Abstract
Little is known of the effects of obesity on ertapenem drug disposition and pharmacodynamics. Thirty healthy volunteers in three body mass index (BMI) groups (10 per group), normal weight (BMI, 18.5 to 24.9 kg/m2), class I-II obesity (BMI, 30 to 39.9 kg/m2), and class III obesity (BMI, ≥40 kg/m2), were administered a 1-g dose of ertapenem. Serum concentrations were obtained over 24 h. Population pharmacokinetic data were obtained using a nonparametric adaptive grid followed by Monte Carlo simulation to determine the probability of obtaining the free drug exposure targets of the time that the free drug concentration remains above the MIC (fT>MIC) of 20% and 40% for bacteriostatic and maximal bactericidal activity, respectively. Compared to the subjects in the obese groups, area under the concentration-time curve from 0 h to infinity was significantly higher in the normal-weight subjects, whereas the total central compartment volume was higher in the class III obese subjects (P ≤ 0.05). Achieving a bacteriostatic target of fT>MIC of 20% with a 90% probability was attained at MICs of ≤0.5 μg/ml for normal-weight subjects. Class I-II and class III obese subjects were able to achieve this target only at a MIC of ≤0.25 μg/ml. For maximal bactericidal activity (fT>MIC, 40%), no group attained the target at the 90% probability level at any tested MIC. The results suggest that the standard 1-g ertapenem dose may not provide adequate drug exposure for any body mass index classification for MICs in excess of 0.25 to 0.5 μg/ml.
The prevalence of obesity is on the rise, and obesity has become an epidemic in many countries. In the United States alone, more than 44 million adults are obese (body mass index [BMI], ≥30 kg/m2) (1), and some regional and ethnic groups of the population exhibit high rates of obesity. Recent data from the 1999 to 2002 National Health and Nutrition Examination Survey indicate that 65% of U.S. adults are either overweight or obese (2). Nevertheless, only a limited number of studies have been conducted that evaluate obesity-associated physiological changes and their pharmacokinetic (PK) ramifications. The effect of altered body composition on drug disposition and therapeutic outcome with increasing obesity is particularly pertinent in antimicrobial therapy. Suboptimal drug exposure can lead to clinical failure and increase the risk of drug resistance.
Several studies that specifically examined drug disposition of β-lactam antibiotics in obesity found an increase in the volume of distribution and/or drug clearance in obese subjects (3, 12, 24). This suggests that such patients may require higher doses or more frequent administration in order to achieve adequate drug exposure.
Ertapenem (Invanz) is a carbapenem antibiotic recommended for therapy (one gram once a day) of patients with appropriate renal function (creatinine clearance >30 ml/min/1.73 m2) (19). Similar to other carbapenems, ertapenem demonstrates broad-spectrum activity against gram-positive, gram-negative, and anaerobic pathogens (4). However, due to its limited activity against Acinetobacter spp. and Pseudomonas aeruginosa, it is less suitable for nosocomial infections (19, 21). Like all β-lactams, the time that the free drug concentration remains above the MIC (fT>MIC) is the major pharmacodynamic index that determines bactericidal killing activity. fT>MICs of 20% and 40% of the dosing interval are commonly cited pharmacodynamic targets for bacteriostatic and maximal bactericidal effect, respectively (7).
The objective of this study was to compare pharmacokinetic and pharmacodynamic (PD) target attainment in three BMI groups (normal weight, class I-II obesity, and class III [extreme] obesity) using the recommended 1-gram once-daily ertapenem dose through population modeling and Monte Carlo simulations.
(Part of this research was presented as an abstract and poster at the 44th Interscience Conference on Antimicrobial Agents and Chemotherapy in Washington, D.C. [30 October 2004] and at the 106th Annual Meeting of the American Society for Clinical Pharmacology and Therapeutics in Orlando, Florida [4 March 2005].)
MATERIALS AND METHODS
The study protocol was approved by the Institutional Review Board of Bassett Healthcare. All subjects gave written informed consent prior to study procedures.
Subjects and inclusion criteria.
This was an open-label healthy volunteer study. Thirty healthy adults, 10 in each of three BMI groups with equal numbers of men and women in each group, participated in the study. The three BMI groups were normal weight (BMI, 18.5 to 24.9 kg/m2), class I-II obesity (BMI, 30 to 39.9 kg/m2), and class III (extreme) obesity (BMI, ≥40 kg/m2) (14). All subjects underwent a complete medical history, physical examination, 12-lead electrocardiogram, and laboratory screening that included sodium, potassium, chloride, bicarbonate, blood urea nitrogen, serum creatinine, alanine aminotransferase (ALT), aspartate aminotransferase (AST), bilirubin, calcium, albumin, and 24-h urine collection for creatinine clearance measurement. Subjects were included if they were between the ages of 18 and 65 years, had a measured 24-h creatinine clearance of >80 ml/min/1.73 m2, ALT and AST levels no greater than twice the upper limit of normal (ALT, 21 to 72 U/liter for males and 9 to 52 U/liter for females; AST, 17 to 59 U/liter for males and 14 to 36 U/liter for females), and no known history of allergy to β-lactam antibiotics or carbapenems. Only those individuals deemed healthy by the study investigator were included in the study. Urine pregnancy tests were performed for all women of childbearing potential during the screening phase and prior to the dosing period. Additionally, women of childbearing potential were required to use a nonhormonal method of contraception. Use of any medications known to affect renal tubular secretion or reabsorption of β-lactams, monobactams, or carbapenems was prohibited.
Study design.
Following an overnight fast of at least 8 h, subjects were brought into the clinical research center and two intravenous (IV) lines were placed in each subject (one in each forearm). A single 1-g dose of ertapenem was infused over 30 min using an IV infusion pump. Twenty-five milliliters of 0.9% sodium chloride was used to flush the IV line at the completion of the infusion. To determine the ertapenem concentrations, 7-ml blood samples were collected from the contralateral arm predose and 5, 10, 15, and 30 min and 1, 2, 4, 6, 8, 12, 14, and 24 h after drug administration. Serum samples were immediately harvested and frozen at −80°C until analysis. Subjects were allowed to eat after the 2-h blood sample was obtained.
Sample size determination.
According to prestudy sample size determinations, 30 subjects (10 per group) were required to detect a minimum difference of 25% in ertapenem clearance based on an average total body clearance of 29 ml/min for 1-g dose of ertapenem with 80% power and alpha of 0.05. Healthy volunteer pharmacokinetic data for sample size calculations were obtained from the drug manufacturer (Merck clinical investigator's confidential informational brochure MK-0826 summary of information; Merck & Co., Inc., Whitehouse Station, NJ).
Analytical procedure.
Total ertapenem serum concentrations were assayed by Merck & Co., Inc., using a previously validated assay (13). In brief, reverse-phase high-performance liquid chromatography with UV absorbance detection (300 nm) was used. Samples were extracted online with column switching of stabilized aliquots of quantitation of 0.125 and 1.25 μg/ml, respectively. The intraday accuracy and precision of the assays did not deviate more than 15% of nominal or exceed 10% coefficient of variation at all standard concentrations. During batch analysis, quality control concentrations did not deviate by more than 20% of normal.
PK/PD analysis.
Pharmacokinetic parameters were determined via population methods using a nonparametric adaptive grid program of Leary et al. (10). Weights were estimated as the inverse of the observation variance (weight = 1/variance). Data were fit to a two-compartment IV infusion model. For pharmacodynamic analyses, MICs of 0.25, 0.5, 1, 2, 4, and 8 μg/ml were tested, on the basis of microorganism susceptibility data obtained from the ertapenem package insert (Invanz package insert, Merck & Co., Inc., Whitehouse Station, NJ). Monte Carlo simulations were performed using the ADAPT II software programs of D'Argenio and Schumitzky (5). Normal and log-normal distributions were evaluated and examined for the fidelity with which the original parameter values and their distributions were repeated. A total of 9,999 simulations were conducted to determine the probability of obtaining free drug target values of fT>MIC of 20% and 40% for bacteriostatic and maximum bactericidal activity, respectively, for each BMI group. An unbound drug fraction of 5% was used in all PD analyses (11, 16). Statistical analyses comparing the PK parameters were performed using analysis of variance and Scheffe post hoc testing in SYSTAT version 11.0 (Systat Software Inc., Point Richmond, CA). Data are presented as means ± standard deviations unless otherwise noted. P values of ≤0.05 were considered statistically significant.
RESULTS
Thirty-two subjects were screened and enrolled for the study. Two subjects were removed prior to administration of study drug. One subject was removed due to difficulty in obtaining venous access. The second subject requested withdrawal from the study. Thirty subjects in all completed the study and were included in the analysis. Demographic data are shown in Table 1. The ranges of BMI for the BMI groups were as follows: normal weight, 19.2 to 24.6 kg/m2; class I-II obesity, 30.5 to 37.8 kg/m2; and class III obesity (40 to 50.1 kg/m2). The ranges of body weights for the BMI groups were as follows: normal weight, 49.8 to 78.6 kg; class I-II obesity, 79.6 to 107.6 kg; and class III obesity, 107.4 to 140.0 kg. Ertapenem infused over 30 min was well tolerated, and no significant adverse events were reported.
TABLE 1.
Demographic characteristics of 30 healthy subjects by body mass index group
| Demographic characteristic | Mean value (SD) for BMI group
|
||
|---|---|---|---|
| Normal wt (18.5-24.9 kg/m2) | Class I-II obesity (30-39.9 kg/m2) | Class III obesity (≥40 kg/m2) | |
| No. of women | 5 | 5 | 5 |
| No. of men | 5 | 5 | 5 |
| Age (yr) | 34.1 (8.4) | 41.8 (5.1) | 35.9 (7.1) |
| Ht (cm) | 171.9 (8.5) | 170.1 (9.9) | 171.4 (8.2) |
| Wt (kg) | 66.7 (9.6)a | 96.0 (9.1)b | 127.2 (12.5) |
| BMI (kg/m2) | 22.5 (1.9)a | 33.4 (2.6)b | 43.4 (2.9) |
| CLCR (ml/min/1.73 m2)c | 101.9 (13.2) | 119.6 (38.3) | 98.8 (31.8) |
Significantly different from the values for class I-II and class III obesity groups (P < 0.001).
Significantly different from the values for class III obesity group (P < 0.001).
CLCR, creatinine clearance.
PK.
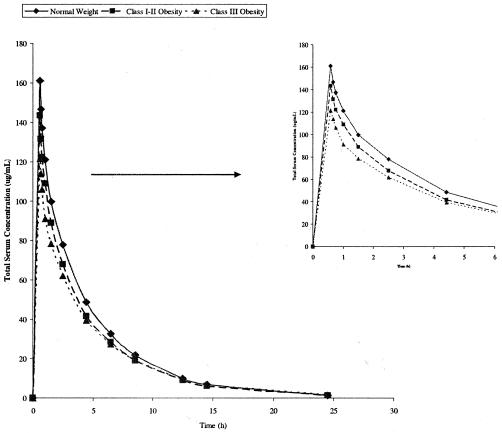
Figure 1 displays the mean serum concentration-time profiles of total ertapenem for each BMI group. Table 2 summarizes ertapenem pharmacokinetic parameters also by BMI group. The area under the concentration-time curve from 0 h to infinity of normal-weight individuals (586 ± 50.4 μg · h/ml) was significantly higher (P ≤ 0.04) than the values for class I-II obese individuals (513 ± 63.2 μg · h/ml) and class III obese individuals (486 ± 64.9 μg · h/ml). Ertapenem total body clearance normalized for body surface area showed a decreasing trend with increase in BMI group; however, this was not statistically significant. Compared to class I-II and class III obese subjects, the central compartment volume (V1) corrected for weight was significantly higher (P ≤ 0.004) in the normal-weight subjects (0.078 ± 0.008 liter/kg), whereas total V1 was higher (P ≤ 0.04) in class III obese subjects (7.18 ± 1.1 liter).
FIG. 1.
Total concentration of ertapenem in serum versus time profile over 24 h for normal-weight, class I-II obesity, and class III obesity groups. The figure on the right shows an enlarged time scale and shows the total drug concentration from 0 to 6 h.
TABLE 2.
Pharmacokinetic parameters of total ertapenem concentration for 30 subjects by body mass index group
| Pharmacokinetic parametera | Mean (SD) value for BMI group
|
||
|---|---|---|---|
| Normal wt | Class I-II obesity | Class III obesity | |
| AUC0-∞ (μg · h/ml) | 586 (50.4)b | 513 (63.2) | 486 (64.9) |
| CL (liter/h/1.73 m2) | 1.58 (0.2) | 1.50 (0.2) | 1.38 (0.2) |
| CL (liter/h/kg) | 0.024 (0.004)c | 0.019 (0.003)d | 0.015 (0.002) |
| V1 (liter/kg) | 0.078 (0.008)c | 0.063 (0.01) | 0.057 (0.009) |
| Total V1 (liter) | 5.15 (0.5) | 6.04 (1.2) | 7.18 (1.1)e |
AUC0-∞, area under the concentration-time curve from 0 h to infinity; CL, total body clearance; V1, central compartment volume.
Significantly different from the values for class I-II and class III obesity groups (P ≤ 0.05).
Significantly different from the values for the class I-II obesity group (P ≤ 0.05) and the class III obesity group (P < 0.001).
Significantly different from the value for the class III obesity group (P ≤ 0.05).
Significantly different from the values for the class I-II obesity group (P ≤ 0.05) and the normal-weight group (P < 0.001).
PD.
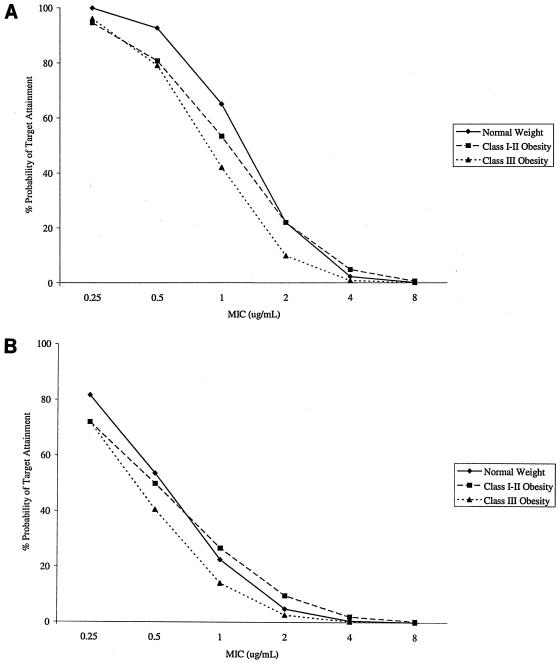
Figure 2 displays the probability distribution of achieving pharmacodynamic targets of fT>MICs of 20% (Fig. 2A) and 40% (Fig. 2B). At the lowest MIC of 0.25 μg/ml, all BMI groups are predicted to attain the bacteriostatic target, fT>MIC of 20% with greater than 90% probability. At a higher MIC of 1 μg/ml, only 65% of normal-weight subjects, 53% of class I-II obese subjects, and 42% of class III obese subjects are projected to meet the target. At the highest MIC of 8 μg/ml, less than 0.6% of the subjects (irrespective of BMI group) are predicted to attain the bacteriostatic target of 20%.
FIG. 2.
Percent probability of attaining the target of 20% (A) or 40% (B) for fT>MIC with a single 1-gram dose of ertapenem at MICs of 0.25, 0.5, 1, 2, 4, and 8 μg/ml in normal-weight, class I-II obese, and class III obese groups.
By comparison, the likelihood of achieving the target for maximal bactericidal activity (fT>MIC, 40%) are even lower. Probabilities of ≥50% are predicted at MICs of ≤0.5 μg/ml for normal-weight and class I-II obese groups, whereas class III individuals are predicted to achieve this target only at a MIC of 0.25 μg/ml. None of the groups were able to attain ≥90% probability for achieving a free drug concentration fT>MIC of 40%.
DISCUSSION
Ertapenem is a carbapenem antibiotic that is given once daily. The drug is extensively protein bound, exhibiting concentration-dependent, saturable binding. The highly protein-bound nature of this antibiotic (∼95% at plasma drug concentrations of <100 μg/ml with ∼85% bound at concentrations of >300 μg/ml) extends the half-life (∼4 h) of the drug, allowing for once-daily dosing (11, 15). On the basis of clinically achieved concentrations (maximum concentration of drug in serum, ∼155 μg/ml), the higher value of 95% is predicted to be reflective of binding observed after IV administration of a 1-g dose in humans.
Several studies examining the impact of obesity-associated physiological changes on drug disposition noted pharmacokinetic differences in obese subjects. Higher creatinine clearance has been observed in obese subjects compared to lean controls (18). The exact mechanism behind this finding is unknown; however, an increase in blood volume has been proposed (22). Other studies found higher drug clearance and/or volume of distribution and lower drug exposure in obese patients. One study observed increased cefotiam clearance and volume of distribution of 63% and 69%, respectively, in Japanese sumo wrestlers compared to controls (3). This suggests that obese patients may have inadequate antimicrobial exposure. Other investigators found significantly lower blood and tissue concentrations of cefazolin in obese patients after administration of 1 g intravenously (8). This same group noted a 5.6% drop in wound infection after increasing the surgical prophylactic dose of cefazolin from 1 g to 2 g IV in obese patients. To date, however, there is limited data on pharmacokinetics in extremely obese persons.
In our study, we examined ertapenem pharmacokinetics and pharmacodynamics in three different BMI groups of normal weight, class I-II obesity, and class III obesity. We found an increase in total V1 with elevated BMI. Compared to the normal-weight subjects, subjects in the class III obesity group had a mean increase in V1 of approximately 40% (P < 0.001). Total body clearance adjusted for body surface area was also lower in the obese subjects, but this trend was not found to be significant. When clearance was adjusted for body weight, a significant difference was observed between normal-weight subjects (0.024 liter/h/kg) versus class I-II (0.019 liter/h/kg) and class III (0.015 liter/h/kg) obese subjects (P ≤ 0.007) and between class I-II and class III (P ≤ 0.05) obese subjects. The literature is unclear as to the most appropriate method of comparing total body clearance in normal-weight versus obese individuals. While clearance calculations are often adjusted for body surface area or body weight, which method of estimation is superior remains debatable.
Ertapenem is predominantly renally excreted via glomerular filtration with tubular secretion having a minor component. Studies have demonstrated an increase in glomerular filtration in obese subjects (6, 20). Therefore, we expected to see an increase in drug clearance with increasing obesity. Clearance was normalized for body surface area and total body weight, and both showed decreasing clearance with increasing obesity. Our results indicate that there was a modest decrease in drug exposure in the obese subjects compared to normal-weight subjects. Whether this is of clinical significant difference in therapeutic outcome is uncertain.
Like all β-lactams, the efficacy of ertapenem is determined by the time that the free drug concentration remains above the MIC. For carbapenems, fT>MICs of 20% and 40% are considered pharmacodynamic target attainment goals for bacteriostatic and maximum bactericidal activity, respectively (7). Using data from this study, we performed Monte Carlo simulations to determine the probability of achieving these targets. On the basis of the results, the probability of obtaining PD targets dropped sharply with increasing MICs. The normal-weight subjects had higher percentages of target attainment than the obese subjects at each MIC. However, these differences were modest.
According to the FDA-approved ertapenem package insert, a MIC of ≤2 μg/ml is considered susceptible against aerobic pathogens (members of the family Enterobacteriaceae and Staphylococcus spp.). The results of our simulations indicate probabilities of approximately 22% of normal-weight and class I-II obese subjects would meet the bacteriostatic target attainment of 20% above a MIC of ≤2 μg/ml. For the class III obese subjects, the probability is lower (<10%).
In the United States, probability of ≥90% is recognized as an acceptable PD target (P. G. Ambrose, S. M. Bhavnani, R. N. Jones, W. A. Craig, and M. N. Dudley, Abstr. 44th Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-138, 2004). While this value is somewhat arbitrary, it has been adopted by the Clinical and Laboratory Standards Institute (CLIS) as the standard. On the basis of our results for bacteriostatic activity, normal-body-weight individuals were able to achieve this target only at MICs of ≤0.5 μg/ml. Neither obesity group was able to reach 90% probability at MICs of >0.25 μg/ml. For maximal kill activity, no groups met the 90% target at any tested MIC. Thus, subjects failed to achieve acceptable PD targets except at the lowest MICs. Findings from recent publications (9, 17) suggest that five major organisms had ertapenem MIC90s of ≤0.25 μg/ml. These were Escherichia coli, Klebsiella pneumoniae, Serratia marcescens, Enterobacter spp., and oxacillin-susceptible Staphylococcus aureus, with the latter two having MIC90s of 0.25 μg/ml. In these in vitro studies, S. pneumoniae, oxacillin-susceptible coagulase-negative staphylococci, Acinetobacter spp., and P. aeruginosa all had MIC90s that exceeded 0.25 μg/ml.
A limitation to our study is that it was conducted in healthy volunteers. It is well recognized that pharmacokinetics and pharmacodynamics of antimicrobials can vary significantly in sick patients. Therefore, drug exposure may be higher in the clinical setting due to reduced clearance, decreased protein binding, or both. In addition, while fT>MICs of 20% and 40% are commonly cited pharmacodynamic targets, lower targets for specific pathogens have been suggested for carbapenems. One study suggests the pharmacodynamic target against Streptococcus pneumoniae may be lower at a fT>MIC of 15% (W. A. Craig and D. R. Andes, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., poster 2094, 2001). Another study evaluating the activity of ertapenem against Streptococcus pneumoniae in a murine neutropenic thigh infection model found that a fT>MIC of 6% provided adequate static effect (23). Use of ertapenem in patients with physiologic impairment of renal function or use with organisms where pharmacodynamic targets are lower may explain the discordance between our findings and the clinical outcome for infections due to organisms that ertapenem is approved for in the product label.
In summary, our results suggest that the standard dose of ertapenem (1 g daily) may not be sufficient to achieve 90% probability of target attainment for bacteriostatic (fT>MIC, 20%) or maximum bactericidal (fT>MIC, 40%) activity for organisms with MICs in excess of 0.25 to 0.5 μg/ml in any of the BMI groups. Further investigation of optimal ertapenem dosing in patient populations infected with organisms in which MIC determination has been done should be considered.
Acknowledgments
We are grateful for the assistance of Anne Gartung, Cheryl Michalak, Jennifer Victory, and Patrick Johnson.
This study was funded by a grant from Merck & Co., Inc.
REFERENCES
- 1.Centers for Disease Control and Prevention. 2003. 1991-2001 prevalence of obesity among U.S. adults, by characteristics. Centers for Disease Control and Prevention, Atlanta, Ga. [Online.] http://www.cdc.gov/nccdphp/dnpa/obesity/trend/prev_char.htm.
- 2.Centers for Disease Control and Prevention. 2004. Prevalence of overweight and obesity among adults: United States, 1999-2002. Centers for Disease Control and Prevention, Atlanta, Ga. [Online.] http://www.cdc.gov/nchs/products/pubs/pubd/hestats/obese/obse99.htm.
- 3.Chiba, K., M. Tsuchiya, J. Kato, K. Ochi, Z. Kawa, and T. Ishizaki. 1989. Cefotiam disposition in markedly obese athlete patients, Japanese sumo wrestlers. Antimicrob. Agents Chemother. 33:1188-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Curran, M., D. Simpson, and C. Perry. 2003. Ertapenem: a review of its use in the management of bacterial infections. Drugs 63:1855-1878. [DOI] [PubMed] [Google Scholar]
- 5.D'Argenio, D. Z., and A. Schumitzky. 1997. ADAPT II user's guide: pharmacokinetic/pharmacodynamic systems analysis software. Biomedical Simulations Resource, Los Angeles, Calif.
- 6.Davis, R. L., R. W. Quenzer, H. P. Bozigian, and C. W. Warner. 1990. Pharmacokinetics of ranitidine in morbidly obese women. Ann. Pharmacother. 24:1040-1043. [DOI] [PubMed] [Google Scholar]
- 7.Drusano, G. L. 2004. Antimicrobial pharmacodynamics: critical interactions of ‘bug and drug.’ Nat. Rev. Microbiol. 2:289-300. [DOI] [PubMed] [Google Scholar]
- 8.Forse, R. A., B. Karam, L. D. MacLean, and N. V. Christou. 1989. Antibiotic prophylaxis for surgery in morbidly obese patients. Surgery 106:750-756. [PubMed] [Google Scholar]
- 9.Jones, R. N., H. S. Sader, and T. R. Fritsche. 2005. Comparative activity of doripenem and three other carbapenems tested against Gram-negative bacilli with various beta-lactamase resistance mechanisms. Diagn. Microbiol. Infect. Dis. 52:71-74. [DOI] [PubMed] [Google Scholar]
- 10.Leary, R., R. Jelliffe, A. Schumitzky, and M. Van Guilder. 2001. An adaptive grid, non-parametric approach to pharmacokinetic and dynamic (PK/PD) models, p. 389-394. In Proceedings of the 14th IEEE Symposium on Computer Based Medical Systems. IEEE Computer Society, Bethesda, Md.
- 11.Livermore, D. M., A. M. Sefton, and G. M. Scott. 2003. Properties and potential of ertapenem. J. Antimicrob. Chemother. 52:331-344. [DOI] [PubMed] [Google Scholar]
- 12.Mann, H. J., and H. Buchwald. 1986. Cefamandole distribution in serum, adipose tissue, and wound drainage in morbidly obese patients. Drug Intell. Clin. Pharm. 20:869-873. [DOI] [PubMed] [Google Scholar]
- 13.Musson, D. G., K. L. Birk, C. J. Kitchen, J. Zhang, J. Y. Hsieh, W. Fang, A. K. Majumdar, and J. D. Rogers. 2003. Assay methodology for the quantitation of unbound ertapenem, a new carbapenem antibiotic, in human plasma. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 783:1-9. [DOI] [PubMed] [Google Scholar]
- 14.National Institutes of Health. 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. NIH publication 98-4083. National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Md. [Online.] http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf. Accessed 2 August 2004.
- 15.Nix, D. E., A. K. Majumdar, and M. J. DiNubile. 2004. Pharmacokinetics and pharmacodynamics of ertapenem: an overview for clinicians. J. Antimicrob. Chemother. 53(Suppl. S2):ii23-ii28. [DOI] [PubMed] [Google Scholar]
- 16.Odenholt, I. 2001. Ertapenem: a new carbapenem. Expert Opin. Investig. Drugs 10:1157-1166. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds, R., N. Potz, M. Colman, A. Williams, D. Livermore, and A. MacGowan. 2004. Antimicrobial susceptibility of the pathogens of bacteraemia in the UK and Ireland 2001-2002: the BSAC Bacteraemia Resistance Surveillance Programme. J. Antimicrob. Chemother. 53:1018-1032. [DOI] [PubMed] [Google Scholar]
- 18.Salazar, D. E., and G. B. Corcoran. 1988. Predicting creatinine clearance and renal drug clearance in obese patients from estimated fat-free body mass. Am. J. Med. 84:1053-1060. [DOI] [PubMed] [Google Scholar]
- 19.Shah, P. M., and R. D. Isaacs. 2003. Ertapenem, the first of a new group of carbapenems. J. Antimicrob. Chemother. 52:538-542. [DOI] [PubMed] [Google Scholar]
- 20.Stokholm, K. H., J. Brochner-Mortensen, and P. F. Hoilund-Carlsen. 1980. Increased glomerular filtration rate and adrenocortical function in obese women. Int. J. Obes. 4:57-63. [PubMed] [Google Scholar]
- 21.Wexler, H. M. 2004. In vitro activity of ertapenem: review of recent studies. J. Antimicrob. Chemother. 53(Suppl. S2):ii11-ii21. [DOI] [PubMed] [Google Scholar]
- 22.Wurtz, R., G. Itokazu, and K. Rodvold. 1997. Antimicrobial dosing in obese patients. Clin. Infect. Dis. 25:112-118. [DOI] [PubMed] [Google Scholar]
- 23.Xuan, D., M. Banevicius, B. Capitano, M. K. Kim, C. Nightingale, and D. Nicolau. 2002. Pharmacodynamic assessment of ertapenem (MK-0826) against Streptococcus pneumoniae in a murine neutropenic thigh infection model. Antimicrob. Agents Chemother. 46:2990-2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yost, R. L., and H. Derendorf. 1986. Disposition of cefotaxime and its desacetyl metabolite in morbidly obese male and female subjects. Ther. Drug Monit. 8:189-194. [DOI] [PubMed] [Google Scholar]