Abstract
Agar dilution was used, and MICs of metronidazole, tizoxanide, nitazoxanide, denitrotizoxanide, RM 4803, RM 4807, RM 4809, RM 4819, amoxicillin-clavulanate, and clindamycin were measured against 412 anaerobes. Nitazoxanide, tizoxanide, RM 4807, and RM 4809 were active against all groups, except for gram-positive non-spore-forming rods with 50% minimum inhibitory concentrations (when the latter were excluded) of 1 to 2 μg/ml and 90% minimum inhibitory concentrations of 4 to 8 μg/ml, respectively. Metronidazole MICs were usually lower against all groups except clostridia.
Metronidazole, a member of the imidazole group, has been in clinical use for many decades in treatment of anaerobic infections caused by all groups except the gram-positive non-spore-formers (which are in truth usually microaerophilic), amebiasis, and giardiasis (8). Metronidazole is also widely used in treatment of pseudomembranous colitis (1, 5), notwithstanding reported high relapse rates (1, 11). Metronidazole has a black box warning (carcinogenic in mice and rats), problems with drug interactions (warfarin, phenytoin, phenobarbital, cimetidine, and lithium), and significant side effects, including nausea, peripheral neuropathy, leukopenia, seizures, antabuse effect, metallic taste, furry tongue, and vaginal candidiasis.
The thiazolide group of antimicrobials has been known for many years. Nitazoxanide (the first in the class thiazolide) (2, 4) is moderately absorbed, with 33% of the drug eliminated in the urine and 67% in the feces. These compounds have a wider spectrum of activity than metronidazole, including against anaerobic bacteria but also against Helicobacter pylori. Recent studies have also shown them to be active against all intestinal protozoa, including Cryptosporidium spp. (2, 4, 6, 10).
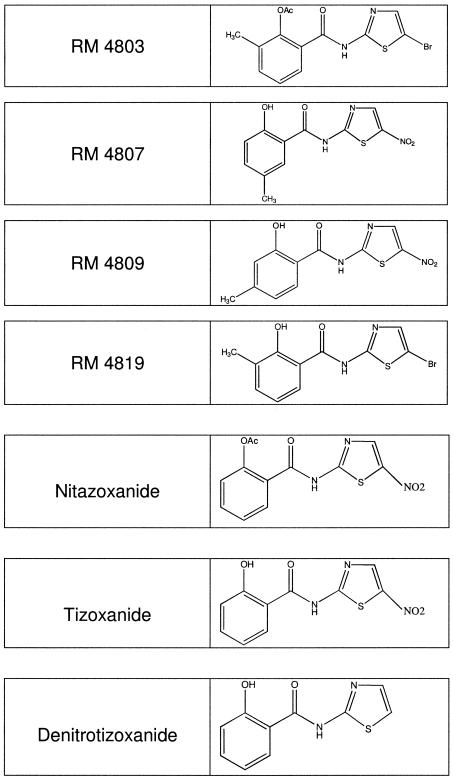
Nitazoxanide (2, 4) is approved for the treatment of diarrhea caused by Giardia lamblia and Cryptosporidium parvum in patients 1 year of age and older. This study compares the in vitro activity of nitazoxanide to those of tizoxanide (the primary metabolite of nitazoxanide) and five other thiazolides (denitrotizoxanide, RM 4803, RM 4807, RM 4809, and RM 4819) (Fig. 1) to those of amoxicillin-clavulanate, clindamycin, and metronidazole against 412 anaerobes.
FIG. 1.
Chemical structure of the seven thiazolides.
All seven thiazolides were obtained from Romark Laboratories, Tampa, Fla., and other drugs were from respective manufacturers. Solubility in water of the seven thiazolides was <0.1%. All seven thiazolides were dissolved in dimethyl sulfoxide (DMSO) and then further diluted to the appropriate concentration. The final concentration of DMSO in agar dilution plates was ≤0.5%. Three control plates containing 0.5% DMSO were included with each test run to ensure their growth matched that of the growth control medium plates without antibiotic. Clavulanate was combined with amoxicillin in a 1:2 ratio.
All anaerobes were clinical strains isolated between 2002 and 2005 from specimens such as wounds, pus, blood, and properly taken lower respiratory tract and female genital tract infections. Strains (including Clostridium difficile) were isolated from four different medical centers and, as far as we could ascertain, all represented different clones. Strains were identified by standard procedures (7) and kept frozen in double-strength skim milk (dehydrated skim milk; Difco Laboratories, Detroit, Mich.) at −70°C until use. Agar dilution susceptibility testing was according to the latest method recommended by the CLSI (formerly the National Committee for Clinical Laboratory Standards) (9), using enriched brucella agar supplemented with 5 μg/ml hemin, 1 μg/ml vitamin K1, and 5% (vol/vol) laked sheep blood. Prior to testing, strains were subcultured twice onto enriched brucella agar plates (9). The direct colony suspension method was used to prepare inoculum for agar dilution testing. Plates were incubated for 48 h in an anaerobic glove box (Coy Laboratory Products, Ann Arbor, Mich.). Quality control strains Bacteroides fragilis ATCC 25285, B. thetaiotamicron ATCC 29741, and Eubacterium lentum 43055 were included; results were in range (where ranges were available) (9) and are listed in Table 1.
TABLE 1.
MIC ranges (in micrograms/milliliter) for quality control strains
| Drug | B. fragilis ATCC 25285 | B. thetaiotaomicron ATCC 29741 | E. lentum ATCC 43055 |
|---|---|---|---|
| Metronidazole | 0.25-0.5 | 1.0-2.0 | 0.25-0.5 |
| Tizoxanide | 2.0-4.0 | 2.0 | 0.5-1.0 |
| Nitazoxanide | 2.0-4.0 | 2.0-4.0 | 1.0-2.0 |
| Denitrotizoxanide | >32 | >32 | >32 |
| RM 4803 | >32 | >32 | >32 |
| RM 4807 | 2.0-4.0 | 1.0-4.0 | 1.0 |
| RM 4809 | 4.0 | 2.0-4.0 | 0.5-2.0 |
| RM 4819 | >32 | >32 | >32 |
| Amoxicillin-clavulanate | 0.25-1.0 | 0.5-1.0 | 0.5-1.0 |
| Clindamycin | 1.0-2.0 | 4.0 | 0.12-0.25 |
Results of MIC testing are presented in Table 2. As can be seen, nitazoxanide, tizoxanide, RM 4807, and RM 4809 were all equally potent against all anaerobe groups except for gram-positive non-spore-forming rods (which are, in reality, mostly microaerophils) (8). Against the B. fragilis group, all 4 active agents had MICs between 0.12 and 4 μg/ml. By contrast, MICs were higher against Prevotella bivia, P. disiens, P. intermedia, P. buccalis, and P. corporis (0.5 to 16 μg/ml) than P. melaninogenica (0.12 to 0.5 μg/ml) and other prevotellas (0.12 to 4 μg/ml) as well as Porphyromonas spp. (0.03 to 2 μg/ml). All four compounds were more potent against Fusobacterium nucleatum and F. necrophorum (0.06 to 2.0 μg/ml) than against F. mortiferum and F. varium (0.5 to 16 μg/ml). All four drugs were active against anaerobic gram-positive (0.12 to 2.0 μg/ml) and gram-negative cocci (2.0 to 8.0). Potency against all groups of anaerobic gram-positive non-spore-forming rods except for Eubacterium spp. (MICs of all 4 drugs against all 14 strains tested were 0.5 to 1 μg/ml) was low. All four compounds were equally active against clostridia, with lower MICs (0.015 to 0.5 μg/ml) against the 10 C. difficile strains tested.
TABLE 2.
MICs (in micrograms/milliliter) of compounds
| Strain (no. of isolates) and drug | MIC range | MIC50 | MIC90 | Strain (no. of isolates) and drug | MIC range | MIC50 | MIC90 | |
|---|---|---|---|---|---|---|---|---|
| Bacteroides fragilis (50) | RM 4819 | >32 | >32 | |||||
| Metronidazole | 0.12-2.0 | 1.0 | 2.0 | Amoxicillin-clavulanate | 0.5-2.0 | 0.5 | ||
| Tizoxanide | 1.0-4.0 | 2.0 | 4.0 | Clindamycin | 4.0->32 | 16 | ||
| Nitazoxanide | 1.0-4.0 | 4.0 | 4.0 | |||||
| Denitrotizoxanide | >32 | >32 | >32 | Bacteroides uniformis (6) | ||||
| RM 4803 | >32 | >32 | >32 | Metronidazole | 0.5-1.0 | 0.5 | ||
| RM 4807 | 1.0-4.0 | 4.0 | 4.0 | Tizoxanide | 0.25-2.0 | 1.0 | ||
| RM 4809 | 1.0-4.0 | 4.0 | 4.0 | Nitazoxanide | 0.5-2.0 | 1.0 | ||
| RM 4819 | >32 | >32 | >32 | Denitrotizoxanide | >32 | >32 | ||
| Amoxicillin-clavulanate | 0.25-4.0 | 0.5 | 2.0 | RM 4803 | >32 | >32 | ||
| Clindamycin | 0.03->32 | 1.0 | >32 | RM 4807 | 0.5-2.0 | 1.0 | ||
| RM 4809 | 1.0-2.0 | 1.0 | ||||||
| Bacteroides thetaiotaomicron (10) | RM 4819 | >32 | >32 | |||||
| Metronidazole | 1.0-2.0 | 1.0 | 2.0 | Amoxicillin-clavulanate | 0.5-16 | 1.0 | ||
| Tizoxanide | 1.0-2.0 | 1.0 | 2.0 | Clindamycin | 1.0->32 | 2.0 | ||
| Nitazoxanide | 1.0-2.0 | 2.0 | 2.0 | |||||
| Denitrotizoxanide | >32 | >32 | >32 | Bacteroides fragilis group (101) | ||||
| RM 4803 | >32 | >32 | >32 | Metronidazole | ≤0.125-2.0 | 1.0 | 2.0 | |
| RM 4807 | 1.0-2.0 | 1.0 | 2 | Tizoxanide | 0.12-4.0 | 2.0 | 4.0 | |
| RM 4809 | 2.0-4.0 | 2.0 | 2 | Nitazoxanide | 0.12-4.0 | 2.0 | 4.0 | |
| RM 4819 | >32 | >32 | >32 | Denitrotizoxanide | >32 | >32 | >32 | |
| Amoxicillin-clavulanate | 0.5-8.0 | 1.0 | 4 | RM 4803 | >32 | >32 | >32 | |
| Clindamycin | 2.0->32 | 4.0 | >32 | RM 4807 | 0.25-4.0 | 2.0 | 4.0 | |
| RM 4809 | 0.25-4.0 | 4.0 | 4.0 | |||||
| Bacteroides distasonis (11) | RM 4819 | >32 | >32 | >32 | ||||
| Metronidazole | 0.5-2.0 | 1.0 | 2.0 | Amoxicillin-clavulanate | 0.25-32 | 1.0 | 4.0 | |
| Tizoxanide | 2.0-4.0 | 2.0 | 2.0 | Clindamycin | ≤0.015->32 | 1.0 | >32 | |
| Nitazoxanide | 2.0-4.0 | 2.0 | 4.0 | |||||
| Denitrotizoxanide | >32 | >32 | >32 | Prevotella bivia (16) | ||||
| RM 4803 | >32 | >32 | >32 | Metronidazole | 1.0-4.0 | 2.0 | 4.0 | |
| RM 4807 | 2.0-4.0 | 4.0 | 4.0 | Tizoxanide | 1.0-8.0 | 4.0 | 8.0 | |
| RM 4809 | 2.0-4.0 | 4.0 | 4.0 | Nitazoxanide | 1.0-8.0 | 4.0 | 8.0 | |
| RM 4819 | >32 | >32 | >32 | Denitrotizoxanide | >32 | >32 | >32 | |
| Amoxicillin-clavulanate | 1.0-32 | 2.0 | 4.0 | RM 4803 | >32 | >32 | >32 | |
| Clindamycin | 0.03->32 | 8.0 | 32 | RM 4807 | 1.0-8.0 | 4.0 | 8.0 | |
| RM 4809 | 1.0-8.0 | 2.0 | 4.0 | |||||
| Bacteroides vulgatus (10) | RM 4819 | >32 | >32 | >32 | ||||
| Metronidazole | ≤0.12-1.0 | 1.0 | 1.0 | Amoxicillin-clavulanate | 0.06-4.0 | 1.0 | 4.0 | |
| Tizoxanide | 0.12-2.0 | 1.0 | 2.0 | Clindamycin | ≤0.015->32 | ≤0.015 | >32 | |
| Nitazoxanide | 0.12-2.0 | 1.0 | 2.0 | |||||
| Denitrotizoxanide | >32 | >32 | >32 | Prevotella disiens (7) | ||||
| RM 4803 | >32 | >32 | >32 | Metronidazole | 0.5-2.0 | 1.0 | ||
| RM 4807 | 0.25-4.0 | 2.0 | 2.0 | Tizoxanide | 1.0-16 | 8.0 | ||
| RM 4809 | 0.25-4.0 | 2.0 | 4.0 | Nitazoxanide | 1.0-16 | 8.0 | ||
| RM 4819 | >32 | >32 | >32 | Denitrotizoxanide | >32 | >32 | ||
| Amoxicillin-clavulanate | 0.25-8.0 | 1.0 | 8.0 | RM 4803 | >32 | >32 | ||
| Clindamycin | ≤0.015->32 | 0.03 | 1.0 | RM 4807 | 2.0-16 | 4.0 | ||
| RM 4809 | 1.0-16 | 4.0 | ||||||
| Bacteroides ovatus (9) | RM 4819 | >32 | >32 | |||||
| Metronidazole | 0.25-2.0 | 2.0 | Amoxicillin-clavulanate | 0.03-2.0 | 0.25 | |||
| Tizoxanide | 1.0-4.0 | 2.0 | Clindamycin | ≤0.015-0.06 | ≤0.015 | |||
| Nitazoxanide | 1.0-2.0 | 2.0 | ||||||
| Denitrotizoxanide | >32 | >32 | Prevotella intermedia (9) | |||||
| RM 4803 | >32 | >32 | Metronidazole | ≤0.12-1.0 | 0.25 | |||
| RM 4807 | 1.0-2.0 | 2.0 | Tizoxanide | 2.0-16 | 4.0 | |||
| RM 4809 | 2.0-4.0 | 4.0 | Nitazoxanide | 2.0-16 | 4.0 | |||
| RM 4819 | >32 | >32 | Denitrotizoxanide | >32 | >32 | |||
| Amoxicillin-clavulanate | 0.5-2.0 | 0.5 | RM 4803 | >32 | >32 | |||
| Clindamycin | 1.0->32 | 2.0 | RM 4807 | 2.0-8.0 | 4.0 | |||
| RM 4809 | 1.0-8.0 | 4.0 | ||||||
| Bacteroides stercoris (5) | RM 4819 | >32 | >32 | |||||
| Metronidazole | 1.0-2.0 | 1.0 | Amoxicillin-clavulanate | 0.015-0.5 | 0.03 | |||
| Tizoxanide | 1.0-4.0 | 2.0 | Clindamycin | ≤0.015 | ≤0.015 | |||
| Nitazoxanide | 1.0-4.0 | 2.0 | ||||||
| Denitrotizoxanide | >32 | >32 | Prevotella melaninogenica (16) | |||||
| RM 4803 | >32 | >32 | Metronidazole | ≤0.12-1.0 | 0.5 | 1.0 | ||
| RM 4807 | 1.0-2.0 | 2.0 | Tizoxanide | 0.12-0.5 | 0.25 | 0.5 | ||
| RM 4809 | 1.0-4.0 | 2.0 | Nitazoxanide | 0.12-0.5 | 0.25 | 0.25 | ||
| Denitrotizoxanide | >32 | >32 | >32 | Porphyromonas asaccharolytica (4) | ||||
| RM 4803 | 16->32 | >32 | >32 | Metronidazole | ≤0.12-2.0 | |||
| RM 4807 | 0.12-0.5 | 0.5 | 0.5 | Tizoxanide | 0.06-2.0 | |||
| RM 4809 | 0.12-0.5 | 0.25 | 0.5 | Nitazoxanide | 0.12-2.0 | |||
| RM 4819 | >32 | >32 | >32 | Denitrotizoxanide | >32 | |||
| Amoxicillin-clavulanate | 0.06-2.0 | 0.25 | 2.0 | RM 4803 | >32 | |||
| Clindamycin | ≤0.015-0.12 | ≤0.015 | 0.06 | RM 4807 | 0.06-0.5 | |||
| RM 4809 | 0.12-0.5 | |||||||
| Prevotella buccalis (14) | RM 4819 | >32 | ||||||
| Metronidazole | 0.5-2.0 | 1.0 | 2.0 | Amoxicillin-clavulanate | ≤0.008-0.015 | |||
| Tizoxanide | 4.0-8.0 | 4.0 | 8.0 | Clindamycin | ≤0.015->32 | |||
| Nitazoxanide | 4.0-8.0 | 4.0 | 8.0 | |||||
| Denitrotizoxanide | >32 | >32 | >32 | Porphyromonas gingivalis (3) | ||||
| RM 4803 | >32 | >32 | >32 | Metronidazole | ≤0.125 | |||
| RM 4807 | 2.0-8.0 | 4.0 | 8.0 | Tizoxanide | 0.03-0.06 | |||
| RM 4809 | 2.0-8.0 | 4.0 | 8.0 | Nitazoxanide | 0.03-0.06 | |||
| RM4819 | >32 | >32 | >32 | Denitrotizoxanide | >32 | |||
| Amoxicillin-clavulanate | 0.015-2.0 | 0.06 | 0.5 | RM 4803 | >32 | |||
| Clindamycin | 0.015-0.03 | ≤0.015 | ≤0.015 | RM 4807 | 0.06-0.12 | |||
| RM 4809 | 0.03-0.06 | |||||||
| Prevotella corporis (9) | RM 4819 | >32 | ||||||
| Metronidazole | ≤0.12-2.0 | 0.5 | Amoxicillin-clavulanate | 0.015-0.06 | ||||
| Tizoxanide | 0.5-16 | 2.0 | Clindamycin | ≤0.015 | ||||
| Nitazoxanide | 0.5-16 | 4.0 | ||||||
| Denitrotizoxanide | >32 | >32 | Prevotella and Porphyromonas (94) | |||||
| RM 4803 | >32 | >32 | Metronidazole | ≤0.12-4.0 | 0.5 | 2.0 | ||
| RM 4807 | 2-16 | 4.0 | Tizoxanide | 0.03-16 | 2.0 | 8.0 | ||
| RM 4809 | 1-16 | 4.0 | Nitazoxanide | 0.03-16 | 2.0 | 8.0 | ||
| RM 4819 | >32 | >32 | Denitrotizoxanide | >32 | >32 | >32 | ||
| Amoxicillin-clavulanate | 0.03-0.5 | 0.06 | RM 4803 | 16->32 | >32 | >32 | ||
| Clindamycin | ≤0.015 | ≤0.015 | RM 4807 | 0.06-16 | 4.0 | 8.0 | ||
| RM 4809 | 0.03-16 | 2.0 | 8.0 | |||||
| Prevotella loescheii (5) | RM 4819 | >32 | >32 | >32 | ||||
| Metronidazole | 0.25-0.5 | 0.5 | Amoxicillin-clavulanate | ≤0.008-4.0 | 0.12 | 2.0 | ||
| Tizoxanide | 0.12-0.5 | 0.25 | Clindamycin | ≤0.015->32 | ≤0.015 | 0.12 | ||
| Nitazoxanide | 0.12-0.5 | 0.25 | ||||||
| Denitrotizoxanide | >32 | >32 | Fusobacterium nucleatum (16) | |||||
| RM 4803 | >32 | >32 | Metronidazole | ≤0.12-0.5 | ≤0.12 | 0.25 | ||
| RM 4807 | 0.12-1.0 | 0.5 | Tizoxanide | 0.06-0.5 | 0.25 | 0.5 | ||
| RM 4809 | 0.12-0.5 | 0.25 | Nitazoxanide | 0.06-1.0 | 0.25 | 1.0 | ||
| RM 4819 | >32 | >32 | Denitrotizoxanide | >32 | >32 | >32 | ||
| Amoxicillin-clavulanate | 0.03-0.25 | 0.25 | RM 4803 | 32->32 | >32 | >32 | ||
| Clindamycin | ≤0.015 | ≤0.015 | RM 4807 | 0.12-2.0 | 0.5 | 1.0 | ||
| RM 4809 | 0.06-1.0 | 0.25 | 0.5 | |||||
| Prevotella oralis group (2) | RM 4819 | >32 | >32 | >32 | ||||
| Metronidazole | 0.5-1.0 | Amoxicillin-clavulanate | ≤0.008-1.0 | 0.12 | 0.5 | |||
| Tizoxanide | 0.25-0.5 | Clindamycin | ≤0.015-0.12 | 0.06 | 0.12 | |||
| Nitazoxanide | 0.5 | |||||||
| Denitrotizoxanide | >32 | Fusobacterium necrophorum (14) | ||||||
| RM 4803 | >32 | Metronidazole | ≤0.12-0.5 | ≤0.12 | 0.25 | |||
| RM 4807 | 0.5-1.0 | Tizoxanide | 0.12-0.5 | 0.25 | 0.5 | |||
| RM 4809 | 0.25-1.0 | Nitazoxanide | 0.12-0.5 | 0.25 | 0.5 | |||
| RM 4819 | >32 | Denitrotizoxanide | >32 | >32 | >32 | |||
| Amoxicillin-clavulanate | 0.06-0.5 | RM 4803 | 32->32 | >32 | >32 | |||
| Clindamycin | ≤0.015 | RM 4807 | 0.12-1.0 | 0.25 | 0.5 | |||
| RM 4809 | 0.06-1.0 | 0.25 | 0.5 | |||||
| Prevotella oris (9) | RM 4819 | >32 | 0.03 | >32 | ||||
| Metronidazole | 0.125-1.0 | 0.5 | Amoxicillin-clavulanate | ≤0.008-0.25 | 0.03 | 0.06 | ||
| Tizoxanide | 0.125-2.0 | 1.0 | Clindamycin | ≤0.015-0.06 | ≤0.12 | 0.06 | ||
| Nitazoxanide | 0.125-4.0 | 1.0 | ||||||
| Denitrotizoxanide | >32 | >32 | Fusobacterium mortiferum (14) | |||||
| RM 4803 | >32 | >32 | Metronidazole | ≤0.12-0.5 | 0.25 | 0.5 | ||
| RM 4807 | 0.125-4.0 | 1.0 | Tizoxanide | 0.5-4.0 | 2.0 | 2.0 | ||
| RM 4809 | 0.125-2.0 | 1.0 | Nitazoxanide | 1.0-4.0 | 2.0 | 4.0 | ||
| RM 4819 | >32 | >32 | Denitrotizoxanide | >32 | >32 | >32 | ||
| Amoxicillin-clavulanate | 0.015-0.5 | 0.03 | RM 4803 | >32 | >32 | >32 | ||
| Clindamycin | ≤0.015->32 | ≤0.015 | RM 4807 | 4.0-8.0 | 4.0 | 4.0 | ||
| RM 4809 | 2.0-4.0 | 4.0 | 4.0 | Tizoxanide | 0.25-1.0 | 0.5 | ||
| RM 4819 | >32 | >32 | >32 | Nitazoxanide | 0.25-2.0 | 0.5 | ||
| Amoxicillin-clavulanate | 0.5-32 | 1.0 | 32 | Denitrotizoxanide | >32 | >32 | ||
| Clindamycin | 0.06-0.5 | 0.12 | 0.12 | RM 4803 | >32 | >32 | ||
| RM 4807 | 0.25-1.0 | 1.0 | ||||||
| Fusobacterium varium (19) | RM 4809 | 0.5-1.0 | 0.5 | |||||
| Metronidazole | ≤0.12-0.5 | 0.25 | 0.5 | RM 4819 | >32 | >32 | ||
| Tizoxanide | 4.0-8.0 | 8.0 | 8.0 | Amoxicillin-clavulanate | ≤0.008-0.03 | 0.015 | ||
| Nitazoxanide | 4.0-16 | 8.0 | 16 | Clindamycin | 0.03->32 | 0.06 | ||
| Denitrotizoxanide | >32 | >32 | >32 | |||||
| RM 4803 | >32 | >32 | >32 | Peptostreptococcus prevotii (2) | ||||
| RM 4807 | 8.0-16 | 16 | 16 | Metronidazole | 1.0-2.0 | |||
| RM 4809 | 8.0-16 | 16 | 16 | Tizoxanide | 1.0 | |||
| RM 4819 | >32 | >32 | >32 | Nitazoxanide | 0.5-1.0 | |||
| Amoxicillin-clavulanate | 0.5-4.0 | 1.0 | 4.0 | Denitrotizoxanide | >32 | |||
| Clindamycin | 1.0-32 | 8.0 | 16 | RM 4803 | >32 | |||
| RM 4807 | 0.5-1.0 | |||||||
| Fusobacteria (63) | RM 4809 | 1.0 | ||||||
| Metronidazole | ≤0.12-0.5 | ≤0.12 | 0.5 | RM 4819 | >32 | |||
| Tizoxanide | 0.06-8.0 | 0.5 | 8.0 | Amoxicillin-clavulanate | 0.015-0.06 | |||
| Nitazoxanide | 0.06-16 | 1.0 | 8.0 | Clindamycin | 0.125-0.25 | |||
| Denitrotizoxanide | >32 | >32 | >32 | |||||
| RM 4803 | 32->32 | >32 | >32 | Peptostreptococcus tetradius (7) | ||||
| RM 4807 | 0.12-16 | 4.0 | 16 | Metronidazole | 1.0 | 1.0 | ||
| RM 4809 | 0.06-16 | 2.0 | 16 | Tizoxanide | 0.25-0.5 | 0.25 | ||
| RM 4819 | >32 | >32 | >32 | Nitazoxanide | 0.25-0.5 | 0.25 | ||
| Amoxicillin-clavulanate | ≤0.008-32 | 0.5 | 2 | Denitrotizoxanide | >32 | >32 | ||
| Clindamycin | ≤0.015-32 | 0.06 | 8 | RM 4803 | >32 | >32 | ||
| RM 4807 | 0.25-1.0 | 0.5 | ||||||
| Finegoldia magna (10) | RM 4809 | 0.25-0.5 | 0.5 | |||||
| Metronidazole | ≤0.12-1.0 | 0.5 | 0.5 | RM 4819 | >32 | >32 | ||
| Tizoxanide | 0.12-1.0 | 0.5 | 1.0 | Amoxicillin-clavulanate | ≤0.008-0.5 | 0.03 | ||
| Nitazoxanide | 0.12-1.0 | 0.5 | 1.0 | Clindamycin | 0.5-1.0 | 0.5 | ||
| Denitrotizoxanide | >32 | >32 | >32 | |||||
| RM 4803 | >32 | >32 | >32 | Actinomyces spp. (6) | ||||
| RM 4807 | 0.12-1.0 | 1.0 | 1.0 | Metronidazole | 1.0->16 | 16 | ||
| RM 4809 | 0.25-1.0 | 0.5 | 1.0 | Tizoxanide | 0.5-16 | 4.0 | ||
| RM 4819 | >32 | >32 | >32 | Nitazoxanide | 0.5-16 | 8.0 | ||
| Amoxicillin-clavulanate | 0.12-0.25 | 0.25 | 0.25 | Denitrotizoxanide | >32 | >32 | ||
| Clindamycin | 0.06->32 | 0.12 | 2.0 | RM 4803 | >32 | >32 | ||
| RM 4807 | 0.5-32 | 16 | ||||||
| Micromonas micros (8) | RM 4809 | 1.0-8.0 | 8.0 | |||||
| Metronidazole | ≤0.12-0.5 | 0.25 | RM 4819 | >32 | >32 | |||
| Tizoxanide | 0.12-0.5 | 0.25 | Amoxicillin-clavulanate | 0.12-1.0 | 0.25 | |||
| Nitazoxanide | 0.25-0.5 | 0.25 | Clindamycin | 0.015-4.0 | 0.06 | |||
| Denitrotizoxanide | >32 | >32 | ||||||
| RM 4803 | >32 | >32 | Bifidobacterium spp. (8) | |||||
| RM 4807 | 0.12-0.5 | 0.25 | Metronidazole | 8.0->16 | >16 | |||
| RM 4809 | 0.25-0.5 | 0.5 | Tizoxanide | 0.25->32 | 32 | |||
| RM 4819 | >32 | >32 | Nitazoxanide | 0.5->32 | 16 | |||
| Amoxicillin-clavulanate | 0.03-0.5 | 0.06 | Denitrotizoxanide | >32 | >32 | |||
| Clindamycin | 0.12-0.25 | 0.25 | RM 4803 | >32 | >32 | |||
| RM 4807 | 1.0->32 | >32 | ||||||
| Peptostreptococcus anaerobius (9) | RM 4809 | 0.5->32 | 32 | |||||
| Metronidazole | ≤0.12-1.0 | 0.5 | RM 4819 | >32 | >32 | |||
| Tizoxanide | 0.12-1.0 | 1.0 | Amoxicillin-clavulanate | 0.03-0.25 | 0.06 | |||
| Nitazoxanide | 0.5-1.0 | 1.0 | Clindamycin | ≤0.015->32 | 0.03 | |||
| Denitrotizoxanide | >32 | >32 | ||||||
| RM 4803 | >32 | >32 | Eubacterium lentum (14) | |||||
| RM 4807 | 0.5-2.0 | 1.0 | Metronidazole | 0.25-0.5 | 0.25 | 0.5 | ||
| RM 4809 | 0.25-2.0 | 1.0 | Tizoxanide | 0.5-1.0 | 0.5 | 1.0 | ||
| RM 4819 | >32 | >32 | Nitazoxanide | 0.5-1.0 | 0.5 | 1.0 | ||
| Amoxicillin-clavulanate | 0.03-32 | 0.25 | Denitrotizoxanide | >32 | >32 | >32 | ||
| Clindamycin | ≤0.015-0.5 | 0.03 | RM 4803 | >32 | >32 | >32 | ||
| RM 4807 | 0.5-1.0 | 1.0 | 1.0 | |||||
| Peptostreptococcus asaccharolyticus (7) | RM 4809 | 0.5-1.0 | 1.0 | 1.0 | ||||
| Metronidazole | ≤0.125-2.0 | 1.0 | RM 4819 | >32 | >32 | >32 | ||
| Amoxicillin-clavulanate | 0.25-2.0 | 1.0 | 1.0 | Denitrotizoxanide | >32 | >32 | >32 | |
| Clindamycin | 0.06-0.5 | 0.25 | 0.25 | RM 4803 | >32 | >32 | >32 | |
| RM 4807 | 0.06-0.5 | 0.06 | 0.25 | |||||
| Lactobacillus spp. (6) | RM 4809 | 0.06-0.25 | 0.12 | 0.12 | ||||
| Metronidazole | >16 | >16 | RM 4819 | >32 | >32 | >32 | ||
| Tizoxanide | >32 | >32 | Amoxicillin-clavulanate | 0.5-2.0 | 1.0 | 1.0 | ||
| Nitazoxanide | >32 | >32 | Clindamycin | 0.06->32 | 4.0 | >32 | ||
| Denitrotizoxanide | >32 | >32 | ||||||
| RM 4803 | >32 | >32 | Miscellaneous clostridiaa (29) | |||||
| RM 4807 | >32 | >32 | Metronidazole | ≤0.12-2.0 | 0.5 | 1.0 | ||
| RM 4809 | >32 | >32 | Tizoxanide | 0.12-4.0 | 1.0 | 4.0 | ||
| RM 4819 | >32 | >32 | Nitazoxanide | 0.12-8.0 | 1.0 | 4.0 | ||
| Amoxicillin-clavulanate | 1.0-2.0 | 1.0 | Denitrotizoxanide | >32 | >32 | >32 | ||
| Clindamycin | 0.5-4.0 | 0.5 | RM 4803 | >32 | >32 | >32 | ||
| RM 4807 | 0.25-4.0 | 1.0 | 4.0 | |||||
| Propionbacterium spp. (14) | RM 4809 | 0.25-8.0 | 1.0 | 8.0 | ||||
| Metronidazole | >16 | >16 | >16 | RM 4819 | >32 | >32 | >32 | |
| Tizoxanide | 16-32 | 32 | 32 | Amoxicillin-clavulanate | 0.03-1.0 | 0.25 | 0.5 | |
| Nitazoxanide | 16-32 | 32 | 32 | Clindamycin | 0.03->32 | 1.0 | 16 | |
| Denitrotizoxanide | >32 | >32 | >32 | |||||
| RM 4803 | >32 | >32 | >32 | Veillonella spp. (5) | ||||
| RM 4807 | 16->32 | 32 | 32 | Metronidazole | 0.25-2.0 | 0.25 | ||
| RM 4809 | 8.0-32 | 16 | 32 | Tizoxanide | 2.0-4.0 | 4.0 | ||
| RM 4819 | >32 | >32 | >32 | Nitazoxanide | 2.0-4.0 | 2.0 | ||
| Amoxicillin-clavulanate | 0.12-0.5 | 0.25 | 0.5 | Denitrotizoxanide | >32 | >32 | ||
| Clindamycin | 0.06 | 0.06 | 0.06 | RM 4803 | >32 | >32 | ||
| RM 4807 | 4.0-8.0 | 4.0 | ||||||
| Clostridium perfringens (19) | RM 4809 | 2.0-4.0 | 2.0 | |||||
| Metronidazole | 0.25-2.0 | 0.5 | 2.0 | RM 4819 | >32 | >32 | ||
| Tizoxanide | 0.25-2.0 | 1.0 | 2.0 | Amoxicillin-clavulanate | 0.06-4.0 | 0.25 | ||
| Nitazoxanide | 0.25-4.0 | 2.0 | 4.0 | Clindamycin | 0.03-0.06 | 0.06 | ||
| Denitrotizoxanide | >32 | >32 | >32 | |||||
| RM 4803 | >32 | >32 | >32 | All strains (412) | ||||
| RM 4807 | 0.5-8.0 | 4.0 | 4.0 | Metronidazole | ≤0.12->16 | 0.5 | 2.0 | |
| RM 4809 | 0.5-8.0 | 2.0 | 4.0 | Tizoxanide | 0.015->32 | 1.0 | 8.0 | |
| RM 4819 | >32 | >32 | >32 | Nitazoxanide | 0.015->32 | 2.0 | 8.0 | |
| Amoxicillin-clavulanate | 0.015-0.12 | 0.03 | 0.12 | Denitrotizoxanide | >32 | >32 | >32 | |
| Clindamycin | 0.06->32 | 0.5 | 2.0 | RM 4803 | 16->32 | >32 | >32 | |
| RM 4807 | 0.06->32 | 2.0 | 16 | |||||
| Clostridium difficile (10) | RM 4809 | 0.03->32 | 2.0 | 16 | ||||
| Metronidazole | 0.12-0.25 | 0.25 | 0.25 | RM 4819 | >32 | >32 | >32 | |
| Tizoxanide | 0.015-0.5 | 0.06 | 0.12 | Amoxicillin-clavulanate | ≤0.008-32 | 0.5 | 2.0 | |
| Nitazoxanide | 0.015-0.25 | 0.06 | 0.12 | Clindamycin | ≤0.015->32 | 0.12 | 16 |
Species and number of isolates tested: Clostridium cadaveris, 3; Clostridium bifermentans, 1; Clostridium clostridioforme, 1; Clostridium hastiforme, 1; Clostridium innocuum, 1; Clostridium ramosum, 4; Clostridium sordellii, 2; Clostridium spp., 11; and Clostridium tertium, 5.
When metronidazole MICs are compared and contrasted with those of the above four active thiazolides, it can be seen that metronidazole MICs were usually 1 to 2 dilutions lower for the Bacteroides fragilis group and between 1 and >3 dilutions lower against most Prevotella spp. (notably Prevotella disiens, Prevotella intermedia, and Prevotella corporis). Metronidazole MICs were similar to those of the active thiazolides against Fusobacterium nucleatum and Fusobacterium necrophorum but were lower against Fusobacterium varium and Fusobacterium mortiferum. MICs were similar against gram-positive anaerobic cocci and Clostridium perfringens, but the active thiazolides had lower MICs than metronidazole against the 10 Clostridium difficile strains tested.
By contrast, denitrotizoxanide, RM 4803, and RM 4819 (all three compounds with the nitro moiety missing or replaced with bromide) were without significant activity against any anaerobe group. Amoxicillin-clavulanate was active against all anaerobe groups. Clindamycin resistance occurred in the B. fragilis group and clostridia, while metronidazole was potent against all strains except (similar to the active thiazolides) gram-positive non-spore-forming rods. MICs for the four active thiazolides appeared to be higher against non-Bacteroides fragilis group gram-negative anaerobes than against members of the Bacteroides fragilis group. We have no explanation for this phenomenon, which needs to be confirmed by testing of more freshly isolated strains. Strains other than gram-positive non-spore-forming rods with MICs that were >8 μg/ml for the four active thiazolides included 31 for nitazoxanide (16 Prevotella spp. isolates, 14 Fusobacterium varium isolates, and 1 Clostridium sp. isolate); 31 for tizoxanide (18 Prevotella spp. isolates and 13 Fusobacterium varium isolates), 37 for RM 4807 (15 Prevotella spp. isolates, 20 fusobacteria isolates [19 Fusobacterium varium isolates], 1 Clostridium perfringens isolate, and 1 Veillonella sp. isolate), and 35 for RM 4809 (12 Prevotella spp. isolates, 19 Fusobacterium varium isolates, and 4 clostridia isolates).
Nitazoxanide, tizoxanide, RM 4807, and RM 4809 are all members of the thiazolide group of antimicrobials with in vitro and in vivo activity against anaerobic microorganisms, including protozoa. A previous study published in 1996 by Dubreuil and coworkers (2) on the activity of nitazoxanide and tizoxanide against 241 strains of clinical anaerobic organisms showed that all strains were inhibited by nitazoxanide, with 90% minimum inhibitory concentrations (MIC90s) being between 0.06 and 4.0 μg/ml for all strains except for propionibacteria, for which the MIC90 was 16.0 μg/ml. The MIC90s of nitazoxanide were 0.5 μg/ml for the Bacteroides fragilis group (80 strains), 0.06 μg/ml for Clostridium difficile (21 strains), and 0.5 μg/ml for Clostridium perfringens (16 strains). Metronidazole had an activity level comparable to that of nitazoxanide except against Bifidobacterium species, against which it was poorly active, and propionibacteria, which were metronidazole resistant. Tizoxanide was less effective than nitazoxanide except against the Bacteroides fragilis group, against which its activity was similar to that of nitazoxanide. MICs reported in the previous study were generally lower for tizoxanide and nitazoxanide than those obtained in the current study. This could be due to the Wilkins-Chalgren agar plus 5% defibrinated blood which Dubreuil and coworkers used in their study (2) and also to the older organisms tested. Exact inocula used by the Dubreuil group are similar to those used in our study. Results for other compounds in the current study were as reported previously (3).
Results of this study suggest a potential place for nitazoxanide, tizoxanide, RM 4807, and RM 4809 in treatment of clostridial infections, especially pseudomembranous colitis caused by C. difficile toxin. More strains will need to be tested in order to validate this hypothesis, but our results against these organisms are similar to those reported by Dubreuil et al. (2) even given the older strains and different methodology employed. Pharmacokinetic/pharmacodynamic and additional experimental animal studies are necessary to further delineate the clinical role of these compounds in treatment of anaerobic infections.
Acknowledgments
This study was supported by a grant from Romark Laboratories, Tampa, FL.
REFERENCES
- 1.Bartlett, J. G. 1992. Antibiotic-associated diarrhea. Clin. Infect. Dis. 15:573-581. [DOI] [PubMed] [Google Scholar]
- 2.Dubreuil, L., I. Houck, Y. Mouton, and J. F. Rossini. 1996. In vitro evaluation of activities of nitazoxanide and tizoxanide against anaerobes and aerobic organisms. Antimicrobial. Agents Chemotherapy 40:2266-2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ednie, L. M., A. Rattan, M. R. Jacobs, and P. C. Appelbaum. 2003. Antianaerobic activity of RBX 7644 (ranbezolid), a new oxazolidinone, compared with those of eight other agents. Antimicrob. Agents Chemother. 47:1143-1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fox, L. M., and L. D. Saravolatz. 2005. Nitazoxanide: a new thiazolide antiparasitic agent. Clin. Infect. Dis. 40:1173-1180. [DOI] [PubMed] [Google Scholar]
- 5.Guerrant, R. L., J. M. Hughes, N. L. Lima, and J. Crane. 1990. Diarrhea in developed and developing countries: magnitude, special settings and etiologies. Rev. Infect. Dis. 12(Suppl. 1):S41-S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guttner, Y., H. M. Windsor, C. H. Viiala, L. Dusci, and B. J. Marshall. 2003. Nitazoxanide in treatment of Helicobacter pylori: a clinical and in vitro study. Antimicrob. Agents Chemother. 47:3780-3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jousimies-Somer, H. R., P. Summanen, D. M. Citron, E. J. Baron, H. M. Wexler, and S. M. Finegold. 2002. Wadsworth-KTL anaerobic bacteriology manual, 6th ed. Star Publishing Co., Belmont, Calif.
- 8.Murray, P. R., E. J. Baron, J. H. Jorgensen, M. A. Pfaller, and R. H. Yolken (ed.) 2003. Manual of clinical microbiology, 8th ed. American Society for Microbiology, Washington, D.C.
- 9.National Committee for Clinical Laboratory Standards. 2004. Methods for antimicrobial susceptibility testing of anaerobic bacteria-sixth edition; approved standard. NCCLS publication no. M11-A6. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 10.Pearson, R. D. 2004. Nitazoxanide as treatment of intestinal parasites in children. Curr. Infect. Dis. Rep. 6:25-26. [DOI] [PubMed] [Google Scholar]
- 11.Pépin, J., M.-E. Alary, L. Valiquette, E. Raiche, J. Ruel, K. Fulop, D. Godin, and C. Bourassa. 2005. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin. Infect. Dis. 40:1591-1597. [DOI] [PubMed] [Google Scholar]