Abstract
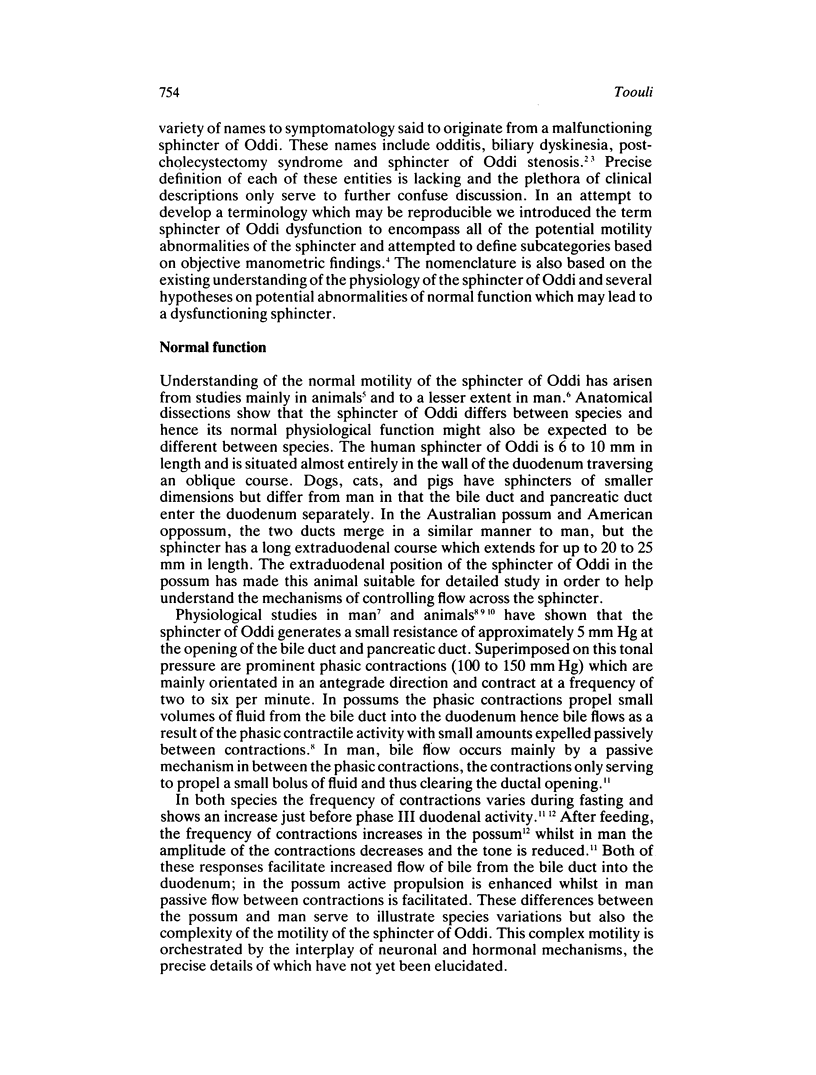
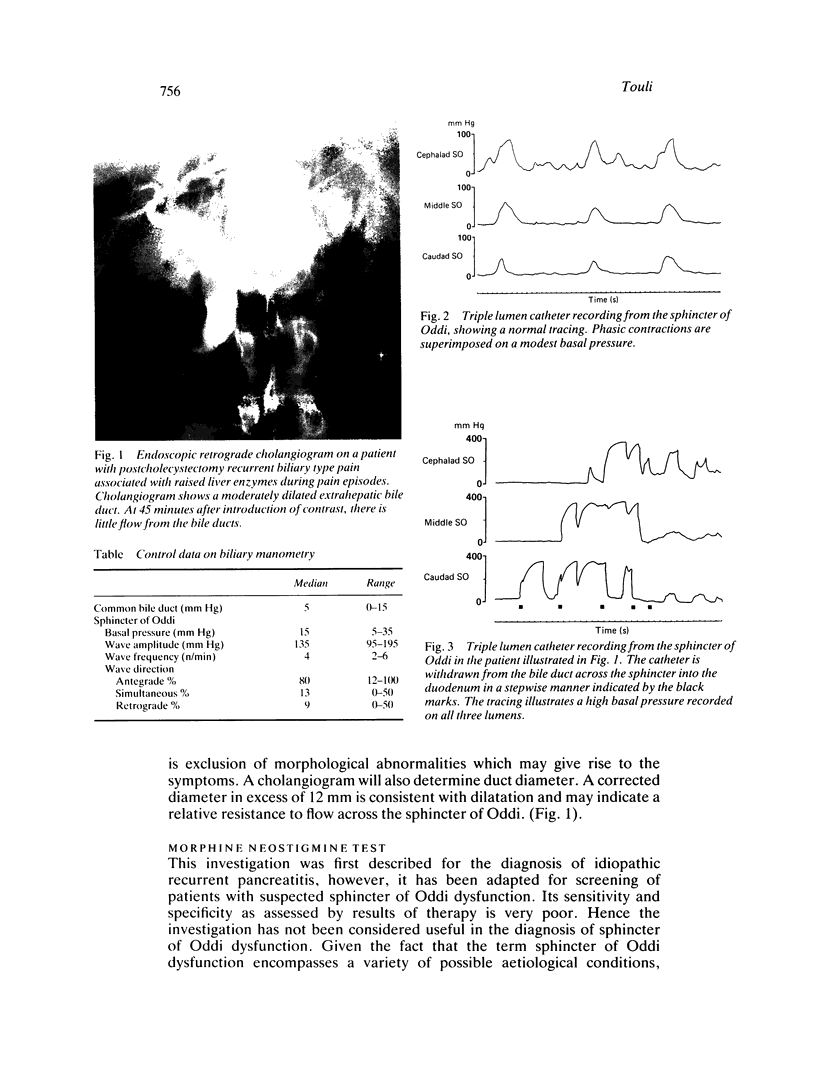
Ever since its description approximately 100 years ago, the sphincter of Oddi has been surrounded by controversy. First, whether it indeed existed, second, whether it had a significant physiological role in man and more recently whether abnormalities in its function give rise to a clinical syndrome. Data from animal and human studies, using sensitive techniques, have helped define the physiological role of the sphincter of Oddi, and more recent studies are determining the factors which control sphincter of Oddi function. These studies support Oddi's original description that the sphincter has a major role in the control of flow of bile and pancreatic juice into the duodenum, and equally importantly helps prevent the reflux of duodenal contents into the biliary and pancreatic ductal systems. The controversy of whether abnormalities in sphincter of Oddi motility result in clinical syndromes has not been totally resolved. Part of the difficulty has been inability to document normal and hence abnormal function of the sphincter. With the emergence of endoscopic biliary manometry as a sensitive and reproducible technique, however, the motility of the human sphincter of Oddi has come under closer scrutiny and allowed definition of possible disorders. We have used the term sphincter of Oddi dysfunction to define manometric abnormalities in patients who present with signs and symptoms consistent with a biliary or pancreatic ductal origin. Based on the manometry, we have subdivided the dysfunction into two groups; a group characterised by a stenotic pattern - that is, raised sphincter basal pressure - and a second group having a dyskinetic pattern - that is, paradoxical response to cholecystokinin injection, rapid contraction frequency, high percentage of retrograde contractions, or short periods of raised basal percentage of retrograde contractions, or short periods of raised basal pressure. It is apparent from the mamometry but also from the clinical data that the patients are a heterogeneous group and thus any therapy would need to be tailored for each patient and abnormality. The most recent therapeutic data suggest that patients with the stenotic pattern on manometry respond to division of the sphincter, however, those patients with the dyskinetic manometric pattern show no significant effect after sphincterotomy. Further prospective trials evaluating therapeutic options are under way and their results are eagerly awaited.
Full text
PDF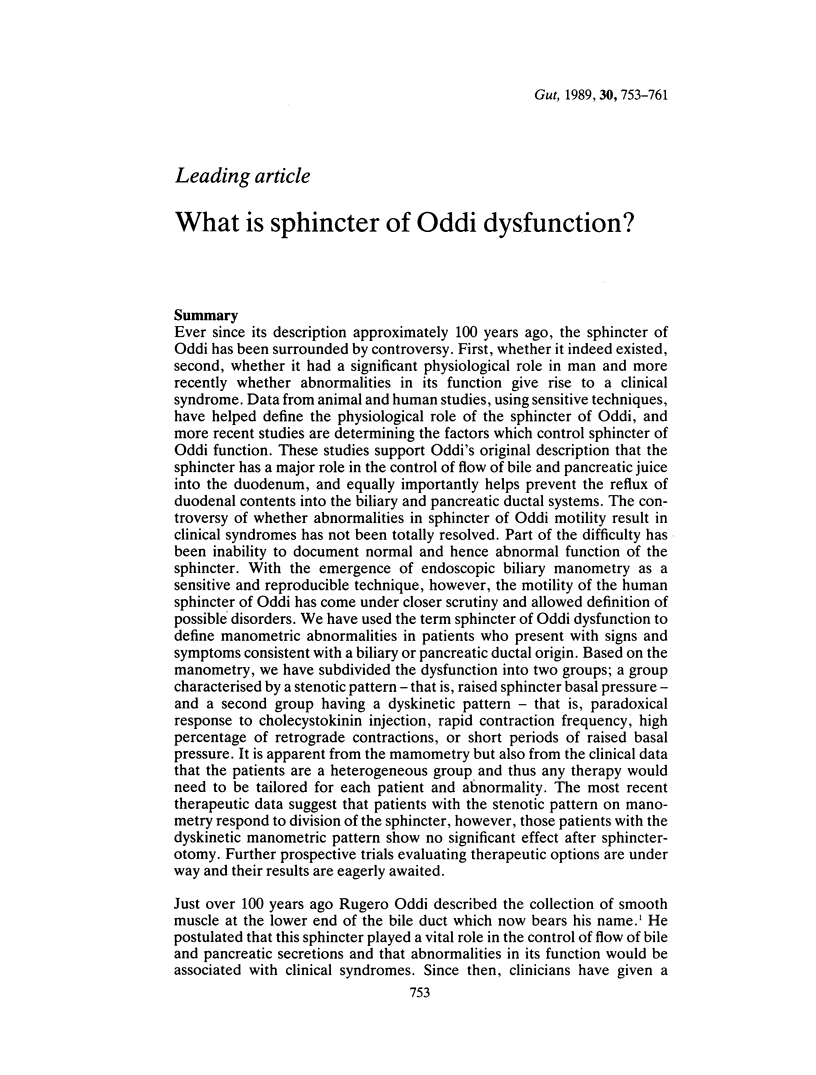

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BERCI G., JOHNSON N. FUNCTIONAL STUDIES OF THE EXTRAHEPATIC BILIARY SYSTEM IN THE DOG BY USE OF A CONTROLLED BILIARY FISTULA. Ann Surg. 1965 Feb;161:286–292. doi: 10.1097/00000658-196502000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BOYDEN E. A. The anatomy of the choledochoduodenal junction in man. Surg Gynecol Obstet. 1957 Jun;104(6):641–652. [PubMed] [Google Scholar]
- Bar-Meir S., Halpern Z., Bardan E. Nitrate therapy in a patient with papillary dysfunction. Am J Gastroenterol. 1983 Feb;78(2):94–95. [PubMed] [Google Scholar]
- Behar J., Biancani P. Effect of cholecystokinin and the octapeptide of cholecystokinin on the feline sphincter of Oddi and gallbladder. Mechanisms of action. J Clin Invest. 1980 Dec;66(6):1231–1239. doi: 10.1172/JCI109974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolondi L., Gaiani S., Gullo L., Labò G. Secretin administration induces a dilatation of main pancreatic duct. Dig Dis Sci. 1984 Sep;29(9):802–808. doi: 10.1007/BF01318422. [DOI] [PubMed] [Google Scholar]
- Darweesh R. M., Dodds W. J., Hogan W. J., Geenen J. E., Collier B. D., Shaker R., Kishk S. M., Stewart E. T., Lawson T. L., Hassanein E. H. Efficacy of quantitative hepatobiliary scintigraphy and fatty-meal sonography for evaluating patients with suspected partial common duct obstruction. Gastroenterology. 1988 Mar;94(3):779–786. doi: 10.1016/0016-5085(88)90254-5. [DOI] [PubMed] [Google Scholar]
- Dodds W. J., Dent J., Hogan W. J., Patel G. K., Toouli J., Arndorfer R. C. Paradoxical lower esophageal sphincter contraction induced by cholecystokinin-octapeptide in patients with achalasia. Gastroenterology. 1981 Feb;80(2):327–333. [PubMed] [Google Scholar]
- Funch-Jensen P., Kruse A., Ravnsbaek J. Endoscopic sphincter of Oddi manometry in healthy volunteers. Scand J Gastroenterol. 1987 Mar;22(2):243–249. doi: 10.3109/00365528708991887. [DOI] [PubMed] [Google Scholar]
- Geenen J. E., Hogan W. J., Dodds W. J., Stewart E. T., Arndorfer R. C. Intraluminal pressure recording from the human sphincter of Oddi. Gastroenterology. 1980 Feb;78(2):317–324. [PubMed] [Google Scholar]
- Gregg J. A., Carr-Locke D. L. Endoscopic pancreatic and biliary manometry in pancreatic, biliary, and papillary disease, and after endoscopic sphincterotomy and surgical sphincteroplasty. Gut. 1984 Nov;25(11):1247–1254. doi: 10.1136/gut.25.11.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda R., Toouli J., Dodds W. J., Sarna S., Hogan W. J., Itoh Z. Relationship of sphincter of Oddi spike bursts to gastrointestinal myoelectric activity in conscious opossums. J Clin Invest. 1982 Apr;69(4):770–778. doi: 10.1172/JCI110515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R. G., Gregg J. A., Koroshetz A. M., Hill T. C., Clouse M. E. Sphincter of Oddi stenosis: diagnosis using hepatobiliary scintigraphy and endoscopic manometry. Radiology. 1985 Sep;156(3):793–796. doi: 10.1148/radiology.156.3.4023245. [DOI] [PubMed] [Google Scholar]
- Moody F. G., Becker J. M., Potts J. R. Transduodenal sphincteroplasty and transampullary septectomy for postcholecystectomy pain. Ann Surg. 1983 May;197(5):627–636. doi: 10.1097/00000658-198305000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nardi G. L., Michelassi F., Zannini P. Transduodenal sphincteroplasty. 5-25 year follow-up of 89 patients. Ann Surg. 1983 Oct;198(4):453–461. doi: 10.1097/00000658-198310000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nardi G. L. Papillitis and stenosis of the sphincter of Oddi. Surg Clin North Am. 1973 Oct;53(5):1149–1160. doi: 10.1016/s0039-6109(16)40143-x. [DOI] [PubMed] [Google Scholar]
- Roberts-Thomson I. C., Toouli J. Abnormal responses to morphine-neostigmine in patients with undefined biliary type pain. Gut. 1985 Dec;26(12):1367–1372. doi: 10.1136/gut.26.12.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts-Thomson I. C., Toouli J., Blanchett W., Lichtenstein M., Andrews J. T. Assessment of bile flow by radioscintigraphy in patients with biliary-type pain after cholecystectomy. Aust N Z J Med. 1986 Dec;16(6):788–793. doi: 10.1111/j.1445-5994.1986.tb00038.x. [DOI] [PubMed] [Google Scholar]
- Steinberg W. M. Sphincter of Oddi dysfunction: a clinical controversy. Gastroenterology. 1988 Nov;95(5):1409–1415. doi: 10.1016/0016-5085(88)90381-2. [DOI] [PubMed] [Google Scholar]
- Tondelli P., Gyr K. Biliary tract disorders. Postsurgical syndromes. Clin Gastroenterol. 1983 Jan;12(1):231–254. [PubMed] [Google Scholar]
- Tondelli P., Gyr K., Stalder G. A., Allgöwer M. The biliary tract. Part I: Cholecystectomy. Clin Gastroenterol. 1979 May;8(2):487–505. [PubMed] [Google Scholar]
- Toouli J., Dodds W. J., Honda R., Sarna S., Hogan W. J., Komarowski R. A., Linehan J. H., Arndorfer R. C. Motor function of the opossum sphincter of Oddi. J Clin Invest. 1983 Feb;71(2):208–220. doi: 10.1172/JCI110761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toouli J., Geenen J. E., Hogan W. J., Dodds W. J., Arndorfer R. C. Sphincter of Oddi motor activity: a comparison between patients with common bile duct stones and controls. Gastroenterology. 1982 Jan;82(1):111–117. [PubMed] [Google Scholar]
- Toouli J., Roberts-Thomson I. C., Dent J., Lee J. Manometric disorders in patients with suspected sphincter of Oddi dysfunction. Gastroenterology. 1985 May;88(5 Pt 1):1243–1250. doi: 10.1016/s0016-5085(85)80086-x. [DOI] [PubMed] [Google Scholar]
- Toouli J., Roberts-Thomson I. C., Dent J., Lee J. Sphincter of Oddi motility disorders in patients with idiopathic recurrent pancreatitis. Br J Surg. 1985 Nov;72(11):859–863. doi: 10.1002/bjs.1800721104. [DOI] [PubMed] [Google Scholar]
- Toouli J., Roberts-Thomson I. C., Dent J., Lee J. Sphincter of Oddi motility disorders in patients with idiopathic recurrent pancreatitis. Br J Surg. 1985 Nov;72(11):859–863. doi: 10.1002/bjs.1800721104. [DOI] [PubMed] [Google Scholar]
- Torsoli A., Corazziari E., Habib F. I., De Masi E., Biliotti D., Mazzarella R., Giubilei D., Fegiz G. Frequencies and cyclical pattern of the human sphincter of Oddi phasic activity. Gut. 1986 Apr;27(4):363–369. doi: 10.1136/gut.27.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeman R. K., Burrell M. I., Dobbins J., Jaffe M. H., Choyke P. L. Postcholecystectomy syndrome: evaluation using biliary scintigraphy and endoscopic retrograde cholangiopancreatography. Radiology. 1985 Sep;156(3):787–792. doi: 10.1148/radiology.156.3.4023244. [DOI] [PubMed] [Google Scholar]