Abstract
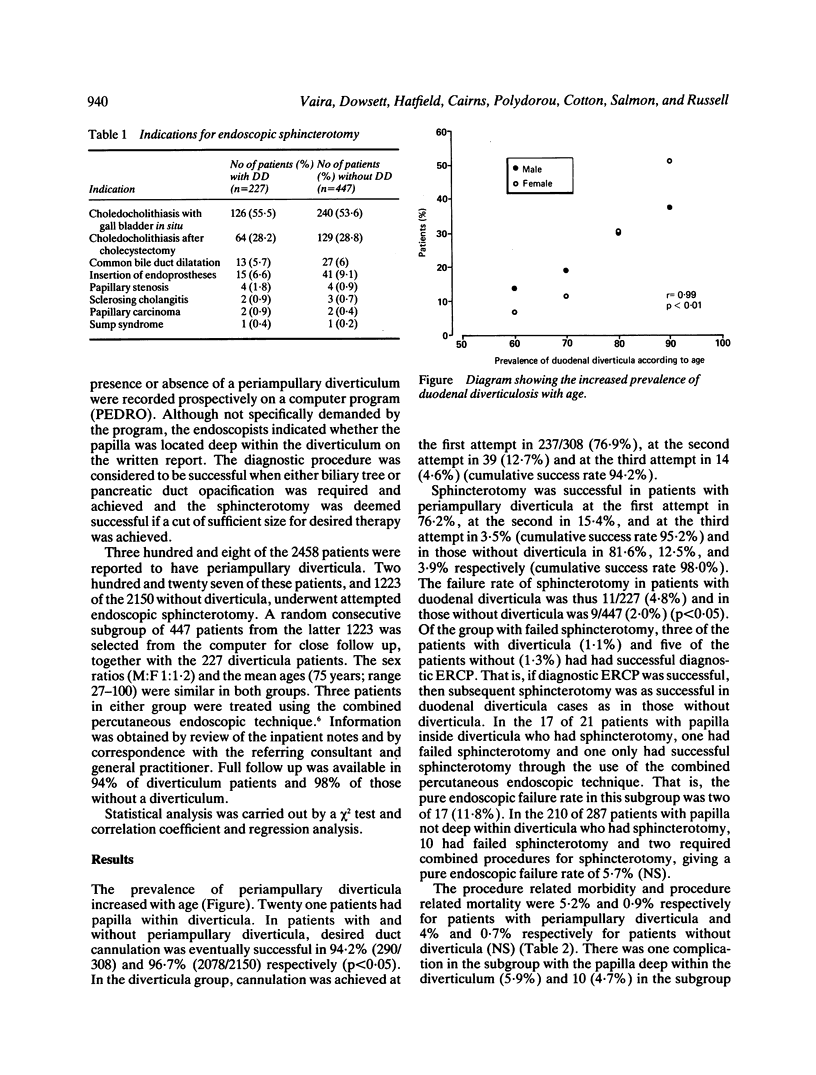
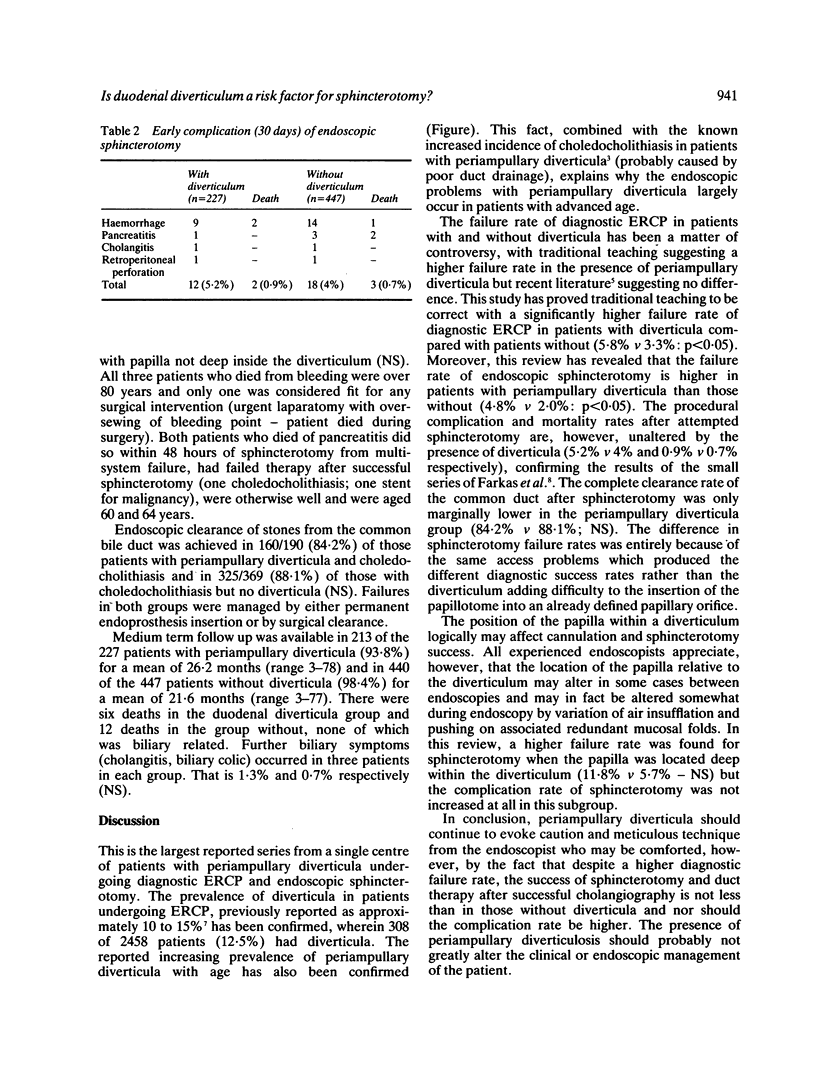
It is uncertain whether ERCP and associated procedures are more difficult when the papilla is inside or adjacent to a duodenal diverticulum. We have therefore reviewed the data from 2458 consecutive, prospectively reported ERCPs between November 1983 and March 1988. Three hundred and eight patients (12.5%) had periampullary diverticula and in 21 the papilla was located deep within the diverticulum of whom 227 had undergone endoscopic sphincterotomy (73.7%). Comparison was made with the 2150 patients without diverticula of whom 1223 (56.9%) had undergone sphincterotomy. The success rate of specific duct cannulation was 94.2% in the diverticulum group and 96.7% in those without diverticula (p less than 0.05). The overall success rate of endoscopic sphincterotomy was 95.2% in the diverticulum group, as compared with 98.0% in those without diverticula (p less than 0.05). The procedure related morbidity and mortality of sphincterotomy were 5.2%/0.9% and 4.0%/0.7% respectively (NS). If only those who had successful cholangiography were included there was no difference in sphincterotomy success between those with and without diverticula. The group of patients with papilla deep within diverticula had a slightly higher failure rate of pure endoscopic sphincterotomy (11.8% v 5.7%: NS) but did not have a higher complication rate. In the subgroup of patients with choledocholithiasis, duct clearance of stones was as successful after sphincterotomy in those with diverticula as in those without. Medium term complications (mean 26 months) occurred in 1.4% of patients with diverticula and in 0.7% of patients without diverticula. We conclude that diagnostic cholangiography is more difficult when the papilla is closely associated with a diverticulum but that if diagnostic cholangiography is obtained, sphincterotomy may be performed as successfully and as safely in those with or without diverticula.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chang-Chien C. S. Do juxtapapillary diverticula of the duodenum interfere with cannulation at endoscopic retrograde cholangiopancreatography? A prospective study. Gastrointest Endosc. 1987 Aug;33(4):298–300. doi: 10.1016/s0016-5107(87)71602-2. [DOI] [PubMed] [Google Scholar]
- Cotton P. B. Endoscopic management of bile duct stones; (apples and oranges). Gut. 1984 Jun;25(6):587–597. doi: 10.1136/gut.25.6.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowsett J. F., Vaira D., Hatfield A. R., Cairns S. R., Polydorou A., Frost R., Croker J., Cotton P. B., Russell R. C., Mason R. R. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology. 1989 Apr;96(4):1180–1186. doi: 10.1016/0016-5085(89)91639-9. [DOI] [PubMed] [Google Scholar]
- Kirk A. P., Summerfield J. A. Incidence and significance of juxtapapillary diverticula at endoscopic retrograde cholangiopancreatography. Digestion. 1980;20(1):31–35. doi: 10.1159/000198411. [DOI] [PubMed] [Google Scholar]
- Lintott D. J., Ruddell W. S., Axon A. T. Pseudostone at ERCP due to juxtapapillary diverticulum. Clin Radiol. 1981 Mar;32(2):173–176. doi: 10.1016/s0009-9260(81)80154-7. [DOI] [PubMed] [Google Scholar]


