Abstract
A lipid-based formulation has been developed for oral delivery of Mycobacterium bovis bacille Calmette-Guérin (BCG) vaccine. The formulated M. bovis BCG was fed to BALB/c mice to test for immune responses and protection against M. bovis infection. The immune responses included antigen-specific cytokine responses, spleen cell proliferation, and lymphocyte-mediated macrophage inhibition of M. bovis. Oral delivery of formulated M. bovis BCG to mice induced strong splenic gamma interferon levels and macrophage inhibition of virulent M. bovis compared with results with nonformulated M. bovis BCG. Formulated oral M. bovis BCG significantly reduced the bacterial burden in the spleen and lungs of mice following aerosol challenge with virulent M. bovis. Our data suggest that oral delivery of formulated M. bovis BCG is an effective means of inducing protective immune responses against tuberculosis. Lipid-based, orally delivered mycobacterial vaccines may be a safe and practical method of controlling tuberculosis in humans and animals.
Tuberculosis (TB) remains the leading cause of death by a single disease-causing organism, with an estimated 2 million deaths each year (18, 37). In addition, the disease is a threat to the agricultural industry due to persistence of TB in farmed animals (16). Human TB is predominantly caused by Mycobacterium tuberculosis, while TB in animals is caused by Mycobacterium bovis. Both M. tuberculosis and M. bovis are members of the TB complex and are very closely related genetically. While effective chemotherapy for human TB has been available for many years, treatment is lengthy and relatively expensive, making widespread control of the disease difficult to achieve in developing countries. Prophylactic vaccination may be a better option for controlling TB.
M. bovis bacille Calmette-Guérin (BCG) is the world's most widely used vaccine, with an estimated 3 billion doses having been administered since its discovery and initial testing in the 1920s (20, 33). M. bovis BCG consists of a live attenuated strain of M. bovis and was originally derived from a cow with tuberculous mastitis. Despite its widespread use, the efficacy of M. bovis BCG remains highly variable, with success rates in human and animal trials ranging between 0 and 80% protection (14, 15, 20). In a recent meta-analysis of human M. bovis BCG vaccination trials, M. bovis BCG was shown to reduce the risk of pulmonary TB by 50% and the number of deaths due to TB by 71% (5). There are a number of reasons proposed for the variation in efficacy; however, it is clear that killed M. bovis BCG is poorly protective and that acquired immunity against TB depends on survival and persistence of live M. bovis BCG, or its secreted products, in the host (17, 21, 36). These reports suggest that under the appropriate conditions, M. bovis BCG can be effective against TB. Furthermore, to date no TB vaccine has been shown to provide greater protection than M. bovis BCG against experimental infection with TB. Taken together, these data lend weight to arguments favoring modification of M. bovis BCG to improve its efficacy.
Oral administration of M. bovis BCG was used with children between 1921 and 1976, but this route was abandoned due to low rates of delayed-type hypersensitivity conversion and occasional development of cervical lymphadenitis (21). Since these trials, there have been substantial improvements in oral delivery systems and the use of immune modulators for oral vaccines (4, 41). Oral administration of a vaccine against TB has a number of advantages, including ease of administration, low cost, and avoidance of needles and the associated reduced risk of disease transfer. Furthermore, oral immunization more effectively targets the mucosal immune response. Control of bovine TB is difficult in countries which have wildlife reservoirs of M. bovis infection, such as New Zealand and the United Kingdom. Vaccination of wildlife against bovine TB is currently being considered, and an oral bait containing M. bovis BCG would be a promising option if the M. bovis BCG could be protected from degradation in the stomach (9).
Oral immunization of guinea pigs and mice with M. bovis BCG has been shown to induce immune responses in spleen and lymph node cell populations as well as purified protein derivative (PPD)-specific delayed-type hypersensitivity and antibody responses (28, 29, 36). Mice immunized orally or intragastrically with high doses of M. bovis BCG showed similar levels of protective immunity to mice immunized via the subcutaneous route and induced protection against intravenous challenge with M. tuberculosis (29). These reports suggest that mucosal immunization with M. bovis BCG can be an effective means of inducing protective systemic immune responses.
Current commercially available human M. bovis BCG vaccines (e.g., Glaxo) are derived from freeze-dried M. bovis BCG preparations. Although in animal trials, fresh M. bovis BCG is frequently used (2, 8, 22, 30, 35), the freeze-drying procedure results in reduced viability of bacteria, with reports of between 30 and 50% loss of viability and impaired recovery of remaining live bacteria (21). A method of preparing M. bovis BCG that retains optimal viability of the bacteria prior to vaccination would contribute greatly to the success of this vaccine.
Lipids are only partially degraded in the stomach, as the majority of lipolytic enzymes are present in the large intestine (11, 13, 24, 32). Lipids may therefore provide some protection for the M. bovis BCG vaccine against degradation in the stomach. Furthermore, ingestion of lipids decreases gastrointestinal motility, and the presence of lipid digestive products within the upper small intestine induces the secretion of biliary and pancreatic fluids that dramatically alter the luminal environment (13). These conditions may assist in the transfer of live M. bovis BCG through the intestinal epithelium. Based on these observations, we hypothesized that protection of M. bovis BCG against gastric secretions with lipids would enhance viability and improve uptake of viable bacilli across the intestinal wall. We report here the development and testing of a novel lipid-based M. bovis BCG formulation for oral vaccination of mice.
MATERIALS AND METHODS
Bacteria.
M. bovis BCG Pasteur 1173P2 was used as the vaccine strain. The virulent M. bovis strain used for macrophage infection studies and for aerosol challenge of mice was M. bovis 83/6235, which been described in previous studies (1, 6). For M. bovis BCG formulation and macrophage infection, bacteria were grown to mid-log phase in 175-ml flasks (Falcon) containing Middlebrook 7H9 medium (Difco, Detroit, Mich.) supplemented with albumin-dextrose-catalase (8). Bacilli were harvested by centrifugation and washed twice in phosphate-buffered saline (PBS) prior to storage at −70°C. For aerosol challenge of mice, M. bovis was grown to mid-log phase in Tween albumin broth containing a Dubos broth base (Difco) supplemented with 0.006% (vol/vol) alkalinized oleic acid, 0.5% (wt/vol) albumin fraction V, and 0.25% (wt/vol) glucose. The number of CFU of M. bovis BCG or virulent M. bovis was determined retrospectively by plating on 7H11 agar plates as described previously (7).
Lipid composition.
A fractionated lipid product was selected for formulation of M. bovis BCG on the basis of melting temperature (32°C) and the ability to maintain bacilli in a viable and uniform suspension as assessed by counting CFU (data not shown). The lipid consisted of tryglycerides of fatty acids comprising 1% myristic acid, 25% palmitic acid, 15% stearic acid, 50% oleic acid, and 6% linoleic acid.
Formulation of M. bovis BCG.
Glucose (10 mg/ml), monosodium glutamate (1 mg/ml; Sigma), and 10% vol/vol albumin-dextrose-catalase were added to the lipid (lipid formulation). These additives were dispersed with the lipid in the liquid phase (40°C) and were previously shown not to affect viability of M. bovis BCG. Pelleted M. bovis BCG was resuspended in liquefied formulation medium which had been warmed to 40°C. M. bovis BCG formulations were transferred to 15-ml tubes (Falcon) and allowed to solidify with gentle mixing at 4°C. Formulations were removed from the tubes and aseptically cut into 1-g pellets as required for viability testing and vaccination studies.
Vaccination of mice.
Female BALB/c mice (6 to 8 weeks old) were obtained from the University of Otago Department of Animal Laboratory Sciences, Dunedin, New Zealand. Mouse experiments were conducted under ethics approval from the University of Otago Animal Ethics Committee (approval no. 51/2000).
For time course experiments, mice were vaccinated subcutaneously with 106 CFU of BCG. For oral vaccination, mice were separated into individual cages and taken off food for 12 h prior to oral vaccination. Nonformulated controls consisted of M. bovis BCG in Craig's preservative-free strawberry jam (Heinz-Watties Ltd., Hastings, New Zealand). A previous study had shown that M. bovis BCG viability over a 24-h interval was not affected by mixing M. bovis BCG in the jam (data not shown). Nonvaccinated controls consisted of lipid formulation alone. For dose response and time course experiments, mice were given vaccine in two separate doses at 24-h intervals. For aerosol challenge experiments, mice were given a single oral dose of BCG (5 × 107 CFU) or vaccinated subcutaneously with 106 CFU of BCG and challenged 8 weeks postvaccination. The mice were observed at various intervals during consumption of pellets and jam to ensure the full dose was eaten. At various time points postvaccination, the mice were sacrificed by CO2 inhalation and their spleens were removed aseptically.
Spleen cell proliferation assay.
Spleen cell suspensions were prepared by filtering cells through a cell strainer (70-μm-pore-size mesh; Becton Dickinson). Cells were washed twice in PBS and resuspended to a concentration of 106/ml in Dulbeccos's modified Eagles medium (DMEM) containing 10% fetal calf serum, 20 mM HEPES penicillin (100 U/ml), streptomycin (100 μg/ml), 5.5 × 10−5 M 2-mercaptoethanol (all from Gibco-BRL). Cells were resuspended to a concentration of 107 per ml in RPMI plus 10% fetal calf serum (Gibco). Splenocytes (5 × 105 per well) were plated out in triplicate wells in 96-well plates (Nunc). Cells were cultured purified protein derivative from a culture of M. bovis (bovine PPD) (Commonwealth Serum Laboratories, Melbourne, Australia), 60-μg/ml final concentration, or with medium alone. Cells were harvested 4 days later, after an 18-h pulse with 1 μCi of [3H]thymidine (Amersham, Buckinghamshire, England), and the incorporated thymidine was measured as previously described (44). A stimulation index was obtained by dividing the mean counts per minute for the triplicate cultures incubated with bovine PPD by the mean counts per minute for splenocytes cultured with medium only.
In vitro assay for cytokine production by spleen cells.
Spleen cell suspensions were prepared as described above for the spleen cell proliferation assay. One milliliter of cell suspension was dispensed into 24-well plates (Costar), and 100 μl of either PBS or bovine PPD (final concentration, 60 μg/ml) was added to the wells. Cultures were incubated for 72 h in 5% CO2 at 37°C, after which time 200 μl of culture supernatant was collected and frozen at 70°C for cytokine analysis. Interleukin-2 (IL-2) and gamma interferon (IFN-γ) capture enzyme-linked immunosorbent assays (ELISAs) were performed according to the manufacturer's instructions using a commercial kit (Duoset; R&D Systems, Minneapolis, Minn.). Cytokine levels in culture supernatants were quantified by extrapolation from standard curves. The minimum sensitivities of the two ELISAs were determined to be 50 pg/ml for IFN-γ and 35 pg/ml for IL-2.
M. bovis inhibition assay.
Peritoneum-derived macrophages were tested for inhibition of intracellular growth of M. bovis following coculture with or without autologous lymphocytes. Experiments were performed according to a modification of previously described protocols (26, 31, 39, 43). Peritoneal exudate cells were obtained by lavage from female BALB/c mice. Cells were collected in PBS supplemented with 1% bovine serum albumin and 20 U of heparin/ml, washed once, and resuspended in DMEM containing 10% fetal calf serum and 1,00 U of penicillin/ml (supplemented DMEM) at 2 × 106 cells/ml. One hundred microliters of cell suspension was dispensed into a 96-flat-well plate (Nunc). After incubation for 2 h in 5% CO2 at 37°C, the nonadherent cells were removed, washed, and resuspended at a density of 5 × 106/ml in supplemented DMEM. Nonadherent cells were selectively depleted of the remaining adherent population by incubation in 25-ml flasks (Falcon). Nonadherent peritoneal exudate cells (NPEC) were determined to comprise >90% lymphocytes following May-Grunwald/Giemsa staining. Warm supplemented DMEM was added to the adherent monolayer, which was estimated to contain 5 × 104 cells/well. This population was found to be 98% positive with a nonspecific esterase staining kit (catalog no. 181-B; Sigma, St. Louis, Mo.) and is henceforth referred to as macrophages. Macrophages were infected with M. bovis at a multiplicity of infection of two bacilli per macrophage as described previously (3). Nonphagocytosed bacteria were removed by gentle washing. One hundred microliters (containing 5 × 105 cells) of autologous NPEC was added to each well containing infected macrophages, and cultures were further incubated in 5% CO2 at 37°C. The resulting 10:1 NPEC-to-macrophage ratio was selected to approximate the ratio found in peripheral blood mononuclear cells. Control wells consisted of M. bovis-infected macrophages alone or uninfected NPEC and macrophages. After 72 h, cells were pulsed with 1.0 μCi of [3H]uracil for 18 h. The cells were lysed with 0.1% saponin, and the bacteria were heat killed at 80 to 90°C for 20 min prior to harvesting onto glass fiber filters (Whatman, Inc., Clifton, N.J.) using an automated cell harvester (Cambridge Technology). The amount of [3H]uracil incorporated was determined using a liquid β-scintillation counter.
Aerosol challenge with M. bovis.
Six mice per vaccine group were challenged by aerosol with virulent M. bovis 8 weeks after vaccination. A single-cell suspension of M. bovis 83/6235 was prepared using a modification of a method described by A. A. Grover et al. (1967) and stored at −70°C. To prepare these suspensions, the bacterial cells were dispersed by sonication for 30 s and filtered through an 8-μm-pore-size-membrane filter. Mice were infected via the respiratory route using an aerosol chamber which produces droplet nuclei of the size appropriate for entry into alveolar spaces (34). The concentration of viable M. bovis in the nebulizer fluid was empirically adjusted to result in the inhalation and retention of 5 to 20 viable organisms per pair of mouse lungs (B. Buddle and G. de Lisle, unpublished data). A similar procedure has been shown to result in reproducible, uniform infection of the lungs of guinea pigs (40, 42). The aerosol infection and subsequent maintenance and manipulation of infected mice were performed under strict isolation conditions in a biohazard facility.
Isolation of M. bovis.
Mice were euthanatized between 37 and 40 days after aerosol challenge. The lungs and spleen from each mouse were processed individually for mycobacterial isolation. The organs were homogenized in a Ten-Broeck grinder, and samples were centrifuged at 3,500 × g for 20 min. The deposits were resuspended in 1 ml of distilled water. Appropriate dilutions were made in Tween albumin broth, and a 0.1-ml volume of a diluted or undiluted sample was inoculated onto a modified mycobacterium 7H11 agar containing sodium pyruvate (7). In the absence of glycerol, sodium pyruvate is selective for virulent M. bovis but not M. bovis BCG. The minimum detectable level of viable bacteria in lung and spleen homogenates was 10 CFU/lung or spleen. Two replicates were prepared for each dilution. Culture conditions and methods for identification of isolates were carried out as previously described (7).
Analysis of data.
Statistically analyses of differences in the mean cytokine levels and log10 transformed spleen cell proliferation responses for the vaccine groups were determined using the Student t test. The bacterial counts from the lung and spleen were log10 transformed and analyzed using analysis of variance. For statistical purposes, when no bacteria were cultured from tissues, half the lowest detectable count (percent CFU/organ) was used.
RESULTS
A lipid product has been identified as being compatible with M. bovis BCG. Chemical analysis of the lipid showed that it consists of a mixture of medium and long-chain fatty acids. The lipid is liquid at 37°C but forms a solid at 30 to 33°C. Formulation of M. bovis BCG in the lipid matrix has no immediate detrimental effect on bacterial viability. M. bovis BCG is maintained and stored in a solid matrix which is suitable for oral delivery.
M. bovis BCG viability is retained following formulation.
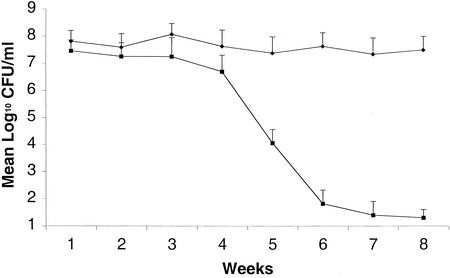
Retrospective testing of M. bovis BCG viability following formulation with lipid showed that the number of CFU recovered immediately following formulation did not significantly decrease. Over time however, the number of CFU decreased in relation to increased storage temperature. Figure 1 shows the number of CFU of M. bovis BCG which could be recovered following storage in lipid formulation. Formulated M. bovis BCG could be stored for at least 8 weeks at 4°C with minimal loss of viability. Further tests at 16 weeks after storage at 4°C showed similar levels of M. bovis BCG viability (data not shown). However, with storage at room temperature, viability of M. bovis BCG began to decrease after 32 days. By 8 weeks of storage at this temperature, few viable M. bovis BCG could be detected. These results show that the shelf life of formulated M. bovis BCG is maintained at a low temperature but shortens considerably at higher temperatures.
FIG. 1.
Influence of temperature on viability of lipid-formulated M. bovis BCG following storage. The number of CFU of M. bovis BCG was determined by plating serial dilutions of formulated M. bovis BCG which had been stored at 4°C (diamonds) or at room temperature (10 to 25°C) (squares) The data shown are the means of M. bovis BCG CFU ± standard errors. The experiment was repeated three times with similar results.
Oral delivery of formulated M. bovis BCG induces immune responses in mice.
To determine a suitable method of measuring systemic immune responses following oral delivery of M. bovis BCG, we compared bovine PPD-induced splenocyte proliferation (LTA) and splenic IL-2 and IFN-γ responses with subcutaneous BCG vaccination at 8 weeks. Mice were fed 5 × 107 CFU of lipid-formulated M. bovis BCG or M. bovis BCG in jam (nonformulated M. bovis BCG) or were subcutaneously vaccinated with 106 CFU of M. bovis BCG. Table 1 shows that while both the LTA and IFN-γ assays showed significant differences between the formulated and nonformulated oral M. bovis BCG groups, the differences for the IL-2 assay were not significant. The IFN-γ assay was used in further experiments to monitor systemic immune responses due to the importance of IFN-γ for protection against TB.
TABLE 1.
Bovine PPD-stimulated spleen cell responses in mice 8 weeks after vaccinationa
| Immunization | Response
|
||
|---|---|---|---|
| IL-2 (pg/ml) | IFN-γ (pg/ml) | LTA (SI) | |
| Formulation only | 110.62 (±14.06) | 51.44 (±14.38) | 1.67 (±0.49) |
| Nonformulated oral BCG | 153.51 (±25.22) | 65.10 (±20.05) | 1.83 (±0.51) |
| Formulated oral BCG | 230.23 (±54.13) | 778.95* (±76.80) | 6.26* (±0.33) |
| Subcutaneous BCG | 330.56 (±61.12) | 536.88* (±86.70) | 8.22* (±0.73) |
Asterisk indicates a mean which is significantly different from the mean of the formulation-only control group. P value, <0.05 (Student t test). Standard errors are given in parentheses. SI, stimulation index.
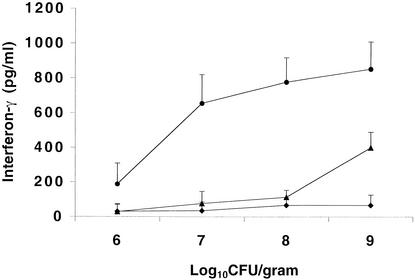
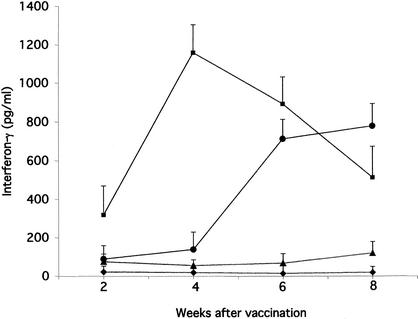
To determine the effect of dose of M. bovis BCG following oral delivery, we compared splenic IFN-γ responses to bovine PPD in mice vaccinated with various doses of formulated or nonformulated M. bovis BCG at 8 weeks postvaccination. Figure 2 shows that a low level of IFN-γ (<200 pg/ml) was detected in the formulated group following oral immunization with 106 CFU of M. bovis BCG, but there were no significant differences between the vaccine groups. When the dose was increased to 107 CFU, IFN-γ responses in the nonformulated group remained low whereas responses to formulated M. bovis BCG increased significantly (P < 0.05). Similar differences were seen with 108 CFU of M. bovis BCG. When the vaccine dose was increased to 109 CFU of BCG, an increase in the levels of IFN-γ was seen in the nonformulated group while levels in the formulated group remained high. At doses of M. bovis BCG ranging from 107 to 109 CFU, IFN-γ responses in the formulated M. bovis BCG group were significantly greater than those of nonformulated M. bovis BCG. The increase in IFN-γ responses seen at the high dose in the nonformulated group shows that considerably higher doses of oral M. bovis BCG are required for induction of immune responses than are required with formulated M. bovis BCG. To determine the time course of immune responses to oral M. bovis BCG, we compared splenic IFN-γ responses at 2-week intervals following oral or subcutaneous vaccination with M. bovis BCG. Figure 3 shows that IFN-γ responses following subcutaneous vaccination peaked at 4 weeks and gradually declined at weeks 6 and 8. By comparison, IFN-γ responses following oral vaccination with formulated M. bovis BCG first increased at 6 weeks and remained high at 8 weeks postvaccination. IFN-γ responses to nonformulated M. bovis BCG or formulation material alone remained low between 2 and 8 weeks. These results show that immune responses following oral vaccination with formulated M. bovis BCG are delayed compared to results with subcutaneous vaccination but appear to persist at least to 8 weeks.
FIG. 2.
Bovine PPD induced IFN-γ responses following oral vaccination with various doses of formulated M. bovis BCG. Mice were sacrificed at 8 weeks after oral immunization with formulated M. bovis BCG (circles), nonformulated M. bovis BCG (triangles), or formulation material only (diamonds). Splenocytes were incubated with bovine PPD for 72 h. Supernatants were then collected and analyzed using a sandwich ELISA. Each treatment group contained six mice. Spleens were individually processed. Results are expressed in picograms/milliliter and are presented as means of triplicate determinations. Bars indicate standard errors.
FIG. 3.
Antigen-induced splenic IFN-γ responses to M. bovis BCG vaccination in BALB/c mice. Mice were euthanatized at 2, 4, 6, and 8 weeks after vaccination with 106 CFU of subcutaneous M. bovis BCG (squares), oral delivery of 107 CFU of formulated M. bovis BCG (circles), nonformulated M. bovis BCG (triangles), or formulation material only (diamonds). Splenocytes were incubated with bovine PPD for 72 h. Supernatants were then collected and analyzed using a sandwich ELISA. Each treatment group contained five to six mice. Spleens were individually processed. Results are expressed in picograms/milliliter and are presented as means of triplicate determinations. Results at 8 weeks are from two separate experiments. P value was <0.05 (Student t test). Bars indicate standard errors.
Peritoneum-derived lymphocytes from mice orally vaccinated with formulated M. bovis inhibit growth of M. bovis in autologous macrophages.
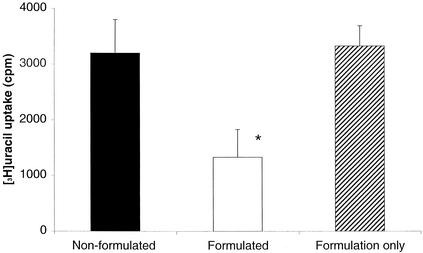
The addition of NPEC to M. bovis-infected macrophages from mice vaccinated with oral M. bovis BCG formulations was performed in order to determine whether lymphocyte-mediated effector mechanisms could inhibit intracellular growth of M. bovis. Growth of M. bovis in macrophages was determined by [3H]uracil uptake. The growth of M. bovis within macrophages alone or when cocultured with NPEC from orally vaccinated mice is illustrated in Fig. 4 Macrophages prepared from mice orally vaccinated with formulated or nonformulated M. bovis BCG or mice given formulation material alone showed no differences in their ability to control M. bovis growth. When NPEC from mice vaccinated with formulated M. bovis BCG were cocultured with autologous M. bovis-infected macrophages, the [3H]uracil counts were significantly reduced from those for coculture of NPEC from mice vaccinated with nonformulated M. bovis BCG or formulation material alone (P < 0.05). These results demonstrate that lymphocytes from mice orally vaccinated with formulated M. bovis BCG activate macrophages to inhibit intracellular growth of M. bovis. Control of intracellular growth of M. bovis in vitro may reflect growth inhibition in vivo, leading to reduced dissemination of M. bovis in the host.
FIG. 4.
Growth inhibition of M. bovis by macrophages cocultured with NPEC. Macrophages were infected with M. bovis at a multiplicity of infection of two bacilli per macrophage. Nonadherent autologous NPEC were added at a ratio of 10 NPEC per macrophage. Incorporation of [3H]uracil was then assessed at 72 h postinfection. The mean [3H]uracil uptake by cell cultures which did not contain M. bovis was 460 cpm. Growth of intracellular bacilli from cocultured macrophages and NPEC was expressed as means of triplicates. The results are representative of two experiments. The asterisk represents a mean which is significantly different from the mean of the formulation-only control group; bars indicate standard errors.
Oral vaccination with formulated M. bovis BCG protects against aerosol challenge with virulent M. bovis.
In order to determine the protective efficacy of formulated oral M. bovis BCG, mice were orally vaccinated with 5 × 107 CFU of formulated M. bovis BCG or subcutaneously vaccinated with 106 CFU of M. bovis BCG. Nonvaccinated mice served as controls. Mice were challenged with virulent M. bovis by the aerosol route 8 weeks after vaccination and euthanatized 37 to 40 days after challenge. Table 2 shows that subcutaneous M. bovis BCG vaccination reduced the bacterial count in the lungs by approximately 2.34 logs and reduced the bacterial count in the spleen by 1.90 logs. By comparison, formulated oral M. bovis BCG reduced the lung bacterial count by approximately 1.0 log and the spleen bacterial count by 1.48 logs. The results in Table 2 showed that oral formulated M. bovis BCG and subcutaneous M. bovis BCG induced significant protection against aerosol challenge with virulent M. bovis, although the protective efficacy of subcutaneous M. bovis BCG in the lung was greater than that for the oral formulated M. bovis BCG group.
TABLE 2.
Effect of vaccination on protection of mice against aerosol challenge with M. bovisa
| Vaccine group | Lung bacterial countb | Log10 resistancec | Spleen bacterial countb | Log10 resistancec |
|---|---|---|---|---|
| Nonvaccinated | 5.837 (±0.362) (A) | NA | 4.565 (±0.189) (A) | NA |
| Formulated oral BCG | 4.774 (±0.270) (B) | 1.06 | 3.084 (±0.176) (B) | 1.48 |
| Subcutaneous BCG | 3.498 (±0.237) (C) | 2.34 | 2.660 (±0.181) (B) | 1.90 |
Figures in columns with the same parenthetical letter are not significantly different (P > 0.05).
Values are log10 numbers of CFU (±standard error) of M. bovis from the lungs or spleens of six animals per group 37 to 40 days postchallenge.
Data are expressed as levels of log10 resistance calculated by subtracting the log10 mean number of bacilli in the organs of vaccinated animals from the log10 mean number of bacilli in the organs of nonvaccinated animals. NA, not applicable.
DISCUSSION
This study demonstrates that encapsulation of M. bovis BCG in a lipid matrix enhances vaccine efficacy following oral delivery. Consumption of lipid-formulated M. bovis BCG by mice induced strong protective immune responses compared to results with nonformulated M. bovis BCG. This finding is important for developing live vaccines which can be administered through the oral route. Oral delivery of vaccines is also likely to target mucosal immune responses at the barriers where most pathogens enter the host.
Our study extends earlier studies with young children as well as those with mice and guinea pigs which used high doses of oral M. bovis BCG to vaccinate against TB (10, 29). In these studies the oral route of delivery was shown to be less effective than subcutaneous or intradermal administration for preventing aerosol or intravenous infection with TB. High doses of oral M. bovis BCG sometimes resulted in lymphadenitis.
Oral vaccination of BALB/c mice with formulated M. bovis BCG stimulated protective immune responses and provided protection against aerosol challenge with M. bovis. Oral delivery of formulated M. bovis BCG to mice induced strong immune responses—as indicated by tuberculin-induced lymphocyte proliferation responses, IFN-γ levels in the spleen, and macrophage inhibition—compared to nonformulated M. bovis. The results from the time course study showed that the mean IFN-γ response of the oral formulated M. bovis BCG group remained high at 8 weeks after vaccination, while the response for the subcutaneous M. bovis BCG group declined between 4 and 8 weeks after vaccination. Oral vaccination of mice with formulated M. bovis BCG also reduced the number of M. bovis organisms in the spleen and lungs compared to results with mice vaccinated with nonformulated M. bovis BCG, although the level of protection was greater for the subcutaneous M. bovis BCG group at this time point. The immunological data suggested that a more sustained immune response may have been induced in the oral formulated M. bovis BCG group, and further studies are in progress to determine if the level of protection was greater for the oral formulated M. bovis BCG group when the vaccination-challenge interval is increased.
The present results demonstrate that oral formulation of M. bovis BCG enhanced delivery of M. bovis BCG to the immune system. The capacity of formulated M. bovis BCG but not nonformulated M. bovis BCG to stimulate strong systemic immune responses suggests that the formulation procedure protects M. bovis BCG against degradation in the stomach or enables live bacilli to be more efficiently taken up through the gastrointestinal mucosa for processing and presentation to the immune system. Others have shown that high numbers of M. bovis BCG (2 × 109 to 5 × 109 CFU) administered either orally or intragastrically can reduce the bacterial burden in the spleen, liver, and lungs following intravenous challenge with M. tuberculosis (30, 29). Our data show that similar levels of protection can be achieved against aerosol challenge using considerably fewer M. bovis BCG organisms which are protected in a lipid formulation.
Maintenance of BCG viability prior to vaccination is an important first step for oral vaccine formulation since killed M. bovis BCG has been shown to induce weaker protection against TB than live M. bovis BCG (17, 21). The second step is preventing loss of M. bovis BCG viability in the stomach. Finally, successful oral vaccination against TB depends on uptake of viable M. bovis BCG through the gastrointestinal tract and replication of bacilli in the host. In the present study, lipid formulation of M. bovis BCG resulted in minimal loss of viability after storage for up to 16 weeks at 4°C. This suggests that certain lipid preparations are suitable for long-term storage of M. bovis BCG. Further work is required to determine the conditions under which the viability of lipid-formulated M. bovis BCG can be maintained at temperatures above 4°C.
Since formulated oral M. bovis BCG elicited stronger immune responses than nonformulated BCG, we suggest that the formulated M. bovis BCG was protected from degradation in the stomach by the lipid formulation. The majority of enzymes involved in lipolysis are secreted in the lower intestine (13, 25, 44). This may have allowed the lipid formulation to protect M. bovis BCG from the harsh acidic and enzymatic environment of the stomach. In humans, the process of fat digestion begins in the stomach, with a fraction of the triacylglycerols being hydrolyzed by preduodenal lipases (12, 23, 38). The dietary lipids are also emulsified in the stomach by the action of peristalsis (11). However, lipid digestion in the stomach is incomplete, and dietary fats are delivered to the intestinal lumen as crude lipid emulsion particles in association with the undigested triacylglycerols and phospholipids (25, 44). The mechanism of enhanced oral delivery of lipid-formulated BCG remains to be determined, and it is possible that lipids may also act as mucosal adjuvants in the small intestine. Although this study did not examine the in vivo dissemination of viable M. bovis BCG across the gut wall, the observation that immune responses were detected in the spleens of mice suggests that M. bovis BCG was able to attach to and cross the gastrointestinal barrier. Live mycobacteria are known to use the complement receptor and the mannose receptor to bind to and invade epithelial cells (19, 27). The onset of immune responses following oral immunization supports the hypothesis that M. bovis BCG was able to translocate across the gut and replicate in the host. Our data support the hypothesis that M. bovis BCG multiplies following translocation across the gut and that it is the replication of live bacilli in the host that leads to the generation of immune responses and to subsequent protection against TB.
We have previously demonstrated that direct administration of M. bovis BCG into the duodenum induced enhanced immune responses and protection against bovine TB compared to responses following intragastric administration of M. bovis BCG (6). These results showed that administration of M. bovis BCG into the duodenum was an effective means of stimulating mucosal immune responses in the lungs and suggested that if M. bovis BCG vaccine is protected from degradation in the stomach its efficacy should improve.
Lipid-formulated BCG has several properties which distinguish it from the currently available BCG vaccine. The lipid matrix is hydrophobic and is hence able to be stored under humid or moist conditions without gross contamination. Additives can be included in the lipid matrix as required—for example, to improve palatability or survival of the bacteria in vitro or following ingestion. Lastly, the lipid matrix maintains high levels of M. bovis BCG viability and hence vaccine efficacy.
In conclusion, a method of formulating and protecting M. bovis BCG in a viable state for oral delivery has been developed. Oral delivery of formulated M. bovis BCG to mice induced strong immune responses, as indicated by splenic IFN-γ levels and by macrophage inhibition of virulent M. bovis, compared to nonformulated M. bovis BCG. Oral vaccination induced significant protection in mice against aerosol challenge with virulent M. bovis. Our data suggest that formulated oral M. bovis BCG is an effective means of inducing protective immune responses against TB. Lipid-based orally delivered mycobacterial vaccines may be a safe and effective means of controlling TB in humans and animals.
Acknowledgments
This work was supported by a grant from the New Zealand Animal Health Board.
We are grateful for the assistance of Barry Wards for aerosol challenge and Gary Yates and Maree Joyce for the bacteriological examinations. We thank Clare Fitzpatrick for assistance with cytokine ELISAs and BCG survival. We acknowledge the assistance of the staff of the Wallaceville Small Animal Unit and the University of Otago Department of Animal Laboratory Sciences in caring for the mice.
Editor: W. A. Petri, Jr.
REFERENCES
- 1.Aldwell, F. E., D. L. Keen, V. C. Stent, A. Thomson, G. F. Yates, G. W. de Lisle, and B. M. Buddle. 1995. Route of BCG administration in possums affects protection against bovine tuberculosis. N. Z. Vet. J. 43:356-359. [DOI] [PubMed] [Google Scholar]
- 2.Aldwell, F. E., A. Pfeffer, G. W. de Lisle, G. Jowett, J. Heslop, D. Keen, A. Thomson, and B. M. Buddle. 1995. Effectiveness of BCG vaccination in protecting possums against bovine tuberculosis. Res. Vet. Sci. 58:90-95. [DOI] [PubMed] [Google Scholar]
- 3.Aldwell, F. E., D. N. Wedlock, and B. M. Buddle. 1996. Bacterial metabolism, cytokine mRNA transcription and viability of bovine alveolar macrophages infected with Mycobacterium bovis BCG or virulent M. bovis. Immunol. Cell Biol. 74:45-51. [DOI] [PubMed] [Google Scholar]
- 4.Barletta, R. G., B. Snapper, J. D. Cirillo, N. D. Connell, D. D. Kim, W. R. Jacobs, and B. R. Bloom. 1990. Recombinant BCG as a candidate oral vaccine vector. Res. Microbiol. 141:931-939. [DOI] [PubMed] [Google Scholar]
- 5.Brewer, T. F. 2000. Preventing tuberculosis with bacillus Calmette-Guerin vaccine: a meta-analysis of the literature. Clin. Infect. Dis. 31(Suppl. 3):S64-S67. [DOI] [PubMed] [Google Scholar]
- 6.Buddle, B. M., F. E. Aldwell, D. L. Keen, N. A. Parlane, G. Yates, and G. W. de Lisle. 1997. Intraduodenal vaccination of brushtail possums with bacille Calmette-Guerin enhances immune responses and protection against Mycobacterium bovis infection. Int. J. Tuber. Lung Dis. 1:377-383. [PubMed] [Google Scholar]
- 7.Buddle, B. M., F. E. Aldwell, A. Pfeffer, and G. W. de Lisle. 1994. Experimental Mycobacterium bovis infection in the brushtail possum (Trichosurus vulpecula): pathology, haematology and lymphocyte stimulation responses. Vet. Microbiol. 38:241-254. [DOI] [PubMed] [Google Scholar]
- 8.Buddle, B. M., G. W. de Lisle, A. Pfefer, and F. E. Aldwell. 1995. Immunological responses and protection against mycobacterium bovis in calves vaccinated with a low dose of BCG. Vaccine 13:1123-1130. [DOI] [PubMed] [Google Scholar]
- 9.Buddle, B. M., M. A. Skinner, and M. A. Chambers. 2000. Immunological approaches to the control of tuberculosis in wildlife reservoirs. Vet. Immunol. Immunopathol. 74:1-16. [DOI] [PubMed] [Google Scholar]
- 10.Calmette, A., B. Weill-Hallé, A. Saenz, and L. Costil. 1933. Démonstration expérimentale du passage des bacilles vaccins… travers la musqueuse de l' intestin chez l'enfant et chez le singe. Bull. Acad. Med. (Paris) 110:203-206. [Google Scholar]
- 11.Carey, M. C., D. M. Small, and C. M. Bliss. 1983. Lipid digestion and absorption. Annu. Rev. Physiol. 45:651-677. [DOI] [PubMed] [Google Scholar]
- 12.Carriere, F., J. A. Barrowman, R. Verger, and R. Laugier. 1993. Secretion and contribution to lipolysis of gastric and pancreatic lipases during a test meal in humans. Gastroenterology 105:876-888. [DOI] [PubMed] [Google Scholar]
- 13.Charman, W. N., C. J. Porter, S. Mithani, and J. B. Dressman. 1997. Physiochemical and physiological mechanisms for the effects of food on drug absorption: the role of lipids and pH. J. Pharm. Sci. 86:269-282. [DOI] [PubMed] [Google Scholar]
- 14.Colditz, G. A., C. S. Berkey, F. Mosteller, T. F. Brewer, M. E. Wilson, E. Burdick, and H. V. Fineberg. 1995. The efficacy of bacillus Calmette-Guerin vaccination of newborns and infants in the prevention of tuberculosis: meta-analyses of the published literature. Pediatrics 96:29-35. [PubMed] [Google Scholar]
- 15.Colditz, G. A., T. F. Brewer, C. S. Berkey, M. E. Wilson, E. Burdick, H. V. Fineberg, and F. Mosteller. 1994. Efficacy of BCG vaccine in the prevention of tuberculosis. Meta-analysis of the published literature. JAMA 271:698-702. [PubMed] [Google Scholar]
- 16.Cosivi, O., J. M. Grange, C. J. Daborn, M. C. Raviglione, T. Fujikura, D. Cousins, R. A. Robinson, H. F. Huchzermeyer, I. de Kantor, and F. X. Meslin. 1998. Zoonotic tuberculosis due to Mycobacterium bovis in developing countries. Emerg. Infect. Dis. 4:59-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daugelat, S., C. H. Ladel, and S. H. Kaufmann. 1995. Influence of mouse strain and vaccine viability on T-cell responses induced by Mycobacterium bovis bacillus Calmette-Guerin. Infect. Immun. 63:2033-2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dye, C., S. Scheele, P. Dolin, V. Pathania, and M. C. Raviglione. 1999. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. W. H. O. Global Surveillance and Monitoring Project. JAMA 282:677-686. [DOI] [PubMed] [Google Scholar]
- 19.Ehlers, M. R., and M. Daffe. 1998. Interactions between Mycobacterium tuberculosis and host cells: are mycobacterial sugars the key? Trends Microbiol. 6:328-335. [DOI] [PubMed] [Google Scholar]
- 20.Fine, P. E. M. 1995. Variation in protection by BCG: implications of and for heterologous immunity. Lancet 346:1339-1345. [DOI] [PubMed] [Google Scholar]
- 21.Gheorghiu, M., M. Lagranderie, and A. M. Balazuc. 1996. Stabilisation of BCG vaccines. New approaches to stabilisation of vaccine potency. Dev. Biol. Stand. 87:251-261. [PubMed] [Google Scholar]
- 22.Griffin, J. F. T., and G. S. Buchan. 1993. Vaccination against tuberculosis: is BCG more sinned against than sinner? Immunol. Cell Biol. 71:431-442. [DOI] [PubMed] [Google Scholar]
- 23.Hamosh, M., and R. O. Scow. 1973. Lingual lipase and its role in the digestion of dietary lipid. J. Clin. Investig. 52:88-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henning, S. J., and N. Kretchmer. 1973. Development of intestinal function in mammals. Enzyme 15:3-23. [PubMed] [Google Scholar]
- 25.Hernell, O., J. E. Staggers, and M. C. Carey. 1990. Physical-chemical behavior of dietary and biliary lipids during intestinal digestion and absorption. 2. Phase analysis and aggregation states of luminal lipids during duodenal fat digestion in healthy adult human beings. Biochemistry 29:2041-2056. [DOI] [PubMed] [Google Scholar]
- 26.Hubbard, R. D., and F. M. Collins. 1991. Immunomodulation of mouse macrophage killing of Mycobacterium avium in vitro. Infect. Immun. 59:570-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kang, B. K., and L. S. Schlesinger. 1998. Characterization of mannose receptor-dependent phagocytosis mediated by Mycobacterium tuberculosis lipoarabinomannan. Infect. Immun. 66:2769-2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lagranderi, M., A. Murray, G. Gicquel, C. Leclerc, and M. Gheorghiu. 1993. Oral immunization with recombinant BCG induces cellular and humoral immune responses against the foreign antigen. Vaccine 11:1283-1290. [DOI] [PubMed] [Google Scholar]
- 29.Lagranderie, M., P. Chavarot, A. M. Balazuc, and G. Marchal. 2000. Immunogenicity and protective capacity of Mycobacterium bovis BCG after oral or intragastric administration in mice. Vaccine 18:1186-1195. [DOI] [PubMed] [Google Scholar]
- 30.Lagranderie, M. R. R., A.-M. Balazuc, E. Deriaud, C. D. Leclerc, and M. Gheorghiu. 1996. Comparison of immune responses of mice immunized with five different Mycobacterium bovis BCG vaccine strains. Infect. Immun. 64:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liebana, E., A. Aranaz, M. Welsh, S. D. Neill, and J. M. Pollock. 2000. In vitro T-cell activation of monocyte-derived macrophages by soluble messengers or cell-to-cell contact in bovine tuberculosis. Immunology 100:194-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lowe, M. E., M. H. Kaplan, L. Jackson-Grusby, D. D'Agostino, and M. J. Grusby. 1998. Decreased neonatal dietary fat absorption and T cell cytotoxicity in pancreatic lipase-related protein 2-deficient mice. J. Biol. Chem. 273:31215-31221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lugosi, L. 1992. Theoretical and methodological aspects of BCG vaccine from the discovery of Calmette and Guerin to molecular biology. A review. Tuber. Lung Dis. 73:252-261. [DOI] [PubMed] [Google Scholar]
- 34.McMurray, D. N., F. M. Collins, A. M. Dannenberg, Jr., and D. W. Smith. 1996. Pathogenesis of experimental tuberculosis in animal models. Curr. Top. Microbiol. Immunol. 215:157-179. [DOI] [PubMed] [Google Scholar]
- 35.McMurray, D. N., M. S. Kimball, C. L. Tetzlaff, and C. L. Mintzer. 1986. Effects of protein deprivation and BCG vaccination on alveolar macrophage function in pulmonary tuberculosis. Am. Rev. Respir. Dis. 133:1081-1085. [DOI] [PubMed] [Google Scholar]
- 36.Muller-Schoop, J. W., and R. A. Good. 1975. Functional studies of Peyer's patches: evidence for their participation in intestinal immune responses. J. Immunol. 114:1757-1760. [PubMed] [Google Scholar]
- 37.Raviglione, M. C., D. E. Snider, Jr., and A. Kochi. 1995. Global epidemiology of tuberculosis. Morbidity and mortality of a worldwide epidemic. JAMA 273:220-226. [PubMed] [Google Scholar]
- 38.Roy, C. C., M. Roulet, D. Lefebvre, L. Chartrand, G. Lepage, and L. A. Fournier. 1979. The role of gastric lipolysis on fat absorption and bile acid metabolism in the rat. Lipids 14:811-815. [DOI] [PubMed] [Google Scholar]
- 39.Silver, R. F., Q. Li, and J. J. Ellner. 1998. Expression of virulence of Mycobacterium tuberculosis within human monocytes: virulence correlates with intracellular growth and induction of tumor necrosis factor alpha but not with evasion of lymphocyte-dependent monocyte effector functions. Infect. Immun. 66:1190-1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith, D. W., D. N. McMurray, E. H. Wiegeshaus, A. A. Grover, and G. E. Harding. 1970. Host-parasite relationships in experimental airborne tuberculosis. IV. Early events in the course of infection in vaccinated and nonvaccinated guinea pigs. Am. Rev. Respir. Dis. 102:937-949. [DOI] [PubMed] [Google Scholar]
- 41.Stover, C. K., V. F. de la Cruz, T. R. Fuerst, J. E. Burlein, L. A. Benson, L. T. Bennett, G. P. Bansal, J. F. Young, M. H. Lee, G. F. Hatfull, S. B. Snapper, R. G. Barletta, W. R. Jacobs, and B. R. Bloom. 1991. New use of BCG for recombinant vaccines. Nature 351:456-460. [DOI] [PubMed] [Google Scholar]
- 42.Wiegeshaus, E. H., D. N. McMurray, A. A. Grover, G. E. Harding, and D. W. Smith. 1970. Host-parasite relationships in experimental airborne tuberculosis. 3. Relevance of microbial enumeration to acquired resistance in guinea pigs. Am. Rev. Respir. Dis. 102:422-429. [DOI] [PubMed] [Google Scholar]
- 43.Worku, S., and D. F. Hoft. 2000. In vitro measurement of protective mycobacterial immunity: antigen-specific expansion of T cells capable of inhibiting intracellular growth of bacille Calmette-Guerin. Clin. Infect. Dis. 30(Suppl. 3):S257-S261. [DOI] [PubMed] [Google Scholar]
- 44.Young, S. C., and D. Y. Hui. 1999. Pancreatic lipase/colipase-mediated triacylglycerol hydrolysis is required for cholesterol transport from lipid emulsions to intestinal cells. Biochem. J. 339:615-620. [PMC free article] [PubMed] [Google Scholar]