Abstract
We have monitored the in vitro sensitivities of Plasmodium falciparum isolates predeployment and during the deployment of artesunate plus amodiaquine treatment in Mlomp, Casamance (southwestern Senegal) during 2000 to 2004. Parasites remained susceptible to both drugs. Chloroquine resistance levels were high but stable. Quinine continues to be effective.
Parasite resistance to chloroquine (CQ) is widespread in sub-Saharan Africa. Artemisinin-based combinations (ACTs) are currently recommended instead for the treatment of uncomplicated falciparum malaria (13). In southern Senegal, in vitro and in vivo CQ resistance is established (9, 11), causing an excess burden (12). We compared in controlled trials CQ versus amodiaquine (AQ) (4) and also artesunate-amodiaquine (AS-AQ) versus AQ (1) in children in Mlomp (Casamance, southwestern Senegal). Subsequently, we deployed AS-AQ in 2000 for all age groups, first during the rainy seasons and then year-round (2). AS-AQ has been consistently efficacious and well-tolerated. With several countries scaling up the use of ACTs, it is important to know whether parasite sensitivity is affected by the widespread use of these drugs. Therefore, we monitored the in vitro susceptibility of local isolates to CQ, quinine (QN), artemisinin (ART), and the AQ metabolite monodesethylamodiaquine (MdAQ) using the DELI test (7) pre-ACT (1997) and during deployment (2000 to 2004).
Malaria is mesoendemic in Mlomp (25 infective bites/person-year). Malaria transmission occurs year-round, with a peak during the rainy season (July to December).
Isolates were collected at regular intervals pretreatment from consecutive subjects with a Plasmodium falciparum monoinfection and parasitemia of ≥0.2% (6) and used for the in vitro assay within 4 h. Methodology was as described by Brasseur et al. (3), except for 0.5% Albumax supplementation (Gibco BRL, Grand Island, NY) instead of human serum. Drug stock solutions were prepared in RPMI and serially diluted twofold to obtain final concentrations ranging from 14.6 to 3,750 nM (CQ), 14.4 to 3,692.3 nM (QN), 5.9 to 1,518.9 nM (MdAQ), and 1 to 532 nM (ART). Parasite growth in control and treated wells was measured as the optical density, reflecting the parasite lactic dehydrogenase level (7). Drug activity was expressed as the concentration of drug resulting in a 50% inhibition of parasite growth (IC50), as calculated from maximal OD values from test wells compared to control wells. The cutoff values of the IC50 for resistance were 100 nM (CQ), 500 nM (QN), 60 nM (MdAQ), and 15 nM (ART) (10).
IC50s were log transformed; analysis of variance was used to generate least squares means (LSM); geometric LSM (GLSM) were obtained by antilogarithm transformation of LSMs. The ratio of GLSM (with 95% confidence intervals [CIs]) was estimated between years for each treatment (it was concluded that there was no difference if the 95% CI of the comparison included 1.0). For each treatment, a generalized linear model (GLM) was estimated with year as the categorical factor, using 1997 as reference. Changes in the proportion of resistant isolates over time were explored by using the Cochran-Armitage test for trends. Statistical significance was at a P level of <0.05 (two-tailed).
IC50s were obtained for 242 (CQ), 236 (QN), 250 (MdAQ), and 183 subjects (ART). Different analyses concurred to show that CQ resistance was established but steady; IC50s were higher than in 1997 for QN but otherwise stable during 2000 to 2004, decreased for MdAQ, and were consistent for ART.
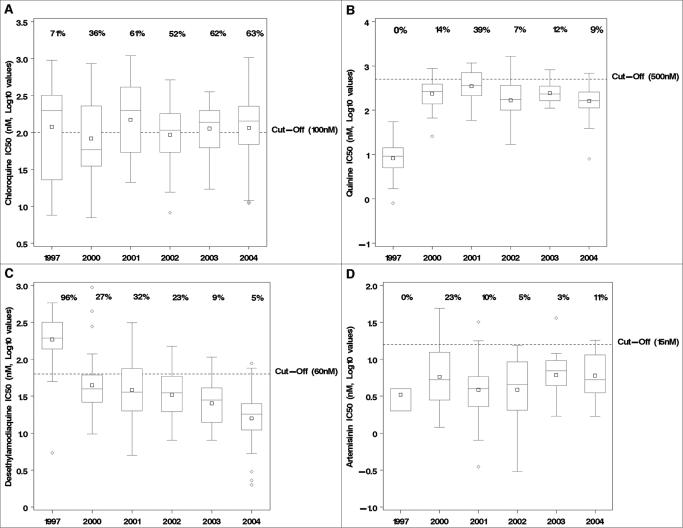
Figure 1a to d shows log-transformed IC50s. CQ values were stable (Fig. 1a), QN increased from 1997 to 2000 and then remained stable during 2000 to 2004 (Fig. 1b), MdAQ decreased during 1997 to 2004 (Fig. 1c), and ART showed discreet fluctuations over time (Fig. 1d).
FIG. 1.
Box plots of log-transformed IC50s (in nM) for chloroquine (a), quinine (b), monodesethyl amodiaquine (c), and artemisinin (d) by year (1997 and 2000 to 2004). The percentages of isolates above the cutoff value for in vitro resistance (dotted horizontal lines) are displayed for each drug. The top (or the base) of the whisker corresponds to the largest (or the lowest) observed value within the 1.5× interquartile range (IQ) from the 75th (or 25th) percentile. □, mean; ⋄, values outside 1.5× IQ.
GLSM and pair-wise GLSM ratios are reported in Tables 1 and 2. CQ values were constant, except 2000 versus 1997 and 2002 versus 2001. For QN, differences were statistically significant between 1997 and all years 2000 to 2004 (95% CIs of the ratios, >1; thus, IC50s increased versus 1997), with occasional differences between years. For MdAQ, differences were significant between 1997 and 2000 to 2004 (95% CIs, <1; IC50s decreased versus 1997) and sporadically between years (always decreasing with time). For ART, erratic differences were seen in either direction.
TABLE 1.
GLSM results
| Year | GLSM (95% CI)
|
|||
|---|---|---|---|---|
| Chloroquine | Quinine | Desethylamodiaquine | Artemisinin | |
| 1997 | 119.0 (86.7, 163.4) | 8.2 (6.8, 10.1) | 185.7 (151.1, 228.2) | 3.3 (2.2, 5.1) |
| 2000 | 82.6 (60.8, 112.4) | 238.2 (184.8, 306.9) | 44.5 (34.9, 56.6) | 5.8 (4.5, 7.5) |
| 2001 | 148.4 (108, 203.8) | 350.1 (275.1, 445.5) | 38.5 (30.0, 49.4) | 3.9 (3.0, 5.0) |
| 2002 | 93.3 (71.9, 121.0) | 168.4 (136.2, 208.2) | 33.1 (26.8, 40.8) | 3.9 (3.1, 4.8) |
| 2003 | 112.7 (83.3, 152.5) | 245.0 (194.6, 308.3) | 25.3 (20.0, 32.1) | 6.1 (4.8, 7.8) |
| 2004 | 115.0 (92.7, 142.7) | 162.2 (136.0, 193.5) | 15.9 (13.3, 18.9) | 6.0 (4.7, 7.6) |
TABLE 2.
GLSM ratios
| Reference year | Comparison year | GLSM ratioa (95% CI).
|
|||
|---|---|---|---|---|---|
| Chloroquine | Quinine | Desethylamodiaquine | Artemisinin | ||
| 1997 | 2000 | 0.7* (0.4, 0.9) | 28.9* (19.0, 38.7) | 0.2* (0.2, 0.3) | 1.8 (0.8, 2.7) |
| 2001 | 1.2 (0.8, 1.7) | 42.4* (27.5, 57.4) | 0.2* (0.1, 0.3) | 1.2 (0.5, 1.8) | |
| 2002 | 0.8 (0.5, 1.1) | 20.4* (14.3, 26.5) | 0.2* (0.1, 0.2) | 1.2 (0.5, 1.8) | |
| 2003 | 0.9 (0.6, 1.3) | 29.7* (19.7, 39.7) | 0.1* (0.1, 0.2) | 1.8 (0.8, 2.9) | |
| 2004 | 1 (0.6, 1.3) | 19.7* (13.9, 25.4) | 0.1* (0.1, 0.1) | 1.8 (0.8, 2.8) | |
| 2000 | 2001 | 1.8 (1.2, 2.4) | 1.5 (1.0, 2.0) | 0.9 (0.5, 1.2) | 0.7* (0.4, 0.9) |
| 2002 | 1.1 (0.7, 1.5) | 0.7* (0.5, 0.9) | 0.7 (0.5, 1.0) | 0.7* (0.4, 0.9) | |
| 2003 | 1.4 (0.9, 1.8) | 1 (0.7, 1.4) | 0.6* (0.4, 0.8) | 1.1 (0.7, 1.4) | |
| 2004 | 1.4 (0.9, 1.9) | 0.7* (0.4, 0.9) | 0.4* (0.2, 0.5) | 1 (0.7, 1.4) | |
| 2001 | 2002 | 0.6* (0.4, 0.8) | 0.5* (0.3, 0.7) | 0.9 (0.6, 1.2) | 1 (0.6, 1.3) |
| 2003 | 0.8 (0.5, 1.0) | 0.7* (0.5, 0.9) | 0.7* (0.4, 0.9) | 1.6* (1.0, 2.1) | |
| 2004 | 0.8 (0.5, 1.0) | 0.5* (0.3, 0.6) | 0.4* (0.3, 0.6) | 1.6* (1.0, 2.1) | |
| 2002 | 2003 | 1.2 (0.8, 1.6) | 1.5 (1.0, 1.9) | 0.8 (0.5, 1.0) | 1.6* (1.1, 2.1) |
| 2004 | 1.2 (0.9, 1.6) | 1 (0.7, 1.3) | 0.5* (0.3, 0.6) | 1.6 (1.0, 2.1) | |
| 2003 | 2004 | 1 (0.7, 1.4) | 0.7* (0.4, 0.9) | 0.6* (0.4, 0.8) | 1 (0.7, 1.3) |
Comparison year GLSM/reference year GLSM. *, statistically significant (P < 0.05) increase (GLSM ratio > 1) or decrease (GLSM ratio < 1) from reference year to comparison year.
The GLM confirmed the above results: Spearman correlation coefficients showed no relationship for CQ, a significant relationship for QN (positive estimates, P < 0.0001; r = 0.34) and AQ (negative estimates, P < 0.0001; r = −0.63), and limited fluctuation for ART (P = 0.03; r = 0.16).
The proportions of resistant isolates (IC50 > cutoff) are shown in Fig. 1a to d. The Cochran-Armitage trend test was nonsignificant for all drugs except MdAQ (significant decrease of resistant isolates over time [P < 0.0001]).
Some methodological issues of this study deserve further comment.
We used artemisinin (from which all artemisinin derivatives are synthesized) and monodesethylamodiaquine (AQ main metabolite); both are intrinsically less bioactive than artesunate (8) and AQ (5), respectively.
There are no well-established methodologies to analyze in vitro sensitivity data. To confidently classify a strain as resistant or sensitive requires validated thresholds; although we adopted predefined cutoff values (>2 standard deviations above the mean) (10), their clinical significance is doubtful, especially for ART and somewhat for MdAQ. In addition, comparison of IC50s, particularly trends over time, poses problems. We explored several approaches (including a Welch-adjusted analysis of variance or the nonparametric Kruskal-Wallis sign rank test as appropriate) and opted for presenting the GLSM ratios complemented with GLM. We are confident in the results presented, as all tests converge and point to the same conclusions.
In the past decade, QN (intramuscular twice a day for 3 days) has been preferred over failing CQ in this area (2). Attendance registries in Mlomp report a total of 6,642 first-line treatments of fevers with antimalarials during 1996 to 2000, 96% of which were consistently QN and 4% CQ. In 2000, we started using AS-AQ for parasitologically confirmed falciparum malaria. During the first 5 years of deployment, close to 2,800 treatments were delivered in Mlomp. In 2004 nearly all treatments of confirmed cases were AS-AQ, but QN use continues, particularly when a parasitological diagnosis cannot be made. AS-AQ has consistently been >90% parasitologically and clinically effective (2).
To date, the level of CQ in vitro resistance is stable (50 to 60%), and there is little resistance in vitro to QN, AQ, and ART. IC50s are decreasing for MdAQ and fluctuate for ART; it is too early to determine whether these changes have any clinical significance. These in vitro data are consistent with in vivo responses. Our data allow us to conclude that parasite sensitivities have not been adversely altered by this initial phase of deployment of AS-AQ. QN should still be used for severe malaria cases. The combination of geometric least square mean ratios (with 95% CIs) and the generalized linear model is useful for the analysis of in vitro sensitivity data.
Acknowledgments
This study was funded by grants from the French Ministry of Foreign Affairs (FAC 2000) and Ministry of Research (PAL+) and the UNICEF/UNDP/WB/WHO Special Programme for Research & Training in Tropical Diseases.
We thank W. R. J. Taylor and F. Derouin for assistance, and we thank the personnel and patients in Mlomp.
REFERENCES
- 1.Adjuik, M., P. Agnamey, A. Babiker, S. Borrmann, P. Brasseur, F. Cobelens, S. Diallo, J. F. Faucher, P. Garner, S. Gikunda, P. G. Kremsner, S. Krishna, B. Lell, M. Loolpapit, P. B. Matsiegui, M. A. Missinou, J. Mwanza, F. Ntoumi, P. Olliaro, P. Osimbo, P. Rezbach, M. Cisse, E. Some, and W. R. J. Taylor. 2002. Artesunate-amodiaquine versus amodiaquine for uncomplicated Plasmodium falciparum malaria in African children: a randomised, multicentre trial. Lancet 359:1365-1372. [DOI] [PubMed] [Google Scholar]
- 2.Agnamey, P., P. Brasseur, M. Cissé, O. Gaye, J. Dumoulin, J. Rigal, W. R. J. Taylor, and P. Olliaro. 2005. Economic evaluation of a policy change from single-agent treatment for suspected malaria to artesunate-amodiaquine for microscopically confirmed uncomplicated falciparum malaria in the Oussouye district of southwestern Senegal. Trop. Med. Int. Health 10:926-933. [DOI] [PubMed] [Google Scholar]
- 3.Brasseur, P., P. Druilhe, J. Kouamouo, O. Brandicourt, M. Danis, and S. R. Moyou. 1986. High level of sensitivity to choloroquine of 72 Plasmodium falciparum isolates from southern Cameroon in January 1985. Am. J. Trop. Med. Hyg. 35:711-716. [DOI] [PubMed] [Google Scholar]
- 4.Brasseur, P., R. Guiguemde, S. Diallo, V. Guiyedi, M. Kombila, P. Ringwald, and P. Olliaro. 1999. Amodiaquine remains effective for treating uncomplicated malaria in West and Central Africa. Trans. R. Soc. Trop. Med. Hyg. 86:609-612. [DOI] [PubMed] [Google Scholar]
- 5.Churchill, F. C., L. C. Patchen, C. C. Campbell, I. K. Schwartz, P. Nguyen-Dinh, and C. M. Dickinson. 1985. Amodiaquine as pro-drug: the importance of metabolite(s) in the antimalarial effect of amodiaquine in humans. Life Sci. 36:53-62. [DOI] [PubMed] [Google Scholar]
- 6.Desjardins, R. E., C. J. Canfield, J. D. Haynes, and J. D. Chulay. 1979. Quantitative assessment of antimalarial activity in vitro by a semiautomated microdilution technique. Antimicrob. Agents Chemother. 16:710-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Druilhe, P., A. Moreno, C. Blanc, P. Brasseur, and P. Jacquier. 2001. A colorimetric in vitro drug sensitivity assay for Plasmodium falciparum based on highly sensitive double-site lactate dehydrogenase antigen-capture enzyme-linked immunosorbent assay. Am. J. Trop. Med. Hyg. 64:233-241. [DOI] [PubMed] [Google Scholar]
- 8.Grace, J., A. J. Aguilar, K. M. Trotman, and T. G. Brewer. 1998. Metabolism of beta-arteether to dihydroqinghaosu by human liver microsomes and recombinant cytochrome P450. Drug Metab. Dispos. 26:313-317. [PubMed] [Google Scholar]
- 9.Moreno, A., P. Brasseur, N. Cuzin-Ouattara, C. Blanc, and P. Druilhe. 2001. Evaluation under field conditions of colourimetric DELI-microtest for the assessment of Plasmodium falciparum drug resistance. Trans. R. Soc. Trop. Med. Hyg. 95:100-103. [DOI] [PubMed] [Google Scholar]
- 10.Pradines, B., A. Tall, D. Parzy, A. Spiegel, T. Fusai, R. Hienne, J. F. Trape, and J. C. Doury. 1998. In-vitro activity of pyronaridine and amodiaquine against African isolates (Senegal) of Plasmodium falciparum in comparison with standard antimalarial agents. J. Antimicrob. Chemother. 42:333-339. [DOI] [PubMed] [Google Scholar]
- 11.Sokhna, C. S., J. F. Molez, P. Ndiaye, B. Sane, and J. F. Trape. 1997. Tests in vivo de chimiosensibilité de Plasmodium falciparum à la choloroquine au Sénégal: évolution de la résistance et estimation de l'efficacité thérapeutique. Bull. Pathol. Exot. 90:83-89. [PubMed] [Google Scholar]
- 12.Trape, J. F., and C. Rogier. 1996. Combating malaria morbidity and mortality by reducing transmission. Parasitol. Today 12:236-240. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. 2001. Antimalarial drug combination therapy. Report of a WHO technical consultation. Document WHO/CDS/RBM/2001.35. World Health Organization, Geneva, Switzerland.