Abstract
1 Midazolam, in an oral dose of 15 mg, and placebo were administered to 15 children aged 6-15 years in treatment of night terrors.
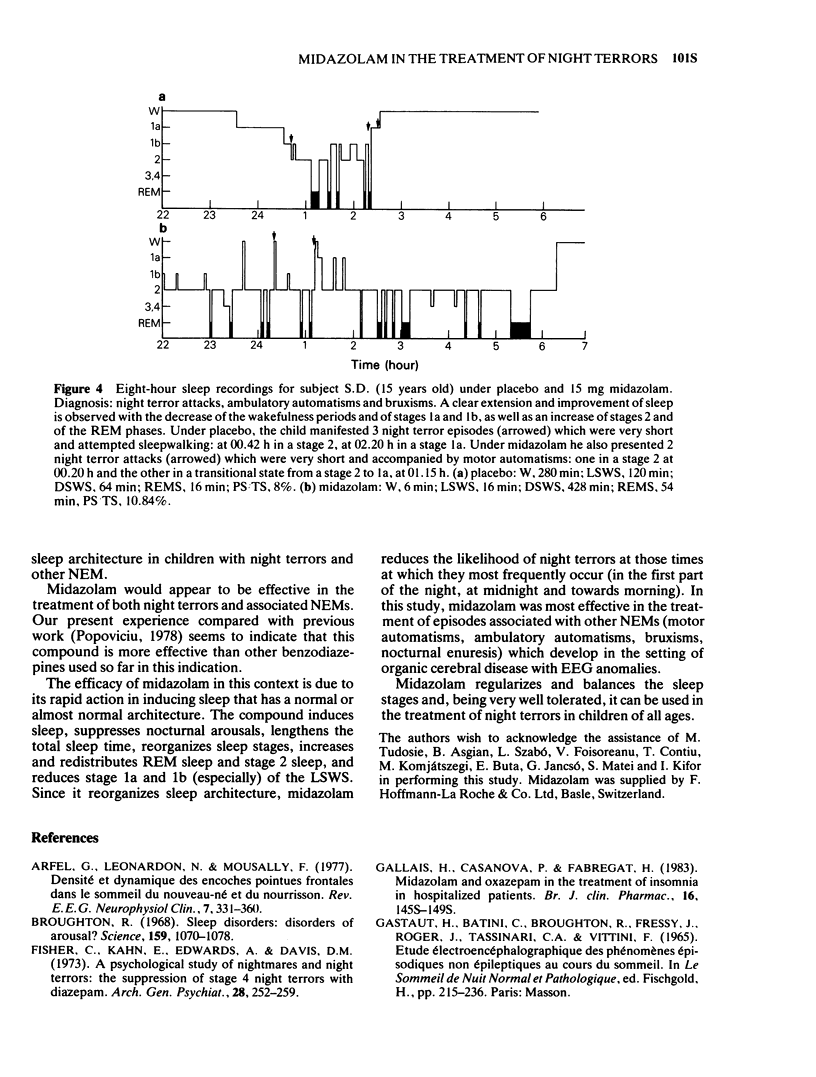
2 After an initial adaptation night, the patients received placebo for 2 nights, followed by 15 mg midazolam for 2 nights and placebo again on the final 2 nights. Eight-hour nocturnal polygraphic recordings were made after the administration of both placebo and midazolam. The patients were continuously monitored by means of closed circuit infra-red television.
3 Ten of the patients manifested simple episodes while five had attacks associated with motor automatisms and EEG anomalies.
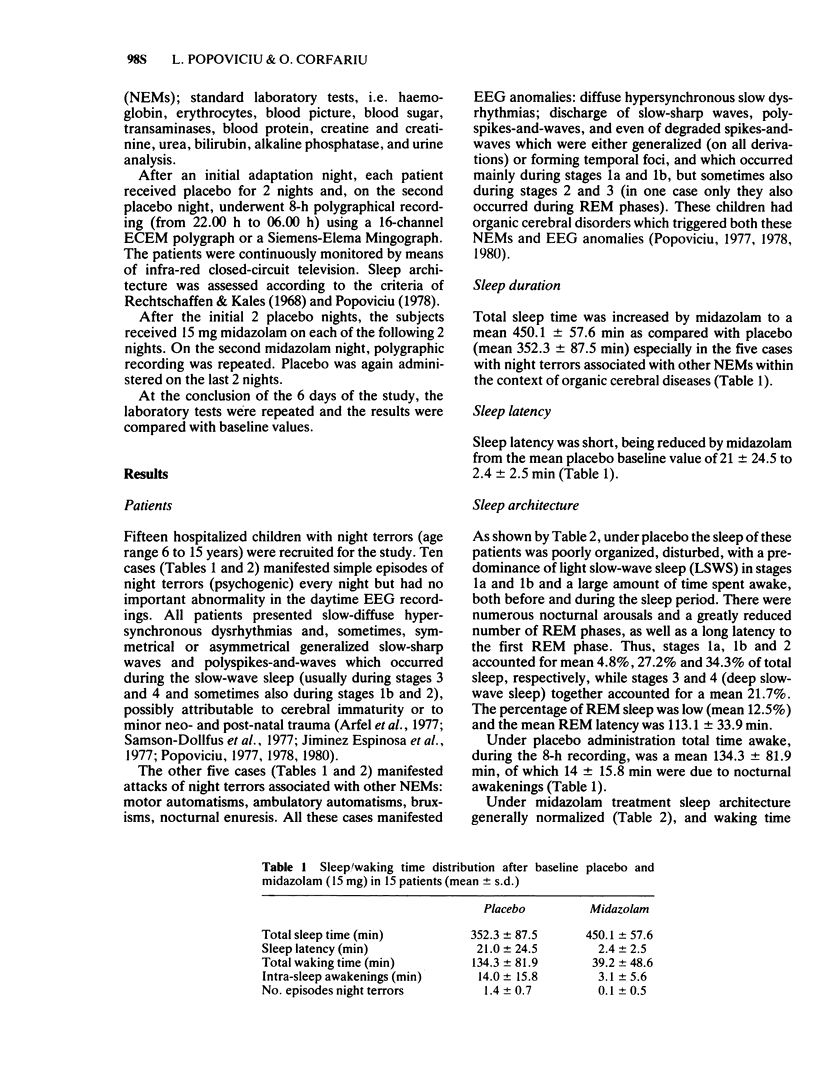
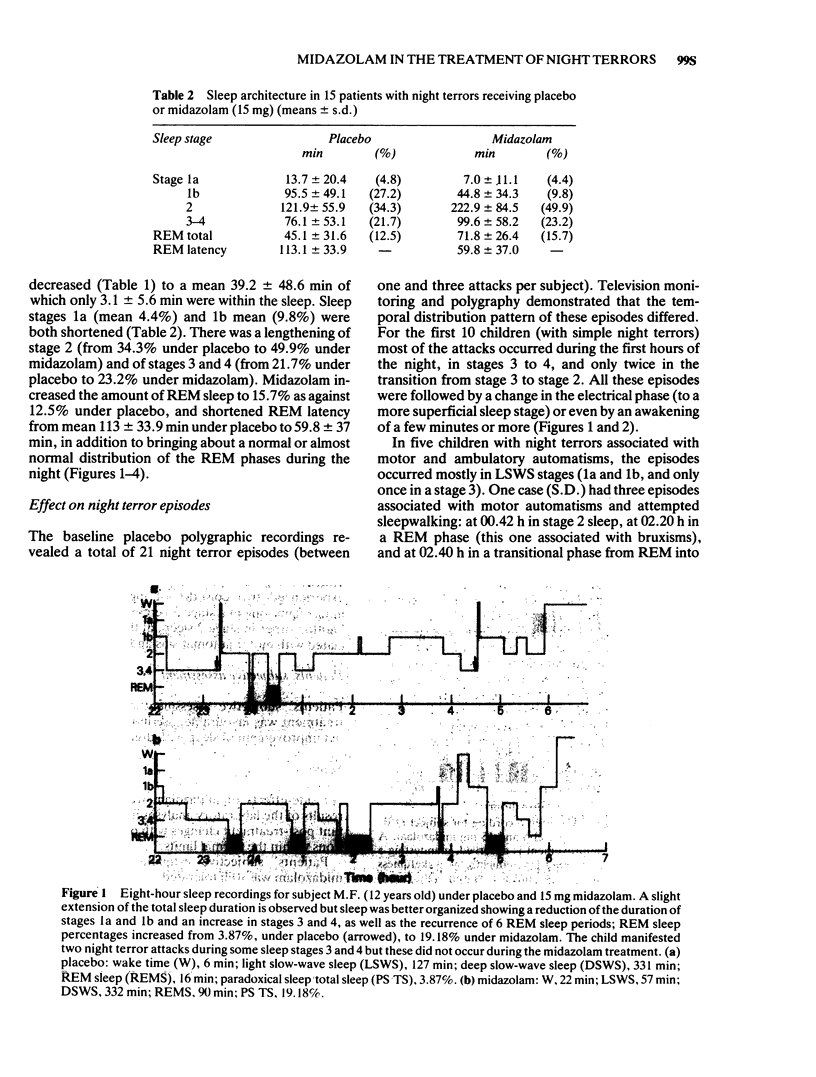
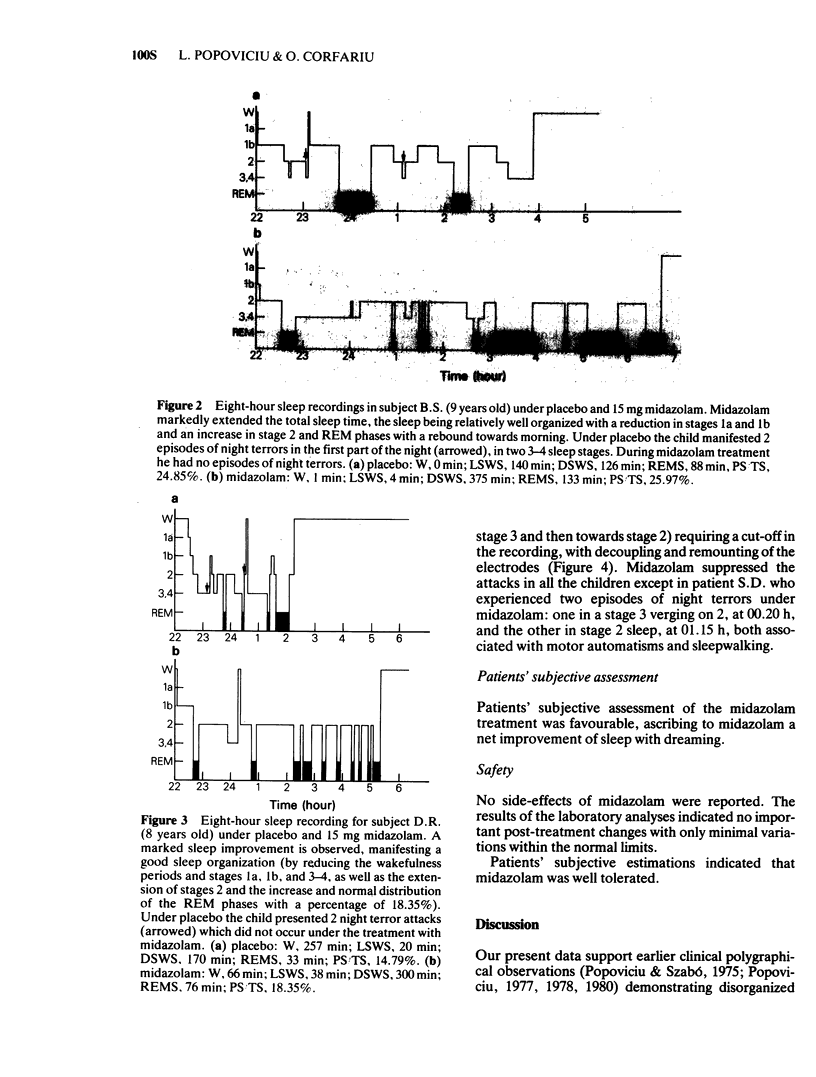
4 The total sleep time was lengthened by midazolam in most of the children; sleep architecture was favourably modified, mainly in terms of the amount and proportion of REM sleep (accompanied by dreams) and stage 2 sleep. Night terrors were eliminated by midazolam in all except one patient. REM sleep latency also decreased as did the number of nocturnal arousals (clinical and/or EEG). In the five cases with a background of organic cerebral disorders, the EEG anomalies and these attacks were suppressed by midazolam especially during the first sleep cycles.
5 Patients' subjective assessment of the quality of sleep was favourable. Midazolam was well tolerated with no side-effects.
Full text
PDF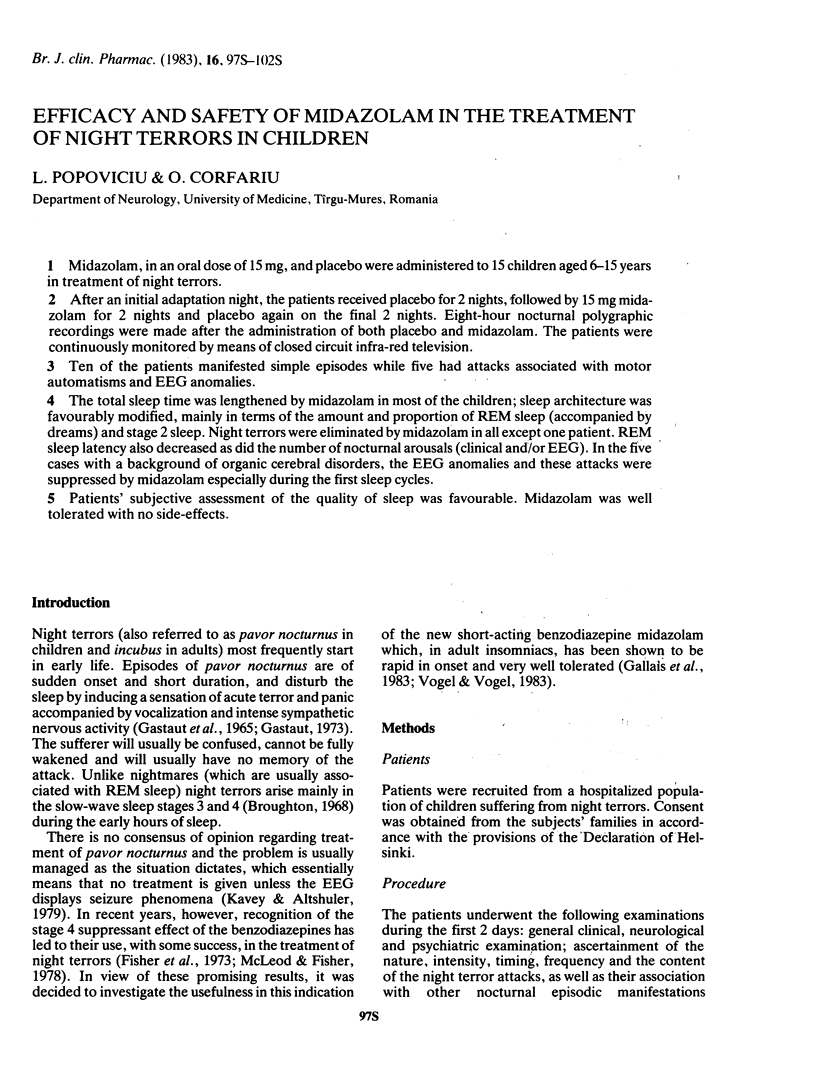
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arfel G., Leonardon N., Moussalli F. Densité et dynamique des encoches pointues frontales dans le sommeil du nouveau-né et du nourrisson. Rev Electroencephalogr Neurophysiol Clin. 1977 Jul-Sep;7(3):351–360. doi: 10.1016/s0370-4475(77)80014-2. [DOI] [PubMed] [Google Scholar]
- Broughton R. J. Sleep disorders: disorders of arousal? Enuresis, somnambulism, and nightmares occur in confusional states of arousal, not in "dreaming sleep". Science. 1968 Mar 8;159(3819):1070–1078. doi: 10.1126/science.159.3819.1070. [DOI] [PubMed] [Google Scholar]
- Fisher C., Kahn E., Edwards A., Davis D. M. A psychophysiological study of nightmares and night terrors. The suppression of stage 4 night terrors with diazepam. Arch Gen Psychiatry. 1973 Feb;28(2):252–259. doi: 10.1001/archpsyc.1973.01750320082013. [DOI] [PubMed] [Google Scholar]
- Gallais H., Casanova P., Fabregat H. Midazolam and oxazepam in the treatment of insomnia in hospitalized patients. Br J Clin Pharmacol. 1983;16 (Suppl 1):145S–149S. doi: 10.1111/j.1365-2125.1983.tb02286.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod M. N., Fisher P. Pavor nocturnus in a schizophrenic patient: a review and case study. Am J Psychiatry. 1978 Feb;135(2):235–236. doi: 10.1176/ajp.135.2.235. [DOI] [PubMed] [Google Scholar]
- Samson-Dollfus D., Nogues B., Verdure-Poussin A., Malleville F. Electroencéphalogramme du sommeil de l'enfant normal entre 5 mois et 3 ans. Rev Electroencephalogr Neurophysiol Clin. 1977 Jul-Sep;7(3):335–345. doi: 10.1016/s0370-4475(77)80012-9. [DOI] [PubMed] [Google Scholar]
- Vogel G. W., Vogel F. Effect of midazolam on sleep of insomniacs. Br J Clin Pharmacol. 1983;16 (Suppl 1):103S–108S. doi: 10.1111/j.1365-2125.1983.tb02279.x. [DOI] [PMC free article] [PubMed] [Google Scholar]



