Abstract
Objective
To examine whether nursing homes would behave more efficiently, without compromising their quality of care, under prospective payment.
Data Sources
Four data sets for 1994: the Skilled Nursing Facility Minimum Data Set, the Online Survey Certification and Reporting System file, the Area Resource File, and the Hospital Wage Indices File. A national sample of 4,635 nursing homes is included in the analysis.
Study Design
Using a modified hybrid functional form to estimate nursing home costs, we distinguish our study from previous research by controlling for quality differences (related to both care and life) and addressing the issues of output and quality endogeneity, as well as using more recent national data. Factor analysis was used to operationalize quality variables. To address the endogeneity problems, instrumental measures were created for nursing home output and quality variables.
Principal Findings
Nursing homes in states using prospective payment systems do not have lower costs than their counterpart facilities under retrospective cost-based payment systems, after quality differences among facilities are controlled for and the endogeneity problem of quality variables is addressed.
Conclusions
The effects of prospective payment on nursing home cost reduction may be through quality cuts, rather than cost efficiency. If nursing home payments under prospective payment systems are not adjusted for quality, nursing homes may respond by cutting their quality levels, rather than controlling costs. Future outcomes research may provide useful insights into the adjustment of quality in the design of prospective payment for nursing home care.
Keywords: Nursing home cost, prospective payment, quality of care, quality of life
With an aging population, American society has faced an increasing demand for nursing home care. Consequently, nursing home expenditures have increased significantly from $20 billion in 1980 to more than $87 billion in 1998 (Levit, Cowan, Lazenby, et al. 2000; Rosko et al. 1995). As a result, the cost of nursing home care has become a key area of public policy concern. To control nursing home expenditures effectively, Medicaid programs in many states have shifted from retrospective cost-based system to prospective payment system (PPS). In addition, the Medicare program has recently implemented a per diem PPS for its beneficiaries who seek skilled nursing facility (SNF) care in nursing homes. The underlying assumption behind recent payment changes for nursing homecare is that prospective payments would drive greater efficiency, thus helping tocontain the growth of nursing home expenditures. However, the effects ofprospective payment in controlling nursing home costs remain unknown.
Although a few previous studies addressed the impact of prospective payment on nursing home costs, most of them do not control for quality variables or output and/or quality endogeneity in their studies. In addition, most of these studies used data prior to 1987, when the Nursing Home Reform Act of the Omnibus Budget Reconciliation Act (OBRA) was passed and nursing homes were required to provide a higher quality of care to their patients. It is unknown how nursing homes responded to the changes in their regulatory environment in terms of their operational efficiency and quality. To fill this gap in the nursing home literature, we investigated the impacts of prospective payment on nursing home costs using more recent national data. Our study also tried to minimize the cost function estimation biases from which the previous studies have suffered.
Previous Research
Empirical evidence has shown inconclusive results regarding the effect of prospective payments on nursing home costs. A number of nursing home cost studies indicate that prospective payment has lowered nursing home costs when compared with cost-based reimbursement (Bishop and Dor 1994; Dor 1989; Meiners 1982; Thorpe, Gertler, and Goldman 1991). On the other hand, some studies show that prospective payment either may not lower nursing home costs or may achieve cost savings through reductions in access and quality of care. For instance, Sexton et al. (1989) used Data Envelopment Analysis to estimate the relative efficiencies of nursing homes in Maine before and after the implementation of a PPS. They found nursing homes became less efficient after the introduction of prospective reimbursement. In addition, Coburn et al. (1993) suggested that nursing homes under prospective reimbursement may reduce access of Medicaid patients. Moreover, although finding that the PPS lowers nursing home costs, Cohen and Dubay (1990) suggested the savings are achieved through decreasing case mix or lowering staff levels by nursing homes.
The inconclusive results regarding the effectiveness of the PPS in previous studies may stem from the difficulty in estimating nursing home cost function. For instance, some studies used capacity measures (e.g., number of beds, occupancy rate) as their output variable. These measures do not really reflect the magnitude of output produced by nursing homes. Although some studies used a better measure, such as number of patients, the great variation in the length of stay among patients still makes this measure inappropriate. Although the use of payment-type (Medicare/Medicaid/private) patient days by Bishop and Dor (1994) and Dor (1989) may correct for output measurement errors by reflecting length of stay as well as the disparity in case mix among different payer types of patients, admission and discharge practices may be based on the patient's payment source. As a result, patient's length of stay may be “manipulated” in nursing homes (Breyer 1987; Frank and Lave 1985; Freiman and Murtaugh 1993; Grannemann, Brown, and Pauly 1986; Vitaliano 1987). The ability of nursing homes to manipulate patients' length of stay, based on their payment sources, indicates that payment-type patient days (e.g., Medicare days) should not be considered as exogenous variables in the cost function.
Because nursing homes have some ability to choose their quality level, quality must be regarded as a choice of the firm. As a result, in a cost function, quality cannot be considered as an exogenous variable, either. Gertler and Waldman (1992) suggested that a nursing home cost function that treats quality as exogenous produces misleading estimates of coefficients. Davis and Provan (1996) also suggested that quality orientation is a function of a nursing home's emphasis on cost control or cost consideration. Their argument about quality as a function of cost consideration indicated that quality should not be considered exogenous to cost in the nursing home cost function.
In addition, previous research did not adequately investigate whether the cost reduction of nursing homes, if any, comes from more efficient operation or from other sources. Efficiency would mean the nursing home produces the same output at lower cost. However, nursing homes might lower costs, but also reduce quality. In effect, this is not improved cost efficiency because one output of the nursing home—quality—has been changed. Because most previous studies did not control for quality and/or case-mix variable in their cost functions, their findings on the effect of PPS on cost could be misleading. More importantly, almost none of the previous studies controlled for quality of life or addressed the possible endogeneity of quality variables. Quality of life, in addition to quality of care, is an important construct that needs to be measured and controlled for in the nursing home cost function. Nyman and Geyer (1989) suggested that “nursing home patients are in fact living in these health care institutions and that the quality of their lives within these institutions may be at least as important as the quality of the health care they receive there” (p. 797).
Data
Sources of Data
The data for this study come from four different sources: The Skilled Nursing Facility Minimum Data Set (SNF-MDS) contains cost and patient utilization information for all skilled nursing facilities (SNFs) and nursing facilities (NFs) in the United States. The Online Survey Certification and Reporting System (OSCAR) provides survey and certification information for facilities. The Area Resources File (ARF) provides information that describes the socioeconomic and demographic environment in which nursing homes are operated. Aggregate area wage indices were extracted from the Hospital Wage Indices File (HWAGIF) to reflect the wage level of each specific area where facilities are located. For all of the four data sources, the information for the calendar year 1994 was used.1
The nursing home facility, either a SNF or a NF,2 is the unit of analysis. After merging the SNF-MDS and the OSCAR file by provider identification number, 10,022 records of facilities with data from both sources were obtained. After excluding those records with either incomplete cost information or missing information on key regression variables, 4,635 facilities were finally used in our analyses.3
Operationalization of Variables
Medicaid Payment Methods for Nursing Home Care
Payment methods for nursing home care vary greatly from state to state under the Medicaid program. The information regarding the 1994 Medicaid payment methods for nursing home care in all individual states was obtained from the Medicaid Reimbursement Survey by a research team at the University of California in San Francisco and Wichita State University.4 Three dichotomous variables were created to indicate the measures of state Medicaid payment policy. COMBINATION equals 1 if a facility was located in a state where some form of a combination of retrospective and prospective payment methods was used in 1994. These combinations include a prospective payment method in which the rate could be adjusted upward. FACILITY-SPECIFIC PPS equals 1 if a facility was located in a state where the payment rate was predetermined based on their individual situations. CLASS PPS equals 1 if a facility was located in a state where the payment rate was predetermined based on the situations of an entire group to which a facility belongs. The facilities that were located in states where a retrospective system was implemented were used as the reference group in the regression analyses. The more flexible and facility-specific the payment is, the less financial risk a facility faces. Therefore, the degree of financial risk imposed on nursing homes ascends from retrospective, combination, facility-specific prospective, to class prospective.
Other Explanatory Variables
Nursing Home Outputs
Three types of patient days are used as the nursing home output measures: Medicare days, Medicaid days, and private days. As discussed earlier, the use of the payment-type output measures could cause endogeneity problems, and thus, we created instrumental measures for these output variables (Method section).
Nursing Home Input Prices
Wage information specific to nursing homes is not available from national data sources, so the 1994 area wage indices from the HWAGIF were used as proxy indicators of nursing home labor wages. The logarithm form of wages was used in the regression analyses of nursing home cost function.
Quality of Nursing Home Outputs
Using Donabedian's (1966) conceptual model of health care quality, this study measures nursing home quality from three aspects: structural, process, and outcome. Both quality of life and quality of care are measured. Based on this conceptual framework, 19 variables were created from the OSCAR file, including 10 staffing ratios (e.g., RNs, LPNs), 5 process-related quality indicators (e.g., physical restraint rate), and 4 regulatory deficiency variables (e.g., number of life safety code deficiencies). A principal component factor analysis was used to integrate this information into seven more meaningful variables.5 For example, the ratios on RNs, LPNs, nurse aides, and pharmacists fall in the same group so that they were combined into one variable that measures the per resident ratio of full-time equivalent (FTE) personnel who can contribute to quality of care for nursing home residents. Similarly, another structural quality indicator was created to measure the per resident ratio of the FTE personnel who can contribute to quality of life for nursing home residents. These personnel include mental health professionals, social workers and staff, food service staff, dietitians, housekeeping staff, activity professionals and staff, and various kinds of professional therapists and therapy staff.6 The prevalence rates of catheterization, physical restraints, and drug administration error in a nursing home, which stand alone in the factor analysis, were used as care-related process quality variables. According to literature, the practices of catheterization and physical restraints have great negative impacts on the quality of care for nursing home residents (Zinn 1994). Another process quality variable is related to quality of life. It indicates a facility's degree of involvement in the provision of organized groups for its residents and their families. Participation in organized group activities may enrich the lives of nursing home residents, and the provision of group organization is also a signal that demonstrates the willingness and determination of a facility to improve the quality of life of its residents. The last quality variable is the number of regulatory deficiencies for a nursing home facility (a combination of four individual deficiency variables).7 This is a proxy measure for the outcome element of nursing home quality. Although it may not directly reflect the outcomes of nursing home patients, the assumption is that patients in a facility with more violations have greater chances to produce poorer outcomes. The values of catheterization rate, physical restraint rate, drug error rate, and regulatory deficiencies were transformed into negative values so that all quality measures have the same direction that the greater the values are, the higher the quality is indicated.
Case Mix Indicator of Nursing Home
An indicator score was calculated for each facility using activity-of-daily-life (ADL) information. These ADLs include eating, dressing, bathing, toilet use, and transferring. For each ADL, different weights were given to patients with different degrees of functional dependence. Then ADL-specific case-mix scores accounting for patient composition were calculated for each facility.8
By summing all five ADL scores, a general case-mix index was obtained for each facility, ranging from 0 to 10. A higher value indicates a facility had a more severe case mix of patients in terms of their patients' functional dependence.
Organizational Structure of Nursing Homes
Using government-owned nursing homes as the reference group, two dichotomous variables (profit and nonprofit) were created to indicate the nature of ownership for nursing homes. In addition, two non-mutually-exclusive dichotomous variables were created to indicate whether a facility is hospital based and if a facility is owned by a chain organization, respectively.
Environmental Descriptors of Nursing Home Markets
A county-based Herfindahl measure was created using private patient day variable to control for the degree of competition in nursing home markets. The value ranges from 0 to 1, with higher values indicating higher concentration. Using rural facilities as the reference group, two dummy variables were created to indicate whether a facility was located in a metropolitan county and whether a facility was located in a smaller urban county, respectively. Finally, eight dummy variables were created to indicate the geographic locations of nursing homes. The facilities located in the Pacific area were used as the reference group in the regression analyses.
Dependent Variable
This study focuses on the investigation of short-term operating costs of nursing homes. The total operating cost of a facility in 1994 was created, from the SNF-MDS, by summing up salary costs and other direct costs in 1994 for each facility. The logarithm form of the total cost was used in the regression analyses.
Methods
Creation of Instrumental Measures for Nursing Home Output and Quality Variables
To resolve endogeneity, we used two-stage least square (2SLS) to create instrumental measures for the three payment-type patient day variables as well as the three process quality of care variables. The decision to focus only on these three quality variables is based on the assumption that in the short run, they are more likely to be “manipulated” (than the other four) by nursing homes in response to their financial concerns.9 Table 1 shows the results of the first-stage regressions for these suspected endogenous variables. The ordinary least square (OLS) model was used for Medicare days, private days, catheterization rate, and physical restraint rate. The Tobit model was used to predict Medicaid days and drug error rate.10
Table 1.
The Results of the First-Stage Regressions for Suspected Endogenous Variables in the 2SLS
| Coefficients Under Each Dependent Variable Model | ||||||
|---|---|---|---|---|---|---|
| Care-Related Process Quality Variables | Patient Day Variables | |||||
| Explanatory variables | (OLS) Catheterization | (OLS) Restraint | (Tobit) Drug error | (OLS) Medicare | (Tobit) Medicaid | (OLS) Private |
| Intercept | 13.17‡ | 31.48‡ | 0.86‡ | −738.70† | 9.49‡ | 5539.91 † |
| County-level variables | ||||||
| %Population 65+ | 19.75 | 8.54 | 5.07 | 5,592.93 | 3.66‡ | −53,031.00* |
| %Population 75+ | −1.48 | −46.68 | −13.75 | 29,288.00 † | −21.81‡ | 137,517.00 |
| %Population 84+ | −255.46‡ | −86.10 | −5.87 | −125,661.00‡ | 44.21‡ | 39,136.00 |
| Income | 8.12E −5† | −3.25E −5 | 7.15 −6 | 0.05‡ | −7.13E −6‡ | 0.09 |
| Poverty | 0.005* | −0.003 | 0.002‡ | 0.78 | −0.0004 † | −9.84* |
| Facility-level variables | ||||||
| Number of beds | 0.028‡ | −0.01 | −0.003‡ | 4.56‡ | 0.001‡ | 37.07‡ |
| Number of certified beds | −0.04‡ | 0.027‡ | 0.002 † | 13.08‡ | 0.005‡ | 105.14‡ |
| Profit ownership | −3.83‡ | −4.63‡ | 0.28 | |||
| Nonprofit ownership | −3.48‡ | −5.21‡ | 0.47‡ | |||
| State or Region-level variables | ||||||
| Combination | −2.09‡ | −12.24‡ | −0.04 | |||
| Facility-specific PPS | −1.74 † | −5.02‡ | 0.12 | |||
| Class PPS | 0.20 | 1.13 | 0.51 † | |||
| New England | −1.84‡ | 5.33‡ | 0.58‡ | |||
| Mid-Atlantic | −1.69 † | −0.22 | 0.56‡ | |||
| South Atlantic | 0.48 | 3.70‡ | 0.37‡ | |||
| East North Central | 1.34 † | 5.28‡ | 0.19* | |||
| East South Central | 2.18‡ | 6.82‡ | 0.11 | |||
| West North Central | 0.73 | 2.19 | 0.16 | |||
| West South Central | 7.08‡ | 1.07 | 0.37‡ | |||
| Mountain | −0.03 | 1.86 | 0.49‡ | |||
| R2 | 0.10 | 0.08 | 0.25 | 0.23 | ||
| Likelihood Ratio | 99.94‡ | 1,776.14‡ | ||||
| F-statistics | 27.48‡ | 22.36‡ | 240.22‡ | 215.47‡ | ||
Note: The above statistical results of coefficients come from t-test for the two OLS models and from chi-square test for the Tobit model.
p <0.10.
p <0.05.
p <0.01.
We also used the Hausman test to do an empirical examination of endogeneity. The results of this test indicated that output (payment-type patient days) and quality (quality of care process) variables are not exogenous to nursing home costs (p <0.005).11
Model Specification of the Nursing Home Cost Function
We used a hybrid functional form to estimate nursing home costs because the hybrid form combines the “economic rigor” and the specification flexibility of the translog form and the “intuitive appeal” of the ad hoc approach (Nyman 1988).12
In addition, the hybrid form allows for zero value for output variables and does not involve as many interaction terms for independent variables as a translog form does (Dor 1989; Grannemann, Brown, and Pauly 1986; Nyman 1988). The hybrid model used in this study was derived by modifying the equations in the studies by Dor (1989), Nyman (1988), and Grannemann, Brown, and Pauly (1986). The total cost function equation can be expressed as:
By taking the logarithm form for both sides of the above total cost function equation, the hybrid cost function is specified as follows:
In this equation, C is the total operating cost of a nursing home facility in 1994, P is the input price of nursing home, X is a vector of variables that describe the nature and environments of nursing homes, and f is a function that describes the amount (output quantity Y ) and the feature (case-mix CM and quality Q) of the outputs of a nursing home in 1994; f was specified as the following functional form:
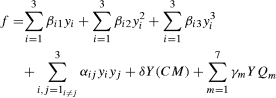 |
where Y = y1 + y2 + y3; and y1, y2, and y3 represent the instrumental measures for the 1994 Medicare days, Medicaid days, and private days served by a nursing home, respectively. CM is the patient case-mix score of a nursing home. Q1 through Q7 represent the seven quality indicator variables. Instrumental measures were used for the three quality of care process variables. To make sure that all quality indicator variables have the same direction so that higher number indicates higher quality, we transformed the values of three prevalence rate variables and the deficiency variable into negative values.
X includes Medicaid payment methods, ownership indicators, the affiliation status (hospital-based and chain status), the interaction term variables between ownership and chain status, the market concentration indicator variable, the degree of environmental urbanization, and the geographic location of nursing homes. The OLS approach was used to estimate the nursing home hybrid cost function.
Results
Table 2 shows the descriptive statistics for dependent and explanatory variables used in the regression analysis. Table 3 shows the results of regression.
Table 2.
The Descriptive Statistics of the Regression Variables
| Variable (The Number of Facilities=4,635) | Mean | Standard Deviation |
|---|---|---|
| (Dependent variable) Logarithm of total cost (Explanatory variables) | 15.05 | 0.78 |
| Medicare days* | 2,866.80 | 1,435.71 |
| Medicaid days* | 30,575.63 | 105,216.22 |
| Private days* | 22,412.38 | 10,793.13 |
| Logarithm of wage | 9.17 | 0.19 |
| Care personnel ratio | 86.07 | 209.34 |
| Life personnel ratio | 49.25 | 230.88 |
| Catheterization rate‡* | −8.79 | 2.95 |
| Physical restraint rate‡* | −20.73 | 5.01 |
| Drug error rate‡* | −4.51 | 1.22 |
| Group organization indicator | 1.49 | 0.58 |
| Number of regulatory deficiencies‡ | −1.0 | 1.19 |
| ADL indicator | 5.91 | 0.98 |
| Profit ownership | 0.72 | 0.45 |
| Nonprofit ownership | 0.24 | 0.42 |
| Hospital based | 0.08 | 0.27 |
| Chain owned | 0.58 | 0.49 |
| Herfindahl indicator | 0.32 | 0.34 |
| Combination | 0.48 | 0.50 |
| Facility-specific PPS | 0.35 | 0.48 |
| Class PPS | 0.11 | 0.31 |
| Metropolitan located | 0.73 | 0.44 |
| Urban located | 0.24 | 0.43 |
| New England | 0.08 | 0.28 |
| Mid-Atlantic | 0.18 | 0.38 |
| South Atlantic | 0.11 | 0.31 |
| East North Central | 0.23 | 0.42 |
| East South Central | 0.05 | 0.22 |
| West North Central | 0.08 | 0.28 |
| West South Central | 0.06 | 0.24 |
| Mountain | 0.05 | 0.22 |
Note:
Instrumental variables.
These variables have been transformed into negative values to indicate the same direction as other quality variables. Therefore, their mean values are negative.
Table 3.
The Regression Results of the Nursing Home Cost Function Estimation (Dependent Variable: Logarithm of Total Cost; n = 4,635)
| Variable | Coefficient | T-statistics |
|---|---|---|
| Intercept | 7.04*** | 14.47 |
| Medicare days | 0.0007*** | 9.92 |
| (Medicare days) 2 | −1.16E−7*** | −4.64 |
| (Medicare days) 3 | 1.23E−11*** | 6.28 |
| Medicaid days | 0.000006 | 1.49 |
| (Medicaid days) 2 | −4.73E−12** | −2.39 |
| (Medicaid days) 3 | 6.93E−19*** | 2.78 |
| Private days | −0.00002 | −1.39 |
| (Private days) 2 | 2.52E−9*** | 4.38 |
| (Private days) 3 | −2.84E−14*** | −4.55 |
| (Medicare days) (Medicaid days) | −2.85E−9*** | −3.41 |
| (Medicare days) (private days) | −1.04E−8** | −2.15 |
| (Medicaid days) (private days) | 3.73E−10*** | 2.59 |
| Logarithm of wage | 0.73*** | 14.07 |
| (Care personnel ratio) (total days) | 1.56E−9* | 1.68 |
| (Life personnel ratio) (total days) | −6.11E−10 | −0.78 |
| (Catheterization rate) (total days) | 2.0E−7*** | 2.93 |
| (Physical restraint rate) (total days) | −6.27E−8*** | −3.17 |
| (Drug error rate) (total days) | 3.36E−7** | 2.41 |
| (Group organization indicator) (total days) | 6.72E−7*** | 4.09 |
| (# of regulatory deficiencies) (total days) | 1.20E−7*** | 2.90 |
| (ADL indicator) (total days) | 1.46E−7 | 1.59 |
| Profit ownership | −0.26*** | −7.37 |
| Nonprofit ownership | 0.02 | 0.42 |
| Urban located | 0.03 | 0.79 |
| Metropolitan located | 0.06* | 1.73 |
| Hospital-based | −1.09*** | −42.25 |
| Chain-owned | 0.17 | 1.04 |
| (Chain-owned) (profit ownership) | −0.09 | −0.55 |
| (Chain-owned) (nonprofit ownership) | −0.20 | −1.20 |
| Herfindahl concentration index | −0.15*** | −6.43 |
| Combination | 0.02 | 0.77 |
| Facility-specific PPS | −0.03 | −1.00 |
| Class PPS | −0.07 | −1.50 |
| New England | 0.11*** | 3.22 |
| Mid-Atlantic | 0.20*** | 5.98 |
| South Atlantic | 0.20*** | 6.01 |
| East North Central | 0.07*** | 2.62 |
| East South Central | 0.18*** | 4.84 |
| West North Central | 0.0007 | 0.02 |
| West South Central | 0.05 | 1.31 |
| Mountain | 0.08** | 2.30 |
| R2 | 0.77 | |
| F statistics | 376.34*** |
Note:
Significant at p <0.10
Significant at p <0.05
Significant at p <0.01.
Catheterization rate, physical restraint rate, drug error rate, and regulatory deficiencies are transformed into negative values so that greater values indicate higher quality.
According to the regression results in Table 3, quality of output is a strong predictor of cost, and higher quality predicts higher cost in nursing homes. Six of the seven quality-output interaction variables are statistically significant. The coefficients of these six variables all indicate that higher nursing home quality predicts higher costs, except for the physical restraint rate variable. These results confirm the importance of controlling for quality variation from various perspectives. The positive effects of nursing home quality on cost were calculated and listed in Table 4. The improvement in process-related quality indicators seems to cost more than that in structural indicator or regulatory compliance. In particular, the marginal increase by organizing a resident group or a family group would lead to an increase of $131,439 (3.8 percent) in the annual total cost for an average nursing home with 55,853 patient days in 1994. These findings on cost of quality improvement in nursing homes will provide useful information for the evaluation of cost-effectiveness of alternative quality initiatives in this industry.
Table 4.
The Estimated Effects of Nursing Home Quality on Cost
| Quality Indicator | Improvement in Quality | Resulting Change in Annual Total Cost ($) | Change as % of Annual Total Cost |
|---|---|---|---|
| Care-related personnel* | Increase by 1 FTE staff per resident | Increase by $299 | +0.009% |
| Catheterization rate | Decrease by 1% | Increase by $38,604 | +1.1% |
| Drug error rate | Decrease by 1% | Increase by $65,103 | +1.9% |
| Group organization** | None → One Type or One Type → Both | Increase by $131,439 | +3.8% |
| Regulatory deficiencies | Decrease by 1 citation | Increase by $23,111 | +0.7% |
Care-related personnel includes RNs, LPNs, nurse aides, pharmacists, and medication aides.
“Group organization” was coded as a category variable: it equals 0 if there is no group organization activities in a facility; it equals 1 if there is one type of activity (resident or familygroup) in a facility; and it equals 2 if there are both resident and family groups in a facility.
None of the three Medicaid payment method variables are significant. According to our results, nursing homes located in the states where a PPS is implemented do not appear to have lower costs than their counterpart facilities under a cost-based retrospective payment system. If correct, this implies that prospective payments may not be truly effective in containing nursing home costs. Because this result is inconsistent with conventional wisdom, another model that does not address the endogeneity problems of nursing home quality variables was run to illustrate the differences in estimates of key policy parameters, and the results are shown in Table 5.
Table 5.
The Regression Results of the Nursing Home Cost Function for the Model that Does Not Address the Endogeneity Problem of Quality Variables (Dependent Variable: Logarithm of Total Cost)
| Variable | Coefficient | T statistics |
|---|---|---|
| Intercept | 6.37*** | 13.25 |
| Medicare days | 0.0007*** | 9.54 |
| (Medicare days) 2 | −9.34E−8*** | −3.87 |
| (Medicare days) 3 | 1.02E−11*** | 5.41 |
| Medicaid days | 0.000006* | 1.67 |
| (Medicaid days) 2 | −3.58E−12* | −1.75 |
| (Medicaid days) 3 | 5.71E−19** | 2.19 |
| Private days | −0.000009 | −0.71 |
| (Private days) 2 | 2.24E−9*** | 3.85 |
| (Private days) 3 | −2.25E−14*** | −3.61 |
| (Medicare days)(Medicaid days) | −2.47E−9*** | −3.12 |
| (Medicare days)(private days) | −1.21E−8** | −2.48 |
| (Medicaid days)(private days) | 3.12E−10** | 2.22 |
| Logarithm of wage | 0.79*** | 15.10 |
| (Care personnel ratio)(total days) | 1.59E−9* | 1.67 |
| (Life personnel ratio)(total days) | −6.62E−10 | −0.82 |
| (Catheterization rate)(total days) | 3.85E−8*** | 2.80 |
| (Physical restraint rate)(total days) | 6.04E−9 | 1.35 |
| (Drug error rate)(total days) | −2.13E−8 | −0.97 |
| (Drug error rate)(total days) | 0.0000006*** | 3.54 |
| (# of regulatory deficiencies)(total days) | −9.46E−9*** | −2.90 |
| (ADL indicator)(total days) | 7.31E−8 | 0.79 |
| Profit ownership | −0.23*** | −7.53 |
| Nonprofit ownership | −0.04 | −1.39 |
| Urban located | 0.07** | 1.98 |
| Metropolitan located | 0.15*** | 4.33 |
| Hospital-based | −1.08*** | −42.76 |
| Chain owned | 0.05*** | 4.14 |
| (Chain owned)(profit ownership) | −0.10 | −0.59 |
| (Chain owned)(nonprofit ownership) | −0.20 | −1.23 |
| Herfindahl concentration index | −0.16*** | −6.93 |
| Combination | 0.02 | 0.53 |
| Facility-specific PPS | −0.03 | −0.87 |
| Class PPS | −0.09** | −2.05 |
| New England | 0.11*** | 3.78 |
| Mid-Atlantic | 0.20*** | 6.10 |
| South Atlantic | 0.18*** | 5.57 |
| East North Central | 0.05** | 2.11 |
| East South Central | 0.13*** | 3.50 |
| West North Central | −0.02 | −0.54 |
| West South Central | −0.04 | −1.42 |
| Mountain | 0.01 | 0.32 |
| R2 | 0.77 | |
| F statistics | 422.32*** | |
| n = 4,635 |
Note:
Significant at p <0.10
Significant at p <0.05
Significant at p <0.01.
According to Table 5, the class prospective variable is statistically significant and has a negative coefficient. This seems to indicate that nursing homes located in the states where a class PPS is implemented for Medicaid have lower costs than their counterpart facilities under a cost-based retrospective Medicaid payment system. Examining the results from this model, where quality endogeneity is not controlled for, would lead to the conclusion that prospective payment for nursing homes reduces costs. However, as discussed previously, the findings of this study, as well as those of Mukamel (1997), indicate that quality is positively associated with cost in nursing homes (Table 3). What the comparison between these two models suggests is that the cost savings found in those nursing homes under PPS shown in Table 5 may be achieved through quality cuts because nursing home quality is not appropriately controlled for in this cost function. To the extent that the results in Table 3 appropriately control for quality, they suggest that costs may be lower under prospective payment because quality is reduced. As further research on the appropriate model specification and in measuring quality for nursing homes continues, it will be important to continue to test this finding, identify areas where quality is reduced, and develop new payment methods that provide incentives for both quality care and efficient cost.
Most of the results in Table 3 on other controlled variables comply with either the findings of previous research or the common wisdom. For instance, scale and scope economies exist for nursing home care. For-profit facilities had lower costs than their counterpart facilities. Those facilities located in a metropolitan area or in the Northeast region had higher costs, and there is a positive association between wage and nursing home costs.
Limitations
One limitation of this study is the correlation between the instruments and their corresponding suspected endogenous variables is not very strong because of the low R2 in the first stage regressions of the 2SLS (although the F statistics and likelihood ratio tests show a satisfactory model goodness of fit). This is especially true for the quality instruments. The limited availability of our data on the exogenous information that can be used to create instruments results in the relatively low correlation between our instruments and the suspected endogenous variables. Future research using improved output and quality instruments is suggested. Another limitation is the wage information used in our regression analysis is not facility specific because our data do not provide this type of information. Using facility-specific wage data may better account for the variation in costs among nursing homes. In addition, some degree of heteroskedasticity may exist because of the use of county-level Herfindahl index and region-level wage data in the regression model, where facility is the unit of analysis. Moreover, our results were based on a sample that may not be well representative of nursing homes across the country.3 We should be cautious when applying these results.
Discussion
The results of our study show that quality does have a positive effect on cost in the nursing home industry. This result has important implications on nursing home policies because of the significant changes in the nursing home industry within the last two decades. Nursing homes have been “held to higher standards of accountability… particularly with respect to the quality of care” (Castle et al. 1997, p. 43). On the one hand, under the Nursing Home Reform Act of the OBRA 1987, nursing homes must meet more (e.g., patient rights and patient assessment) and higher (e.g., training for nurse aides) quality requirements to be eligible for Medicare/Medicaid reimbursement. Also, under the new law, nursing homes will face more stringent penalties if they violate the regulation. On the other hand, the increasing stringency of Medicare and Medicaid payments and the growing role of the managed care in long-term care financing have compelled nursing homes to compete increasingly for private pay patients on the basis of quality and price. In addition, increasing competition between nursing homes and hospitals (for postacute care patients) and home care providers (for lower acuity level patients) will force nursing homes to enhance their quality of care and services (Castle et al. 1997).
Under the newly shaped operating environment, nursing homes are expected to provide higher quality of services to their customers than ever before. In fact, some evidence suggests that the quality of care has been improved in terms of the declining use of physical restraints and psychotropic medications as well as the decreasing likelihood of residents' hospitalization and functional decline in nursing homes since the implementation of the OBRA 1987 (Castle et al. 1997; Phillips, Hawes, and Mor 1996). Based on the previously mentioned observation and the results of our study, nursing homes right now may have higher costs than ever before because of their enhanced quality.
The research findings also show that the PPS is not more effective in containing nursing home costs than the cost-based retrospective payment system. The common thoughts and expectation that nursing homes under PPS have lower costs than their counterpart facilities under a cost-based retrospective payment system may be misleading. The “cost savings” of these nursing homes under PPS may result from quality cuts. In other words, these facilities may not operate more efficiently in response to the financial incentives of PPS. Instead, they may cut the quality level provided to their patients to reduce their production costs. This response, however, can only take place in certain ways. Because of continued concerns about quality of care in nursing homes (Institute of Medicine 1986), nursing homes have faced increased regulatory restraints on quality in recent years. These regulations have increasingly focused on patient care process and outcomes issues, in contrast to previous regulations that addressed structural aspects of quality. Our results suggest that if prospective payment is not coupled with some method of monitoring quality, payers may find costs and quality reduced. Payers who care about both cost efficiency and quality must find ways to link PPS to measures of quality to reward those who achieve both desired outcomes.
To contain nursing home costs, there has been an increasing industry trend, regardless of payer source, toward a capitation payment system. Since 1998, Medicare has also implemented PPS for the care of its beneficiaries (those who need postacute care) in nursing homes. Most state Medicaid programs right now adopt either a prospective or a mixed system, which combines PPS and retrospective methods for the nursing home care of their recipients. With the increasing penetration of managed care in the market of nursing home care, the prospective payment method is expected to dominate this industry further. However, although the original intent of prospective payments was to drive nursing homes toward greater efficiency, the lack of adjusting for quality in payments may lead to reductions in quality of patient care. To contain nursing home costs effectively, it is important for policymakers and legislators to take quality into account when designing prospective payments for nursing home care.
Although the adjustments of Medicare/Medicaid nursing home payments by provider quality may still challenge health services researchers and policymakers because of the great difficulties in accurately measuring nursing home quality, outcomes research in recent years may provide some rich insights into this issue. Promoting quality of care and controlling costs have been two of the most critical goals of long-term care policies in the United States. The design of PPS clearly serves the purpose of cost containment. However, as we have discussed, prospective payments may not effectively contain nursing home costs in that the cost savings may result from the compromise in quality of care and life of nursing home patients. These negative consequences are certainly beyond the initial expectation of policymakers and legislators. Therefore, we need to be very careful in designing any regulatory initiative that serves public goals. Public goals, like the case discussed here, could sometimes be compromised instead of accomplished by regulation.
Acknowledgments
This article was presented at the 127th annual meeting of the American Public Health Association. The authors would like to thank Joe Vasey for his assistance in the process of data analysis and Dr.Stephen Foreman, Dr. Diane Brannon, and two anonymous reviewers for their insightful comments.
Notes
The only exceptions are some demographic variables created from the ARF. Because the 1994 information for these variables is not available in the ARF, data from 1989 and 1990 were used as proxy information.
A SNF provides care to patients with a higher level of acuity and a NF provides care to patients who need custodial care. Because the great majority of nursing homes (73.2 percent) in the United States are certified both as a Medicare SNF and as a Medicaid NF (MEPS 1996), we did not separate SNFs from NFs in the analysis.
A number of facilities were dropped from our sample because they did not have complete cost information for the entire period of the 1994 calendar year. The reason for this was that cost data were reported based on fiscal-year schedule so that some facilities ended (or began) their reporting before December 31, 1994 (or after January 1, 1994). We did a series of t tests on the means of variables between our analytic sample (n = 4,635) and the excluded sample (n = 5,387). The results show that facilities from both samples had no statistically significant difference (p <0.05) in their patients' case mix and two quality indicators (prevalence of physical restraint and drug error rate), although the other quality variables were significantly different across these two samples. In addition, the analytic sample had a significantly greater proportion of metropolitan-located, free-standing, and for-profit facilities than the excluded sample did. However, the disparity was reduced when the analytic sample was compared with the national sample (n = 16,840) from the 1996 MEPS. In general, the analytic sample was more representative of nursing homes across the nation than the excluded sample was.
We would like to express our appreciation for the permission to use these 1994 state Medicaid payment method data from Dr. James H. Swan and Dr.Charlene Harrington.
The detailed results of the factor analysis are available from the authors by request.
To test the validity of the constructed structural quality measures (e.g., care-related staff ratio), which were obtained by adding up multiple individual personnel ratios (e.g., RNs, LPNs) based on the factor analysis results, we ran another cost function regression using all individual staff ratios (results are available from the authors by request). There is no significant difference in the results between the model using constructed variables and the model using individual staff variables.
There might be some variation in the strictness of law enforcement on the quality violations of nursing homes among states. This variation may impose measurement errors on this variable. Therefore, the number of regulatory deficiencies of each facility was divided by the mean of facility deficiencies of the state where this facility is located. The resulting measure was used in the regression analysis to adjust for state variation.
The weighting value 2 was assigned to those patients who are totally dependent on other people's assistance for any of the five ADLs, and the weighting values 1 and 0 were assigned to those patients who need partial assistance and no assistance at all, respectively. For instance, if 40 percent and 30 percent of patients in a facility are totally and partially, respectively, dependent on others for the act of eating, then the ADL-specific score for eating for this facility is (0.4)(2) + (0.3)(1) + (0.3)(0)=1.1. This calculation was repeated for every ADL and for each facility.
The reasoning behind our assumption includes the following: (1) Care-related process variables, which reflect daily practices of providers, are more “visible” and “tangible” so that they are more likely to be manipulated. (2) In the short run (i.e., a 1-year period), the everyday care process is more likely to be a function of cost consideration than the structural and outcome aspects of quality, which reflect more long-term strategic actions of providers. (3) Providers need to meet certain regulatory requirements (including staffing) by law, so the room for their manipulation in staffing and regulatory compliance is much smaller than that in care process.
Because a proportion of facilities in our sample has a zero value for the Medicaid patient day or drug error rate variable, the estimated regression line through the OLS method could be distorted and the predicted instruments based on these estimates may be biased, too. Therefore, the Tobit model was used to address the censored data.
The detailed results on the Hausman test are available by request from the authors.
A hybrid cost function has the basic structure of a cost function determined from economic theory, in which cost is a function of output and input prices. It also adds additional independent terms to capture the effects of other regressors that are not implied strictly by the economic theory, but are typically expected to impact nursing home costs (e.g., Medicaid payment methods).
References
- Bishop C, Dor A. “Medicare Costs in Urban and Rural Nursing Homes: Are Differential Payments Required?”. Inquiry. 1994;31(4):153–62. [PubMed] [Google Scholar]
- Breyer F. “The Specification of a Hospital Cost Function: A Comment on the Recent Literature.”. Journal of Health Economics. 1987;6(2):147–57. doi: 10.1016/0167-6296(87)90004-x. [DOI] [PubMed] [Google Scholar]
- Castle NG, Zinn JS, Brannon D, Mor V. Quality Improvement in Nursing Homes: Health Care Management: State of the Art Reviews. Philadelphia: Hanley and Belfus; 1997. pp. 39–53. [PubMed] [Google Scholar]
- Coburn AF, Fortinsky R, McGuire C, McDonald TP. “Effect of Prospective Reimbursement on Nursing Home Costs.”. Health Services Research. 1993;28(1):45–68. [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Dubay L. “The Effects of Medicaid Reimbursement Method and Ownership on Nursing Home Costs, Case Mix and Staffing.”. Inquiry. 1990;27(2):183–200. [PubMed] [Google Scholar]
- Davis MA, Provan KG. “A Cost-Constrained Model of Strategic Service Quality Emphasis in Nursing Homes.”. Health Services Management Research. 1996;9(1):24–33. doi: 10.1177/095148489600900103. [DOI] [PubMed] [Google Scholar]
- Donabedian A. “Evaluating the Quality of Medical Care.”. Milbank Memorial Fund Quarterly. 1966;44(3):166–203. [PubMed] [Google Scholar]
- Dor A. “The Costs of Medicare Patients in Nursing Homes in the United States: A Multiple Output Analysis.”. Journal of Health Economics. 1989;8(3):253–70. doi: 10.1016/0167-6296(89)90021-0. [DOI] [PubMed] [Google Scholar]
- Frank RG, Lave JR. “The Impact of Medicaid Benefit Design on Length of Hospital Stay and Patient Transfers.”. Hospital and Community Psychiatry. 1985;36(7):749–53. doi: 10.1176/ps.36.7.749. [DOI] [PubMed] [Google Scholar]
- Freiman MP, Murtaugh CM. “The Determinants of the Hospitalization of Nursing Home Residents.”. Journal of Health Economics. 1993;12(3):349–59. doi: 10.1016/0167-6296(93)90017-9. [DOI] [PubMed] [Google Scholar]
- Gertler PJ, Waldman DM. “Quality-adjusted Cost Functions and Policy Evaluation in the Nursing Home Industry.”. Journal of Political Economy. 1992;100(6):1232–56. [Google Scholar]
- Grannemann TW, Brown RS, Pauly MV. “Estimating Hospital Costs: A Multiple-Output Analysis.”. Journal of Health Economics. 1986;5(2):107–27. doi: 10.1016/0167-6296(86)90001-9. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Improving the Quality of Care in Nursing Homes Publication No. IOM-85-10. Committee on Nursing Home Regulation. Washington DC: National Academy Press; 1986. [Google Scholar]
- Levit K, Cowan C, Lazenby H, Sensenig PM, Stiller J, Martin A the Health Accounts Team. “Health Spending in 1998: Signals of Change.”. Health Affairs. 2000;19(1):124–32. doi: 10.1377/hlthaff.19.1.124. [DOI] [PubMed] [Google Scholar]
- Meiners MR. “An Econometric Analysis of the Major Determinants of Nursing Home Costs in the United States.”. Social Science and Medicine. 1982;16(8):887–98. doi: 10.1016/0277-9536(82)90208-8. [DOI] [PubMed] [Google Scholar]
- Medical Expenditure Panel Survey. Nursing Homes: Structure and Selected Characteristics, 1996. Rockville MD: Agency for Health Care Policy and Research; 1996. [Google Scholar]
- Mukamel DB. “Risk-adjusted Outcome Measures and Quality of Care in Nursing Homes. Medical Care. 1997;35(4):367–85. doi: 10.1097/00005650-199704000-00007. [DOI] [PubMed] [Google Scholar]
- Nyman JA. “The Marginal Cost of Nursing Home Care: New York, 1983.”. Journal of Health Economics. 1988;7(4):393–412. doi: 10.1016/0167-6296(88)90022-7. [DOI] [PubMed] [Google Scholar]
- Nyman JA, Geyer CR. “Promoting the Quality of Life in Nursing Homes: Can Regulation Succeed? Journal of Health Politics, Policy and Law. 1989;14(4):797–816. doi: 10.1215/03616878-14-4-797. [DOI] [PubMed] [Google Scholar]
- Phillips C, Hawes C, Mor V. Evaluation of the Implementation of the Nursing Home Resident Assessment System. Washington DC: Health Standards and Quality Bureau Health Care Financing Administration; 1996. [Google Scholar]
- Rosko MD, Chilingerian JA, Zinn JS, Aaronson WE. “The Effects of Ownership, Operating Environment, and Strategic Choices on Nursing Home Efficiency.”. Medical Care. 1995;33(10):1001–21. doi: 10.1097/00005650-199510000-00003. [DOI] [PubMed] [Google Scholar]
- Sexton TR, Leiken AM, Sleeper S, Coburn A. “The Impact of Prospective Reimbursement on Nursing Home Efficiency.”. Medical Care. 1989;27(2):154–63.. doi: 10.1097/00005650-198902000-00006. [DOI] [PubMed] [Google Scholar]
- Thorpe KE, Gertler PJ, Goldman P. “The Resource Utilization Group System: Its Effect on Nursing Home Case Mix and Costs.”. Inquiry. 1991;28(4):357–65. [PubMed] [Google Scholar]
- Vitaliano DF. “On the Estimation of Hospital Cost Functions.”. Journal of Health Economics. 1987;6(4):305–18. doi: 10.1016/0167-6296(87)90018-x. [DOI] [PubMed] [Google Scholar]
- Zinn JS. “Market Competition and the Quality of Nursing Home Care.”. Journal of Health Politics, Policy and Law. 1994;19(3):555–82. doi: 10.1215/03616878-19-3-555. [DOI] [PubMed] [Google Scholar]


