Abstract
Bloodstream infections due to antimicrobial-resistant Staphylococcus aureus occur with increasing frequency and represent an important cause of morbidity and mortality. To date, the evaluation of pharmacokinetic-pharmacodynamic relationships for efficacy among patients with bacteremia has been limited. The objectives of these analyses were to evaluate relationships between microbiological and clinical responses for patients with S. aureus bacteremia and exposures for oritavancin, a novel bactericidal glycopeptide in development. Bayesian oritavancin exposure predictions, following treatment with 5, 6.5, 8, or 10 mg/kg of body weight/day, were derived using a validated population pharmacokinetic model for 55 patients with S. aureus bacteremia. Using classification and regression tree analysis, a breakpoint of the percentage of the dosing interval duration for which free-drug concentrations were above the MIC (free-drug % time > MIC) of 22% was identified for microbiological response; the probabilities of success greater than or equal to and less than this value were 93% and 76%, respectively. Using logistic regression, a relationship was found between microbiological response and free-drug % time > MIC (odds ratio = 4.42, P = 0.09, and odds ratio = 8.84, P = 0.05, when one patient, a medical outlier, was excluded). A similar relationship was found for clinical response. These results will be valuable in supporting dose selection of oritavancin for patients with S. aureus bacteremia.
An understanding of the relationship between pharmacokinetics and pharmacodynamics has become increasingly important for supporting dose selection of new antimicrobial agents. Data from nonclinical models of infection are commonly used to elucidate the pharmacokinetic-pharmacodynamic (PK-PD) measures associated with efficacy and the magnitude of the PK-PD measures predictive of optimal outcome. While the evaluation of such relationships using clinical data from infected patients is of greater interest, these data have been limited. However, in the case of lower respiratory tract infections, a number of analyses of clinical data have demonstrated exposure-response relationships for efficacy and have also served to validate PK-PD targets derived from nonclinical models (1, 7, 8, 10, 11, 12, 13, 14). To date, the evaluation of PK-PD relationships in patients with other types of infections has been limited.
Bacteremia with resulting sepsis represents a significant cause of morbidity and mortality (16). In the United States alone, the annual number of cases is estimated to range between 200,000 and 300,000, with crude mortality rates as high as 50% (17). The proportion of bloodstream infections arising from gram-positive pathogens has increased markedly over the last few decades (2). For infections arising from Staphylococcus aureus, common sources include nosocomial pneumonia, catheter-related infections, and complicated skin and skin-structure infections. Given that bacteremia either is primary (i.e., has no obvious source) or is associated with infection at an anatomic site and that bacteremic patients with a systemic inflammatory response syndrome represent a very heterogeneous population, the evaluation of antimicrobial efficacy in patients with bloodstream infections is challenging. As a result, indications for bacteremia or septicemia or both can be found in only a limited number of anti-infective labels, all prior to 1992. However, since outcomes in patients with bloodstream infections provide valuable supportive information for other indications, the evaluation of exposure-response relationships for efficacy in patients with bacteremia is of interest.
Oritavancin (LY333328) is a novel glycopeptide antimicrobial agent currently being developed for the treatment of complicated skin and skin-structure infections, including those caused by multidrug-resistant gram-positive pathogens. Oritavancin is active against S. aureus (including methicillin-resistant strains), coagulase-negative staphylococci (including methicillin- and glycopeptide-resistant strains), Enterococcus faecium (including glycopeptide- and ampicillin-resistant strains), and Enterococcus faecalis (including glycopeptide- and quinupristin-dalfopristin-resistant strains) (R. S. Blosser, J. S. Loutit, S. B. Porter, R. K. Flamm, and D. F. Sahm, Abstr. 43rd Intersci. Conf. Antimicrob. Agents Chemother., abstr. C1-1636, 2003; D. F. Sahm, R. S. Blosser, J. S. Loutit, and S. B. Porter, Abstr. 43rdIntersci. Conf. Antimicrob. Agents Chemother., abstr. C1-1640, 2003). Since the relationship between drug exposure and antimicrobial effect in patients with bacteremia has not previously been evaluated, the analyses presented herein, based on data collected from a dose-finding, phase 2 study in patients with S. aureus bacteremia treated with oritavancin (J. S. Loutit, W. O'Riordan, J. San Juan, J. Mensa, R. Hanning, S. Huang, and S. B. Porter, Abstr. 14th Eur. Congr. Clin. Microbiol. Infect. Dis., abstr. P541, 2004), provided an opportunity to explore exposure-response relationships for efficacy.
MATERIALS AND METHODS
Patient population.
This study was conducted in 23 medical centers in Argentina, Australia, Germany, India, The Netherlands, Taiwan, Spain, the United Kingdom, and the United States. Patients were required to have protocol-defined bacteremia arising from S. aureus as described below.
Inclusion criteria were as follows. (i) Patients needed a true or probable diagnosis of S. aureus bacteremia based on blood cultures obtained within 2 days before enrollment. (ii) Patients needed to be at least 18 years old, weighing at least 37 kg (81 lb). Female patients of child-bearing potential (not surgically sterilized and between menarche and 1 year postmenopause) were to have a negative pregnancy test at the time of enrollment and were to have agreed to a reliable method of birth control during the study and for 12 months after the last dose of the study drug. (iii) The patient or his/her legally authorized representative was to have signed and dated an Institutional Review Board/Independent Ethics Committee-approved informed consent form.
Exclusion criteria were as follows: (i) having an underlying preexisting fatal illness(es) that, in the opinion of the investigator, would likely result in death within 14 days of enrollment; (ii) having been declared “Do not resuscitate”; (iii) having an anticipated need for more than 14 days of conventional therapy, including suspected or proven endocarditis, osteomyelitis, or meningitis; (iv) having received antibiotics active in the treatment of gram-positive infections for more than 48 h after initial positive blood cultures were drawn (a patient may have been enrolled if the pathogen manifested in vitro resistance to the antimicrobial agent that had been used before enrollment); (v) failure to remove an infected catheter or other infected device within the first 24 h of initiation of study drug therapy; (vi) having full-thickness burns with ≥30% body surface involvement; (vii) having polymicrobial bacteremia or known S. aureus bacteremia with intermediate sensitivity to vancomycin; (viii) having a history of hypersensitivity reactions to glycopeptides (patients who had a history of histamine-mediated type reactions, e.g., Red-Man syndrome, were not excluded); (ix) having recent local laboratory results indicating alanine transaminase or aspartate transaminase >4 times the upper limit of normal; (x) having had treatment with an investigational agent drug within the last 30 days of study entry; (xi) having previously received oritavancin; (xii) pregnant female patients or lactating female patients who were nursing and would not consent to cease nursing for at least 9 months; and (xiii) investigators and their immediate families.
Diagnostic criteria.
Patients were required to meet criteria for true or probable S. aureus bacteremia based on blood specimens obtained within 2 days before enrollment. True bacteremia was defined as one of the following: (i) growth of the same gram-positive bacteria from two blood cultures, (ii) growth of the same gram-positive bacteria from one blood culture and from another normally sterile site or body fluid, (iii) growth of the same gram-positive bacteria from one blood culture and from a tissue specimen demonstrating histologic evidence of tissue invasion, or (iv) growth of the same gram-positive bacteria from one blood culture and a quantitative or semiquantitative catheter tip culture (3, 6, 15). Probable bacteremia was defined as growth of gram-positive bacteria from one blood culture and clinical evidence of infection within 24 h of obtaining the blood culture specimen, defined by either (i) signs and symptoms of a local, presumed S. aureus infection, such as catheter tunnel infection or skin and skin-structure infection (e.g., tenderness and/or pain, erythema, swelling, purulent exudate within 2 cm of a catheter entry site), or (ii) a core (rectal, central catheter, or tympanic) temperature of ≥38°C (100.4°F) or <36°C (96.8°F) and at least one of the following conditions: (a) hypotension defined as a systolic blood pressure of <90 mm Hg or a reduction of >40 mm Hg from a prior reading; (b) a leukocyte count of >12,000 or <4,000 cells/mm3 or a differential count showing ≥10% band forms; (c) tachypnea, defined as a respiratory rate of >20 breaths/min or Pa CO2 of <32 mm Hg (<4.3 kPa); and/or (d) tachycardia, defined as a heart rate of >100 beats/min.
Drug dosage and administration.
Patients were randomly assigned to receive 10 to 14 days of either oritavancin or control treatment (vancomycin, cephalosporin, or another beta-lactam). Four intravenous dosing regimens of oritavancin (5.0, 6.5, 8.0, or 10.0 mg/kg of body weight/day) were completed sequentially. Oritavancin was infused (250 ml of 5% dextrose in water) intravenously every 24 h over 60 to 90 min (at a rate of ≤10.0 mg/kg/h). Dilution into volumes up to a maximum of 500 ml was permitted with infusion over 90 min; the oritavancin concentration was not to exceed 3 mg/ml. Slower infusion rates were permitted for patients with histamine-like reactions. No dose adjustment was required for subjects with renal impairment.
Evaluation of microbiological and clinical responses.
Microbiological and clinical responses were evaluated at the end-of-therapy visit, 5 to 8 days after the end of therapy (test-of-cure), and 35 to 49 days after starting therapy. Microbiological response was classified as follows: (i) eradication, which was defined as a blood culture negative for the original gram-positive blood pathogen(s) without previous initiation of a concomitant nonstudy systemic antibiotic having proven or presumed in vitro activity against the baseline pathogen; (ii) persistence, which was defined as a blood culture positive for the original gram-positive blood pathogen(s); or (iii) relapse, which was defined as a blood culture positive for the original gram-positive blood pathogen(s) at late follow-up, following a microbiological outcome of eradication at the test-of-cure visit.
Clinical response was classified as (i) a cure, which was defined as the resolution of all or some signs and symptoms attributed to the gram-positive bacteremia and no subsequent antibiotic or surgical treatment provided for the initial infection; (ii) failure, which was defined as persistence or worsening of original signs and symptoms, the emergence of new signs and symptoms, or evidence of metastatic infection attributed to the original gram-positive bacteremia without an initial response of cure; (iii) relapse, which was defined as the recurrence of signs or symptoms of the study condition or evidence of metastatic infection attributable to the original organism following a response of cure at the early follow-up visit; and (iv) indeterminate, which was defined as an inability to assign a clinical response, which may have included but was not limited to the following events: (i) treatment was initiated for a concurrent infection with an antibiotic having proven or presumed in vitro activity against the baseline gram-positive pathogen before the assessment was made or (ii) the patient died of a cause other than the gram-positive bacteremia.
Microbiological and clinical responses within the microbiologically evaluable population included in these analyses represented those assessed at the test-of-cure visit. Eradication or presumed eradication was considered a successful microbiological response. Persistence, presumed persistence, or relapse was considered an unsuccessful microbiological response. Cure was considered a successful clinical response. Failure or relapse was considered an unsuccessful clinical response. All patients with indeterminate microbiological and clinical responses were excluded from these analyses.
Population pharmacokinetic modeling.
The plasma sampling schedule for oritavancin included 15 time points: five on day 1 (0 min, within 5 min of end of infusion, and 2 to 5 h, 6 to 12 h, and 14 to 24 h postinfusion), two on day 4 or 5 (0min and within 5 min of end of infusion), five at end of therapy (0 min, within 5 min of end of infusion, and 2 to 5 h, 6 to 12 h, and 14 to 24 h postinfusion), two at early follow-up (end of treatment plus one sample between days 5 to 8), and one at late follow-up (day 42 ± 7 days). Actual collection times for each plasma sample were used for the pharmacokinetic analyses. Plasma concentrations were measured using liquid chromatography (LC)/mass spectrometry/mass spectrometry, which was validated for the analysis of oritavancin over a linear range of 0.75 to 2.5 μg/ml.
Plasma concentrations were analyzed using NONMEM, version 5, level 1.1 (San Francisco, CA). All data assembly, summary statistics, and graphical analyses were generated using SAS software, version 8.2 (Cary, NC). A previously developed three-compartment population pharmacokinetic model for oritavancin (apparent tissue distribution [α- and β-phase] and plasma-terminal [γ-phase] half-lives of 2.4, 18, and 360 h, respectively), based on a pooled data set from six phase 1, one phase 2, and one phase 3 study in patients with complicated skin and skin-structure infections (J. S. Owen, S. M. Bhavnani, J. Fiedler-Kelly, J. S. Loutit, S. B. Porter, and L. Phillips, Abstr. 44th Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-20, 2004), was applied to the plasma concentration data, without estimation of model parameters, to obtain empirical Bayesian parameter estimates and predicted drug concentrations. Model parameters included clearance (CL, in liters/h), intercompartmental clearance parameters (Q2 and Q3, in liters/h), and compartment volumes (V1, V2, and V3, in liters or liters/kg). Interindividual variability was modeled with exponential error models for CL, V1, Q2, and V2. Covariance was modeled between each pair of the parameters, CL, V1, and Q2. Two model parameters, Q3 and V3, were fixed to constant values estimated in the phase 1 data alone.
Covariate effects in the prior typical value models for CL, V1, and Q2 were characterized by equations 1 through 3:
 |
(1) |
 |
(2) |
 |
(3) |
where ADCT is the presence (ADCT = 1) or absence (ADCT = 0) of drug addiction, RC is the presence (RC = 1) or absence (RC = 0) of concomitant renal cation (e.g., ranitidine) administration, and WTKG is weight (kg).
Other prior model parameters included the following: V2 = 109 liters, Q3 = 0.577 liters/h, and V3 = 8.28 liters. Prior estimates of interindividual variability (IIV) included IIV CL = 35.21%CV, IIV V1 = 40.62%CV, IIV Q2 = 78.42%CV, and IIV V2 = 43.93%CV. Covariance (cov; r2) between parameters was estimated as cov (IIV CL, IIV V1) = 0.450, cov (IIV CL, IIV Q2) = 0.826, and cov (IIV V1, IIV Q2) = 0.464. Residual variability in the prior phase 1 data was estimated to be 16.09%CV and for the prior phase 2 and 3 data, 34.79%CV.
The adequacy of the fit of the prior model to the current data was confirmed both graphically and by computation of measures of bias and precision. If model predictions were found to be substantially biased or imprecise, the model parameters were reestimated and the bias and precision recomputed and evaluated.
Using Bayesian parameter estimates from the final population pharmacokinetic model, deterministic predictions of oritavancin concentrations (i.e., without a residual error component in the prediction) were used to generate the following exposure estimates and PK-PD measures following the first dose (day 1) for each patient: area under the concentration-time curve over a 24-h interval (AUC0-24), ratio of AUC0-24 to the minimum inhibitory value (MIC) of oritavancin to the S. aureus isolate at baseline (AUC0-24/MIC), percentage of the dosing interval duration for which concentrations were above the MIC (% time > MIC), percentage of the dosing interval duration for which free-drug concentrations were above the MIC (free-drug % time > MIC), maximum concentration (Cmax), and ratio of Cmax to the MIC of oritavancin to the S. aureus isolate at baseline (Cmax/MIC). Free concentrations of drug for free-drug % time > MIC were estimated as 10% of the total observed concentrations based on protein binding studies (R. A. Rowe and T. J. Brown, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-2193, 2001).
Pharmacokinetic-pharmacodynamic analysis.
Statistical analyses were performed using SAS software, version 8.2 (SAS Institute, Inc., Cary, NC). Classification and regression tree (CART) analysis was performed using S-Plus, version 6.0.1, release 1 (MathSoft, Inc, Seattle, WA).
Exploratory analyses of microbiological and clinical responses were conducted to identify relationships between response and independent variables of interest (PK-PD and exposure measures and certain patient characteristics including age, weight, and preexisting diabetes). CART analysis was performed to identify breakpoints within continuous independent variables (e.g., exposure and PK-PD measures) predictive of response. These results were used to group continuous measures into categories for subsequent evaluation in logistic regression analyses. Univariate and multivariable logistic regression analyses, with backward elimination (α = 0.05), were used to determine whether independent variables were statistically significant predictors of microbiological and clinical responses.
RESULTS
A total of 86 patients received oritavancin. Plasma concentrations from these patients (921) were included in the evaluation of pharmacokinetics. Given the increased magnitude of weighted residual values for observed versus predicted concentration data, compared to those seen in the earlier analysis (J. S. Owen, S. M. Bhavnani, J. Fiedler-Kelly, J. S. Loutit, S. B. Porter, and L. Phillips, Abstr. 44th Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-20, 2004), the previously developed three-compartment population pharmacokinetic model was reapplied and the parameter for residual variability of all phase 2 and 3 data was estimated. All other model parameters were fixed to their prior values. Residual variability, which was estimated to be 34.64%CV, was not substantially different from the estimate in the model development data set (34.79%CV). Goodness-of-fit plots for the model with estimation of residual error were not substantially changed from the plots of the base model with all parameters fixed.
Median measures of bias for the model that included estimation of residual error were 3.32% and 9.45% for individual and population mean predicted concentration values, respectively. Median measures of precision were 20.22% and 33.34%, respectively. Overall prediction errors were only slightly larger in this analysis than those in the previous analysis (median bias and precision values were 4.54% and 16.61%, respectively, for individual predicted concentration values and −15.11% and 27.53%, respectively, for population mean predicted concentration values). Based on these findings, the existing three-compartment model was considered adequate for prediction of concentrations in this patient population.
Potential relationships between patient covariates and pharmacokinetic parameters were explored graphically; these evaluations failed to reveal any new trends. Diagnostic plots evaluating the covariates included in the model indicated that the relationships described by the prior model were unbiased and appropriate for the current data set.
The mean apparent tissue distribution (α- and β-phase) and plasma-terminal (γ-phase) half-lives for oritavancin were 2.18, 17.6, and 404 h, respectively. The rank order of the rate constants was individually tested, and in each patient, α > β > γ.
A total of 55 patients with S. aureus bacteremia was evaluable for both microbiological and clinical responses and was included in these analyses. The mean (standard deviation [SD]) and median (range) ages of this group of patients were 58 (19) and 60 (19, 89) years, respectively. A summary of additional demographic characteristics for this group of patients can be found in Table 1. Approximately 47% of the patients had a catheter as the primary location of infection, 33% of infections originated from the blood, and 11% originated in the skin. Baseline MICs of oritavancin against S. aureus of 1, 2, and 4 μg/ml were observed for 4%, 80%, and 16% of patients, respectively. The mean (SD) AUC0-24/MIC, Cmax/MIC, % time > MIC, and free-drug % time > MIC on day 1 were 219.4 (136.5), 39.3 (17.9), 96.2 (10.7), and 28.2 (18.7), respectively. A total of 47 (85%) and 45 (78%) patients had successful microbiological and clinical responses, respectively. Six patients had discordant clinical and microbiological responses.
TABLE 1.
Demographic characteristics of the PK-PD efficacy analysis population (n = 55)
| Characteristic | % (n) |
|---|---|
| Gender (male) | 62 (34) |
| Ethnicity | |
| Asian | 13 (7) |
| Black | 4 (2) |
| Caucasian | 45 (25) |
| Hispanic | 38 (21) |
| Bacteremia diagnosis | |
| Probable | 15 (8) |
| True | 85 (47) |
| Location of primary infection | |
| Catheter (indwelling vascular) | 47 (26) |
| Blood (primary bacteremia or unknown) | 33 (18) |
| Skin | 11 (6) |
| Pleural | 3.5 (2) |
| Intra-abdominal (intestinal) | 2 (1) |
| Other | 3.5 (2) |
| Baseline S. aureus MIC (μg/ml) | |
| 1 | 4 (2) |
| 2 | 80 (44) |
| 4 | 16 (9) |
| Preexisting diabetes | 36 (20) |
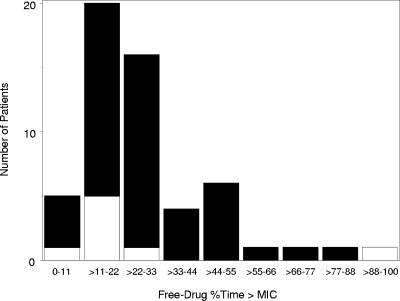
Summary statistics of exposure estimates and PK-PD measures stratified by microbiological response are provided in Table 2. Patients who had a successful microbiological response had higher median exposure and PK-PD measures (excluding % time > MIC) than patients who had microbiological failures. Figure 1 displays the frequency distributions of a free-drug % time > MIC on day 1, stratified by microbiological response. A greater proportion of microbiological failures was evident at lower ranges of a free-drug % time > MIC. Using CART, a breakpoint was identified for a free-drug % time > MIC at 22%. The probability of microbiological success was 93% for those patients with a free-drug % time > MIC greater than or equal to 22%. The probability of microbiological success was 76% for those patients with a free-drug % time > MIC below this threshold. A CART analysis using clinical response revealed the same breakpoint for a free-drug % time > MIC. The probability of clinical success was 87% for those patients with a free-drug % time > MIC greater than or equal to 22%. The probability of clinical success was 68% for those patients with a free-drug % time > MIC below this threshold.
TABLE 2.
Summary statistics of exposure estimates and PK-PD measures from the PK-PD efficacy analysis population, stratified by microbiological response
| Exposure or PK-PD measure | Microbiological response
|
||
|---|---|---|---|
| Success (n = 47) | Failure (n = 8)a | All patients (n = 55) | |
| AUC0-24 (μg · h/ml) | |||
| Mean (SD) | 454.48 (195.49) | 480.78 (408.29) | 458.30 (232.92) |
| Median (range) | 405.69 (144.54-883.27) | 337.13 (244.78-478.49) | 399.07 (144.54-1478.49) |
| AUC0-24/MIC | |||
| Mean (SD) | 219.69 (121.74) | 217.36 (215.06) | 219.35 (136.46) |
| Median (range) | 184.37 (72.27-655.26) | 150.05 (76.90-739.25) | 181.98 (72.27-739.25) |
| Cmax (μg/ml) | |||
| Mean (SD) | 82.13 (24.73) | 81.09 (39.13) | 81.98 (26.83) |
| Median (range) | 81.69 (38.87-130.20) | 71.07 (48.65-172.08) | 79.48 (38.87-172.08) |
| Cmax/MIC | |||
| Mean (SD) | 39.78 (17.21) | 36.31 (22.51) | 39.27 (17.87) |
| Median (range) | 38.86 (15.32-97.09) | 30.71 (15.25-86.04) | 37.94 (15.25-97.09) |
| % Time > MIC | |||
| Mean (SD) | 96.21 (11.04) | 96.35 (8.97) | 96.23 (10.69) |
| Median (range) | 99.58 (38.75-99.58) | 99.58 (74.17-99.58) | 99.58 (38.75-99.58) |
| Free-drug % time > MIC | |||
| Mean (SD) | 28.26 (16.74) | 28.02 (29.26) | 28.23 (18.70) |
| Median (range) | 23.75 (9.17-84.58) | 19.79 (8.75-99.17) | 23.33 (8.75-99.17) |
When contrasting patients with microbiological success versus failure, larger mean differences between the two groups with respect to exposure and PK-PD measures were observed when one patient, considered a medical outlier, was excluded. Although having the highest exposure and PK-PD measure (except for Cmax/MIC, which was the second highest), this patient was a microbiological failure. When excluded, the mean (SD) and median (range) free-drug % time > MIC were 17.86 (5.89) and 18.33 (8.75, 26.25), respectively, for patients with microbiological failure (n = 7).
FIG. 1.
Frequency distribution of free-drug % time > MIC stratified by microbiological response. Black solid bars represent microbiological successes, while white solid bars represent microbiological failures.
Due to the small number of patients with microbiological and clinical failures, exploratory analyses including a limited regression analysis were conducted. Univariate logistic regression models assessing the impact of oritavancin exposure and PK-PD measures (AUC0-24, Cmax, AUC0-24/MIC, Cmax/MIC, % time > MIC, and free-drug % time > MIC) and patient covariates (including age, weight, and preexisting diabetes) on the probability of microbiological and clinical responses were evaluated. A borderline statistically significant association between free-drug % time > MIC and microbiological response (odds ratio = 4.42, P = 0.09) was observed for this PK-PD measure, when defined categorically as <22% and ≥22% following CART analysis (Table 3). As shown in Table 4, the significance of this relationship increased (odds ratio = 8.84, P=0.05) after exclusion of one case considered to be a medical outlier.
TABLE 3.
Univariate logistic regression models for microbiological success from the PK-PD efficacy analysis population (n = 55)
| Parameter | Estimate | SE | Odds ratio | 95% CIe for odds ratio
|
P | |
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| AUC0-24 (μg · h/ml) | −0.0005 | 0.0016 | 1.00 | 0.996 | 1.00 | 0.77 |
| AUC0-24/MIC | 0.0001 | 0.0029 | 1.00 | 0.995 | 1.00 | 0.96 |
| Cmax (μg/ml) | 0.0015 | 0.0145 | 1.00 | 0.973 | 1.03 | 0.92 |
| Cmax/MIC | 0.0120 | 0.0235 | 1.01 | 0.967 | 1.06 | 0.61 |
| % Time > MIC (%) | −0.0014 | 0.0368 | 0.999 | 0.929 | 1.07 | 0.97 |
| Free-drug % time > MIC (%) | 0.0007 | 0.0208 | 1.00 | 0.961 | 1.04 | 0.97 |
| Free-drug % time > MIC ≥ 22%a | 0.743 | 0.434 | 4.42 | 0.805 | 24.3 | 0.09 |
| Preexisting diabetesb | −0.634 | 0.397 | 0.281 | 0.059 | 1.34 | 0.11 |
| Ideal body wtc (kg) | 0.743 | 0.434 | 4.42 | 0.805 | 24.3 | 0.09 |
| Wtd (kg) | — | — | — | — | — | — |
| Age (yr) | −0.0068 | 0.0207 | 0.993 | 0.954 | 1.03 | 0.74 |
Patients with a free-drug % time > MIC less than 22% were used as the reference category.
Patients with no preexisting diabetes were used as the reference category.
Ideal body weight was assessed as a categorical covariate with patients less than 56.6 kg as the reference category.
Weight could not be assessed as a continuous covariate due to failure to meet assumptions of linearity, nor was it evaluated as a categorical covariate due to small sample size.
CI, confidence interval.
TABLE 4.
Univariate logistic regression models for microbiological success from the PK-PD efficacy analysis population excluding one medical outlier (n = 54)
| Parameter | Estimate | SE | Odds ratio | 95% CIe for odds ratio
|
P | |
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| AUC0-24 (μg · h/ml) | 0.0043 | 0.0029 | 1.00 | 0.999 | 1.01 | 0.14 |
| AUC0-24/MIC | 0.0102 | 0.0065 | 1.01 | 0.998 | 1.02 | 0.12 |
| Cmax (μg/ml) | 0.0279 | 0.0198 | 1.03 | 0.989 | 1.07 | 0.16 |
| Cmax/MIC | 0.0529 | 0.0347 | 1.05 | 0.985 | 1.13 | 0.13 |
| % Time > MIC (%) | 0.0026 | 0.0365 | 1.00 | 0.933 | 1.08 | 0.94 |
| Free-drug % time > MIC (%) | 0.0796 | 0.0512 | 1.08 | 0.980 | 1.20 | 0.12 |
| Free-drug % time > MIC ≥ 22%a | 1.09 | 0.560 | 8.84 | 0.984 | 79.5 | 0.05 |
| Preexisting diabetesb | −0.523 | 0.413 | 0.352 | 0.070 | 1.77 | 0.21 |
| Ideal body wtc (kg) | 0.652 | 0.444 | 3.68 | 0.646 | 21.0 | 0.14 |
| Wtd (kg) | — | — | — | — | — | — |
| Age (yr) | −0.0091 | 0.0220 | 0.991 | 0.949 | 1.04 | 0.68 |
Patients with a free-drug % time > MIC less than 22% were used as the reference category.
Patients with no preexisting diabetes were used as the reference category.
Ideal body weight was assessed as a categorical covariate with patients less than 56.6 kg as the reference category.
Weight could not be assessed as a continuous covariate due to failure to meet assumptions of linearity, nor was it evaluated as a categorical covariate due to small sample size.
CI, confidence interval.
While the statistical significance of patient covariates changed only marginally based on the evaluation when this one patient was excluded (n = 54), large decreases in the P values associated with certain exposure and PK-PD measures were observed. P values for the AUC0-24/MIC ratio, Cmax/MIC ratio, and free-drug % time > MIC were 0.12, 0.13, and 0.12, respectively. In addition to similar and lower P values, a high degree of correlation was observed among these measures (Pearson correlation coefficient ≥ 0.8). These results were not surprising given that the case excluded was classified as both a microbiological and clinical failure and had the highest value for practically all exposure and PK-PD measures. This particular patient was considered a medical outlier due to the constellation of medical problems, many of which, together, likely impacted the probability of a successful microbiological or clinical response. The patient was a 54-year-old female with a medical history significant for morbid obesity (weight more than two times the ideal body weight), intravenous drug use, severe chronic obstructive pulmonary disease with sleep apnea, severe diabetes mellitus, hypertension with left ventricular hypertrophy/congestive heart failure, severe duodenal jejunal disease, and renal insufficiency. In addition, this patient was immunosuppressed due to high-dose corticosteroids.
When clinical response was assessed, a similar increase in the significance of the relationship between free-drug % time > MIC (<22% and ≥22%) and outcome was observed when the above-described outlier was excluded (from odds ratio = 3.06, P = 0.1, to odds ratio = 4.08, P = 0.06). Large decreases in the P values associated with certain other PK-PD measures were also observed. For example, P values for AUC0-24/MIC and Cmax/MIC ratios decreased from ≥0.79 to ≤0.30.
Due to the limited sample size and thus the inability to obtain precise and accurate parameter estimates, multivariable logistic regression models for microbiological and clinical responses were not evaluated.
DISCUSSION
An important initial step in the evaluation of exposure-response relationships for safety or efficacy is the characterization of pharmacokinetics. To this end, the development and application of population pharmacokinetic models for predicting drug exposure have proven to be very valuable when investigating exposure-response relationships (1, 7, 18; A. Forrest, C. R. Rayner, A. K. Meagher, M. C. Birmingham, and J. J. Schentag, Abstr. 40th Intersci. Conf. Antimicrob. Agents Chemother., abstr. 283, 2000). The assessment of oritavancin pharmacokinetics based on these phase 2 data from bacteremic patients was consistent with a previous evaluation based on data from normal volunteers and patients with skin and skin-structure infections (J. S. Owen, S. M. Bhavnani, J. Fiedler-Kelly, J. S. Loutit, S. B. Porter, and L. Phillips, Abstr. 44th Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-20, 2004). Both analyses demonstrated the multicompartmental character of the plasma concentration-time profile and linear pharmacokinetic properties of oritavancin. Plasma concentrations in patients with S. aureus bacteremia were well described by the previously developed three-compartment pharmacokinetic model. Mean tissue-distribution (α and β) and terminal (γ) half-lives were quite similar to those estimated in the prior analysis (2.2 versus 2.4, 18 versus 18, and 404 versus 360 h for α, β, and γ, respectively). The evaluation of this population pharmacokinetic model in the data set described herein provided an opportunity for its further validation based on data from a different population of patients.
The application of appropriate patient inclusion and exclusion criteria is a second important step when conducting PK-PD analyses. This is especially true for patients with bloodstream infections arising from different foci. The underlying assumption of such analyses is that the eradication of bacteremia is a suitable surrogate endpoint; however, the ability to detect an exposure-response relationship may be limited in a heterogeneous patient population which includes both primary bacteremia and tissue-based sites of infection. In the present analyses, the site of infection for the majority of patients was indwelling vascular catheter or blood. Additionally, patients with suspected or proven endocarditis, osteomyelitis, meningitis, or polymicrobial bacteremia were excluded from enrollment. Study drug was also discontinued if a patient was found to have evidence of preexisting endocarditis, osteomyelitis, or meningitis during therapy. Thus, given the exclusion criteria and population characteristics, the subset of patients in these analyses was a relatively homogeneous population, thus increasing the likelihood of detecting a potential exposure-response relationship for efficacy.
After exclusion of a patient deemed to be a medical outlier, these exposure-response analyses based on AUC0-24/MIC, Cmax/MIC, and free-drug % time > MIC revealed a borderline or statistically significant relationship with microbiological or clinical response. The lack of a relationship between response and % time > MIC was not surprising given that concentrations were above the MIC for 100% of the interval in most patients. It was only after free-drug concentrations were examined that a relationship between free-drug % time > MIC and response could be discerned. While the merits of routinely adjusting exposures for protein binding continue to be a focus of discussion, the findings of these analyses demonstrate the importance of examining free-drug exposures for agents such as oritavancin which demonstrate a high degree of protein binding (∼90%) (R. A. Rowe and T. J. Brown, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-2193, 2001).
A common factor that can hinder the detection of exposure-response relationships for efficacy is a narrow range of drug exposures, which typically results from the study of a fixed dosing regimen. In these analyses, the range of doses and associated exposures examined was broad (5 to 10 mg/kg/day resulting in AUC values of 144.5 to 1,478.5 μg · h/ml, respectively). Nonetheless, the limited sample size of the analysis data set likely contributed to the borderline significance of the exposure-response relationships for both microbiological and clinical responses and the CART-derived free-drug % time > MIC breakpoint, a conclusion further supported by the increased significance of these relationships after exclusion of a patient considered to be a medical outlier.
The validation of PK-PD targets derived from clinical data with those derived from nonclinical models of infection is an important ongoing effort in advancing the understanding of antimicrobial pharmacology. The findings of these analyses were concordant with a previous evaluation in a neutropenic-mouse thigh model of S. aureus infection (5). Boylan et al. demonstrated a strong association between the free-drug concentrations for both the Cmax/MIC ratio and % time > MIC of oritavancin and reduction in bacterial density (r2 = 0.93 and 0.84, respectively). Bacterial stasis was associated with a free-drug Cmax/MIC ratio of approximately 6 and free-drug % time > MIC targets of approximately 17 to 20%. Near-maximal effect (∼1 to 1.5 log reduction in bacterial density) was achieved for a free-drug Cmax/MIC ratio of approximately 14 and free-drug % time > MICs of approximately 42 to 50%. Unlike the results reported by Boylan et al. (5), free-drug % time > MIC was the PK-PD measure most strongly associated with efficacy in these analyses. Although less impressive, AUC0-24/MIC, when evaluated categorically (using CART), also demonstrated a borderline significant relationship with response (data not shown). Given the colinearity observed among these PK-PD measures, such findings were not unexpected. Just as found by Boylan et al. (5), the magnitude of free-drug % time > MIC associated with efficacy based on their work (∼20% for stasis) was consistent with the findings of our analyses (22%).
Gaining an understanding of PK-PD concepts for an investigational agent using nonclinical data and then “closing the loop” by investigating clinical data for exposure-response relationships is becoming an increasingly important milestone for selecting and confirming dose in drug development (4). A recent investigation by the Food and Drug Administration demonstrated that approximately 50% of clinical trials do not succeed, often due to poor dose selection. This pattern has prompted the agency to request sponsors to present exposure-response data to support a dose and/or dose ranges for further clinical study (9). These analyses of exposure-response for the efficacy of oritavancin in patients with bacteremia, which represent the first of such analyses, revealed a relationship between oritavancin exposure and microbiological response. The results of these analyses will be very useful to support the dose selection of oritavancin for future clinical trials for related indications.
Acknowledgments
We gratefully acknowledge Rick Pendleton for his contribution to data management and Patti Clark for her assistance in manuscript preparation. We also acknowledge Roxann Hanning, Lisa Morello, Susan Owen, and Bettina Sporkenbach, who were instrumental in the conducting of this study.
This study was supported by a grant from InterMune, Inc.
REFERENCES
- 1.Ambrose, P. G., D. M. Grasela, T. H. Grasela, J. Passarell, H. B. Mayer, and P. F. Pierce. 2001. Pharmacodynamics of fluoroquinolones against Streptococcus pneumoniae in patients with community-acquired respiratory tract infections. Antimicrob. Agents Chemother. 45:2793-2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banerjee, S. N., T. G. Emori, D. H. Culver, R. P. Gaynes, W. R. Jarvis, T. Horan, J. R. Edwards, J. Tolson, T. Henderson, W. J. Martone, and the National Nosocomial Infections Surveillance System. 1991. Secular trends in nosocomial primary bloodstream infections in the United States, 1980-1989. Am. J. Med. 91(3B):86S-89S. [DOI] [PubMed] [Google Scholar]
- 3.Bjornson, H. S., R. Colley, R. H. Bower, V. P. Duty, J. T. Schwartz-Fulton, and J. E. Fischer. 1982. Association between microorganism growth at the catheter insertion site and colonization of the catheter in patients receiving total parenteral nutrition. Surgery 92:720-727. [PubMed] [Google Scholar]
- 4.Bonapace, C. R. In vitro/animal models to support dosage selection: FDA perspective. IDSA/ISAP/FDA workshop, April 16, 2004. [Online.] http://www .fda.gov/cder/drug/antimicrobial/FDAIDSAISAPPresentations/Chuck%20 Bonapace.ppt.
- 5.Boylan, C. J., K. Campanale, P. W. Iversen, D. L. Phillips, M. L. Zeckel, and T. R. Parr, Jr. 2003. Pharmacodynamics of oritavancin (LY333328) in a neutropenic-mouse thigh model of Staphylococcus aureus infection. Antimicrob. Agents Chemother. 47:1700-1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cercenado, E., J. Ena, M. Rodriguez-Creixems, I. Romero, and E. Bouza. 1990. A conservative procedure for the diagnosis of catheter-related infections. Arch. Intern. Med. 50:1417-1420. [PubMed] [Google Scholar]
- 7.Forrest, A., D. E. Nix, C. H. Ballow, T. F. Goss, M. C. Birmingham, and J. J. Schentag. 1993. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob. Agents Chemother. 37:1073-1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lacy, M. K., W. Lu, X. Xu, P. R. Tessier, D. P. Nicolau, R. Quintiliani, and C. H. Nightingale. 1999. Pharmacodynamic comparisons of levofloxacin, ciprofloxacin, and ampicillin against Streptococcus pneumoniae in an in vitro model of infection. Antimicrob. Agents Chemother. 43:672-677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lesko, L. Proposal for end-of-phase 2A (EOP2A) meetings, FDA Advisory Committee for Pharmaceutical Science, Clinical Pharmacology Subcommittee, November 17, 2003. [Online.] http://www.fda.gov/ohrms/dockets/ac/03/slides/3998s1.htm.
- 10.Lister, P. D. 2002. Pharmacodynamics of gatifloxacin against Streptococcus pneumoniae in an in vitro pharmacokinetic model: impact of area under the curve/MIC ratios on eradication. Antimicrob. Agents Chemother. 46:69-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lister, P. D., and C. C. Sanders. 2001. Pharmacodynamics of moxifloxacin, levofloxacin, and sparfloxacin against Streptococcus pneumoniae in an in vitro pharmacodynamic model. J. Antimicrob. Chemother. 47:811-818. [DOI] [PubMed] [Google Scholar]
- 12.Lister, P. D., and C. C. Sanders. 1999. Pharmacodynamics of levofloxacin and ciprofloxacin against Streptococcus pneumoniae. J. Antimicrob. Chemother. 43:79-86. [DOI] [PubMed] [Google Scholar]
- 13.Madaras-Kelly, K. J., B. E. Ostergaard, L. B. Hovde, and J. C. Rotschafer. 1996. Twenty-four-hour area under the concentration-time curve/MIC ratio as a generic predictor of fluoroquinolone antimicrobial effect by using three strains of Pseudomonas aeruginosa and an in vitro pharmacodynamic model. Antimicrob. Agents Chemother. 40:627-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madaras-Kelly, K. J., A. J. Larsson, and J. C. Rotschafer. 1996. A pharmacodynamic evaluation of ciprofloxacin and ofloxacin against two strains of Pseudomonas aeruginosa. J. Antimicrob. Chemother. 37:703-710. [DOI] [PubMed] [Google Scholar]
- 15.Maki, D. G., C. E. Weise, and H. W. Sarafin. 1977. A semi-quantitative culture method for identifying intravenous catheter-related infection. N. Engl. J. Med. 296:1305-1309. [DOI] [PubMed] [Google Scholar]
- 16.Pinner, R. W., S. M. Teutsch, L. Simonsen, and L. A. Klug. 1996. Trends in infectious diseases mortality in the United States. JAMA 275:189-193. [PubMed] [Google Scholar]
- 17.Pittet, D., D. Tarara, and R. P. Wenzel. 1994. Nosocomial bloodstream infection in critically ill patients. Excess length of stay, extra costs, and attributable mortality. JAMA 275:1598-1601. [DOI] [PubMed] [Google Scholar]
- 18.Preston, S. L., G. L. Drusano, A. L. Berman, C. L. Fowler, A. T. Chow, B. Dornseif, V. Reichl, J. Natarajan, and M. Corrado. 1998. Pharmacodynamics of levofloxacin: a new paradigm for early clinical trials. JAMA 279:125-129. [DOI] [PubMed] [Google Scholar]