Abstract
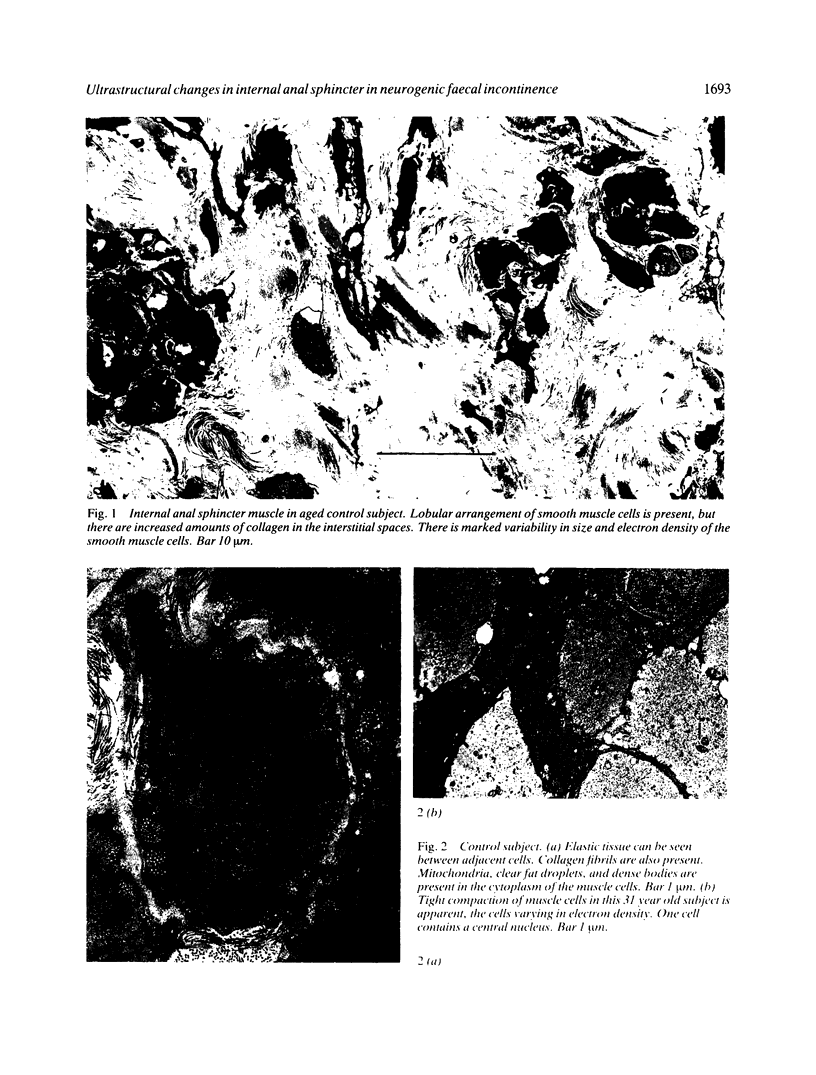
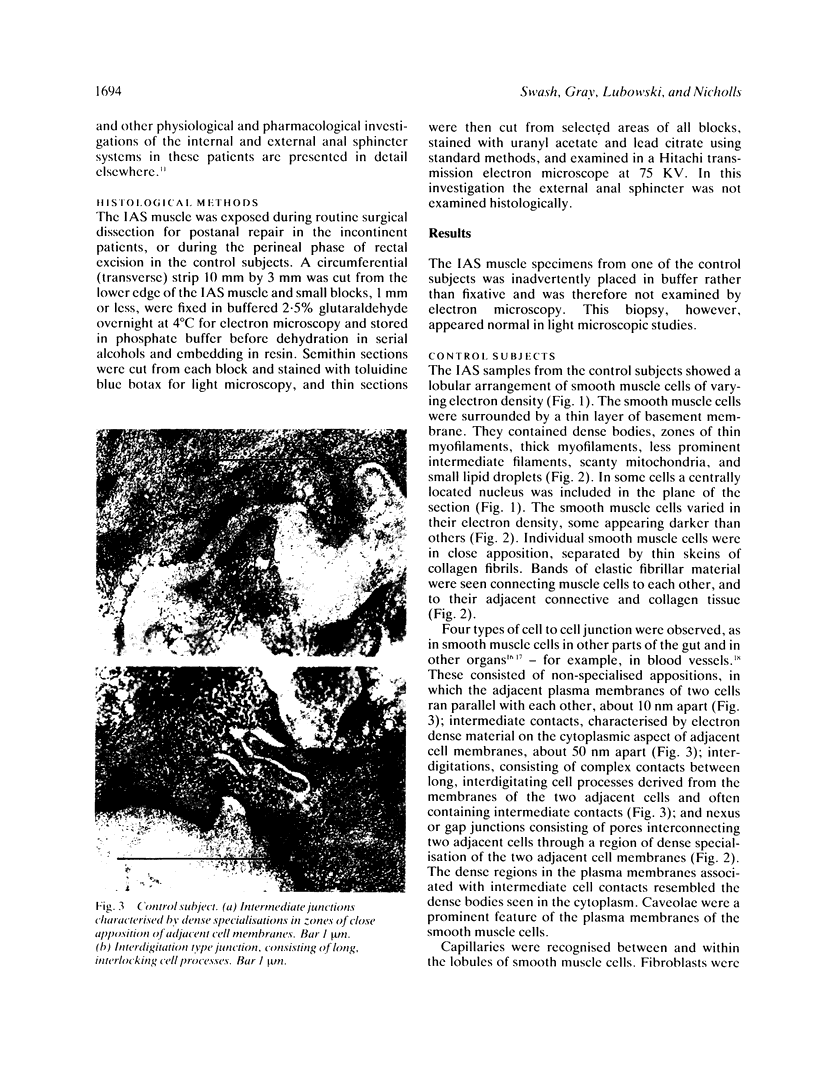
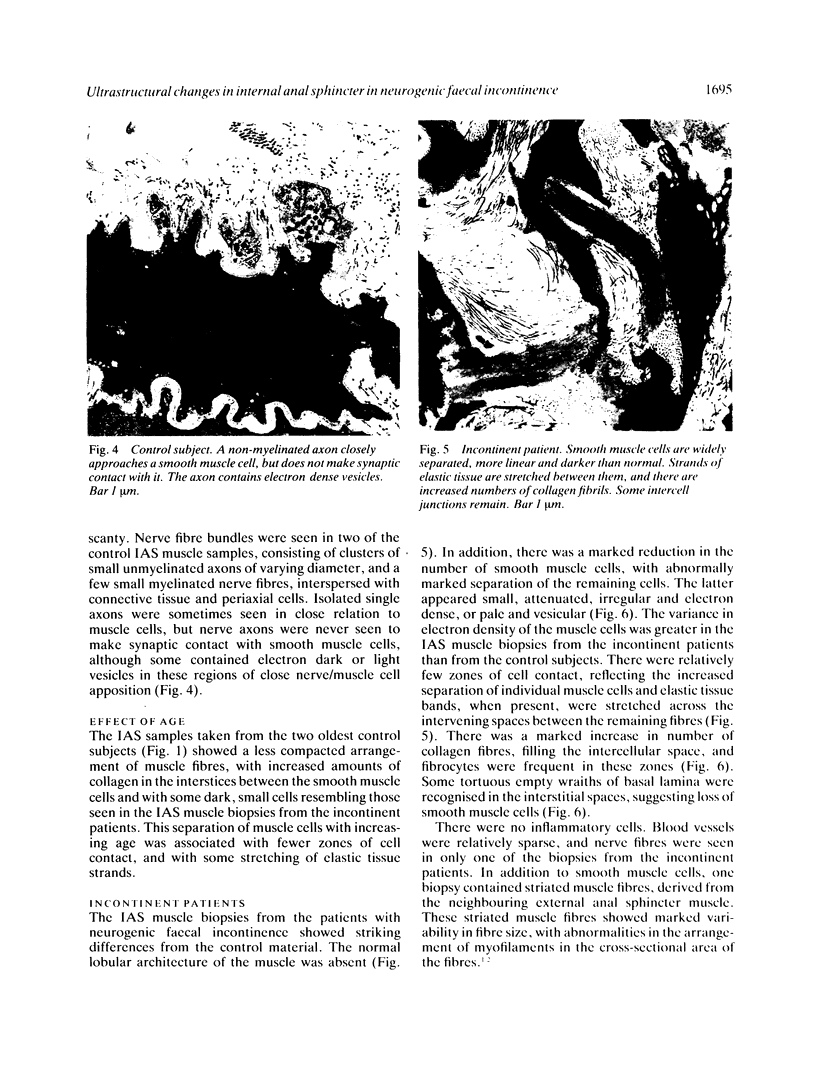
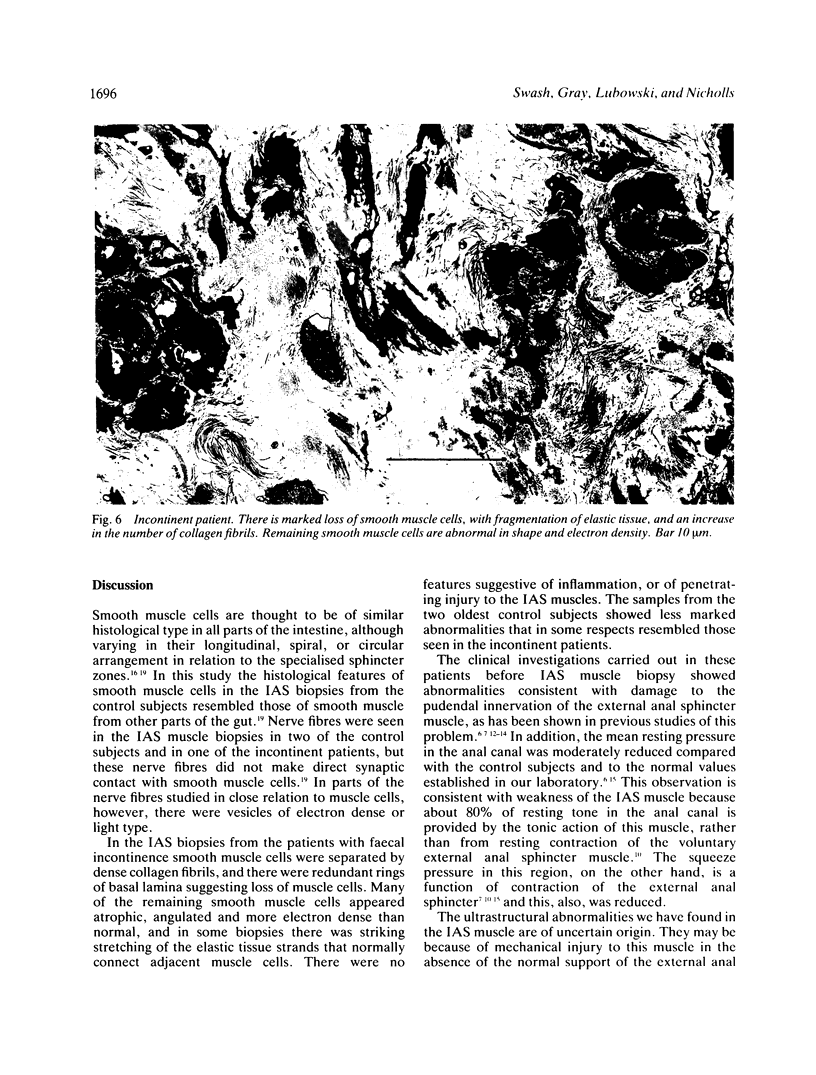
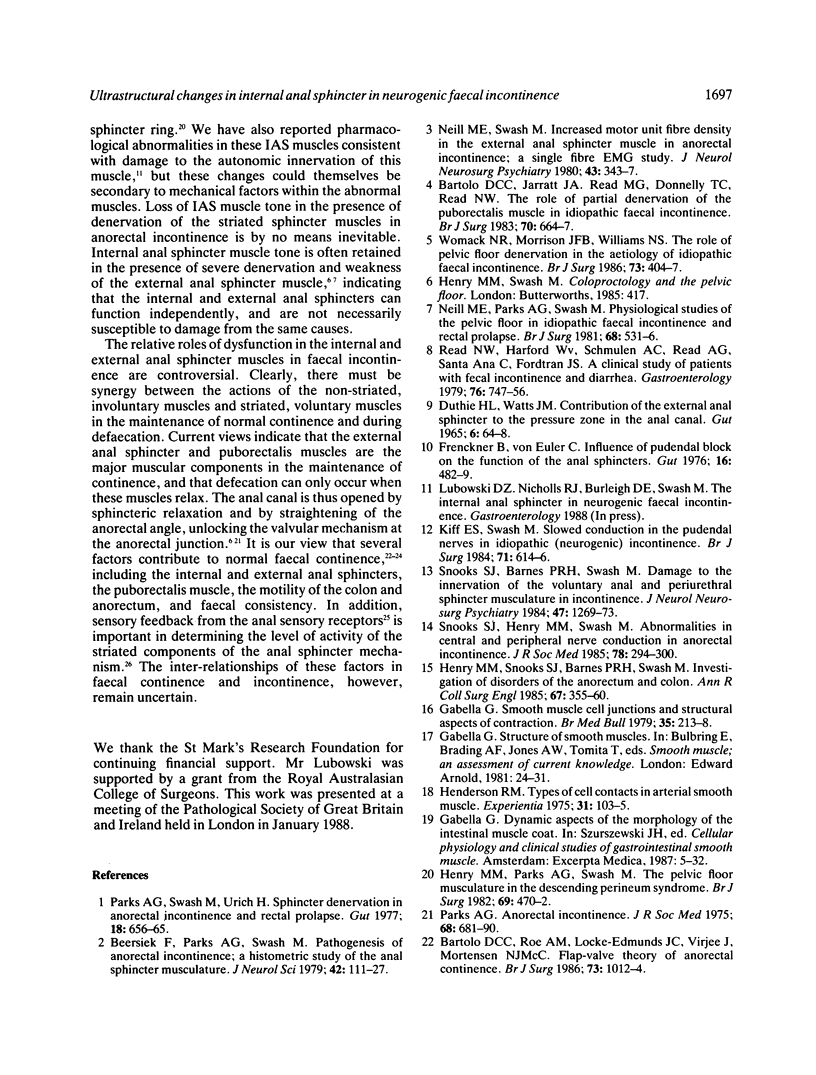
The ultrastructural features of the internal anal sphincter (IAS) muscle were studied in biopsies from five patients with neurogenic anorectal incontinence and six control subjects undergoing anorectal excision for cancer, or for inflammatory bowel disease. In the patients with idiopathic neurogenic anorectal incontinence the internal anal sphincter showed loss of smooth muscle cells, disruption of the normal relationships of the remaining cells, stretching of elastic tissue, and increased collagen fibril content. These ultrastructural changes in the morphology of the internal anal sphincter, although probably not the primary cause of faecal incontinence, have functional relevance in the clinical syndrome, as shown by the reduction in resting anal canal pressure found in some patients with this syndrome.
Full text
PDF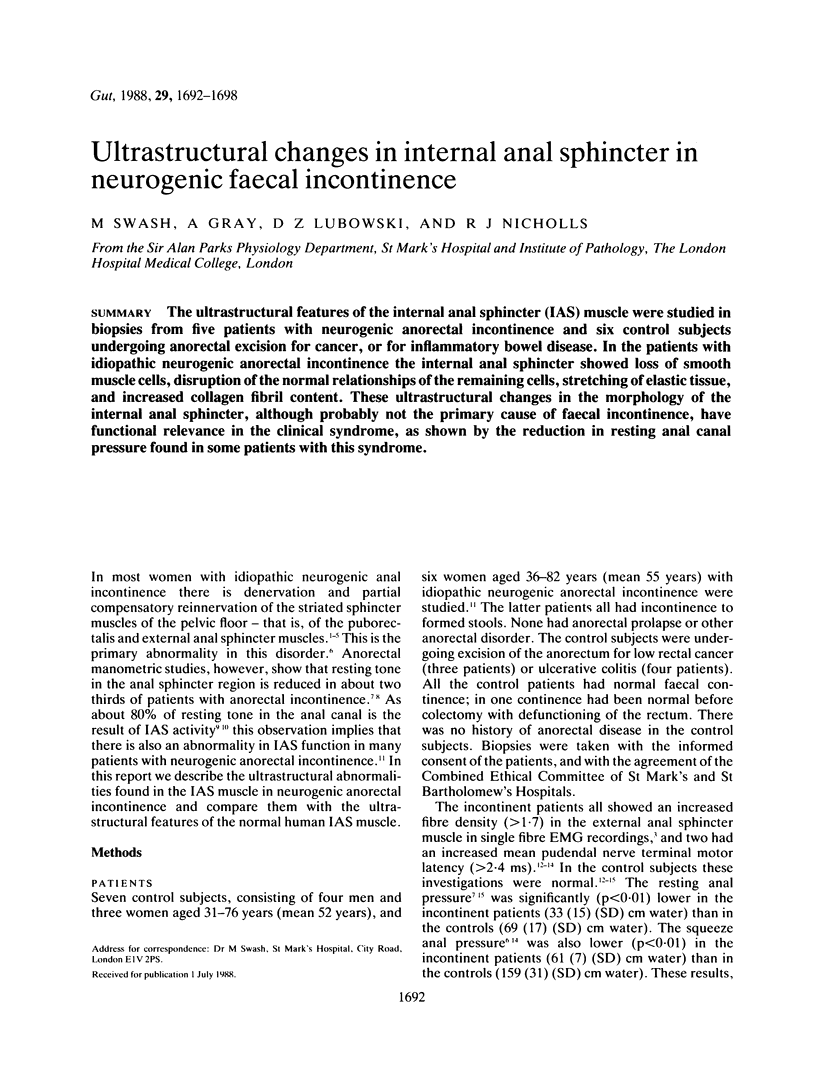
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bartolo D. C., Jarratt J. A., Read M. G., Donnelly T. C., Read N. W. The role of partial denervation of the puborectalis in idiopathic faecal incontinence. Br J Surg. 1983 Nov;70(11):664–667. doi: 10.1002/bjs.1800701108. [DOI] [PubMed] [Google Scholar]
- Bartolo D. C., Roe A. M., Locke-Edmunds J. C., Virjee J., Mortensen N. J. Flap-valve theory of anorectal continence. Br J Surg. 1986 Dec;73(12):1012–1014. doi: 10.1002/bjs.1800731227. [DOI] [PubMed] [Google Scholar]
- Beersiek F., Parks A. G., Swash M. Pathogenesis of ano-rectal incontinence. A histometric study of the anal sphincter musculature. J Neurol Sci. 1979 Jun;42(1):111–127. doi: 10.1016/0022-510x(79)90156-4. [DOI] [PubMed] [Google Scholar]
- DUTHIE H. L., GAIRNS F. W. Sensory nerve-endings and sensation in the anal region of man. Br J Surg. 1960 May;47:585–595. doi: 10.1002/bjs.18004720602. [DOI] [PubMed] [Google Scholar]
- DUTHIE H. L., WATTS J. M. CONTRIBUTION OF THE EXTERNAL ANAL SPHINCTER TO THE PRESSURE ZONE IN THE ANAL CANAL. Gut. 1965 Feb;6:64–68. doi: 10.1136/gut.6.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenckner B., Euler C. V. Influence of pudendal block on the function of the anal sphincters. Gut. 1975 Jun;16(6):482–489. doi: 10.1136/gut.16.6.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabella G. Smooth muscle cell junctions and structural aspects of contraction. Br Med Bull. 1979 Sep;35(3):213–218. doi: 10.1093/oxfordjournals.bmb.a071580. [DOI] [PubMed] [Google Scholar]
- Henderson R. M. Types of cell contacts in arterial smooth muscle. Experientia. 1975 Jan 15;31(1):103–105. doi: 10.1007/BF01924703. [DOI] [PubMed] [Google Scholar]
- Henry M. M., Parks A. G., Swash M. The pelvic floor musculature in the descending perineum syndrome. Br J Surg. 1982 Aug;69(8):470–472. doi: 10.1002/bjs.1800690813. [DOI] [PubMed] [Google Scholar]
- Henry M. M., Snooks S. J., Barnes P. R., Swash M. Investigation of disorders of the anorectum and colon. Ann R Coll Surg Engl. 1985 Nov;67(6):355–360. [PMC free article] [PubMed] [Google Scholar]
- Kiff E. S., Swash M. Slowed conduction in the pudendal nerves in idiopathic (neurogenic) faecal incontinence. Br J Surg. 1984 Aug;71(8):614–616. doi: 10.1002/bjs.1800710817. [DOI] [PubMed] [Google Scholar]
- Neill M. E., Parks A. G., Swash M. Physiological studies of the anal sphincter musculature in faecal incontinence and rectal prolapse. Br J Surg. 1981 Aug;68(8):531–536. doi: 10.1002/bjs.1800680804. [DOI] [PubMed] [Google Scholar]
- Neill M. E., Swash M. Increased motor unit fibre density in the external anal sphincter muscle in ano-rectal incontinence: a single fibre EMG study. J Neurol Neurosurg Psychiatry. 1980 Apr;43(4):343–347. doi: 10.1136/jnnp.43.4.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks A. G. Royal Society of Medicine, Section of Proctology; Meeting 27 November 1974. President's Address. Anorectal incontinence. Proc R Soc Med. 1975 Nov;68(11):681–690. doi: 10.1177/003591577506801105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks A. G., Swash M., Urich H. Sphincter denervation in anorectal incontinence and rectal prolapse. Gut. 1977 Aug;18(8):656–665. doi: 10.1136/gut.18.8.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read N. W., Harford W. V., Schmulen A. C., Read M. G., Santa Ana C., Fordtran J. S. A clinical study of patients with fecal incontinence and diarrhea. Gastroenterology. 1979 Apr;76(4):747–756. [PubMed] [Google Scholar]
- Rogers J., Henry M. M., Misiewicz J. J. Combined sensory and motor deficit in primary neuropathic faecal incontinence. Gut. 1988 Jan;29(1):5–9. doi: 10.1136/gut.29.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snooks S. J., Barnes P. R., Swash M. Damage to the innervation of the voluntary anal and periurethral sphincter musculature in incontinence: an electrophysiological study. J Neurol Neurosurg Psychiatry. 1984 Dec;47(12):1269–1273. doi: 10.1136/jnnp.47.12.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snooks S. J., Swash M., Henry M. M. Abnormalities in central and peripheral nerve conduction in patients with anorectal incontinence. J R Soc Med. 1985 Apr;78(4):294–300. doi: 10.1177/014107688507800405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Womack N. R., Morrison J. F., Williams N. S. The role of pelvic floor denervation in the aetiology of idiopathic faecal incontinence. Br J Surg. 1986 May;73(5):404–407. doi: 10.1002/bjs.1800730531. [DOI] [PubMed] [Google Scholar]