Abstract
Background
The authors conducted a study to examine oral cancer prevention and early detection practice patterns in a population-based random sample of practicing oral health care professionals in New York state.
Methods
The authors surveyed a population-based, self-weighting, stratified random sample of dentists (n = 1,025) and dental hygienists (n = 1,025) in New York state. They assessed the subjects’ readiness to offer tobacco-use cessation and alcohol-abuse counseling and oral cancer examinations.
Results
The effective response rates were 55 and 66 percent for dentists and dental hygienists, respectively. In terms of readiness to perform oral cancer examinations for patients aged 40 years and older, the large majority (82 percent of dentists and 72 percent of dental hygienists) were in the maintenance stage of behavior, indicating that oral cancer examinations were a routine part of their practice. In terms of readiness to offer tobacco-use cessation counseling, only 12 percent of dentists and 21 percent of dental hygienists were in the maintenance stage, and only 2 percent of dentists and 4 percent of dental hygienists were in the maintenance stage of offering alcohol-abuse counseling.
Conclusions
Oral cancer examinations seem to have been adopted as a standard of practice by most oral health care providers in New York state, but cancer prevention services, such as counseling regarding cessation of tobacco use and alcohol abuse, are lacking.
Clinical Implications
Oral health care providers should be trained in oral cancer prevention services such as tobacco-use cessation and alcohol-abuse counseling and encouraged to include these services, along with continued provision of oral cancer examinations, as a standard aspect of care.
Keywords: Oral cancer, tobacco use, alcohol abuse, cancer prevention, counseling, smoking, oral health
In 2002, it was estimated that oral and pharyngeal cancers would account for 28,900 cases and 7,400 deaths in the United States alone.1 The primary risk factors for oral and pharyngeal cancer are tobacco use and the consumption of alcoholic beverages, and their joint effect appears to be multiplicative.2 Moreover, it has been estimated that in the United States, approximately 75 percent of all cancers at these sites are attributable to smoking and drinking.2 Smokeless tobacco use also has been shown to be a significant risk factor for oral and pharyngeal cancer, particularly for oral sites that come into contact with the product.3
Oral health care providers should include tobacco-use cessation and alcohol-abuse counseling as a standard aspect of care.
To reduce morbidity and mortality attributable to oral cancer, greater efforts at primary and secondary prevention are needed. Primary prevention of oral cancer includes avoidance of tobacco use and alcohol abuse, as well as appropriate intake of fruits and vegetables. Secondary prevention of oral cancer consists of a visual and tactile examination of the oral cavity, the head and the neck, which is essential for early detection. In the past few years, awareness of the need for routine oral cancer examinations in populations at risk has increased, particularly among oral health care professionals. However, efforts toward raising the awareness of health care professionals and the general public of the need for primary prevention of oral cancer have been lacking.
The U.S. Preventive Services Task Force4 recommended that clinicians include a careful examination and screening for oral cancer in their care of asymptomatic patients who have a history of tobacco or alcohol use. The American Cancer Society recommends oral cancer checkups for patients undergoing periodic dental and medical examinations.5 But in 2003, the Cochrane Health Education Foundation reported that more evidence is needed to find out whether screening programs are effective in detecting oral cancer earlier and in reducing mortality.6
The primary care dental team has a central role in providing information about the oral health effects of tobacco use and alcohol abuse, including the risks of oral cancer and periodontal disease. However, national as well as local studies have demonstrated that oral health care providers (dentists and dental hygienists) have not widely adopted the published guidelines for tobacco-use cessation counseling.7–10 To date, no prior study has assessed the alcohol-abuse counseling practices of oral health care professionals.
National as well as local studies have demonstrated that oral health care providers have not widely adopted the published guidelines for tobacco-use cessation counseling.
We conducted a study to examine oral cancer prevention and early detection practice patterns in a population-based random sampling of practicing oral health care professionals in the state of New York. In addition, we examined whether there were any demographic or practice-level variables that were associated with lower adherence to recommended health behavior counseling so as to properly target future statewide professional educational initiatives to increase adoption of such practices.
METHODS
We conducted our study as part of a statewide needs assessment for the development of an oral cancer control plan for New York state. We selected a population-based, self-weighting, stratified random sample of dentists (n = 1,025) and dental hygienists (n = 1,025) from the roster of licensed oral health care practitioners in New York. The stratification was based on the geographical location of their residence (New York City versus the remainder of New York state). We used the nQuery Advisor software (Statistical Solutions, Saugus, Mass.) to calculate the sample sizes. Only professionals who were active in the practice of dentistry or dental hygiene were eligible to participate in the mail survey. After eliminating all ineligible providers (because they were deceased, retired, no longer in practice or had moved out of the state), we obtained a final sample size of 904 dentists and 963 dental hygienists. This sample size permitted estimation of several parameters of interest to our study with a power of at least 80 percent. This study was approved by the institutional review boards of New York State Department of Health and New York University, New York City.
We sent five mailings using the Tailored Design Method.11 The subjects were sent initial contact letters in May 2002. Thereafter, we mailed all eligible providers a cover letter, a questionnaire, a stamped return envelope and a new U.S. golden dollar as an incentive. A reminder postcard was mailed two weeks later to the entire study sample. This was followed by a second mailing three weeks later to nonrespondents. Finally, we sent a complete third mailing to 411 nonrespondents by overnight delivery three weeks thereafter, with the principal investigator personally signing each cover letter. Four hundred ninety-nine dentists and 630 dental hygienists responded to the survey, yielding effective response rates of 55 and 66 percent, respectively.
We developed the survey instrument, using the work of Goldstein and colleagues as a basis, 12 to assess the tobacco-use cessation and alcohol-abuse counseling and oral cancer examination practices of the providers in our survey population. The items assessing tobacco-use cessation practices were based on the U.S. Department of Health and Human Services (DHHS) Public Health Service clinical practice guidelines, “Treating Tobacco Use and Dependence.”13 These guidelines include a list of activities and behaviors called “the five As”:
– ask the patient about his or her tobacco use;
– advise the patient to quit;
– assess the patient’s willingness to make a quit attempt;
– assist in the quit attempt;
– arrange follow-up contact, preferably within the first week after the quit date.
We asked the participants to estimate the percentage of their patients for whom they routinely provided each of these five tobacco-use cessation activities: less than 20 percent, 21 to 40 percent, 41 to 60 percent, 61 to 80 percent and greater than 80 percent. A percentage of greater than 80 indicated routine adoption of the recommended practice behavior. We also assessed whether the providers asked in their medical history taking about patients’ present and past use of tobacco, as well as the type and amount of tobacco used.
We developed items assessing alcohol-abuse counseling practices that were similar in content and format to the five As in the DHHS tobacco-use cessation guidelines.
As with tobacco use, we asked the participants to estimate the percentage of their patients for whom they routinely provided each of the five activities, using the same percentage groupings. In addition, we assessed whether the providers asked in their medical history taking about patients’ present and past use of alcohol as well as the type and amount of alcohol used.
We used the Transtheoretical Model of Change (TTM)14 to classify providers’ readiness to conduct oral cancer examinations and to offer tobacco-use cessation and alcohol-abuse counseling. This model, originally developed to help understand the stages of behavioral changes among smokers, has been successfully adapted to provide a framework for understanding physicians’ readiness or willingness to adopt smoking-cessation counseling behaviors12,15 and their attitudes toward cancer screening guidelines.16 The TTM identifies five stages of readiness to change through which people progress when making changes in their behavior:
– precontemplation, in which the person is not thinking of changing behavior;
– contemplation, in which the person is seriously thinking about changing behavior within the next six months;
– preparation, in which the person has taken steps to change behavior within the next month but has not implemented them;
– action, in which the person has made a behavior change within the last six months;
– maintenance, in which the person has sustained the behavior for at least six months.
To calculate the number of providers who were at each of these stages of change in terms of offering tobacco-use cessation counseling, we used only those who reported not assisting more than 80 percent of their tobacco-using patients in developing a quit plan. Thus, we classified these providers’ stages of change as follows:
– precontemplation: not considering assisting more than 80 percent of their tobacco-using patients to quit;
– contemplation: considering assisting more than 80 percent of their tobacco-using patients to quit in the next six months;
– preparation: planning to assist more than 80 percent of their tobacco-using patients to quit in the next month;
– action: had been assisting more than 80 percent of their tobacco-using patients to quit for less than six months;
– maintenance: had been assisting more than 80 percent of their tobacco-using patients to quit for more than six months.
We used nearly identical items to assess the providers’ readiness to offer alcohol-abuse counseling.
To assess providers’ willingness to perform oral cancer examinations, we adapted the tobacco-use cessation items as follows:
– precontemplation: no intention to provide annual oral cancer examinations to more than 80 percent of patients aged 40 years and older;
– contemplation: considering providing annual oral cancer examinations to more than 80 percent of their patients aged 40 years and older in the next month;
– preparation: planning to provide annual oral cancer examinations to more than 80 percent of their patients aged 40 years and older in the next month;
– action: having provided annual oral cancer examinations to more than 80 percent of patients aged 40 years and older for less than six months;
– maintenance: having provided annual oral cancer examinations to more than 80 percent of their patients aged 40 years and older for more than six months.
Finally, we used χ2 tests to examine potential associations between independent variables (such as age, race/ethnicity, smoking status, sex and year of graduation from dental or hygiene school) and dependent variables (such as stages of readiness to conduct oral cancer examinations and offer tobacco-use cessation and alcohol-abuse counseling). A P value of .05 or less was deemed to be significant. We used the specialized software program JMP (SAS Institute, Cary, N.C.) to perform all analyses.
RESULTS
Sociodemographic characteristics
Most dentists (62 percent) and dental hygienists (58 percent) were between 40 and 59 years old. Most of the dentists (87 percent) were male and most of the dental hygienists (99 percent) were female, and the majority of both dentists (89 percent) and dental hygienists (93 percent) identified themselves as white. There were no significant differences in demographic characteristics between responders and nonresponders, suggesting that the survey sample was representative of the population of New York-licensed oral health care providers. Eighty-two percent of the dental hygienists were in general practice and 60 percent of the dentists reported being in solo practice. The median year of graduation was 1978 for the dentists and 1983 for the dental hygienists. Thirty-eight percent of the dentists and 45 percent of the dental hygienists reported having smoked at least 100 cigarettes in their lifetimes (“ever smokers”); 12 and 22 percent of the dentists and dental hygienists, respectively, were current tobacco users (Table 1).
TABLE 1.
DEMOGRAPHIC CHARACTERISTICS OF PARTICIPANTS.
|
ORAL HEALTH CARE PROVIDER |
||
|---|---|---|
| CHARACTERISTIC | Dentists*n (%) | Dental Hygienists*n (%) |
| Age | ||
| 20–39 years | 96 (19) | 228 (36) |
| 40–59 years | 301 (62) | 365 (58) |
| 60 years and older | 98 (20) | 35 (5) |
| Sex | ||
| Male | 408 (87) | 6 (1) |
| Female | 62 (13) | 608 (99) |
| Ethnicity/Racial Group | ||
| White | 426 (89) | 576 (93) |
| African-American | 8 (2) | 12 (2) |
| Hispanic | 11 (2) | 15 (2) |
| Asian/Pacific Islander/other | 36 (8) | 13 (2) |
| Type of Practice | ||
| General practice | N/A† | 506 (82) |
| Solo practice | 292 (60) | N/A |
| Partner/employee | 129 (26) | N/A |
| Independent contractor | 21 (4) | N/A |
| Specialty practice | 20 (4) | 71 (11) |
| Public health/government/other | 26 (5) | 42 (7) |
| Ever Smokers of Tobacco | ||
| Yes | 188 (38) | 238 (45) |
| No | 304 (62) | 346 (55) |
| Current Users of Tobacco | ||
| Yes | 24 (12) | 64 (22) |
| No | 168 (88) | 228 (78) |
| Median Year of Graduation | 1978 | 1983 |
Percentages may not total 100 owing to missing responses.
N/A: Not applicable.
Oral cancer examination practice patterns
The dentists reported providing oral cancer examinations to about 86 percent (standard error [SE] = 1.42) of their patients aged 40 years and older at their initial appointments and to about 80 percent (SE = 1.63) of their patients at their recall appointments. The dental hygienists reported providing oral cancer examinations to about 79 percent (SE = 1.55) of their patients aged 40 years and older at their initial appointments and to 76 percent (SE = 1.55) of their patients at their recall appointments. The classification of the stages of change for performing oral cancer examinations to patients aged 40 and older shows that the large majority (82 percent of the dentists and 72 percent of the dental hygienists) were in the latest change stage, that of maintenance, indicating that according to the respondents, oral cancer examinations are part of their routine standard of practice (Figure 1).
Figure 1.
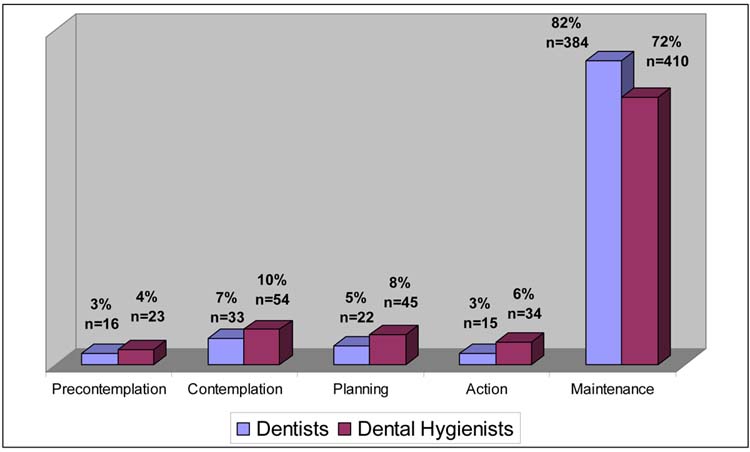
Oral health care providers’ readiness to provide oral cancer examinations. Dentists, n = 470; dental hygienists, n = 566.
Tobacco-use cessation practice patterns
Sixty-one percent of the participating dentists reported routinely asking their patients about tobacco use and advising their tobacco-user patients to quit. Only 24 percent assessed willingness to quit and even fewer (8 percent and 5 percent) reported assisting their patients in developing a quit plan and arranging for a follow-up contact, respectively. Although somewhat less frequently than among dentists, we observed similar patterns of tobacco-use cessation activities among the dental hygienists. Most of the dentists and dental hygienists reported including in their medical histories past and present use of tobacco as well as type and amount of tobacco used (Table 2).
TABLE 2.
ORAL HEALTH CARE PROVIDERS’ ORAL CANCER PREVENTION AND EARLY DETECTION ACTIVITIES.
|
ORAL HEALTH CARE PROVIDER |
||
|---|---|---|
| ACTIVITY | Dentists n (%) | Dental Hygienists n (%) |
| Oral Cancer Examinations* | ||
| Initial examination | (86) | (79) |
| Recall examination | (80) | (76) |
| Tobacco Use† | ||
| Ask | 269 (61) | 276 (48) |
| Advise | 273 (61) | 319 (55) |
| Assess | 95 (24) | 187 (34) |
| Assist | 32 (8) | 50 (9) |
| Arrange | 19 (5) | 26 (5) |
| Tobacco-Use History‡ | ||
| Present | 383 (85) | 515 (88) |
| Past | 303 (69) | 395 (69) |
| Type and amount | 288 (66) | 418 (73) |
| Alcohol Use† | ||
| Ask | 144 (33) | 94 (17) |
| Advise | 108 (26) | 63 (12) |
| Assess | 40 (10) | 34 (7) |
| Assist | 13 (3) | 8 (2) |
| Arrange | 12 (3) | 6 (1) |
| Alcohol-Use History‡ | ||
| Present | 271 (61) | 286 (50) |
| Past | 211 (48) | 198 (35) |
| Type and amount | 154 (36) | 158 (28) |
Mean percentage of patients 40 years and older to whom dentists and dental hygienists reported providing oral cancer examinations.
Number and percentage of dentists and dental hygienists who reported routinely practicing these activities.
Number and percentage of dentists and dental hygienists who reported assessing tobacco- and alcohol-use history when taking patients’ medical histories.
When we consider respondents’ readiness to adopt tobacco-use cessation counseling guidelines, only 12 percent of dentists and 21 percent of dental hygienists were in the maintenance stage, 1 percent of dentists and 3 percent of hygienists were in the action stage, 4 percent of dentists and 6 percent of hygienists were in the preparation stage, and 83 percent of the dentists and 70 percent of the dental hygienists were in the early stages of contemplation and precontemplation (Figure 2, page 600).
Figure 2.
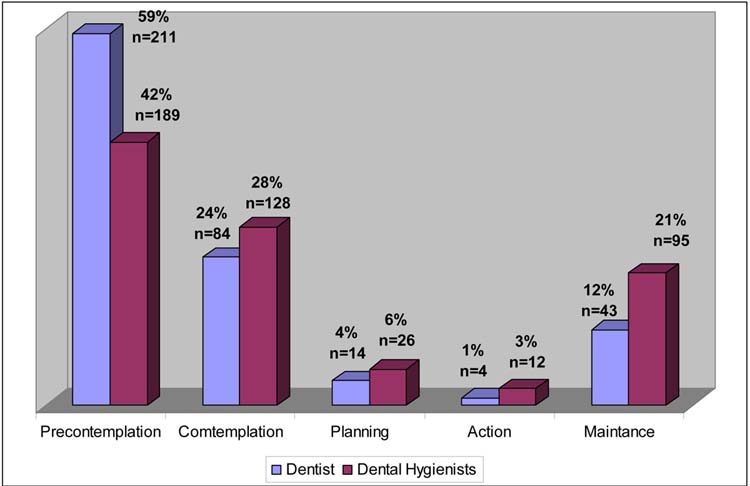
Oral health care providers’ readiness to provide tobacco-use cessation counseling. Dentists, n = 356; dental hygienists, n = 450. This includes only the providers who did not assist more than 80 percent of their patients who used tobacco in developing a plan to quit.
Alcohol-abuse counseling practice patterns
Thirty-three percent of the participating dentists reported routinely asking their patients about alcohol use; 26 percent advised their patients who were heavy alcohol users to reduce use; 10 percent assessed these patients’ willingness to reduce alcohol use and only 3 percent of the dentists reported developing an alcohol-use reduction plan and arranging for a follow-up contact. Sixty-one percent of the dentists and 50 percent of the dental hygienists reported assessing present alcohol use in their medical history taking, 48 and 35 percent of dentists and dental hygienists, respectively, assessed past alcohol use and only 36 and 28 percent, respectively, assessed type and amount of alcohol used.
Seventeen percent of the dental hygienists reported routinely asking their patients about alcohol use; 12 percent advised their patients who were heavy alcohol users to reduce use; 7 percent assessed these patients’ willingness to reduce alcohol use; and only 2 percent and 1 percent of the dental hygienists assisted their patients who were heavy alcohol users in developing an alcohol-use reduction plan and arranging for a follow-up contact, respectively. In terms of readiness to assist their heavy alcohol users in developing an alcohol-use reduction plan, only 2 percent of the dentists and 4 percent of dental hygienists were in the maintenance stage; 1 percent of dentists and 2 percent of hygienists were in the action stage; 2 percent of dentists and 5 percent of hygienists were in the preparation stage and approximately 90 percent of the dentists and dental hygienists were in the early stages of contemplation and precontemplation (Figure 3, page 600).
Figure 3.
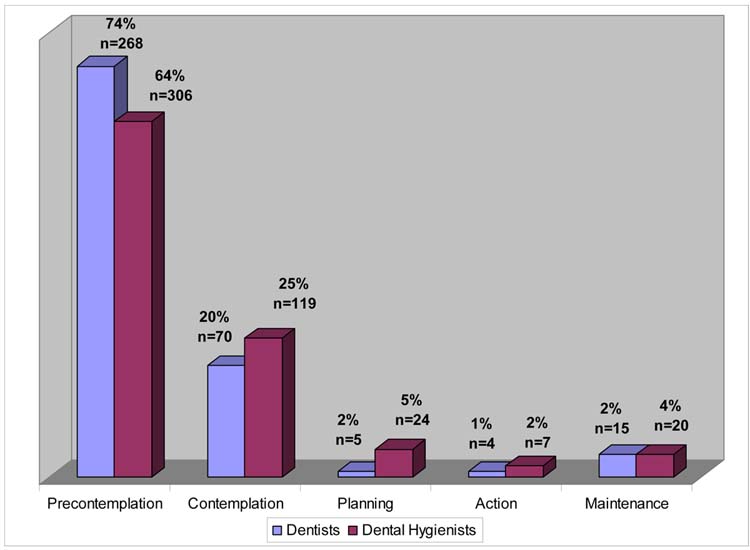
Oral health care providers’ readiness to provide alcohol-abuse counseling. Dentists, n = 362; dental hygienists, n = 476.
Bivariate analyses
Bivariate analyses examining demographics (age, sex), type of practice, year of graduation and smoking status characteristics failed to reveal any significant associations with participants’ readiness to provide tobacco-use cessation counseling, alcohol-abuse counseling or oral cancer examinations.
DISCUSSION
This is the first large-scale study to examine oral health care providers’ adoption of comprehensive efforts to promote oral cancer prevention (that is, tobacco-use and alcohol-abuse counseling) and early detection. The results of this study show underutilization of the DHHS tobacco-use cessation clinical practice guidelines among oral health care providers. Only about one-half of the dentists and dental hygienists ask and advise their patients about tobacco use, and the overwhelming majority do not assist their patients in developing a quitting plan. These results are consistent with those of other reported studies that have shown very low rates of tobacco-use counseling services among both dentists and dental hygienists.9,17
Our investigation also found that counseling patients about the oral health dangers of alcohol abuse is almost nonexistent among oral health care professionals. Furthermore, the majority of the oral health care providers who participated in this study showed low rates of readiness to provide tobacco-use cessation or alcohol-abuse assistance to their patients. No other population-based studies assessing oral health care providers’ self-reported alcohol-consumption counseling have been reported. These results denote an urgent need to develop appropriate interventions to increase primary oral cancer prevention activities in the dental practice. Accurate assessment of and provision of counseling for excessive alcohol use is extremely important not only because of its independent association with oral cancer,18 but also for its significant relationship with nutritional deficiencies, smoking habits and possibly periodontal disease.
Our finding that the large majority of oral health care providers in New York are in the early stages of readiness for offering both of these cancer prevention services represents a challenge to the profession as well as to the efforts to control oral cancer in the state. These providers must be motivated to change their behavior and must be properly trained in the requisite skills to offer these services. Furthermore, systematic barriers to adoption of these services—such as lack of proper reimbursement, lack of appropriate office systems conducive to adherence to these practices and lack of incentives to offer these services—must be overcome.
In 2001, New York state enacted a law mandating dentists to take a two-hour continuing education course on the effects of tobacco on oral health as a requirement for relicensure.19 In addition, the New York State Dental Association, with the help of a grant from the state health department, implemented a continuing education program in 2002 to meet this new statewide requirement at no cost to the practicing dentist. However, this measure alone apparently is not sufficient to change the oral cancer prevention practice patterns of dentists, as evidenced by this study’s results.
National and local campaigns aimed at increasing the rates of oral cancer examinations by oral health care providers could have a much bigger impact on the morbidity and mortality associated with this disease if the dentists and dental hygienists also are encouraged to educate their patients about the risks posed by tobacco use and alcohol abuse. Given the regularity and length of the usual dental visit, the oral health care team is uniquely positioned to promote awareness of the oral and general health risks of tobacco use and alcohol abuse, as well as the availability of evidence-based assistance programs. To adequately control and significantly reduce the burden of oral cancer in the United States, both primary and secondary prevention must become an integral part of the practice of dentistry. At the very least, tobacco-and alcohol-use assessment and advice should be a standard aspect of practice and, thus, should be adequately covered in dental and dental hygiene school curricula. Furthermore, institutions offering continuing education courses to oral health care providers should provide courses in both prevention and early detection of oral cancer.
The results presented here are limited by the self-report nature of this study. Although the rates of oral cancer examinations may be overreported by the respondents, the low rates of oral cancer prevention activities and readiness to offer these services do not indicate that this is the case in this study. In any case, the possibility that tobacco-use cessation and alcohol-abuse counseling activities actually may be occurring less frequently than reported further underscores the urgent need for training and for appropriate interventions aimed at increasing oral cancer prevention activities among oral health care providers, along with continued emphasis on the need for oral cancer examinations.
CONCLUSION AND CLINICAL IMPLICATIONS
Performing oral cancer examinations for patients aged 40 years and older seems to have been adopted as a standard practice by most oral health care providers in New York state. In contrast, greater efforts are needed to motivate oral health care providers to adopt tobacco-use cessation and alcohol-abuse counseling as part of the oral health promotion services they offer their patients. The identification of the providers’ stage of change may assist in influencing the dissemination and adoption of tobacco-use cessation and alcohol-abuse counseling guidelines by tailoring the educational interventions to the individual provider’s specific stage of readiness to adopt preventive practice behaviors.
Oral health care providers should be offered training in tobacco-use cessation and alcohol-abuse counseling. They also should be encouraged to include these services as a standard aspect of their practice, to help their patients avoid not only the devastating consequences of oral cancer but also the myriad of other tobacco- and alcohol-induced oral diseases.
Acknowledgments
The authors would like to thank Christian Salazar, Isabel Roldos and Lauren Di Leonardo for their help with data management and analysis.
Footnotes
This study was supported by National Institute of Dental and Cranio-facial Research (NIDCR) grant DE R21-DE 14425 and by the New York University Oral Cancer Research for Adult and Adolescent Health Promotion Center, an NIDCR-funded Oral Health Disparities Center, NIDCR grant U54 DE 14257.
References
- 1.Jemal A, Thomas A, Murray T, Thun M. Cancer statistics, 2002. CA Cancer J Clin. 2002;52(1):23–47. doi: 10.3322/canjclin.52.1.23. [DOI] [PubMed] [Google Scholar]
- 2.Blot WJ, McLaughlin JK, Winn DM, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48:3282–7. [PubMed] [Google Scholar]
- 3.Winn DM, Blot WJ, Shy CM, Pickle LW, Toledo A, Fraumeni JF., Jr Snuff dipping and oral cancer among women in the southern United States. N Engl J Med. 1981;304:745–9. doi: 10.1056/NEJM198103263041301. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Preventive Services Task Force. Guide to clinical preventive services: Report of the U.S. Preventive Services Task Force. Baltimore: Williams & Wilkins; 1996.
- 5.American Cancer Society. Cancer facts & figures 2003. Available at: “www.cancer.org/docroot/STT/stt_0.asp”. Accessed March 17, 2005.
- 6.Kujan O, Glenny AM, Duxbury AJ, Thakker N, Sloan P. Screening programmes for the early detection and prevention of oral cancer (Cochrane Review). The Cochrane Database of Systematic Reviews, 2003. Available at: “www.cochrane.org/cochrane/revabstr/ab004150.htm”. Accessed March 17, 2005. [DOI] [PubMed]
- 7.Martin LM, Bouquot JE, Wingo PA, Heath CW. Cancer prevention in the dental practice: oral cancer screening and tobacco cessation advice. J Public Health Dent. 1996;56:336–40. doi: 10.1111/j.1752-7325.1996.tb02461.x. [DOI] [PubMed] [Google Scholar]
- 8.Dolan TA, McGorray SP, Grinstead-Skigen CL, Mecklenburg R. Tobacco control activities in U.S. dental practices JADA. 1997;128:1669–79. doi: 10.14219/jada.archive.1997.0129. [DOI] [PubMed] [Google Scholar]
- 9.Tomar SL, Husten CG, Manley MW. Do dentists and physicians advise tobacco users to quit? JADA. 1996;127:259–65. doi: 10.14219/jada.archive.1996.0179. [DOI] [PubMed] [Google Scholar]
- 10.Hayes C, Kressin N, Garcia R, Mecklenberg R, Dolan T. Tobacco control practices: how do Massachussetts dentists compare with dentists nationwide? J Mass Dent Soc. 1997;46(1):9–14. [PubMed] [Google Scholar]
- 11.Dillman DA, Dillman DA. Mail and Internet surveys: The tailored design method. 2nd ed. New York: Wiley; 2000.
- 12.Goldstein MG, DePue JD, Monroe AD, et al. A population-based survey of physician smoking cessation counseling practices. Prev Med. 1998;27:720–9. doi: 10.1006/pmed.1998.0350. [DOI] [PubMed] [Google Scholar]
- 13.Fiore M. Treating tobacco use and dependence. Washington: U.S. Department of Health and Human Services, Public Health Service; 2000.
- 14.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–5. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 15.Wilson DM, Taylor DW, Gilbert JR, et al. A randomized trial of a family physician intervention for smoking cessation. JAMA. 1988;260:1570–4. [PubMed] [Google Scholar]
- 16.Main DS, Cohen SJ, DiClemente CC. Measuring physician readiness to change cancer screening: preliminary results. Am J Prev Med. 1995;11(1):54–8. [PubMed] [Google Scholar]
- 17.Seckler-Walker RH, Solomon LJ, Flynn BS, Dana GS. Comparisons of the smoking cessation counseling activities of six types of health professionals. Prev Med. 1994;23:800–8. doi: 10.1006/pmed.1994.1137. [DOI] [PubMed] [Google Scholar]
- 18.Huang WY, Winn DM, Brown LM, et al. Alcohol concentration and risk of oral cancer in Puerto Rico. Am J Epidemiol. 2003;157:881–7. doi: 10.1093/aje/kwg055. [DOI] [PubMed] [Google Scholar]
- 19.N.Y. Education Law Article 133 §6604-a, Mandatory continuing education for dentists. Available at: http://public.leginfo.state.ny.us/menugetf.cgi?COMMONQUERY=LAWS Accessed April 6, 2005.


