Abstract
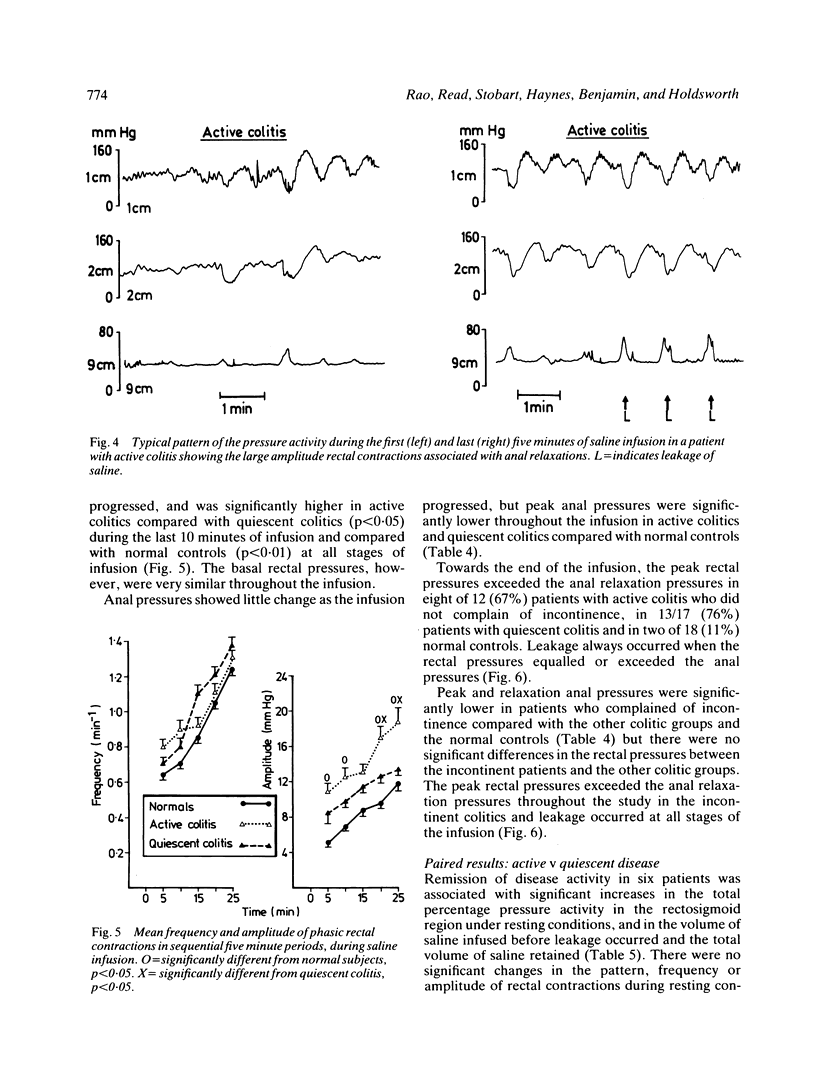
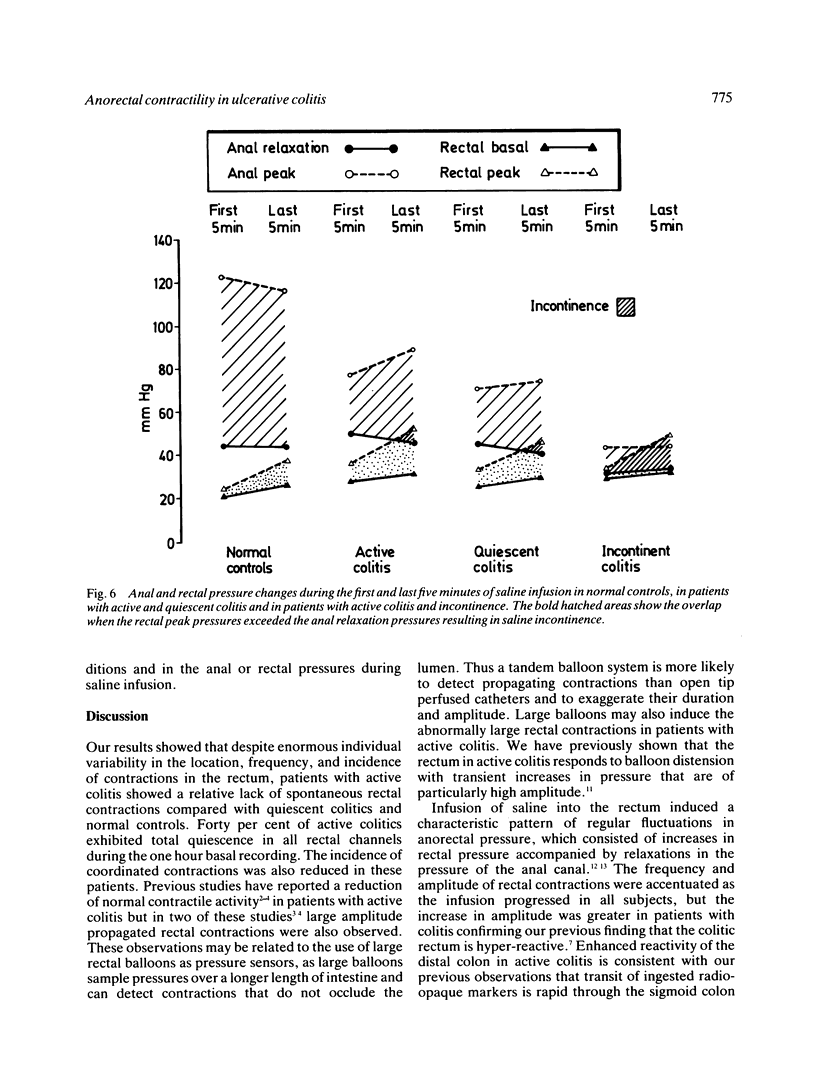
Pressure activity in the rectum and anal canal was measured with a multilumen probe in 29 patients with ulcerative colitis (12 active, 11 quiescent, six studied during both phases) and 18 normal controls under resting conditions and during rectal infusion of saline. Resting motor activity was significantly decreased in patients with active colitis compared with quiescent colitis (p less than 0.005) and normal controls (p less than 0.001). Forty per cent of active colitics showed a featureless record compared with only one patient with quiescent colitis and one normal subject. The volume of saline infused before leakage occurred, and the total volume retained were significantly lower (p less than 0.001) in patients with active and quiescent colitis compared with normal controls. Rectal infusion of saline provoked regular rectal contractions, of significantly higher (p less than 0.05) amplitude in patients with active colitis, than in quiescent colitis or controls. These rectal contractions were associated with simultaneous anal relaxations. During saline infusion, peak and pressures were lower in patients with ulcerative colitis than in normal subjects, but there were no significant differences in relaxation pressures. In normal subjects, the rectal pressures remained below the anal pressures throughout the saline infusion. Peak rectal pressures exceeded the anal relaxation pressures during the last five minutes of saline infusion in patients with ulcerative colitis and throughout the infusion in those patients who complained of incontinence. Results suggest that although the resting rectal motor activity is diminished in patients with ulcerative colitis, luminal distension causes the inflamed rectum to generate abnormally strong contractions that may threaten continence.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- CHAUDHARY N. A., TRUELOVE S. C. Human colonic motility: a comparative study of normal subjects, patients with ulcerative colitis, and patients with the irritable colon syndrome. I. Resting patterns of motility. Gastroenterology. 1961 Jan;40:1–17. [PubMed] [Google Scholar]
- CONNELL A. M. The motility of the pelvic colon. II. Paradoxical motility in diarrhoea and constipation. Gut. 1962 Dec;3:342–348. doi: 10.1136/gut.3.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DAVIDSON M., SLEISENGER M. H., ALMY T. P., LEVINE S. Z. Studies of distal colonic motility in children. I. Non-propulsive patterns in normal children. Pediatrics. 1956 Jun;17(6):807–819. [PubMed] [Google Scholar]
- DAVIDSON M., SLEISENGER M. H., ALMY T. P., LEVINE S. Z. Studies of distal colonic motility in children. II. Propulsive activity in diarrheal states. Pediatrics. 1956 Jun;17(6):820–832. [PubMed] [Google Scholar]
- Dinoso V. P., Jr, Murthy S. N., Goldstein J., Rosner B. Basal motor activity of the distal colon: a reappraisal. Gastroenterology. 1983 Sep;85(3):637–642. [PubMed] [Google Scholar]
- Hancock B. D. Measurement of anal pressure and motility. Gut. 1976 Aug;17(8):645–651. doi: 10.1136/gut.17.8.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes W. G., Read N. W. Ano-rectal activity in man during rectal infusion of saline: a dynamic assessment of the anal continence mechanism. J Physiol. 1982 Sep;330:45–56. doi: 10.1113/jphysiol.1982.sp014327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KERN F., Jr, ALMY T. P., ABBOT F. K., BOGDONOFF M. D. The motility of the distal colon in nonspecific ulcerative colitis. Gastroenterology. 1951 Nov;19(3):492–503. [PubMed] [Google Scholar]
- Narducci F., Bassotti G., Gaburri M., Morelli A. Twenty four hour manometric recording of colonic motor activity in healthy man. Gut. 1987 Jan;28(1):17–25. doi: 10.1136/gut.28.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read N. W., Haynes W. G., Bartolo D. C., Hall J., Read M. G., Donnelly T. C., Johnson A. G. Use of anorectal manometry during rectal infusion of saline to investigate sphincter function in incontinent patients. Gastroenterology. 1983 Jul;85(1):105–113. [PubMed] [Google Scholar]
- Ritchie J. A., Tuckey M. S. Intraluminal pressure studies at different distances from the anus in normal subjects and in patients with the irritable colon syndrome. Am J Dig Dis. 1969 Feb;14(2):96–106. doi: 10.1007/BF02232832. [DOI] [PubMed] [Google Scholar]
- Ruddell W. S., Dickinson R. J., Dixon M. F., Axon A. T. Treatment of distal ulcerative colitis (proctosigmoiditis) in relapse: comparison of hydrocortisone enemas and rectal hydrocortisone foam. Gut. 1980 Oct;21(10):885–889. doi: 10.1136/gut.21.10.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPRIGGS E. A., CODE C. F., BARGEN J. A., CURTISS R. K., HIGHTOWER N. C., Jr Motility of the pelvic colon and rectum of normal persons and patients with ulcerative colitis. Gastroenterology. 1951 Nov;19(3):480–491. [PubMed] [Google Scholar]
- Snape W. J., Jr, Matarazzo S. A., Cohen S. Abnormal gastrocolonic response in patients with ulcerative colitis. Gut. 1980 May;21(5):392–396. doi: 10.1136/gut.21.5.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville K. W., Langman M. J., Kane S. P., MacGilchrist A. J., Watkinson G., Salmon P. Effect of treatment on symptoms and quality of life in patients with ulcerative colitis: comparative trial of hydrocortisone acetate foam and prednisolone 21-phosphate enemas. Br Med J (Clin Res Ed) 1985 Sep 28;291(6499):866–866. doi: 10.1136/bmj.291.6499.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TRUELOVE S. C., WITTS L. J. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955 Oct 29;2(4947):1041–1048. doi: 10.1136/bmj.2.4947.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]



