Abstract
A whole-body mouse model of pneumonic melioidosis was established for future evaluation of biodefense vaccine candidates. The aerosol 50% lethal doses of Burkholderia pseudomallei strain 1026b for BALB/c and C57BL/6 mice and the times to death, dissemination in organs, and tissue loads after exposure of the mice to low- and high-dose aerosols are reported. In addition, rpsL mutant backgrounds were attenuated in this acute model of disease.
The etiologic agent of human and animal melioidosis is Burkholderia pseudomallei (5, 17). Both B. pseudomallei and its close species relative Burkholderia mallei are microbes recognized as having the potential for misuse as biological weapons (1). Typically, signs of pneumonia in patients with clinical melioidosis are a secondary result of sepsis (5). Presumably, victims suffering from a biological attack that employed B. pseudomallei or B. mallei would present clinically with pneumonic disease as the initial aspect. In order to develop a vaccine program for defending U.S. military forces against a potential B. mallei or B. pseudomallei attack, whole-body aerosol laboratory models of disease were established. With these murine melioidosis models, future vaccine candidates can be evaluated and tested for efficacy.
B. pseudomallei strain 1026b was selected because of its ease of genetic manipulation, its ability to replace genes, and its previously characterized virulence (6, 17). The 50% lethal dose (LD50) of strain 1026b for hamsters is <10 bacteria by intraperitoneal (i.p.) administration. Deleting the multidrug efflux pump encoded by the amrR, amrA, amrB, and oprA genes yields the aminoglycoside- and macrolide-sensitive strain DD503 (12). This strain retains a streptomycin resistance phenotype by virtue of a chromosomal mutation in the rpsL gene (12). rpsL encodes a ribosomal-subunit protein which regulates translational fidelity (3). The deletion of the multidrug efflux pump combined with an rpsL mutation generates the correct genotype for facilitating streptomycin-mediated gene replacement. There is no difference in the relative levels of virulence displayed by strains 1026b and DD503 in the Syrian hamster model of acute melioidosis (12).
Recently, a mucosal model of melioidosis which demonstrated that BALB/c and C57BL/6 mice display very different disease outcomes was reported (11). The BALB/c mice succumbed to an acute infection with an altered cytokine response, unlike the more resistant C57BL/6 mice. Because we also found that C57BL/6 mice are more resistant to B. mallei infections when the organisms are administered i.p., we thought it important to explore any correlation within an inhalation disease model (7).
Bacterial strains used in this study are described in Table 1. The whole-body aerosols were generated by nebulization of Luria broth-diluted overnight cultures in a modified Henderson apparatus by a previously described methodology (4, 16). Groups of 10 6- to 8-week-old female mice were exposed to the whole-body aerosol for 10 min. The aerosol concentration in the chamber was calculated on the basis of the number of CFU recovered from an integrated exposure chamber sample and on the exposure time. The dose inhaled was then derived on the basis of the respiratory minute volume of 6- to 8-week-old mice as estimated from the average weight of the animals (4, 8, 16).
TABLE 1.
Burkholderia strains used for this study
| Strain | Relevant genotype | Reference |
|---|---|---|
| 1026b | B. pseudomallei wild-type clinical isolate | 6 |
| DD503 | 1026b Δ(amrA-oprA) rpsL (Smr) | 12 |
| RM102 | 1026b amrB::Tn5 (Tcr) | 12 |
| RM102 SmR | 1026b amrB::Tn5 rpsL(Tcr Smr) | 12 |
| ATCC 23344 | B. mallei wild-type clinical isolate | 18 |
Table 2 depicts the average results of two LD50 determinations for respiratory exposure to B. pseudomallei strains 1026b and DD503, with BALB/c and C57BL/6 mice as the hosts. In each repetition, five groups of 10 mice were exposed to five different aerosols, each containing an increasing density of B. pseudomallei. The targeted delivery doses were 10, 100, 1,000, 10,000, and 100,000 CFU. Actual dose groups received approximately 5, 50, 500, 5,000, and 50,000 CFU. BALB/c and C57BL/6 mice were sensitive to aerosols containing wild-type strain 1026b (13). The LD50 was calculated for each experiment with the Reed-Muench method (14), and the means (± standard deviations) are reported in Table 2. The LD50 of 1026b was approximately 10 ± 8 CFU when it was inhaled by a BALB/c mouse and 27 ± 20 CFU when it was inhaled by a C57BL/6 mouse. The virulence of DD503 was attenuated relative to that of its parent; the LD50 of DD503 was 1,467 ± 301 CFU in BALB/c mice. At equivalent doses, 1026b killed almost 2 days faster than DD503 (data not shown).
TABLE 2.
Mouse LD50 determinations for inhalation of Burkholderia strains
| Mouse genetic background | LD50 (CFU) (mean ± SD)
|
||
|---|---|---|---|
| 1026b | DD503 | ATCC 23344 | |
| BALB/c | 10 ± 8 | 1,467 ± 301 | 1,000a |
| C57BL/6 | 27 ± 20 | NDb | ND |
Unpublished data (D. Fritz and D. Waag, U.S. Army Medical Research Institute of Infectious Diseases).
ND, not done.
Studies by Liu et al. showed that the genetic background of a mouse played a major role in determining disease outcome (11). C57BL/6 mice exhibited approximately 2-log-greater resistance to intranasally delivered B. pseudomallei than BALB/c mice (11). Our observations suggest that both types of mice displayed similar sensitivities to nebulized B. pseudomallei. We do not believe that the discrepancy in outcomes is solely attributable to our strain selection or to the C57BL/6 genetic background of our mice. Early work by the Naval Research Office (13) and our collaborators at Defence Sciences Technology Laboratories (Porton Down, United Kingdom) found that BALB/c animals display similar sensitivities to different strains of nebulized B. pseudomallei (M. S. Lever, personal communication). We believe it more likely that the great differences in levels of virulence observed by Liu et al. were probably due to the method of intranasal delivery employed. The large differences reported are similar to the differences seen between i.p. and intravenous challenge models reported by other groups (2, 10, 13, 15).
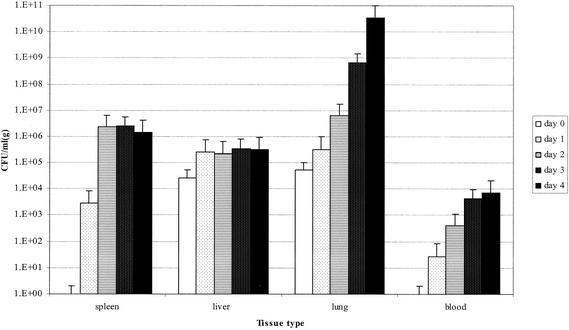
Figure 1 depicts the results from a serial sacrifice experiment after delivery of a high-dose (∼1,000 LD50s) aerosol to BALB/c mice. Twenty-five mice were exposed to whole-body aerosols containing B. pseudomallei 1026b or DD503. At 24-h intervals, five animals were humanely sacrificed, four had their organs harvested for tissue load determination, and the final mouse was preserved in formalin for future histology studies. The numbers of deaths by day for strain 1026b were 0 deaths on day 1, 10 deaths on day 2, and 4 deaths on day 3. Strain DD503 performed differently, yielding 0 deaths on days 1 through 3 and 5 deaths on day 4. Neither of these counts reflects the number of animals sacrificed. Interestingly, both B. pseudomallei 1026b and DD503 proliferated with similar loads and kinetics in all the tissues examined, yet DD503 exhibited reduced overall virulence (Fig. 1 and Table 2). The difference in virulence appeared to manifest itself as a difference in the time to death. In this experiment, the difference in virulence observed was not likely attributable to the twofold difference in delivered dose alone. Twofold differences in delivered doses were frequently observed during our analysis. In four separate experiments where nearly identical doses were delivered, including the two LD50 determinations, DD503 repeatedly killed more slowly and required more CFU to kill than 1026b (Table 2 and data not shown).
FIG. 1.
Mouse high-dose aerosol exposure serial sacrifice. The bar chart depicts the average numbers of CFU per milliliter (per gram) recoverable from four BALB/c mouse organs at 24-h intervals after aerosol exposure to either the wild-type B. pseudomallei strain 1026b or the multidrug efflux pump mutant DD503. At each time interval, five mice were humanely euthanized. Various organs from four of the mice were harvested, weighed, and homogenized in 5 ml of Hank’s balanced salt solution. The recoverable number of CFU per milliliter for each organ homogenate was determined by serial dilution and plating. The CFU values were then adjusted based upon the weight of the homogenized organ. Totals for days 1, 2, and 3 are indicated. The day 3 data for 1026b are not averages but instead are the data from the sole surviving mouse. The exposure doses were calculated to be 4,500 CFU inhaled for 1026b and 2,400 CFU inhaled for DD503. Error bars represent the standard deviations of the four samples per data point.
Given the high death rate after the high-dose challenge experiment, we repeated the preceding experiment with modified parameters. We lowered the inhaled dose of strain 1026b, selected a time point on the day of exposure, and isolated blood at every time point to analyze the rate of sepsis. The results of this challenge experiment are depicted in Fig. 2. The lower-exposure dose allowed the animals to survive until day 4, making our later time point data more representative. The calculated inhaled dose of strain 1026b was 260 CFU (∼50 LD50s). The death-by-day data were as follows: 0 animals died on days 1 to 3, and 4 of the remaining 5 animals died on day 4. The data for day 4 shown in Fig. 3 are based upon the sole survivor. Two hundred sixty CFU of DD503 delivered in parallel to two groups of animals killed only 1 of 20 animals by day 5. The experiment was terminated at day 21 by humane euthanasia; no additional deaths were observed during the 3-week period (data not shown). The tissue proliferation data in Fig. 2 were similar to the data for the higher-dose challenge. Curiously, the bacteria were trafficked to the spleen and liver very quickly (within 6 h). The hepatic and spleenic tropisms that we observed matched those in previous reports of clinical disease (5). The organ most heavily infected by both low-dose and high-dose exposures was the lungs (Fig. 1 and 2). The tissue proliferation of DD503 was not examined for the low-dose exposure.
FIG. 2.
Mouse low-dose aerosol exposure serial sacrifice.The bar chart depicts the average numbers of CFU per milliliter (per gram) recoverable from four BALB/c mouse organs obtained after 6, 24, 48, 72, and 96 h of aerosol exposure to wild-type B. pseudomallei 1026b. At each time interval, five mice were humanely euthanized. Various organs from four of the mice were harvested, weighed, and homogenized in 5 ml of Hank’s balanced salt solution. The number of recoverable CFU per milliliter for each organ homogenate was determined by serial dilution and plating. The CFU values were then adjusted based upon the weight of the homogenized organ. The white bars represent data for the 6-h time point, and the black bars represent data for the 96-h time point. The calculated exposure dose was 250 CFU. Error bars represent the standard deviations for the four samples per data point.
FIG. 3.
Effect of deletion of efflux genes or rpsL mutations on B. pseudomallei virulence. Antibiotic-supplemented Luria broth overnight cultures of B. pseudomallei 1026b, RM102, RM102SmR, and DD503 were diluted into Luria broth and then nebulized. Ten BALB/c animals per group were exposed for 10 min to the aerosol. The calculated inhaled doses were 196 CFU for 1026b, 96 CFU for RM102, 118 CFU for RM102 SmR, and 89 CFU for DD503. Deaths from disease in each group were recorded for 50 days. The data for days 0 through 21 are shown. At day 50, survivors were humanely euthanized and their spleens were harvested for bacterial load determination. The sole surviving mouse from the RM102 SmR experiment had >104 CFU/ml (or g) of spleen tissue. Five of the eight surviving DD503-infected mice had similar spleen loads. Three DD503-infected mice had sterile spleens, which apparently indicated that the animals were resolving their infections.
Wild-type B. mallei is sensitive to both aminoglycoside and macrolide antibiotics (9), and its genome lacks the amrRAB oprA-encoded multidrug efflux pump (The Institute for Genomic Research). We wondered if the difference in virulence exhibited by B. pseudomallei relative to that of B. mallei (Table 2) could be explained by the loss of the multidrug efflux pump. To discriminate between the multidrug efflux pump's effect upon pneumonic virulence and that of the rpsL mutation also present in DD503, we obtained the allelic series generated by Moore et al. (12) and then we exposed mice to a low-dose aerosol of each mutant and its 1026b isogenic parent. Strain RM102 is an aminoglycoside-sensitive 1026b mutant, by virtue of a Tn5 insertion into the amrB gene. RM102 SmR is a streptomycin-resistant spontaneous mutant derived from RM102. If loss of the multidrug efflux pump attenuates the virulence of DD503, then we would expect RM102 to be as attenuated as DD503. If, however, the rpsL mutation in each background attenuates the strain, then RM102 SmR should be similar in virulence to DD503. The results are depicted in Fig. 3.
The multidrug efflux pump played almost no role in pneumonic disease; rather, the rpsL mutation present in DD503 must have been largely responsible for its attenuation (Fig. 3). Mutations in rpsL have attenuated another gram-negative pathogen by enforcing an increase in translational fidelity (3). The i.p. hamster model must not place the same selective criteria upon the bacteria as the aerosol mouse model because, in hamsters, the LD50 of strain DD503 is indistinguishable from that of strain 1026b (a difference in LD50s of <10 by i.p. administration) (12). The different outcome reported may be due to many differences between the experiments. Simple explanations involve differences in the types of host (i.e., hamsters versus mice) or differences in the methods of administration to the tissues (i.e., i.p. versus nebulization). Alternatively, the differences in results may be attributable to differences in the targeted tissues themselves (i.e., peritoneal cavity versus lung epithelium). Because our goal was satisfied by establishing a pneumonic disease model and by characterizing the performance of available molecular genetic tools within the model, we decided against further exploration of the attenuated virulence displayed by rpsL mutants.
The important findings of this work are both that mice are sensitive to aerosols containing B. pseudomallei and that the mouse genetic background played a small role in host protection from inhaled B. pseudomallei, contrary to the results in a previous report (11). Further, our work suggests that, in future mutational analyses and vaccine studies, it is important to consider the rpsL genotype and the use of streptomycin-mediated gene replacement in B. pseudomallei and B. mallei.
Acknowledgments
We gratefully acknowledge the work of an extraordinary technical staff including A. L. O'Quinn, M. England, A. Bassett, and M. West. D. DeShazer, E. Wargo, M. L. Dautle, and D. E. Woods provided critical comments. R. Moore and D. E. Woods graciously provided both strains and insight. We thank T. P. Atikins for 2 weeks of hot lab work. Statistical analyses for LD50 determinations were provided by P. Gibbs.
This work was supported by funds from the U.S. Army Medical Research and Materiel Command (projects 02-4-5x-027 and 02-4-5x-030).
Editor: D. L. Burns
REFERENCES
- 1.Alibek, K., and S. Handelman. 1999. Biohazard: the chilling true story of the largest covert biological weapons program in the world, 1st ed. Random House, New York, N.Y.
- 2.Barnes, J. L., G. C. Ulett, N. Ketheesan, T. Clair, P. M. Summers, and R. G. Hirst. 2001. Induction of multiple chemokine and colony-stimulating factor genes in experimental Burkholderia pseudomallei infection. Immunol. Cell Biol. 79:490-501. [DOI] [PubMed] [Google Scholar]
- 3.Bjorkman, J., P. Samuelsson, D. I. Andersson, and D. Hughes. 1999. Novel ribosomal mutations affecting translational accuracy, antibiotic resistance and virulence of Salmonella typhimurium. Mol. Microbiol. 31:53-58. [DOI] [PubMed] [Google Scholar]
- 4.Bray, M. P., M. J. Martinez, D. Kefauver, M. West, and C. Roy. 2002. Treatment of aerosolized cowpox virus infection in mice with aerosolized cidofovir. Antivir. Res. 54:129-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dance, D. A. B. 1999. Melioidosis, p. 430-437. In R. L. Geurrant, D. H. Walker, and P. F. Weller (ed.), Tropical infectious diseases: principles, pathogens and practice, 1st ed., vol. 1. Churchill Livingstone, Philadelphia, Pa. [Google Scholar]
- 6.DeShazer, D., P. J. Brett, R. Carlyon, and D. E. Woods. 1997. Mutagenesis of Burkholderia pseudomallei with Tn5-OT182: isolation of motility mutants and molecular characterization of the flagellin structural gene. J. Bacteriol. 179:2116-2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fritz, D. L., P. A. Vogel, D. R. Brown, and D. M. Waag. 1999. The hamster model of intraperitoneal Burkholderia mallei. Vet. Pathol. 36:276-291. [DOI] [PubMed] [Google Scholar]
- 8.Guyton, A. C. 1947. Measurement of the respiratory minute volume of laboratory animals. Am. J. Physiol. 150:70-77. [DOI] [PubMed] [Google Scholar]
- 9.Heine, H. S., M. J. England, D. M. Waag, and W. R. Byrne. 2001. In vitro antibiotic susceptibilities of Burkholderia mallei (causative agent of glanders) determined by broth microdilution and E-test. Antimicrob. Agents Chemother. 45:2119-2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoppe, I., B. Brenneke, M. Rohde, A. Kreft, S. Häuβler, A. Reganzerowski, and I. Steinmetz. 1999. Characterization of a murine model of melioidosis: comparison of different strains of mice. Infect. Immun. 67:2891-2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu, B., G. C. Koo, E. H. Yap, K. L. Chua, and Y.-H. Gan. 2002. Model of differential susceptibility to mucosal Burkholderia pseudomallei infection. Infect. Immun. 70:504-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore, R. A., D. DeShazer, S. Reckseidler, A. Weissman, and D. E. Woods. 1999. Efflux-mediated aminoglycoside and macrolide resistance in Burkholderia pseudomallei. Antimicrob. Agents Chemother. 43:465-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nigg, C., J. Ruch, E. Scott, and K. Noble. 1956. Enhancement of virulence of Malleomyces pseudomallei. J. Bacteriol. 71:530-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 15.Santanirand, P., V. S. Harley, D. A. B. Dance, B. S. Drasar, and G. J. Bancroft. 1999. Obligatory role of gamma interferon for host survival in a murine model of infection with Burkholderia pseudomallei. Infect. Immun. 67:3593-3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Waag, D. M., M. J. England, and M. L. Pitt. 1997. Comparative efficacy of a Coxiella burnetii chloroform methanol residue (CMR) vaccine and a licensed cellular vaccine (Q-Vax) in rodents challenged by aerosol. Vaccine 15:1779-1783. [DOI] [PubMed] [Google Scholar]
- 17.Woods, D. E., D. DeShazer, R. A. Moore, P. J. Brett, M. N. Burtnick, S. L. Reckseidler, and M. D. Senkiw. 1999. Current studies on the pathogenesis of melioidosis. Microbes Infect. 1:157-162. [DOI] [PubMed] [Google Scholar]
- 18.Yabuuchi, E., Y. Kosako, H. Oyaizu, I. Yano, T. Ezaki, and M. Arakawa. 1992. Proposal of Burkholderia gen nov. and transfer of seven species of the genus Pseudomonas homology group II to the new genus, with the type species Burkholderia cepacia (Palleroni and Holmes 1981) comb. nov. Microbiol. Immunol. 36:1251-1275. [DOI] [PubMed] [Google Scholar]