Abstract
Pandoraea spp. are gram-negative, glucose nonfermenting rods detectable in blood cultures and sputa of cystic fibrosis patients. They are resistant to various antibiotic groups, with imipenem being the only active β-lactam. We isolated an imipenem-resistant (MIC, 64 μg/ml) Pandoraea pnomenusa strain from a cystic fibrosis patient. Cloning and sequencing identified two β-lactamases of Bush group 2d, namely, the known OXA-33, located on an integron, and the novel carbapenem-hydrolyzing oxacillinase OXA-62. OXA-62 is only distantly related to other oxacillinases (OXA-50 being closest with 43% amino acid identity). It hydrolyzes penicillins, oxacillin, imipenem, and meropenem but not expanded-spectrum cephalosporins. The blaOXA-62 gene is chromosome located. No transposable elements were found in its genetic neighborhood. With OXA-62-specific primers, blaOXA-62 could be identified in all P. pnomenusa strains and appears to be species specific. This additional mechanism of carbapenem resistance further complicates the treatment of infections caused by P. pnomenusa.
The genus Pandoraea was established by Coenye et al. in 2000 (6) as a result of reanalyzing strains not definitely identified to the species level which were phenotypically closest to Burkholderia cepacia, Ralstonia pickettii, or Ralstonia paucula. The genus Pandoraea includes five named species (Pandoraea apista, P. norimbergensis, P. pnomenusa, P. pulmonicola, and P. sputorum) and four unnamed genomospecies (9). Pandoraea sp. strains have been isolated from patients with septicemia and respiratory tract infections (mostly cystic fibrosis), as well as from food, water, and soil (6, 9, 14, 17, 21).
Antibiotic therapy of infections caused by Pandoraea spp. is impaired by their resistance to multiple antibiotics, including penicillins, cephalosporins, cefoxitin, meropenem, aminoglycosides, and chloramphenicol. Their resistance to fluoroquinolones is variable. Only tetracycline, trimethoprim-sulfamethoxazole, and imipenem were found to be active against the majority of isolates (9, 14, 17, 21). We recently cultured a P. pnomenusa strain from a cystic fibrosis patient. For this multiresistant strain, the MIC of imipenem was unusually high. A novel carbapenem-hydrolyzing oxacillinase, OXA-62, turned out to be involved in the mechanism of resistance to imipenem.
(Part of this work was presented at the 43rd Interscience Conference on Antimicrobial Agents and Chemotherapy [abstr. C1-666 and C2-2180].)
MATERIALS AND METHODS
Strains and plasmids.
The strains used in this study are characterized in Table 1. The Pandoraea spp. were isolated from sputa of cystic fibrosis patients between 1997 and 2004 in different centers in Germany, partly as Burkholderia spp. not identifiable to the species level. They were identified by phenotypic (API 20 NE [BioMérieux, Marcy l'Etoile, France] and additional biochemical tests) and genotypic methods (PCR with species-specific oligonucleotides) with Pandoraea sp. type strains obtained from the Laboratorium voor Microbiologie (Universiteit Ghent, Ghent, Belgium) bacterial collection as references. Escherichia coli C600 R− was the recipient strain in conjugation experiments. E. coli DH5α and the plasmid pBC (containing a chloramphenicol resistance gene; Stratagene) were used for cloning experiments.
TABLE 1.
Bacterial strains used in this study
| Organism | Designation | Source or description |
|---|---|---|
| P. pnomenusa | H4-1-1 | CFa sputum (Hannover, Germany) |
| P. pnomenusa | B-31 | CF sputum (Berlin, Germany) |
| P. pnomenusa | E126-13 | CF sputum (Essen, Germany) |
| P. pnomenusa | MUN 66-59 | CF sputum (Munich, Germany) |
| P. pnomenusa | PA 2228 | CF sputum (Passau, Germany) |
| P. pnomenusa | BUC | CF sputum (Magdeburg, Germany) |
| P. pnomenusa | GRO | CF sputum (Magdeburg, Germany) |
| P. pnomenusa | KRU | CF sputum (Magdeburg, Germany) |
| Pandoraea sp. | Va8523 | CF sputum (Frankfurt, Germany) |
| Pandoraea sp. | HD 7676 | CF sputum (Heidelberg, Germany) |
| P. apista | LMG 16407T | CF sputum (Denmark) |
| P. norimbergensis | LMG 18379T | Oxic water layer above a sulfide-containing sediment (Nürnberg, Germany) |
| P. pnomenusa | LMG 18087T | CF sputum (United Kingdom) |
| P. pulmonicola | LMG 18106T | CF sputum (Canada) |
| P. sputorum | LMG 18819T | CF sputum (United States) |
| E. coli C600 R− | Recipient strain for conjugation experiments | |
| E. coli DH5α | Host strain for cloning experiments | |
| E. coli DH5α | T1+ | Transformant harboring plasmid pT1 (vector pBC plus 5-kb insert) |
| E. coli DH5α | T6+ | Transformant harboring plasmid pT6 (vector pBC plus 2.6-kb insert) |
CF, cystic fibrosis patient.
Susceptibility testing.
The following antibiotics were obtained from the respective manufacturers: amoxicillin, Gruenenthal GmbH, Stolberg, Germany; ceftazidime, cefuroxime, clavulanate, and BRL 42715, GlaxoSmithKline GmbH & Co. KG, Munich, Germany; cefotaxime, Hoechst AG, Frankfurt/Main, Germany; cefepime and aztreonam, Bristol-Myers Squibb, Munich, Germany; cefoxitin and imipenem, Merck Sharp & Dohme, Munich, Germany; faropenem, Bayer AG, Wuppertal, Germany; meropenem, AstraZeneca GmbH, Plankstadt, Germany; nalidixic acid, reserpine, rifampin, and sodium azide, Sigma-Aldrich Chemie GmbH, Steinheim, Germany; piperacillin and tazobactam, Wyeth Pharma GmbH, Münster, Germany; chloramphenicol, Boehringer, Mannheim, Germany. The β-lactamase inhibitors clavulanate, tazobactam, and BRL 42715 (7, 16) were used at a fixed concentration of 4 μg/ml, and the efflux pump inhibitor reserpine was used at a fixed concentration of 20 μg/ml. MICs were determined by an agar dilution technique on Mueller-Hinton agar inoculated with 104 CFU/spot with a multipoint inoculator following Clinical and Laboratory Standards Institute (formerly National Institute for Clinical and Laboratory Standards) guidelines (18). E. coli ATCC 25922 was used as the MIC reference strain.
Conjugation.
Conjugation experiments with P. pnomenusa H4-1-1 as the donor strain and E. coli C600 R− as the recipient strain were performed as described previously (2). Selecting agents were amoxicillin (32 μg/ml), ceftazidime (2 μg/ml), imipenem (2 μg/ml), and meropenem (0.5 μg/ml). MacConkey agar was used to counterselect as P. pnomenusa H4-1-1 was resistant to rifampin, nalidixic acid, and sodium azide.
IEF and induction studies.
Sonication of strain suspensions and isoelectric focusing (IEF) were performed as previously described (3), except that suspensions of Pandoraea spp. were exposed to lysozyme (5 mg/ml; SERVA Electrophoresis GmbH, Heidelberg, Germany) for 1 h at 37°C prior to sonication. After focusing, the alkaline rim of the gel was neutralized by replacing the NaOH electrode strip with a strip soaked with 1 N HCl prior to visualization of the β-lactamase bands with nitrocefin. The hydrolytic activities of individual β-lactamase bands were assessed by a bioassay with two consecutive overlays. The first one, with 0.75% tryptic soy agar (TSA) containing the respective β-lactam, was followed, after 2 h of incubation at 35°C, by a second TSA overlay containing a susceptible indicator strain (1.2 × 107 CFU/ml). After overnight incubation at 35°C, growth of the indicator strain on the gel localized the β-lactamase band by which the β-lactam had been inactivated. For induction, an over night culture of P. pnomenusa H4-1-1 was diluted 1:20 and grown for 3 h on a shaker at 37°C. After addition of the potential inducer cefoxitin (64 μg/ml), clavulanate (64 μg/ml), or imipenem (16 μg/ml), the cultures were incubated for an additional 3 h.
Cloning and sequencing.
Cloning was performed as described previously (3). Whole-cell DNA of P. pnomenusa H4-1-1 was extracted with the GFX genomic DNA purification kit (Amersham Pharmacia Biotech), partially digested with Sau3AI or PstI, and ligated into BamHI- or PstI-digested pBC. The ligation product was transformed into E. coli DH5α made competent by the calcium chloride method. Transformants were selected on TSA containing amoxicillin (32 μg/ml) and chloramphenicol (16 μg/ml). Because of its large insert (>7kb), one recombinant plasmid was subjected to subcloning by partial Sau3AI digestion of the insert and ligation into pBC.
Sequencing was performed with consecutive primers by the dideoxy chain termination procedure with an automatic sequencer (ABI 3700). The nucleotide and deduced amino acid sequences were analyzed, and multiple alignments were performed with the DNAMAN 4.1 Software (Lynnon BioSoft).
Kinetic analysis.
Three liters of TSB containing 100-μg/ml amoxicillin was inoculated with E. coli transformant strain T6+ carrying the recombinant plasmid pT6 and shaken overnight at 37°C and 200 rpm. Cells were harvested by centrifugation, washed with 50 mM phosphate buffer (pH 7.0), and resuspended in 5 ml of the same buffer. Five freeze-thaw cycles on dry ice-ethanol were followed by centrifugation at 27,000 × g for 30 min. Several purification schemes were attempted, but OXA-62 did not behave as expected on either gel filtration or ion-exchange chromatography, and a pure preparation was not obtained. For partial purification of the OXA-62 β-lactamase, the supernatant was filtered, loaded onto a Sephacryl S-100 gel filtration column, and eluted with 50 mM phosphate buffer. All nitrocefin-hydrolyzing activity came out in the void volume. The two fractions with the highest nitrocefin-hydrolyzing activity were pooled, precipitated with 90% ammonium sulfate, and then resuspended and dialyzed in 25 mM Tris (pH 8.15)-200 mM K2SO4. Gel filtration on S-100 was repeated. Coomassie-stained polyacrylamide gel electrophoresis gel showed a purification of about 50% at this point. Initial hydrolysis rates were measured spectrophotometrically in 50 mM phosphate buffer containing 10 mM sodium bicarbonate at 25°C (22). Km and Vmax values were obtained with a Hanes plot.
PCR amplification of the oxacillinase gene.
With whole-cell DNA as the template and primers 5′-ACGCACGCAAACCTATCA-3′ and 5′-ATGTTGATCGCGACGCTG-3′ (based on the sequence of the cloned gene), PCR was carried out under the following conditions: 95°C for 1 min; 35 cycles of 95°C for 45 s, 57°C for 45 s, and 72°C for 45 s; and a final elongation step of 72°C for 10 min.
Nucleotide sequence accession number.
The nucleotide sequence of blaOXA-62 has been submitted to the GenBank database and has been assigned accession no. AY423074.
RESULTS AND DISCUSSION
Antibiotic resistance of P. pnomenusa H4-1-1.
P. pnomenusa H4-1-1 was resistant to all of the β-lactams tested (Table 2). Clavulanate and tazobactam reduced the MICs of the penicillins and ceftazidime only weakly. BRL 42715, an inhibitor of active-site serine β-lactamases, lowered the MIC of amoxicillin more than 16 times, that of imipenem 8 times, and that of meropenem 64 times but had no effect in combination with ceftazidime. Reserpine, an efflux pump inhibitor, did not change the MICs of ceftazidime and imipenem but reduced the MIC of meropenem 8 times. The combination of BRL 42715 and reserpine with imipenem or meropenem showed no superior activity compared to the combination with BRL 42715 alone. So the resistance of P. pnomenusa H4-1-1 to meropenem appeared to be the result of two mechanisms, namely, hydrolysis and extrusion by an efflux pump. Their proportion can be roughly estimated from inhibition of the enzymatic component by BRL 42715, which reduces the meropenem MIC from 1,024 to 16 μg/ml (a factor of 64), while inhibition of the efflux by reserpine reduces the MIC to 128 μg/ml (a factor of 8). The MIC of imipenem was reduced by BRL 42715 from 64 to 8 μg/ml (a factor of 8) but remained unchanged in combination with reserpine. The resistance to imipenem appeared to be the result of hydrolysis and possibly impaired expression of outer membrane proteins, while efflux seems not to be involved. No transconjugants could be produced in conjugation experiments.
TABLE 2.
Antibiotic susceptibilities of P. pnomenusa H4-1-1 and E. coli DH5α host and recombinant plasmid-harboring strains
| Compound(s)a | MIC (μg/ml) for:
|
|||
|---|---|---|---|---|
| P. pnomenusa H4-1-1 |
E. coli DH5α
|
|||
| pT1OXA-33 | pT6OXA-62 | Host strain | ||
| Amoxicillin | >512 | 128 | 256 | 4 |
| Plus CLA | >512 | 16 | 64 | 4 |
| Plus TZB | 512 | 32 | 64 | 4 |
| Plus BRL | 32 | 2 | 1 | 2 |
| Piperacillin | >512 | 16 | 16 | 1 |
| Plus TZB | >512 | 4 | 16 | 1 |
| Cefuroxime | 256 | 4 | 4 | 4 |
| Ceftazidime | 256 | 0.06 | 0.13 | 0.13 |
| Plus CLA | 256 | 0.06 | 0.13 | 0.13 |
| Plus BRL | 256 | 0.06 | 0.06 | 0.13 |
| Plus Res | 256 | 0.06 | 0.13 | 0.13 |
| Cefotaxime | 64 | 0.06 | 0.06 | 0.13 |
| Cefepime | 256 | 0.06 | 0.06 | 0.06 |
| Cefoxitin | >128 | 4 | 4 | 8 |
| Aztreonam | >256 | ≤0.06 | ≤0.06 | ≤0.06 |
| Faropenem | 256 | 0.5 | 2 | 0.5 |
| Imipenem | 64 | 0.25 | 0.25 | 0.25 |
| Plus BRL | 8 | 0.25 | 0.25 | 0.25 |
| Plus Res | 64 | 0.5 | 0.5 | 0.5 |
| Plus BRL and Res | 8 | ND | 0.5 | 0.5 |
| Meropenem | 1,024 | 0.03 | 0.13 | 0.03 |
| Plus BRL | 16 | 0.06 | 0.06 | 0.06 |
| Plus Res | 128 | 0.03 | 0.06 | 0.06 |
| Plus BRL and Res | 8 | ND | 0.03 | 0.03 |
Abbreviations: CLA, clavulanate; TZB, tazobactam; BRL, BRL 42715 (inhibits all active-site serine β-lactamases); Res, reserpine.
Isoelectric points.
In the crude homogenate of P. pnomenusa H4-1-1, three β-lactamases with pIs of 7.4, 8.0, and >9.0 were detected (Table 3). Only the β-lactamase with a pI of >9.0 hydrolyzed imipenem and meropenem in the bioassay.
TABLE 3.
Characteristics of Pandoraea sp. β-lactamases
| Organism | Strain designation | MIC (μg/ml)
|
pI(s) of β-lactamasea | Presence of OXA-62-specific PCR product (570 bp) | |
|---|---|---|---|---|---|
| IMIb | MERc | ||||
| P. pnomenusa | H4-1-1 | 64 | 1,024 | 7.4, 8.0, >9.0 | + |
| P. pnomenusa | B-31 | 16 | 1,024 | 8.0, >9.0 | + |
| P. pnomenusa | E126-13 | 4 | 128 | 6.5, >9.0 | + |
| P. pnomenusa | MUN 66-59 | 1 | 64 | 7.7, 8.0, >9.0 | + |
| P. pnomenusa | PA 2228 | 1 | 64 | 7.7, >9.0 | + |
| P. pnomenusa | BUC | 16 | 256 | 8.0, >9.0 | + |
| P. pnomenusa | GRO | 16 | 128 | 8.0, >9.0 | + |
| P. pnomenusa | KRU | 2 | 64 | 8.0, >9.0 | + |
| P. pnomenusa | LMG 18087T | 1 | 64 | 6.7, 7.7, >9.0 | + |
| Pandoraea sp. | Va8523 | 2 | 64 | 7.7, 8.9 | − |
| Pandoraea sp. | HD 7676 | 4 | 64 | 7.0, 7.5, 8.9 | − |
| P. apista | LMG 16407T | 2 | 32 | 7.4, 8.5 | − |
| P. norimbergensis | LMG 18379T | 2 | 128 | 8.8 | − |
| P. pulmonicola | LMG 18106T | 4 | 64 | 8.0, 8.4 | − |
| P. sputorum | LMG 18819T | 2 | 128 | 8.4, 8.8 | − |
The values for carbapenem-hydrolyzing β-lactamases identified by bioassay are in bold.
IMI, imipenem.
MER, meropenem.
Analysis of cloned genes and characterization of β-lactamases.
After ligation of partially digested genomic DNA of P. pnomenusa H4-1-1 into pBC and transformation into E. coli DH5α, we selected the amoxicillin-resistant transformants T1+ and T6+ harboring recombinant plasmids pT1 and pT6 with inserts of about 5.2 and 2.6 kb, respectively.
E. coli DH5α T1+ produced a single β-lactamase with a pI of 7.4, and for this strain, the MICs of amoxicillin and piperacillin, but not those of the carbapenems, were elevated (Table 2). MICs of the penicillins were reduced 4 to 8 times by clavulanate or tazobactam and 64 times by BRL 42715. Sequencing of the 5.2-kb insert of pT1 identified a class 1 integron similar to In40 and In111 (20, 23) containing four gene cassettes in its variable region: aac(6′)-Ib, aac(3)-Ia, qacF, and blaOXA-33 coding for the class D β-lactamase OXA-33.
E. coli DH5α T6+ produced a β-lactamase with a pI of >9.0, and for this strain, in comparison with those for the T− strain, the MICs of amoxicillin (64 times) and piperacillin (16 times) were elevated. Clavulanate and tazobactam reduced the MIC of amoxicillin from 256 to 64 μg/ml, and BRL 42715 reduced it from 256 to 1 μg/ml. No (imipenem) or only a slight increase (meropenem, faropenem) in the MICs of carbapenems were observed. However, in a bioassay following IEF, homogenates of this strain showed high hydrolytic activity for imipenem and meropenem comparable to that of the wild-type strain. Similar observations have been described for several oxacillinases (5, 12, 13).
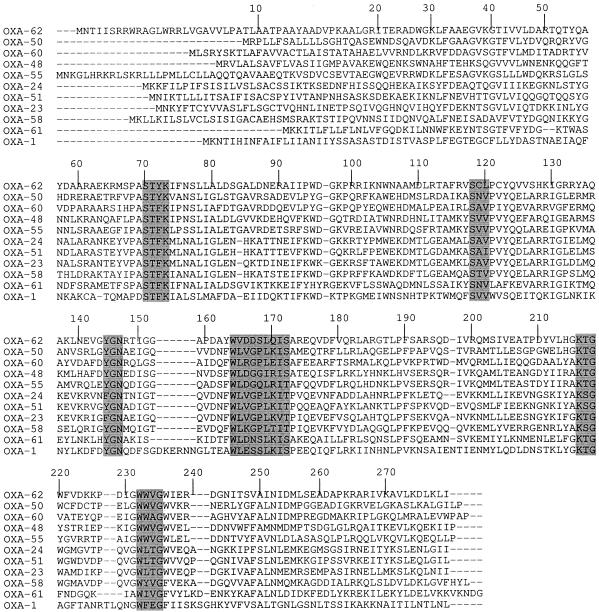
Sequencing of the insert of pT6 revealed an open reading frame (ORF) of 858 bp encoding a protein of 285 amino acids (Fig. 1). The protein showed, at positions 70 to 73 according to the class D β-lactamase (DBL) numbering system (8), an STYK tetrad representing the active site of serine β-lactamases. Among class D β-lactamases, the STYK motif has so far been described only for enzymes of the OXA-50 class D carbapenemase subgroup, while the STFK motif is the most common. Five structural elements characteristic of class D β-lactamases were identified (Fig. 1). Within the SXV motif (DBL positions 118 to 120), valine (V) was replaced by leucine (L), which was otherwise found only in β-lactamase mll0916 from Mesorhizobium loti (15). At positions 144 to 146, we found the YGN motif common to all oxacillinases except enzymes of the OXA-23 and OXA-24 carbapenemase subgroups, where it is replaced by FGN. This motif had recently been associated with the resistance to NaCl inhibition (12). At positions 164 to 172, the motif WXXXXLXIS was observed, as in most of the oxacillinases. The KTG motif (positions 216 to 218), necessary for function, was found as in the OXA-23, OXA-50, and OXA-60 subgroups, whereas it was replaced by KSG in the other two class D carbapenemase subgroups of OXA-24 and OXA-51. The motif WXXG at positions 232 to 235 was found as in all other oxacillinases.
FIG. 1.
Comparison of the amino acid sequence of OXA-62 with those of other carbapenem-hydrolyzing oxacillinases and that of OXA-1. GenBank accession numbers were obtained from www.lahey.org/studies/webt.htm. Conserved residues of oxacillinases are shaded. Numbering of β-lactamase amino acid positions is according to the DBL system (8).
Multiple alignment of protein sequences revealed no close relationship to any of the oxacillinases already known. The highest sequence similarities were found with enzymes of the OXA-50 subgroup (43.1 to 43.6%), class D carbapenemases produced by Pseudomonas aeruginosa (10), and with OXA-36 (41.4%), an oxacillinase closely related to OXA-2 found in P. aeruginosa (4).
We propose the designation OXA-62 for the novel oxacillinase. The full-length protein has a predicted molecular mass of 31.7 kDa. The G+C content of the ORF is 65.3%, which is close to the G+C content of Pandoraea spp. of 61.2 to 64.3% (6). In the genetic neighborhood of blaOXA-62, no transposable elements could be found. Sequencing of the regions up- and downstream of the OXA-62 gene revealed four further ORFs; BLAST searches with the ORFs alone (nucleotide and amino acid sequences) or the whole up- and downstream regions gave only scores of low homology for short sequences. The G+C content of the environment of blaOXA-62 is similar to that of the OXA-62 gene. These findings suggest a chromosomal location of the OXA-62 gene.
Biochemical properties of OXA-62.
After purification from E. coli DH5α harboring recombinant plasmid pT6, the purity of the β-lactamase OXA-62 was estimated as ∼50% by NuPAGE gels. There were at least eight other bands visible, and for this reason, we did not calculate kcat values. The kinetic parameters of OXA-62 obtained with the partially purified extract are shown in Table 4. The hydrolysis profile of OXA-62 includes penicillins and, to a lesser extent, carbapenems, cephaloridine, and cefoxitin, but not ticarcillin, ceftazidime, cefotaxime, and aztreonam. The rate of hydrolysis of oxacillin was higher than that of benzylpenicillin, which is characteristic for oxacillinases. However, most of the other carbapenem-hydrolyzing oxacillinases have weak or no oxacillin-hydrolyzing activity, except OXA-25, -26, and -55 (1, 13). OXA-62 showed Vmax values six times higher for ampicillin than for benzylpenicillin. However, because of its low affinity for ampicillin (Km, 160 μM), its hydrolytic efficiency is about the same as that for benzylpenicillin. The weak hydrolytic efficiency of OXA-62 for cephaloridine resulted from its very low affinity (Km, 3200 μM) for this substrate. OXA-62 showed weak hydrolysis of imipenem, as seen for most of the class D carbapenemases. In contrast to other carbapenem-hydrolyzing oxacillinases, for which hydrolysis of meropenem was less efficient than that of imipenem or even undetectable (like that for OXA-40 and OXA-60 [11, 12]), OXA-62 showed a hydrolytic efficiency two times higher for meropenem than for imipenem. Hydrolysis of the expanded-spectrum cephalosporins ceftazidime and cefotaxime, as well as aztreonam, was very weak, as seen for most of the OXA carbapenemases (1, 5, 10, 11, 12, 13, 19). OXA-62 hydrolyzed the cephamycin cefoxitin at low but measurable rates.
TABLE 4.
Kinetic parameters of partially purified β-lactamase OXA-62
| Substrate | Km (μM) | Vmax (nmol/min/mg) | Relative Vmaxa (%) | Vmax/Km ratio | Relative Vmax/Kma (%) |
|---|---|---|---|---|---|
| Benzylpenicillin | 28 ± 2.3 | 31 ± 0.8 | 100 | 1.1 | 100 |
| Cephaloridine | 3,200 ± 500 | 14 ± 2.0 | 44 | 0.004 | 0.36 |
| Ampicillin | 160 ± 2.1 | 190 ± 8.0 | 600 | 1.2 | 109 |
| Piperacillin | 13 ± 5.7 | 2.1 ± 0.14 | 6.8 | 0.16 | 14.5 |
| Oxacillin | 35 ± 5.5 | 67 ± 2.5 | 220 | 1.9 | 172 |
| Ticarcillinb | NDc | ≤0.31 | ≤1.0 | ND | ND |
| Imipenem | 13 ± 1.4 | 0.044 ± 0.0 | 0.14 | 0.003 | 0.27 |
| Meropenem | 8.0 ± 2.8 | 0.058 ± 0.0 | 0.18 | 0.007 | 0.64 |
| Cefoxitin | 68 ± 1.4 | 0.23 ± 0.016 | 0.74 | 0.003 | 0.27 |
| Ceftazidimeb | ND | ≤0.01 | ≤0.026 | ND | ND |
| Cefotaximeb | ND | ≤0.01 | ≤0.036 | ND | ND |
| Aztreonamb | ND | ≤0.50 | ≤1.6 | ND | ND |
The benzylpenicillin value was taken as 100%.
Vmax was estimated due to slow hydrolysis.
ND, not determined. Hydrolysis was too slow to determine the Km.
Hydrolysis of nitrocefin, indicated by a color change from yellow to red, by crude extracts of E. coli DH5α harboring the blaOXA-62 gene was significantly delayed when the β-lactamase-containing extract was incubated with 0.1 M NaCl (37°C, 10 min) prior to the addition to nitrocefin. This indicates that OXA-62 is inhibited by NaCl, as expected from the presence of the YGN motif at DBL positions 144 to 146. In contrast, pretreatment of the homogenates of E. coli DH5α T6+ with meropenem or imipenem (64 μg/ml) only slightly delayed the reaction while no effect was detectable in the presence of cefoxitin (64 μg/ml). These results indicate that OXA-62 is inhibited poorly by carbapenems and not at all by cephamycins. Crude homogenates of P. pnomenusa H4-1-1 obtained from cultures induced with cefoxitin, imipenem, or clavulanate showed slightly greater amounts of β-lactamase activity for OXA-62 in bioassays than the preparation from an uninduced culture.
Distribution of OXA-62 among Pandoraea spp.
All Pandoraea sp. strains were resistant to piperacillin, piperacillin-tazobactam, cefuroxime, ceftazidime, cefoxitin, aztreonam, and meropenem and intermediately resistant or resistant to cefotaxime (except one strain) and cefepime (data not shown). Four strains were resistant to imipenem (MIC, ≥16 μg/ml); all others were susceptible. Like P. pnomenusa H4-1-1, all Pandoraea sp. isolates were 8 to 64 times more resistant to meropenem than to imipenem, and 11 of the 15 strains were classified as imipenem sensitive and meropenem resistant (Table 3). This has been described by several authors (9, 14, 17, 21). Reduction of the MICs of imipenem (2 to 32 times) and meropenem (4 to 256 times) was achieved in combination with BRL 42715. All Pandoraea spp. harbored meropenem-hydrolyzing β-lactamases. However, only the β-lactamases of the P. pnomenusa isolates focused at a pI of >9.0, comigrating with OXA-62. The meropenem-hydrolyzing β-lactamases of the non-P. pnomenusa strains showed variable pIs between 7.5 and 8.9 (Table 3). With oligonucleotides derived from the sequence of the OXA-62 gene, a 570-bp fragment could be amplified from the whole-cell DNAs of all of the P. pnomenusa wild-type strains but not from those of the other Pandoraea spp. (Table 3). All Pandoraea spp. seemed to produce a meropenem-hydrolyzing oxacillinase, while OXA-62 appeared to be specific for the species P. pnomenusa.
The first carbapenem-hydrolyzing oxacillinase was described in 1993 in an A. baumannii strain isolated in 1985 (19). Since then, more than 25 class D carbapenemases have been found. They form at least six different homology groups with only low identity. Most of their genes were identified on the chromosome of A. baumannii isolates. Their origin is still unknown. Recently, gram-negative environmental species like R. pickettii, P. aeruginosa, Shewanella algae, and Shewanella oneidensis were found to be a natural reservoir of carbapenem-hydrolyzing oxacillinases (10, 11, 13).
OXA-62 of P. pnomenusa is a further carbapenem-hydrolyzing class D β-lactamase produced by a glucose-nonfermenting environmental species. It appears to be species specific and therefore helpful for identification of P. pnomenusa. With benzylpenicillin, amoxicillin, and oxacillin as preferred substrates, slow hydrolysis of carbapenems, and no activity against ceftazidime, cefotaxime, and aztreonam, the biochemical profile of OXA-62 resembles that of other class D carbapenemases (1, 5, 10, 11, 12, 13, 19). The β-lactamase OXA-62 contributes to the resistance of P. pnomenusa H4-1-1 to amoxicillin, imipenem, and meropenem. In addition, the presence of an efflux mechanism for meropenem could be shown. The presence of multiple mechanisms of carbapenem resistance further complicates the treatment of infections caused by P. pnomenusa.
REFERENCES
- 1.Afzal-Shah, M., N. Woodford, and D. M. Livermore. 2001. Characterization of OXA-25, OXA-26, and OXA-27, molecular class D β-lactamases associated with carbapenem resistance in clinical isolates of Acinetobacter baumannii. Antimicrob. Agents Chemother. 45:583-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bauernfeind, A., S. Wagner, R. Jungwirth, I. Schneider, and D. Meyer. 1997. A novel class C β-lactamase (FOX-2) in Escherichia coli conferring resistance to cephamycins. Antimicrob. Agents Chemother. 41:2041-2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauernfeind, A., I. Schneider, R. Jungwirth, H. Sahly, and U. Ullmann. 1999. A novel type of AmpC β-lactamase, ACC-1, produced by a Klebsiella pneumoniae causing nosocomial pneumonia. Antimicrob. Agents Chemother. 43:1924-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bert, F., C. Branger, and N. Lambert-Zechovsky. 2002. Identification of PSE and OXA β-lactamase genes in Pseudomonas aeruginosa using PCR-restriction fragment length polymorphism. J. Antimicrob. Chemother. 50:11-18. [DOI] [PubMed] [Google Scholar]
- 5.Bou, G., A. Oliver, and J. Martinez-Beltran. 2000. OXA-24, a novel class D β-lactamase with carbapenemase activity in an Acinetobacter baumannii clinical strain. Antimicrob. Agents Chemother. 44:1556-1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coenye, T., E. Falsen, B. Hoste, M. Ohlen, J. Goris, J. R. Govan, M. Gillis, and P. Vandamme. 2000. Description of Pandoraea gen. nov. with Pandoraea apista sp. nov., Pandoraea pulmonicola sp. nov., Pandoraea pnomenusa sp. nov., Pandoraea sputorum sp. nov. and Pandoraea norimbergensis comb. nov. Int. J. Syst. Evol. Microbiol. 50:887-899. [DOI] [PubMed] [Google Scholar]
- 7.Coleman, K., D. R. J. Griffin, J. W. J. Page, and P. A. Upshon. 1989. In vitro evaluation of BRL 42715, a novel β-lactamase inhibitor. Antimicrob. Agents Chemother. 33:1580-1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Couture, F., J. Lachapelle, and R. C. Levesque. 1992. Phylogeny of LCR-1 and OXA-5 with class A and class D β-lactamases. Mol. Microbiol. 6:1693-1705. [DOI] [PubMed] [Google Scholar]
- 9.Daneshvar, M. I., D. G. Hollis, A. G. Steigerwalt, A. M. Whitney, L. Spangler, M. P. Douglas, J. G. Jordan, J. P. MacGregor, B. C. Hill, F. C. Tenover, D. J. Brenner, and R. S. Weyant. 2001. Assignment of CDC weak oxidizer group 2 (WO-2) to the genus Pandoraea and characterization of three new Pandoraea genomospecies. J. Clin. Microbiol. 39:1819-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Girlich, D., T. Naas, and P. Nordmann. 2004. Biochemical characterization of the naturally occurring oxacillinase OXA-50 of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 48:2043-2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Girlich, D., T. Naas, and P. Nordmann. 2004. OXA-60, a chromosomal, inducible, and imipenem-hydrolyzing class D β-lactamase from Ralstonia pickettii. Antimicrob. Agents Chemother. 48:4217-4225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Héritier, C., L. Poirel, D. Aubert, and P. Nordmann. 2003. Genetic and functional analysis of the chromosome-encoded carbapenem-hydrolyzing oxacillinase OXA-40 of Acinetobacter baumannii. Antimicrob. Agents Chemother. 47:268-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Héritier, C., L. Poirel, and P. Nordmann. 2004. Genetic and biochemical characterization of a chromosome-encoded carbapenem-hydrolyzing Ambler class D β-lactamase from Shewanella algae. Antimicrob. Agents Chemother. 48:1670-1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson, L. N., J. Y. Han, S. M. Moskowitz, J. L. Burns, X. Qin, and J. A. Englund. 2004. Pandoraea bacteremia in a cystic fibrosis patient with associated systemic illness. Pediatr. Infect. Dis. J. 23:881-882. [DOI] [PubMed] [Google Scholar]
- 15.Kaneko, T., Y. Nakamura, S. Sato, E. Asamizu, T. Kato, S. Sasamoto, A. Watanabe, K. Idesawa, A. Ishikawa, K. Kawashima, T. Kimura, Y. Kishida, C. Kiyokawa, M. Kohara, M. Matsumoto, A. Matsuno, Y. Mochizuki, S. Nakayama, N. Nakazaki, S. Shimpo, M. Sugimoto, C. Takeuchi, M. Yamada, and S. Tabata. 2000. Complete genome structure of the nitrogen-fixing symbiotic bacterium Mesorhizobium loti. DNA Res. 7:331-338. [DOI] [PubMed] [Google Scholar]
- 16.Matagne, A., P. Ledent, D. Monnaie, A. Felici, M. Jamin, X. Raquet, M. Galleni, D. Klein, I. Francois, and J. M. Frere. 1995. Kinetic study of interaction between BRL 42715, β-lactamases, and d-alanyl-d-alanine peptidases. Antimicrob. Agents Chemother. 39:227-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moore, J. E., A. Reid, B. C. Millar, X. Jiru, J. Mccaughan, C. E. Goldsmith, J. Collins, P. G. Murphy, and J. S. Elborn. 2002. Pandoraea apista isolated from a patient with cystic fibrosis: problems associated with laboratory identification. Br. J. Biomed. Sci. 59:164-166. [DOI] [PubMed] [Google Scholar]
- 18.National Center for Clinical and Laboratory Standards. 2002. Performance standards for antimicrobial susceptibility testing, 12th informational supplement. M100-S12. National Center for Clinical and Laboratory Standards, Wayne, Pa.
- 19.Paton, R., R. S. Miles, J. Hood, and S. G. B. Amyes. 1993. ARI-1: β-lactamase-mediated imipenem resistance in Acinetobacter baumannii. Int. J. Antimicrob. Agents 2:81-88. [DOI] [PubMed] [Google Scholar]
- 20.Ploy, M. C., P. Courvalin, and T. Lambert. 1998. Characterization of In40 of Enterobacter aerogenes BM2688, a class 1 integron with two new gene cassettes, cmlA2 and qacF. Antimicrob. Agents Chemother. 42:2557-2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stryjewski, M. E., J. J. LiPuma, R. H. Messier, Jr., L. B. Reller, and B. D. Alexander. 2003. Sepsis, multiple organ failure, and death due to Pandoraea pnomenusa infection after lung transplantation. J. Clin. Microbiol. 41:2255-2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sykes, R. B., D. P. Bonner, K. Bush, and N. H. Georgopapadakou. 1982. Azthreonam (SQ 26,776), a synthetic monobactam specifically active against aerobic gram-negative bacteria. Antimicrob. Agents Chemother. 21:85-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vourli, S., L. S. Tzouvelekis, E. Tzelepi, E. Lebessi, N. J. Legakis, and V. Miriagou. 2003. Characterization of In111, a class 1 integron that carries the extended-spectrum β-lactamase gene blaIBC-1. FEMS Microbiol. Lett. 225:149-153. [DOI] [PubMed] [Google Scholar]