of life, disabilities, or death) are not included in the assessment of quality. Nevertheless, process of care quality indicators for specific clinical areas are evidence-based, and in these areas benchmark comparisons to BHCS standards and expectations of health care as well as national standards are made and tracked. Soon to be developed are BHCS-wide primary care quality indicators for chronic disease care, which should enhance opportunities for identifying and eliminating inequities.
EQUITY DIMENSION OF STEEEP: REMAINING CHALLENGES
Many areas of health care in which inequities may exist have not yet been assessed at BHCS. The 2005 National Healthcare Disparities Report finds that disparities related to race, ethnicity, and SES “pervade the American health care system” and are observed in almost all aspects of health care (39). Disparities are observed across all dimensions of quality (including patient safety, effectiveness, timeliness, and patient-centeredness), in access to care, across many levels and types of care (preventive care, acute care, and chronic disease management), across many clinical conditions (heart disease, cancer, diabetes, HIV disease, mental health, and others), and across many settings (primary care, emergency department, and hospitals). African Americans and Native Americans receive poorer quality of care than Whites for 56% (20/36) and 38% (8/21) of core measures, respectively; Asians receive poorer quality care for 22% of core measures (7/32); and Hispanics receive poorer quality of care for 53% of core measures (20/38) compared with non-Hispanic Whites. Low-income persons invariably receive poorer care quality than high-income persons for 85% of core report measures (11/13) (39). A glimmer of hope, as reported, is that some observed disparities are diminishing.
Measures of quality improvement and equity
In the context of system-level quality improvement and the thesis that improving quality concurrently reduces or eliminates inequities, the same quality measures for quality improvement should be applied to monitoring initiatives to reduce inequities. The AHRQ National Healthcare Quality Report and National Healthcare Disparities Report use identical quality measures (179 measures, balanced toward effectiveness) across 8 quality dimensions of patient safety, 38 of timeliness, 122 of effectiveness, and 8 of patient-centeredness. The use of identical measures for improving quality and concurrently eliminating health care inequities is based on previous guidance by the IOM (40, 41). The disparities report has the additional quality dimension of care access—appropriate to a comprehensive strategy for eliminating inequities. Its access domains include getting into the health care system, getting care within the health care system, finding providers who meet individual patient needs, and utilizing health care (i.e., successful receipt of needed services).
BHCS needs a methodical approach to establish a balanced set of measures for the equity component of STEEEP, based on importance (potential impact on health problems, policy makers' and consumers' concerns, and the system's capacity to address the problem), scientific soundness (scientific evidence for the measure, validity, reliability across population groups), and feasibility (amount and timeliness of data collection, cost of data collection, comparison across population groups) (42). These measures should be linked to the various perspectives and priorities articulated in the BHCS organizational goals. Focused research on specific problems identified in the hospitals, emergency departments, and ambulatory practice settings, and targeted interventions to address these problems, must necessarily complement this approach of measuring and reporting a core set of quality indicators.
Equity tracking and monitoring system
More detailed self-reported race and ethnicity data, reflective of the Dallas–Fort Worth population (Table 9), are needed. Individual-level data for SES (education and individual and family income) and, ideally, primary language are also needed. Collection of accurate, individual-level data is essential to BHCS's ability to track and monitor inequities in health care delivery of services and outcomes of care.
Table 9.
Racial and ethnic composition of the Baylor Health Care System (BHCS) patient population, the patient population reported by the Dallas–Fort Worth Hospital Council (DFWHC) for area hospitals, and the Dallas–Fort Worth (DFW) metroplex∗
| Race/ethnicity | BHCS patients N = 292,065) n (%) | DFWHC (N = 660,129) n (%) | DFW counties N = 5,221,801) n (%) |
| Race/ethnicity | |||
| Race (non-Hispanic) | |||
| White alone | 184,541 (63.2%) | 398,991 (60.4%) | 3,096,104 (59.3%) |
| Black or African American alone | 46,913 (16.1%) | 101,818 (15.4%) | 711,704 (13.6%) |
| American Indian and Alaska Native alone | 610 (0.2%) | 538 (0.1%) | 21,419 (0.4%) |
| American Indian alone | 21,170 | ||
| Alaska Native alone | 220 | ||
| Asian alone | 4,856 (1.7%) | 12,170 (1.8%) | 193,742 (3.7%) |
| Asian Indian alone | 49,669 | ||
| Bangladeshi alone | 1,192 | ||
| Cambodian alone | 3,310 | ||
| Chinese alone | 33,559 | ||
| Filipino alone | 13,196 | ||
| Hmong alone | 277 | ||
| Indonesian alone | 656 | ||
| Japanese alone | 5,236 | ||
| Korean alone | 18,123 | ||
| Laotian alone | 6,642 | ||
| Malaysian alone | 266 | ||
| Pakistani alone | 5,905 | ||
| Sri Lankan alone | 379 | ||
| Thai alone | 2,843 | ||
| Vietnamese alone | 47,090 | ||
| Other specified Asian alone | 590 | ||
| Native Hawaiian and Other Pacific | |||
| Islander alone | (390 (0.1%) | † | 3,705 (0.1%) |
| Polynesian alone | 2,661 | ||
| Native Hawaiian alone | 823 | ||
| Samoan alone | 645 | ||
| Tongan alone | 1,032 | ||
| Micronesian alone | 983 | ||
| Guamanian or Chamorro alone | 691 | ||
| Some other race alone | 14,619 (5.0%) | 23,364 (3.5%) | 5,519 (0.1%) |
| Two or more races | 69,258 (1.3%) | ||
| Hispanic/Latino (of any race) | 40,136 (13.7%) | 123,236 (18.7%) | 1,120,350 (21.5%) |
| Mexican | 889,879 (17.0%) | ||
| Puerto Rican | 16,191 (0.3%) | ||
| Cuban | 7,072 (0.1%) | ||
| Other Hispanic or Latino | 207,208 (4.0%) |
∗BHCS data are from inpatient administrative data for patients seen between July 1, 2005, and December 31, 2005, at the following BHCS hospitals: Baylor University Medical Center at Dallas, Baylor Medical Center at Irving, Baylor Medical Center at Garland, Baylor Regional Medical Center at Grapevine, Baylor Medical Center at Waxahachie, Baylor Regional Medical Center at Plano, Baylor All Saints Medical Center at Fort Worth, and Baylor Medical Center at Southwest Fort Worth. DFWHC data are for January 1 to December 31, 2004. DFW metroplex counties are defined by the US Census Bureau as a Metropolitan Statistical Area (updated November 2004) and include the following counties: Collin, Dallas, Delta, Denton, Ellis, Hunt, Kaufman, Rockwall, Johnson, Parker, Tarrant, and Wise.
†Combined with Asian.
An equity tracking and monitoring system is recommended across the STEEEP quality dimensions, with additional quality indicators of access and outcomes of care measures. Such a system, using an established core set of measures, would provide the means to track inequities and report changes. Analyses and reports should be stratified by age, gender, race/ethnicity, and SES to allow identification of inequities among population subgroups. Multivariate analyses could identify the relative effects or importance of age, gender, race/ethnicity, SES, residence, or other personal characteristics on inequities. Multivariate analyses could also make appropriate adjustments for these personal characteristics within and across the other dimensions of quality, such as when reporting estimates of patient safety, effectiveness of AMI care, or measures of patient satisfaction. Accounting for confounding of other personal characteristics in multivariate analyses, trends over time in observed racial/ethnic inequities, and progress made in eliminating them could be monitored and reported.
To meet its goal to provide “best care,” BHCS must create a culturally competent health care system capable of delivering the highest quality and safest care available to every patient regardless of race, ethnicity, social class, culture, ability to pay, or language proficiency. Cultural competence is an important element of health care quality. Competence implies that an organization has the capacity to function effectively within the context of cultural beliefs, behaviors, values, social norms and needs of the patients and their communities of origin, affiliation, or residence (43). An early stage of cultural competence, i.e. cultural sensitivity, is the extent to which ethnic or cultural characteristics, experiences, norms, values, behavioral patterns, and beliefs of subgroups, as well as relevant historical, environmental, and social forces, are incorporated in the design, delivery, and evaluation of health care interventions (44). The patient-centeredness dimension of quality, as recommended by the IOM and incorporated in the BHCS STEEEP quality improvement initiative and challenge for best care, embodies the concept of cultural competence.
There is a considerable interest in cultural competence among health care providers, public health practitioners, community program planners, policy makers, and academics. This interest is stimulated, to a large extent, by the growing racial and ethnic diversity of the US population and the desire of health care professionals to address the health needs of African Americans, Hispanics, Asian/Pacific Islanders, Native Americans, and other ethnic Americans. Providing culturally competent services also has the potential to improve health care outcomes, increase patient satisfaction, and increase the efficiency and effectiveness of clinical and support staff, simultaneously reducing health care inequities (44, 45)
Despite widespread agreement on the need for culturally competent care interventions, the lack of consensus on a definition of cultural competence and, consequently, the difficulties associated with assessing and measuring its effectiveness have slowed progress. Nevertheless, cultural competence is emerging as a strategy for not only eliminating inequities but also improving health care quality and operations (46). Generally, it is agreed that a culturally competent health care system would have the following components:
Interpreter services: translation services to improve communication between people who speak different languages.
Recruitment and retention efforts: the employment and retention of a culturally diverse clinical staff that reflects the communities being served.
Training: the implementation of training programs that help educate practitioners and other members of the staff on effective communication methods and that increase cultural awareness and produce changes in attitudes about cross-cultural interactions.
Use of community health workers: liaisons to the community who provide ways to improve associated access to care and communication between providers and patients and who serve as mediators and endorsers of the health care system.
Culturally competent health promotion: incorporation of culturally specific and sensitive messages into health promotion efforts (i.e., screening tools and health literature) to encourage healthy behaviors that decrease risk, increase knowledge, and change attitudes.
-
Administrative and organizational accommodations: The change of physical environments and assessment procedures to enhance sensitivity to the unique languages, cultures, and environment of the population (e.g., signage, directions, or procedures written in appropriate languages; reading materials, artwork, or decor reflective of cultural diversity and the culture of the patients being served) (45, 47).
A culturally competent health care system can improve communication between providers and patients. Ineffective communication creates barriers to health care access, reducing the likelihood of appropriate follow-up, and may undermine the trust in the quality of care received (43). A culturally competent health care system recognizes that ethnicity and culture influence health beliefs, perception of health and disease, individual symptom recognition, health care–seeking behavior, and the use of health care services. Inappropriate treatment and referral patterns and unconscious and conscious negative attitudes and stereotypes based on personal characteristics may be minimized—along with their effect on clinical decisions—in a health care organization that strives for cultural competence.
Beyond the bricks and mortar
In addition to tracking and reporting equity measures, implementing specific initiatives aimed at reducing the inequities thus identified, and “building” a culturally competent health care system, establishing a mutually beneficial relationship between health care providers and the community is an important aspect of eliminating health inequities. Important components of building such a relationship include strengthening patient relationships with primary care providers who can help navigate the health care system and thus improve access to care and developing a relationship with the local community leaders, organizations, and community lay health advisors and advocates. The IOM report Unequal Treatment (21) advocates the use of community health workers who serve multiple roles, including improving access to care. They act as liaisons between patients and providers and contribute to the continuity and coordination of care: they help patients make and keep clinic appointments and help them adhere to treatment and disease management recommendations and prescribed medications. Community health workers can also help increase the use of preventive and primary care services and provide patient education, as well as education for providers about community needs and the culture. There is some evidence that implementing this model can help improve the quality of care and reduce health care costs (21).
BHCS needs to move beyond the “brick and mortar” to enhance its presence and increase its visibility in the local community—particularly in areas where health care needs are greatest. To be trusted as the best place to receive safe, quality, and compassionate health care, BHCS must be seen as a respectful and trusted partner to local communities whose own expertise and capacity are equal to BHCS's health care expertise and resources. It is only in this delicate balance of “equals” that sustainable health promotion, disease prevention, and quality health care can achieve the goal of eliminating health care and health inequities.
Acknowledgments
The authors thank Briget da Graca, MS, for writing and editorial support.
References
- 1.Corrigan JM, Donaldson MS, Kohn LT, Maguire SK, Pike KC. A New Health System for the 21st Century. Washington, DC: Institute of Medicine, National Academy of Sciences, National Academies Press; 2001. Crossing the Quality Chasm. [Google Scholar]
- 2.Ballard DJ, Spreadbury B, Hopkins RS., III Health care quality improvement across the Baylor Health Care System: the first century. Proc (Bayl Univ Med Cent) 2004;17(3):277–288. doi: 10.1080/08998280.2004.11927982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Claritas Inc. Population and Housing Profiles of all US Residential 5-digit ZIP Codes. Alexandria, VA: Claritas; 1999. REZIDE: The National ZIP Code Encyclopedia. [Google Scholar]
- 4.Centers for Disease Control and Prevention Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2005;54(1):7–9. [PubMed] [Google Scholar]
- 5.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290(14):1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 6.Alexander M, Grumbach K, Remy L, Rowell R, Massie BM. Congestive heart failure hospitalizations and survival in California: patterns according to race/ethnicity. Am Heart J. 1999;137(5):919–927. doi: 10.1016/s0002-8703(99)70417-5. [DOI] [PubMed] [Google Scholar]
- 7.Philbin EF, DiSalvo TG. Prediction of hospital readmission for heart failure: development of a simple risk score based on administrative data. J Am Coll Cardiol. 1999;33(6):1560–1566. doi: 10.1016/s0735-1097(99)00059-5. [DOI] [PubMed] [Google Scholar]
- 8.Davis SK, Liu Y, Gibbons GH. Disparities in trends of hospitalization for potentially preventable chronic conditions among African Americans during the 1990s: implications and benchmarks. Am J Public Health. 2003;93(3):447–455. doi: 10.2105/ajph.93.3.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. Health, United States, 2005. Washington, DC: US Government Printing Office, 2005. Available at http://www.cdc.gov/nchs/hus.htm; accessed January 16, 2006.
- 10.The Henry J. Kaiser Family Foundation. Race, Ethnicity and Medical Care: A Survey of Public Perceptions and Experiences. Menlo Park, CA, 1999. Available at http://www.kff.org/minorityhealth/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=13294; accessed January 16, 2006.
- 11.Nerenz DR. Health care organizations' use of race/ethnicity data to address quality disparities. Health Aff (Millwood) 2005;24(2):409–416. doi: 10.1377/hlthaff.24.2.409. [DOI] [PubMed] [Google Scholar]
- 12.Hassett P. Taking on racial and ethnic disparities in health care: the experience at Aetna. Health Aff (Millwood) 2005;24(2):417–420. doi: 10.1377/hlthaff.24.2.417. [DOI] [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and Quality. Major health plans and organizations join AHRQ to reduce racial and ethnic disparities in health care [press release]. Rockville, MD: AHRQ, December 14, 2004. Available at http://www.ahrq.gov/news/press/pr2004/dispcolpr.htm; accessed January 5, 2006.
- 14.Health Research and Educational Trust. Eliminating Disparities Through Community and Hospital Partnerships. Available at http://www.hret.org/hret/programs/eliminatingdisparities.html; accessed January 5, 2006.
- 15.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353(7):683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 16.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 17.Sehgal AR. Impact of quality improvement efforts on race and sex disparities in hemodialysis. JAMA. 2003;289(8):996–1000. doi: 10.1001/jama.289.8.996. [DOI] [PubMed] [Google Scholar]
- 18.Aaron KF, Clancy CM. Improving quality and reducing disparities: toward a common pathway. JAMA. 2003;289(8):1033–1034. doi: 10.1001/jama.289.8.1033. [DOI] [PubMed] [Google Scholar]
- 19.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Aff (Millwood) 2005;24(2):398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- 20.Baquet CR, Carter-Pokras O, Bengen-Seltzer B. Healthcare disparities and models for change. Am J Manag Care. 2004;10(Spec No):SP5–SP11. [PubMed] [Google Scholar]
- 21.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine, National Academy of Sciences, National Academies Press; 2002. [PubMed] [Google Scholar]
- 22.Henry Ford Health System. Health and healthcare research. Available at http://www.henryfordhealth.org/body.cfm?id=40610#Institute; accessed January 5, 2006.
- 23.Adventist Healthcare. Washington Adventist Hospital announces expanded vision for service to community. Available at http://www.adventist healthcare.com/wah/vision/; accessed January 5, 2006.
- 24.Northwest Health Foundation. Kaiser Permanente Community Fund at Northwest Health Foundation. Available at http://www.nwhf.org/ opportunities/kaiser.php; accessed January 6, 2006.
- 25.Chong N, Tico S, Gupte S. Kaiser Permanente Institute for Culturally Competent Care. Paper presented at the 131st Annual Meeting of the American Public Health Association, 2003.
- 26.Kaiser Permanente. News, views & issues: Racial and ethnic health disparities. Available at http://xnet.kp.org/communitybenefit/news/disparities.html; accessed January 6, 2006.
- 27.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 28.Baylor Health Care System. Best Care Report. Dallas, TX: BHCS, December 2005.
- 29.Agency for Healthcare Research and Quality. National Health Care Quality Report [AHRQ Pub. No. 06–0018]. Rockville, MD: AHRQ, December 2005. Available at http://www.ahrq.gov/qual/nhqr05/nhqr05.pdf; accessed January 13, 2005.
- 30.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57(Suppl 1):108–145. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 31.Carlisle DM, Leake BD, Shapiro MF. Racial and ethnic differences in the use of invasive cardiac procedures among cardiac patients in Los Angeles County, 1986 through 1988. Am J Public Health. 1995;85(3):352–356. doi: 10.2105/ajph.85.3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lillie-Blanton M, Maddox TM, Rushing O, Mensah GA. Disparities in cardiac care: rising to the challenge of Healthy People 2010. J Am Coll Cardiol. 2004;44(3):503–508. doi: 10.1016/j.jacc.2004.04.043. [DOI] [PubMed] [Google Scholar]
- 33.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269(12):1537–1539. [PubMed] [Google Scholar]
- 34.Selim AJ, Fincke G, Berlowitz DR, Cong Z, Miller DR, Ren XS, Qian S, Rogers W, Lee A, Rosen AK, Selim BJ, Kazis LE. No racial differences in mortality found among Veterans Health Administration out-patients. J Clin Epidemiol. 2004;57(5):539–542. doi: 10.1016/j.jclinepi.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 35.Goldstein LB, Matchar DB, Hoff-Lindquist J, Samsa GP, Horner RD. Veterans Administration Acute Stroke (VASt) Study: lack of race/ethnic-based differences in utilization of stroke-related procedures or services. Stroke. 2003;34(4):999–1004. doi: 10.1161/01.STR.0000063364.88309.27. [DOI] [PubMed] [Google Scholar]
- 36.Rehman SU, Hutchison FN, Hendrix K, Okonofua EC, Egan BM. Ethnic differences in blood pressure control among men at Veterans Affairs clinics and other health care sites. Arch Intern Med. 2005;165(9):1041–1047. doi: 10.1001/archinte.165.9.1041. [DOI] [PubMed] [Google Scholar]
- 37.US Preventive Services Task Force. Guide to Clinical Preventive Services, 2nd ed. Washington, DC: Office of Disease Prevention and Health Promotion, 1996. Available at http://www.ahrq.gov/clinic/cpsix.htm; accessed February 9, 2006.
- 38.Alleyne GAO. Equity and health. Speech presented at the XI World Congress of Psychiatry, Hamburg, Germany, August 1999.
- 39.Agency for Healthcare Research and Quality. National Health Care Disparities Report [AHRQ Pub. No. 06–0017]. Rockville, MD: AHRQ, December 2005. Available at http://www.qualitytools.ahrq.gov/disparitiesreport/2005/browse/browse.aspx; accessed February 14, 2006.
- 40.Swift EK. Guidance for the National Healthcare Disparities Report. Washington, DC: Institute of Medicine, National Academies Press; 2002. [PubMed] [Google Scholar]
- 41.Hurtado MP, Swift EK, Corrigan JM. Envisioning the National Health Care Quality Report. Washington, DC: Institute of Medicine, National Academies Press; 2001. [PubMed] [Google Scholar]
- 42.Kelley E, McNeill D, Moy E, Stryer D, Burgdorf J, Clancy CM. Balancing the nation's health care scorecard: the National Healthcare Quality and Disparities Reports. Jt Comm J Qual Patient Saf. 2005;31(11):622–630. doi: 10.1016/s1553-7250(05)31080-4. [DOI] [PubMed] [Google Scholar]
- 43.Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J, Task Force on Community Preventive Services Culturally competent healthcare systems. A systematic review. Am J Prev Med. 2003;24(3 Suppl):68–79. doi: 10.1016/s0749-3797(02)00657-8. [DOI] [PubMed] [Google Scholar]
- 44.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10–21. [PubMed] [Google Scholar]
- 45.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57(Suppl 1):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Betancourt JR, Green AR, Carrillo JE, Park ER. Cultural competence and health care disparities: key perspectives and trends. Health Aff (Millwood) 2005;24(2):499–505. doi: 10.1377/hlthaff.24.2.499. [DOI] [PubMed] [Google Scholar]
- 47.Department of Health and Human Services. The Office of Minority Health. Available at http://www.omhrc.gov/; accessed February 14, 2006.