Abstract
Research Objectives
To describe the use of post-acute home care (PAHC) and total Medicaid expenditures among hospitalized nonelderly adult Medicaid eligibles and to test whether health services utilization rates or total Medicaid expenditures were lower among Medicaid eligibles who used PAHC compared to those who did not.
Study Population
5,299 Medicaid patients aged 18–64 discharged in 1992–1996 from 29 hospitals in the Cleveland Health Quality Choice (CHQC) project.
Data Sources
Linked Ohio Medicaid claims and CHQC medical record abstract data.
Data Extraction
One stay per patient was randomly selected.
Design
Observational study. To control for treatment selection bias, we developed a model predicting the probability (propensity) a patient would be referred to PAHC, as a proxy for the patient's need for PAHC. We matched 430 patients who used Medicaid-covered PAHC (“USE”) to patients who did not (“NO USE”) by their propensity scores. Study outcomes were inpatient re-admission rates and days of stay (DOS), nursing home admission rates and DOS, and mean total Medicaid expenditures 90 and 180 days after discharge.
Principal Findings
Of 3,788 medical patients, 12.1 percent were referred to PAHC; 64 percent of those referred used PAHC. Of 1,511 surgical patients, 10.9 percent were referred; 99 percent of those referred used PAHC. In 430 pairs of patients matched by propensity score, mean total Medicaid expenditures within 90 days after discharge were $7,649 in the USE group and $5,761 in the NO USE group. Total Medicaid expenditures were significantly higher in the USE group compared to the NO USE group for medical patients after 180 days (p<.05) and surgical patients after 90 and 180 days (p<.001). There were no significant differences for any other outcome. Sensitivity analysis indicates the results may be influenced by unmeasured variables, most likely functional status and/or care-giver support.
Conclusions
Thirty-six percent of the medical patients referred to PAHC did not receive Medicaid-covered services. This suggests potential underuse among medical patients. The high post-discharge expenditures suggest opportunities for reducing costs through coordinating utilization or diverting it to lower-cost settings. Controlling for patients' need for services, PAHC utilization was not associated with lower utilization rates or lower total Medicaid expenditures. Medicaid programs are advised to proceed cautiously before expanding PAHC utilization and to monitor its use carefully. Further study, incorporating non-economic outcomes and additional factors influencing PAHC use, is warranted.
Keywords: Medicaid, home care; post-acute care; outcomes; cost of care; propensity score
Objectives
We report here on a study of the use of home care following hospital discharge by nonelderly adult Medicaid eligibles in the Greater Cleveland area. The study was prompted by the fact that post-acute home care (PAHC) use increased by 60 percent in the area from 1992 through 1996, raising questions about whether services were appropriately targeted and cost-effective. The study had two objectives: (1) To describe use of post-acute home care (PAHC) and total Medicaid expenditures among hospitalized nonelderly adult Medicaid eligibles, and (2) To test whether use of PAHC was associated with lower health services utilization rates and/or lower total Medicaid expenditures, controlling for factors related to the need for PAHC.
The study is one of a series of evaluations of Medicaid expenditures and outcomes commissioned by the Ohio Department of Human Services (ODHS) as part of a concerted effort to become a value purchaser of health care services. It uses data from hospitals participating in the Cleveland Health Quality Choice (CHQC) hospital report card project (Rosenthal and Harper 1994; Rosenthal et al. 1998). By taking advantage of clinical, treatment, and health status data abstracted from medical records for the CHQC project, we could make finer distinctions in patients' severity of illness on admission than are possible in studies limited to administrative data in hospital discharge data bases (Iezzoni 1997).
Background
Home care can be provided on a short-term basis for the post-acute convalescence of recently discharged hospital patients or on a longer-term basis for maintenance in the home of clients who need sub-acute health care or social support services (Welch, Wennberg, and Welch 1996). Traditionally, Medicare has been the major source of coverage for short-term post-acute care for disabled and elderly individuals and Medicaid has been the source for long-term care for disabled and low-income individuals, although this distinction has blurred due to greater use of long-term home care by Medicare beneficiaries (Welch, Wennberg, and Welch 1996).
From 1991 to 1998, U.S. expenditures for home care increased by 82 percent, compared to a 50 percent increase in expenditures for all personal health care services (Health Care Financing Administration 2000a). Expenditures by Medicaid for home care increased even more sharply—by 100 percent (Health Care Financing Administration 2000a). Medicaid now pays 17 cents of every dollar spent on home care in the United States (Health Care Financing Administration 2000a).
The dramatic increase in Medicaid home care expenditures is due in part to the same factors affecting total U.S. home care expenditures—an aging population, a changing family structure and labor force composition, the increased prevalence of chronic conditions as survival rates improve, a broader range of services and technologies provided in the home, and, perhaps, the growth of financial and organizational ties between hospitals and home care providers (Kramer, Shaughnessy, and Pettigrew 1985; Kenney 1991; Wiener and Hanley 1992; Blewett, Kane, and Finch 1995–1996; Dansky, Milliron, and Gamm 1996; National Association for Home Care 2000). Medicaid home care expenditures were also influenced by programs specifically designed to shift utilization to home- and community-based services and away from institutional care (Dobson, Moran, and Young 1992; Riley 1995; Leutz 1999; Health Care Financing Administration 2000b).
Data and methods
Study Population
We studied Medicaid patients aged 18–64 years old who had been admitted for one of the six medical conditions (acute myocardial infarction [AMI], congestive heart failure [CHF], gastrointestinal [GI] hemorrhage, chronic obstructive pulmonary disease [COPD], pneumonia, or stroke) or seven surgical procedures (coronary artery bypass graft [CABG], hysterectomy, laminectomy, lower bowel resection, prostatectomy, hip replacement, or vascular surgery) and who were discharged from the 29 hospitals participating in the Cleveland Health Quality Choice (CHQC) project during state fiscal years 1992 through 1996.
The CHQC project, a joint collaboration among hospitals, physicians, and employers, was implemented in November 1989. Its primary objectives were to provide valid, case-mix-adjusted outcome data for use by employers in selective contracting and by hospitals for internal quality improvement initiatives and to provide incentives for hospitals to improve competitive position and market share by improving quality (Rosenthal and Harper 1994; Rosenthal et al. 1998). Mortality and length-of-stay outcomes were adjusted for admission severity of illness using a measurement system (CHOICE) and risk adjustment models developed and validated by the CHQC project. Expert medical and surgical physician advisory panels recommended variables for use in risk-adjustment. Separate severity adjustment models were developed by consultants and project staff for cesarean section rates (not reported here) and the six medical diagnoses and seven surgical procedures used in this study. Preliminary diagnosis-specific risk-adjustment models based on data from the first collection period (January–June 1991) were developed. Stepwise logistic regression was used to predict in-hospital mortality for medical stays; stepwise linear regression was used to predict length of stay for surgical stays. The models were validated by physician panels and by empirical analyses. Subsequently, after each interval of data collection, models were refined and evaluated. Performance of the mortality and length of stay models are comparable to other diagnosis-specific reported methods: ROC curve areas for the mortality model, by diagnosis, range from .80 to .91 and the variance explained (R2) by the length of stay models ranges from .159 to .367. (Rosenthal et al. 1998; Rosenthal, personal communication). Abstractors trained for the project retrospectively reviewed patients' medical records in each study hospital. They collected information on nearly 250 sociodemographic and clinical variables, including diagnoses, procedures, cognitive and motor function, results of examinations and tests, admission and discharge dates, and discharge destination.
In this study we included stays of patients for whom Medicaid was the first-listed payer and who were either discharged to home with a referral to PAHC or to home with no referral to PAHC. We excluded those dually eligible for Medicaid and Medicare because we did not have access to information on services covered by Medicare. Dual eligibles were excluded by age (65 years of age and older) and by payer (i.e., Medicare is the first-listed payer for dual eligibles). We also excluded patients who died in-hospital, left against medical advice, were transferred to another acute-care hospital or to a skilled nursing facility, or who had an unknown discharge destination. Because of the inclusion and exclusion criteria, the study population is comprised of nonelderly adults qualifying for Medicaid due to disability or low-income. In the United States, low-income nonelderly adults and low-income disabled individuals were 20.2 percent and 18.3 percent, respectively, of the persons served by Medicaid in 1997 (Health Care Financing Administration 2000c). They accounted for 10.0 percent and 43.8 percent, respectively, of total U.S. Medicaid payments in 1997 (Health Care Financing Administration 2000c).
Data Used
We used CHQC medical record abstract data, including hospital identification number, diagnoses, procedures performed, results of examinations and diagnostic tests, admission and discharge dates, discharge destination, and either probability of death or expected length of stay (used as proxies for severity of illness of patients with medical or surgical stays, respectively). Level of orientation (oriented, some disorientation, unknown) and level of consciousness (conscious, some unconsciousness, unknown) were used to account for mental functioning. Decreased motor function (no, yes, unknown) was used to account for physical functioning. We used claims data for all Medicaid-covered health services used by the study population, including type of service (inpatient, outpatient, physician, nursing home, home health, prescription drugs, and other), date(s) of service, and amount reimbursed by Medicaid.
Data Extraction Methods
Record Linking Process
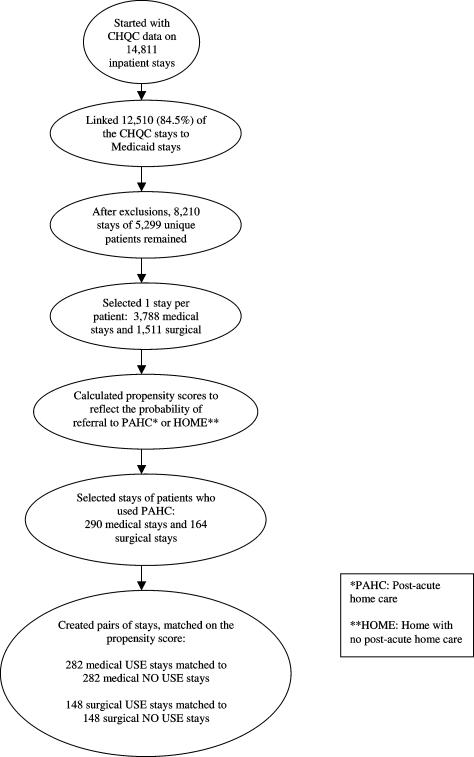
We linked data on hospital stays in the CHQC and Medicaid files. To make the linkage we used the hospital identifier, patient age, patient gender, and at least one of the following variables—principal diagnosis, admission date, or discharge date (Figure 1). (We did not have access to names in the CHQC file.)
Figure 1.
Overview of the Study Design
A large proportion of the patients had more than one CHQC stay during the study period. Because of this, we could not make the assumption of independence required by standard statistical techniques. To avoid the use of complex statistical techniques to account for non-independent observations, which would complicate the sampling methods and the interpretation of the results, we randomly selected one stay per patient, called the “index stay,” and used the resulting sample, called the “analytic cohort,” in the study.
Use of PAHC
Use of PAHC was defined as having a Medicaid claim for home care with a start date within three days or less of the discharge date of the index stay. Patients who used PAHC following the index stay were classified as users of PAHC; the remaining patients were classified as nonusers.
Study Outcomes
We included all Medicaid claims for health services initiated within 180 days after the discharge date of the index stay. Any claim for inpatient service (excluding the index stay), any claim for nursing home service, the number of inpatient days of stay (excluding the index stay), and the number of nursing home days of stay were used to measure health services utilization. The sum of reimbursements for all health services covered by Medicaid was used to measure total Medicaid expenditures. Reimbursements were inflated to 1996 dollars using the medical services consumer price index (Bureau of Labor Statistics 1998).
Study Design
Objective 1
To describe the use of post-acute home care (PAHC) and total Medicaid expenditures among hospitalized nonelderly adult Medicaid eligibles. Using data on the analytic cohort, we calculated rates of referral to PAHC and compared utilization rates and total Medicaid expenditures of patients who used PAHC following the index stay to patients who did not.1 We used two follow-up periods: within 90 days and within 180 days after the index stay discharge date.
Objective 2
To test whether use of PAHC was associated with lower health services utilization rates and/or lower total Medicaid expenditures. For matched pairs of PAHC users and nonusers, we compared the study outcomes, controlling for characteristics of the patients related to their need for PAHC through the propensity score (described below). We first tested the following hypotheses:
Ninety-day hospital re-admission rates were lower for those who used PAHC compared to those who did not, controlling for factors related to referral to PAHC.
One-hundred-eighty-day hospital re-admission rates were lower for those who used PAHC compared to those who did not, controlling for factors related to referral to PAHC.
We then tested the hypotheses for each measure of health services utilization and for total Medicaid expenditures.
Analysis
Descriptive Statistics
We used descriptive statistics (frequencies for categorical variables and mean percentile values [25th, 50th, and 75th] for continuous variables) to describe the study population in terms of patient and stay characteristics and study outcomes.
Propensity Scores
Administrative claims data bases have several advantages for health services research. In addition to including large numbers of observations, they include the full spectrum of practice patterns and are relatively inexpensive to access and use (Rubin 1997). However, the patients have not been randomly assigned to treatment. For example, the decision to refer patients to home care can be influenced by the patient's severity of illness and functional status, the availability of informal supports, and physician and hospital referral patterns. “In observational studies, investigators have no control over the treatment assignment. The treated and nontreated (i.e., control) groups may have large differences on their observed covariates, and these differences can lead to biased estimates of treatment effects” (D'Agostino 1998). For example, severity of illness or functional status may influence the outcomes of post-acute services.
The propensity score was developed to overcome several limitations of observational data (Miettinen 1976; Rosenbaum and Rubin 1983a; 1984; Rosenbaum 1991; Connors, et al. 1996). The propensity score is defined as the “conditional probability of being treated given the covariates” (D'Agostino 1998). Matching or stratifying on the propensity score tends to balance the observed covariates ( Joffe and Rosenbaum 1999). “In effect, this technique enables us to assess the association of [the treatment] with specific outcomes in patients with an equal probability of receiving the treatment” (Connors, et al. 1996).
Propensity scores have been used in studies of ambulatory care (Stone et al. 1995; Legoretta et al. 2000), prescription drugs (Smith et al. 1998; Tai-Seale et al. 2000), right-heart catheterization (Connors et al. 1996), and social programs (Heckman et al. 1996). Evaluations of the method indicate that it is more reliable than standard methods of adjusting for covariates such as linear or logistic regression because the assumptions made are “more assessable and transparent to the investigator” (Rubin 1997) and that it eliminates some but not all selection bias (Stone et al. 1995; Heckman et al. 1996). Without knowledge of the probability of exposure to treatment, the validity of the method can only be estimated (Drake and Fisher 1995).
We used propensity scores to adjust for the characteristics of the patients related to referral to PAHC, to allow us to control for treatment selection bias and discern whether differences in study outcomes were due to differences among the patients or to the use of PAHC. We used referral to home care as a proxy for the patient's need for home care.2 To develop models for calculating propensity scores, we convened an expert panel consisting of four general internists, a family practitioner, a specialist in rehabilitative medicine, two research methodologists, and a medical sociologist. The panel identified factors related to the decision to refer a patient to PAHC and suggested how to specify several variables. For example, they suggested that we indicate separately whether a person had one of four diagnoses that would influence the decision to refer a patient to PAHC—asthma, cancer, stroke, or diabetes. We created an “Other Medical Conditions Index” by counting the remaining diagnoses noted on the CHQC data collection form and used that number in the model.
To achieve maximum predictive power with the model, we retained all the independent variables used in the multivariable logistic regression model, regardless of their statistical significance. Discharge destination—referral to home with PAHC or to home without PAHC—was the dependent variable. Separate models were developed for medical and surgical stays.
We evaluated the predictive performance of the models using the area under the receiver operating characteristic (ROC) curve, a measure of the performance of diagnostic tests or predictive models in predicting dichotomous outcomes (Hanley and McNeil 1983; Ash and Shwartz 1997). The ROC curve is generated by comparing the predicted outcomes using the test or model to actual outcomes and plotting sensitivity against (1 − specificity). Pairs of subjects are formed, one of which has the outcome and the other does not (e.g., one subject is referred to home care and the other is not). The test or model is tested for all possible pairs of subjects. The c statistic is a summary measure of the ROC curve; a value of .50 indicates prediction no better than chance and a value of 1.00 indicates perfect rank order prediction (Ash and Shwartz 1997). In the language of the diagnostic test, the c statistic can be interpreted as “the probability that a randomly chosen diseased subject is (correctly) rated or ranked with greater suspicion than a randomly chosen non-diseased subject” (Hanley and McNeil 1983). In this study, the c statistic can be interpreted as the probability that a randomly chosen stay of a patient who was referred to home care was ranked by the model as being more likely to be referred to home care than a randomly chosen stay of a patient who was not referred to home care.
All analyses were generated using SAS software (version Connors, et al. 1996).
To evaluate whether the matching process resulted in pairs of stays that were similar to each other, we compared the values of the matched stays on the covariates used in the logistic regression model to calculate the propensity score. Similar values of the observed covariates for the stays referred to PAHC compared to the stays not referred would be evidence that the matching process successfully paired similar stays.
Hypothesis Testing
We reviewed whether the two groups of stays (USE and NO USE) were statistically significantly different from each other on the covariates in the matched data using the Wilcoxon matched-pairs signed-rank test for continuous and ordinal variables and the McNemar test for categorical variables. Finally, we performed a sensitivity analysis to estimate the impact of unmeasured variables on the results. We determined how substantial the effect of an unobserved covariate would have to be to mask a beneficial effect of PAHC (Connors et al. 1996; Rosenbaum 1991; Rosenbaum and Rubin 1983b).
Principal Findings
Study Population
We obtained information from CHQC on 14,811 inpatient stays that occurred from SFY 1992 through SFY 1996 (Figure 1). We were able to link 84.5 percent (12,510) of the CHQC stays to stays in the Medicaid claims file.3 The link rate increased from 75.1 percent in 1992 to 88.0 percent in 1996. We excluded 2,301 stays which did not link; 499 stays which had missing or inconsistent information; and 3,801 stays because the discharge destination was other than to home or to PAHC, the patient was aged 65 years or older, or the discharge date was January 1, 1996, or later, which allowed insufficient time for follow up. This left 8,210 records, representing stays of 5,299 unique patients, available for study.
Medical patients had an average of 1.7 stays each (6,573/3,788) and surgical patients had an average of 1.1 stays each (1,637/1,511). We randomly selected one stay from each of the 3,788 medical and 1,511 surgical patients for further analysis.
Descriptive information on the analytic cohort supports many of the recommendations from the expert panel as to variable specification (Table 1). For example, the percent of patients referred to PAHC increases gradually as age, length of the index stay, Medical Conditions Index count, and predicted probability of death increase.
Table 1.
Patient and Stay Characteristics, Medicaid Index Stays, CHQC Hospitals, 1992–1996 (n=5,299)
| Medical Stays (n=3,788) | Surgical Stays (n=1,511) | |||
|---|---|---|---|---|
| Characteristics | Column % | Referred to PAHC (row %) | Column % | Referred to PAHC (row %) |
| Fiscal Year of Discharge | ||||
| 1992 | 10.5 | 7.8 | 9.9 | 8.7 |
| 1993 | 22.6 | 12.1 | 25.6 | 11.4 |
| 1994 | 25.7 | 12.0 | 26.4 | 8.5 |
| 1995 | 27.5 | 13.3 | 26.4 | 12.0 |
| 1996 | 13.7 | 12.9 | 11.7 | 14.2 |
| All Stays | 100.0 | 12.1 | 100.0 | 10.9 |
| Study Condition | ||||
| Acute Myocardial Infarction (AMI) | 4.1 | 10.4 | ||
| Congestive Heart Failure (CHF) | 19.5 | 21.3 | ||
| Gastrointestinal (GI) Hemorrhage | 9.0 | 6.2 | ||
| Chronic Obstructive Pulmonary Disease (COPD) | 37.6 | 7.5 | ||
| Pneumonia | 24.8 | 12.5 | ||
| Stroke | 5.1 | 20.2 | ||
| Coronary Artery Bypass Graft (CABG) | 9.3 | 22.9 | ||
| Hysterectomy | 42.9 | 2.9 | ||
| Laminectomy | 14.9 | 4.9 | ||
| Lower Bowel Resection | 7.0 | 28.3 | ||
| Prostatectomy | 2.7 | 12.5 | ||
| Hip Replacement | 17.9 | 15.9 | ||
| Vascular Surgery | 5.4 | 29.6 | ||
| Age | ||||
| 18–19 | 2.2 | 1.2 | 1.1 | 6.3 |
| 20–24 | 7.3 | 4.7 | 5.0 | 9.3 |
| 25–29 | 7.2 | 4.8 | 8.3 | 4.0 |
| 30–34 | 9.6 | 6.4 | 15.6 | 5.1 |
| 35–39 | 11.6 | 6.4 | 19.5 | 7.8 |
| 40–44 | 11.0 | 10.8 | 13.1 | 5.1 |
| 45–49 | 11.0 | 11.7 | 10.7 | 13.0 |
| 50–54 | 11.7 | 15.4 | 8.1 | 18.0 |
| 55–59 | 12.7 | 16.4 | 8.3 | 19.8 |
| 60–64 | 15.8 | 23.1 | 10.3 | 24.4 |
| Gender | ||||
| Female (0) | 71.4 | 11.5 | 77.4 | 9.8 |
| Male (1) | 28.6 | 13.4 | 22.6 | 14.6 |
| Race | ||||
| White | 39.0 | 11.8 | 49.2 | 9.0 |
| Black | 57.5 | 12.5 | 47.1 | 13.2 |
| Other | 2.9 | 7.4 | 2.5 | 8.1 |
| Unknown | 0.6 | 4.2 | 1.3 | 0.0 |
| Hospital Length of Stay in Days | ||||
| 1–2 | 7.5 | 2.8 | 6.9 | 1.9 |
| 3–4 | 33.2 | 5.9 | 33.2 | 3.2 |
| 5–6 | 27.9 | 8.1 | 26.7 | 6.7 |
| 7–8 | 13.3 | 14.5 | 11.9 | 15.6 |
| 9–10 | 7.9 | 25.3 | 7.1 | 18.7 |
| 11–12 | 3.8 | 25.9 | 4.4 | 28.4 |
| 13–14 | 2.3 | 36.1 | 3.5 | 30.2 |
| 15–16 | 1.2 | 38.3 | 1.7 | 28.0 |
| 17–18 | 0.9 | 42.9 | 1.3 | 45.0 |
| 19–20 | 0.4 | 71.4 | 1.0 | 20.0 |
| 21–22 | 0.4 | 35.7 | 0.3 | 20.0 |
| 23–24 | 0.3 | 27.3 | 0.5 | 37.5 |
| 25–26 | 0.1 | 66.7 | 0.3 | 75.0 |
| 27+ | 0.9 | 57.6 | 1.3 | 52.6 |
| Admission Source | ||||
| Home | 98.4 | 12.1 | 97.8 | 10.6 |
| Nursing Home | 0.5 | 22.2 | 0.1 | 0.0 |
| Hospital | 0.0 | --- | 1.3 | 31.6 |
| Other | 1.2 | 4.6 | 0.8 | 8.3 |
| Admission from ER | ||||
| No (0) | 15.4 | 13.5 | 80.1 | 7.8 |
| Yes (1) | 84.6 | 11.8 | 19.9 | 23.3 |
| Asthma/COPD | ||||
| No (0) | 52.5 | 14.2 | 89.3 | 11.1 |
| Yes (1) | 47.5 | 9.7 | 10.7 | 8.6 |
| Cancer | ||||
| No (0) | 98.1 | 11.5 | 98.9 | 10.6 |
| Yes (1) | 1.9 | 39.4 | 1.1 | 35.3 |
| Stroke/CVA | ||||
| No (0) | 93.5 | 11.2 | 96.6 | 10.3 |
| Yes (1) | 6.6 | 24.2 | 3.4 | 26.9 |
| Diabetes | ||||
| No (0) | 77.6 | 9.4 | 87.5 | 9.2 |
| Yes (1) | 22.4 | 21.4 | 12.5 | 22.8 |
| Other Medical Conditions Index# | ||||
| 0 | 70.7 | 9.0 | 83.9 | 8.8 |
| 1 | 21.2 | 17.2 | 13.4 | 17.8 |
| 2 | 7.0 | 23.7 | 2.5 | 36.8 |
| 3 | 1.0 | 38.9 | 0.3 | 50.0 |
| 4 | 0.1 | 50.0 | 0.0 | --- |
| 5 | 0.0 | --- | 0.0 | --- |
| Heparin/Coumadin Administered | ||||
| No (0) | 99.4 | 12.0 | 99.9 | 10.8 |
| Yes (1) | 0.6 | 18.2 | 0.1 | 100.0 |
| Medical Devices Present on Admission | ||||
| No (0) | 88.4 | 10.4 | 95.2 | 9.9 |
| Yes (1) | 11.6 | 24.5 | 4.8 | 30.6 |
| Level of Orientation | ||||
| Oriented | 93.1 | 11.4 | 69.0 | 13.1 |
| Some disorientation | 3.6 | 23.7 | 1.8 | 22.2 |
| Unknown | 3.4 | 17.2 | 29.3 | 5.0 |
| Level of consciousness | ||||
| Conscious | 96.6 | 11.8 | 81.4 | 12.2 |
| Some unconsciousness | 2.1 | 19.8 | 0.3 | 0.0 |
| Unknown | 1.3 | 22.5 | 18.3 | 5.1 |
| Decreased Motor Function | ||||
| No | 62.4 | 11.1 | 61.8 | 10.5 |
| Yes | 4.6 | 35.4 | 2.7 | 22.5 |
| Unknown | 33.0 | 10.7 | 35.5 | 10.6 |
| Creatinine Level+ | ||||
| <=3 mg/dL | 87.1 | 11.6 | 69.3 | 12.4 |
| > 3 mg/dL | 3.5 | 28.8 | 0.5 | 37.5 |
| Unknown | 9.4 | 9.9 | 30.2 | 6.8 |
| Albumin Level | ||||
| >=3 g/dL | 63.9 | 11.5 | 51.6 | 11.3 |
| < 3 g/dL | 8.7 | 23.5 | 1.3 | 35.0 |
| Unknown | 27.4 | 9.8 | 47.1 | 9.7 |
| Cholesterol^ | ||||
| < 100 mg/dL | 2.5 | 17.2 | 0.7 | 40.0 |
| 100–119 mg/dL | 3.6 | 11.7 | 0.6 | 11.1 |
| 120+ mg/dL | 46.6 | 13.2 | 31.4 | 11.4 |
| Unknown | 47.3 | 10.7 | 67.3 | 10.3 |
| Predicted Probability of Death“ | ||||
| Decile 1 | 9.9 | 0.8 | 10.0 | 1.3 |
| Decile 2 | 10.0 | 2.6 | 10.0 | 3.3 |
| Decile 3 | 10.0 | 6.9 | 10.0 | 4.6 |
| Decile 4 | 10.0 | 11.9 | 10.0 | 5.3 |
| Decile 5 | 10.0 | 8.2 | 10.0 | 4.0 |
| Decile 6 | 10.0 | 9.0 | 10.0 | 6.0 |
| Decile 7 | 10.0 | 12.1 | 10.0 | 9.9 |
| Decile 8 | 10.0 | 16.1 | 10.0 | 19.2 |
| Decile 9 | 10.0 | 19.3 | 10.0 | 21.9 |
| Decile 10 | 9.9 | 33.9 | 10.0 | 33.1 |
Scale from 0–5 indicating the number of the following diagnoses present on admission: tuberculosis/sarcoidosis, AIDS/HIV, cirrhosis, peripheral vascular disease, and ischemic heart disease.
Lower creatinine level indicates better clinical condition than higher level.
Midrange cholesterol level indicates better clinical condition than low or high level.
Predicted probability of death increases from Decile 1 to Decile 10. Probabilities were calculated by CHQC staff. See the text for details.
Objective 1
During the entire study period 12.1 percent (458/3,788) of the medical patients and 10.9 percent (165/1,511) of the surgical patients were referred to PAHC (Table 1). The percent of medical patients referred to PAHC increased from 7.8 percent in 1992 to 12.9 percent in 1996, an increase of 65.4 percent. The percent of surgical patients referred to PAHC increased from 8.7 percent in 1992 to 14.2 percent in 1996, an increase of 63.2 percent. There was a pronounced difference in the percent of patients referred to PAHC by the condition or procedure, ranging from 6.2 percent for GI hemorrhage to 21.3 percent for CHF among medical patients and from 2.9 percent for hysterectomy to 29.6 percent for vascular surgery among surgical patients.
Sixty-four percent (290/458) of the medical patients referred to PAHC actually used Medicaid-covered PAHC within 3 days of discharge. Ninety-nine percent (164/165) of the referred surgical patients used PAHC. We conducted bivariate statistical analyses comparing the medical patients referred to PAHC who did use it to those who did not, but could detect no differences between the two groups.
Development of Propensity Scores
The variables listed in Table 1 were entered into multivariable models to develop the propensity scores. The area under the ROC curve was .82 for the medical model and .83 for the surgical model, indicating good discrimination between stays referred to PAHC or to HOME.
Stays Matched on Propensity Scores
Objective 2
We were able to match by propensity score 97.2 percent (282/290) of the medical patients who used PAHC and 90.2 percent (148/164) of the surgical patients (Figure 1). We compared the matched stays on the covariates used to calculate the propensity scores. The pairs of medical stays do not differ at the 99 percent confidence level (used to account for multiple comparisons) on any variable, and the pairs of surgical stays are significantly different only for albumin level (at p<.01). (Results are available from the authors.) Thus, the propensity scores paired together stays that are similar to each other in the covariates used to calculate the probability of referral to PAHC.
Hypothesis 1
The only 90-day outcome with significant differences was total Medicaid expenditures, with the USE group having higher expenditures than the NO USE group (p<.05 for medical stays and p<.001 for surgical stays) (Table 2). The only outcome with lower utilization rates for the USE group was nursing home days of stay, although the results are not statistically significant. There were many cells with a median of 0, indicating that inpatient re-admissions and nursing home admissions were relatively rare.
Table 2.
Medicaid Expenditures and Utilization by Study Group, Index Stays Matched by Propensity Score, CHQC Hospitals, 1992–1996
| 90-Day Follow Up | 180-Day Follow Up | |||||
|---|---|---|---|---|---|---|
| Medicaid Expenditures and Utilization | number of stays | mean (cv #) or percent | median | number of stays | mean (cv #) or percent | median |
| Medical Stays (282 matched pairs) | ||||||
| Readmitted to Hospital (%) | ||||||
| USE | 106 | 38% | 0 | 149 | 53% | 1 |
| NO USE | 107 | 38% | 0 | 145 | 51% | 1 |
| Admitted to Nursing Home (%) | ||||||
| USE | 10 | 4% | 0 | 12 | 4% | 0 |
| NO USE | 12 | 4% | 0 | 15 | 5% | 0 |
| Hospital Days of Stay | ||||||
| USE | 106 | 6.6 (191.6) | 0 | 149 | 10.4 (159.1) | 3 |
| NO USE | 107 | 6.3 (236.2) | 0 | 145 | 10.1 (194.3) | 2 |
| Nursing Home Days of Stay | ||||||
| USE | 10 | 0.8 (662.6) | 0 | 12 | 2.2 (658.1) | 0 |
| NO USE | 12 | 2.6 (525.8) | 0 | 15 | 5.8 (491.5) | 0 |
| Total Medicaid Expenditures ($) | ||||||
| USE | 282 | 8,757 (155.6)* | 2,958 | 282 | 14,657 (136.2)* | 7,777 |
| NO USE | 282 | 7,119 (180.9)* | 1,684 | 282 | 12,549 (161.2)* | 5,681 |
| Surgical Stays(148 matched pairs) | ||||||
| Readmitted to Hospital (%) | ||||||
| USE | 45 | 30% | 0 | 54 | 36% | 0 |
| NO USE | 32 | 22% | 0 | 39 | 26% | 0 |
| Admitted to Nursing Home (%) | ||||||
| USE | 4 | 3% | 0 | 4 | 3% | 0 |
| NO USE | 2 | 1% | 0 | 2 | 1% | 0 |
| Hospital Days of Stay | ||||||
| USE | 45 | 3.7 (214.7) | 0 | 54 | 5.3 (204.0) | 0 |
| NO USE | 32 | 3.0 (283.0) | 0 | 39 | 3.8 (251.7) | 0 |
| Nursing Home Days of Stay | ||||||
| USE | 4 | 0.7 (772.5) | 0 | 4 | 0.7 (772.5) | 0 |
| NO USE | 2 | 0.9 (909.8) | 0 | 2 | 1.5 (1,006.4) | 0 |
| Total Medicaid Expenditures ($) | ||||||
| USE | 148 | 5,538(149.5)** | 1,934 | 148 | 8,670 (137.1)** | 3,777 |
| NO USE | 148 | 2,835(176.0)** | 784 | 148 | 4,199 (150.6)** | 1,651 |
cv (coefficient of variation) = (standard deviation/mean) × 100
p < .05,
p < 0.001. Categorical variables were tested with the McNemar test and continuous variables were tested with the Wilcoxon matched-pairs signed-rank test.
Hypothesis 2
The only 180-day study outcome with significant differences was total Medicaid expenditures, with the USE group having higher expenditures than the NO USE group (p<.05 for medical stays and p<.001 for surgical stays) (Table 2). Again, as with 90 days, nursing home days of stay showed a different pattern, with the USE group having (nonsignificantly) lower mean nursing home days of stay than the NO USE group.
The patients had high total Medicaid expenditures: After 90 days, mean total expenditures for patients in the matched pairs (medical and surgical patients combined) were $7,649 in the USE group and $5,761 in the NO USE group. After 180 days mean total expenditures were $12,596 and $9,675, respectively. Expenditures for medical and surgical patients separately are presented in Table 2.
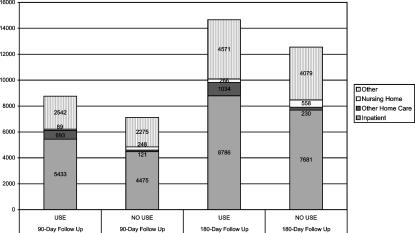
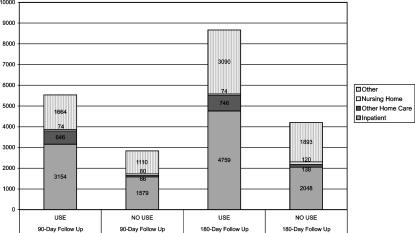
Figure 2 presents mean expenditures by type of health service received by the matched pairs of medical patients during the two follow-up periods. Mean expenditures on inpatient services, home care initiated four days or more after the index stay discharge date, and other services were higher in the USE group than in the NO USE group. Expenditures on nursing home service were lower in the USE group. Results are similar for the surgical stays (Figure 3).
Figure 2.
Differences in Mean Total Medicaid Expenditures in Dollars between Patients Using Post-acute Home Care (“Use”) and Patients Not Using Post-Acute Home Care (“No Use”) by the Type of Service, 282 Pairs of Medical Stays Matched by Propensity Score
Figure 3.
Differences in Mean Total Medicaid Expenditures in Dollars between Patients Using Post-acute Home Care (“Use”) and Patients Not Using Post-acute Home Care (“No Use”) by the Type of Service, 148 Pairs of Surgical Stays Matched by Propensity Score.
Sensitivity Analysis
When we tested the hypotheses, we relied on the propensity score to eliminate any bias in the allocation of stays to the USE or NO USE group. However, if there were variables not in the propensity score that influenced the allocation of stays to the USE and NO USE groups, the results might be biased. To estimate the potential impact of unmeasured variables on the results we conducted a sensitivity analysis.
Table 3 presents the results of the sensitivity analysis. Under an outcome of interest, such as total Medicaid expenditures within 90 days after discharge, maximum and minimum p values are given for various degrees of bias (indicated by the values of W). If a stay has a 50 percent chance of being in either the USE or NO USE group (i.e., if the propensity score perfectly eliminates bias), W would equal 1.00 and the p values would be equal. In the sensitivity analysis, we allowed W to vary, to impose a bias. We measured the bias in both directions, since we did not know its direction (hence the maximum and minimum values of p). Whether or not the results are sensitive to unmeasured variables is indicated by how large W becomes before the p value changes from significant (at the p<.05 level) to insignificant or vice versa relative to the baseline value. (The sensitivity analysis does not indicate what the unmeasured variables might be, however, or the direction of the bias.) A study in which the value of W is 10 before the significance level changes is considered highly robust to unmeasured variables (Rosenbaum 1991). A study in which the value is 2.0 is considered moderately sensitive. Only the p values that are significant or close to significance are presented in Table 3.
Table 3.
Results of the Sensitivity Analysis, CHQC Hospitals, 1992–1996
| P-values | |||||
|---|---|---|---|---|---|
| Outcomes | w=1.0 | w=1.25 | w=1.50 | w=1.75 | w=2.0 |
| Medical Stays(282 matched pairs) | |||||
| Total Medicaid expenditures, 90-day follow up | |||||
| maximum | .010 | .341 | – | – | – |
| minimum | .010 | .000 | – | – | – |
| Total Medicaid expenditures, 180-day follow up | |||||
| maximum | .025 | .537 | – | – | – |
| minimum | .025 | .000 | – | – | – |
| Surgical Stays(148 matched pairs) | |||||
| Readmitted to hospital, 90-day follow up | |||||
| maximum | .049 | .200 | – | – | – |
| minimum | .049 | .007 | – | – | – |
| Total Medicaid expenditures, 90-day follow up | |||||
| maximum | .000 | .000 | .012 | .083 | – |
| minimum | .000 | .000 | .000 | .000 | – |
| Readmitted to hospital, 180-day follow up | |||||
| maximum | .036 | .176 | – | – | – |
| minimum | .036 | .004 | – | – | – |
| Total Medicaid expenditures, 180-day follow up | |||||
| maximum | .000 | .000 | .002 | .022 | .09 |
| minimum | .000 | .000 | .000 | .000 | .00 |
The sensitivity analysis indicates that the most robust results are for total Medicaid expenditures within 180 days after discharge for surgical patients, as indicated by the fact that the significance does not change until W=1.75. This would not, however, be considered a robust result. For the other study outcomes, the significance changes at W=1.5 or lower, indicating that unmeasured variables may have biased the selection of stays into the USE or NO USE group.
Discussion and Policy Relevance
Based on this study of hospitalized Medicaid eligibles in the Greater Cleveland area, it does not appear that post-acute home care (PAHC) utilization was associated with lower health service utilization rates or with lower total Medicaid expenditures, after controlling for the need for post-acute services. At the same time, the results suggest that there was potential underutilization, at least among medical patients, as indicated by the fact that 36 percent of the medical patients referred to PAHC apparently did not receive post-acute Medicaid-covered home care services.
Previous clinical trials of PAHC suggest that it can result in cost savings under specific conditions. Rich and colleagues found that PAHC provided to patients with congestive heart failure, in an intervention including intensive case-management and health education, resulted in savings following the index stay (Rich et al. 1995). A randomized trial of the cost effectiveness of hospital-based home care for 404 disabled and terminally ill veterans found health services costs were 13 percent lower after six months among those assigned to the home-care team compared to those receiving customary care, although the difference was not statistically significant (Cummings et al. 1991). A meta-analysis of 20 randomized clinical trials conducted between 1967 and 1992 found that utilization of PAHC was associated with a small to moderate reduction in subsequent inpatient days of stay, depending on whether a single outlier study with a large effect was included (Hughes et al. 1997). When the outlier study was excluded, effect sizes across studies targeting terminally ill patients were still homogenous, but effect sizes across studies targeting non-terminal patients were not homogeneous, suggesting that the “magnitude of the effect sizes [for non-terminal patients] may be contingent on study characteristics and/or their interactions” (Hughes et al. 1997). These studies and two additional literature reviews indicate that PAHC can result in cost savings if it is targeted to the population most in need of services, who otherwise would have been institutionalized (Weissert 1985; Chappell 1994).
In contrast, the use of PAHC in this study was based on decisions made by the hospital, the home care provider, the patient, and the family, and not on the basis of allocation criteria by representatives or agents of the Medicaid program. Reports on providers' responses to recent changes in Medicare payments for home health care suggest that limiting or rationing the number of high-need clients admitted to home care is a widespread practice (Pear 2000). Anecdotal information suggests that during the study period home care providers in Ohio may have restricted the number or proportion of Medicaid recipients, especially high-need patients, they agreed to accept due to low state reimbursement rates (Madigan, personal communication). (In 1998 Medicaid increased home care nursing rates and physical, occupational, and speech/language therapy visits rates substantially.
As noted above, the traditional focus of Medicaid programs has been on long-term home care use rather than short-term post-acute care. However, post-acute home care will warrant greater attention in the future for two reasons. The first reason is related to decreases in inpatient length of stay. During the four-year study period, the mean inpatient length of stay for the study population decreased by 1 day and 1.3 days for medical and surgical patients, respectively. In the United States, the Medicaid mean inpatient length of stay decreased by .7 days during the same period (Health Care Financing Administration 1998; 1999). These decreases in length of stay suggest that patients may be being discharged “sicker and quicker” and therefore with greater need for PAHC. The second reason PAHC warrants attention is that the number and proportion of hospital-based home care agencies has increased dramatically in the past 30 years, rising from 7.6 percent of Medicare-certified agencies in the United States in 1967 to 25.8 percent in 1997 (National Association for Home Care 2000). Hospitals owning home care agencies may be more likely to refer patients to PAHC, especially in urban areas like Cleveland (Dansky, Milliron, and Gamm 1996).
The results of this study have implications for policy makers and health services researchers:
Monitoring and targeting
Ohio Medicaid may find it useful to target the use of PAHC, monitor its use more closely, and intensify existing utilization review practices.
Potential under-use
Further study is needed to determine whether patients referred to PAHC who do not receive it have unmet need for care or whether their needs are met through other formal mechanisms or through informal support networks. To identify patients who were referred to PAHC but did not receive it, specially abstracted medical record data similar to the CHQC data would not be needed, since patients could be identified through routinely collected Medicaid claims data. However, to determine whether unmet need existed or whether other resources were used to meet patients' needs, it would be necessary to follow up directly with the patients or to review information on patients' functional status, informal supports, and preferences.
Case management
The patients studied had high mean total Medicaid expenditures at both 90 and 180 days after the index stay. More in-depth study of nonelderly Medicaid hospital patients may identify high-cost patients who could benefit from case management to coordinate health services utilization and maximize the use of lower-cost services when appropriate.
Health services research
Two methodological points deserve mention. First, the increase over time in the percent of patients referred to PAHC and the differences in referral rates by condition and procedure emphasize the importance of including temporal and case-mix adjustments in studies of PAHC utilization and costs. Second, we excluded the index stay from the calculations of total Medicaid expenditures. If PAHC substituted for some days of the index stay and resulted in a shorter index stay and lower overall total Medicaid expenditures, then excluding the index stay would mask a possible cost savings associated with PAHC. However, we found that the probability that a patient would be referred to PAHC actually increased as length of stay increased (as shown in Table 1), which suggests that PAHC did not substitute for inpatient days. Thus, the findings do not appear to be biased by excluding the index stay from expenditure calculations.
This study of post-acute home care use has two notable strengths. The first is the availability of sophisticated information on inpatient severity of illness on admission from the CHQC study. The second is the use of propensity score methods to overcome the limitations of observational data. To our knowledge, this is the first application of propensity score methods to home care.
Counterbalancing those strengths are several limitations that must be acknowledged. Because we used observational rather than randomized clinical trial data to study outcomes, we had to rely on the propensity score to account for treatment selection bias. We did not have access to variables on functional status or living situation, two characteristics that are related to use of home care among Ohio Medicaid eligibles (Payne, DiGiuseppe, and Tilahun 1999) and others (Nyman and Svetlik 1989; Wiener and Hanley 1992; Arnold, Gage, and Harris 1994; Chappell 1994; Goldberg 1999). As a result, our ability to reflect differences in patients' need for PAHC may be limited. The CHQC severity information is collected at admission and does not necessarily reflect the patients' severity at discharge. Patients who used home care may have had greater severity of illness at discharge than those who did not. We were limited to economic outcomes relevant to Medicaid; we did not have information on non-economic outcomes or outcomes relevant to patients or their care givers, such as satisfaction or quality of life. The decision to use PAHC is complex and many actors are involved—the physician, discharge planner, patient, family, and home care agency. We have information about the hospitals' assessment of the patients but no information about the other actors' assessments of the patients or about the agencies' decision-making process. Future research will be needed to determine whether variables not measured here, such as functional status or living situation, account for the higher expenditures in the USE group following discharge. Finally, the study was conducted in one metropolitan area and the results may not be representative of the situation elsewhere.
In conclusion, two streams of thought prompted Ohio and other state Medicaid programs to expand the use of home- and community-based services: the social value placed on living at home as long as possible and the belief that community-based services are less expensive than institutional long-term care (Wiener 1999). Home care use is rapidly increasing and dynamically responding to changes in the health care market place. As Medicaid programs strive to become value purchasers of health care, it will be important to monitor the use of PAHC to assure that it is efficient and appropriate.
Notes
A small proportion of the patients not referred to PAHC actually did use PAHC. They were classified in the USE group.
We did not use as the proxy for need whether the patient actually used home care or not, since the use of home care is influenced by factors not related to the patient's need for services, such as agencies' willingness to accept Medicaid referrals or the patient's or family's decision to use home care. We wanted the need proxy to reflect only the patient's need for services based on clinical characteristics.
Two thirds (67.5 percent) of the 14,811 stays linked on all six of the merging variables. An additional 12.8 percent linked on five variables and 4.2 percent linked on four variables.
Supported by the Medicaid Technical Assistance and Policy Program (MEDTAPP) of the Ohio Department of Human Services and the Ohio Board of Regents and by the Cleveland Foundation. The views expressed here are not necessarily those of the funders.
References
- Arnold S, Gage B, Harris J. Interim Analysis of Payment Reform for Home Health Services. Washington DC: Prospective Payment Commission; 1994. [Google Scholar]
- Ash AS, Shwartz M, Iezzoni LI. Risk Adjustment for Measuring Healthcare Outcomes. Chicago: Health Administration Press; 1997. “Evaluating the Performance of Risk-Adjustment Methods: Dichotomous Measures”; pp. 427–71. [Google Scholar]
- Blewett LA, Kane RL, Finch M. “Hospital Ownership of Post-Acute Care: Does It Increase Access to Post-Acute Care Services?”. Inquiry. 1995–1996;32(4):457–67. [PubMed] [Google Scholar]
- Bureau of Labor Statistics. In Statistical Abstract of the United States: 1998. Washington DC: U.S. Bureau of the Census; 1998. “Consumer Price Indexes of Medical Care Prices: 1980–1998”; p. 124. [Google Scholar]
- Chappell NL. “Home Care Research: What Does It Tell Us?”. The Gerontologist. 1994;34(1):116–20. doi: 10.1093/geront/34.1.116. [DOI] [PubMed] [Google Scholar]
- Connors AF, Speroff T, Dawson NV, Thomas C, Harrell Jr FE, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson Jr WJ, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA. “The Effectiveness of Right Heart Catheterization in the Initial Care of Critically Ill Patients.”. Journal of the American Medical Association. 1996;276(11):889–97. doi: 10.1001/jama.276.11.889. [DOI] [PubMed] [Google Scholar]
- Cummings JE, Weaver FM, Hughes SL, Braun B, Romeis JC, Coe RM. Quality and Cost Containment in Care of the Elderly. New York: Springer; 1991. “Cost Effectiveness and Hospital-based Home Care.”; pp. 158–74. [Google Scholar]
- D'Agostino RB., Jr “Propensity Score Methods for Bias Reduction in the Comparison of a Treatment to a Non-randomized Control Group.”. Statistics in Medicine. 1998;17(19):2265–81. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Dansky KH, Milliron M, Gamm L. “Understanding Hospital Referrals to Home Health Agencies.”. Hospital and Health Services Administration. 1996;41(3):331–42. [PubMed] [Google Scholar]
- Dobson A, Moran D, Young G. “The Role of Federal Waivers in the Health Policy Process.”. Health Affairs. 1992;11(4):72–94. doi: 10.1377/hlthaff.11.4.72. [DOI] [PubMed] [Google Scholar]
- Drake C, Fisher L. “Prognostic Models and the Propensity Score.”. International Journal of Epidemiology. 1995;24(1):183–7. doi: 10.1093/ije/24.1.183. [DOI] [PubMed] [Google Scholar]
- Goldberg H. Home Health Case-Mix Project: Second Interim Report. Cambridge MA: Abt Associates; 1999. [Google Scholar]
- Hanley JA, McNeil BJ. “A Method of Comparing the Areas under Receiving Operating Characteristic Curves Derived from the Same Cases.”. Radiology. 1983;148(3):839–43. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- Health Care Financing Administration (HCFA) U.S. Health Care Financing Administration Office of Information Systems Statistical Abstract of the United States: 1998. Washington DC: U.S. Bureau of the Census; 1998. “Medicaid—Selected Utilization Measures: 1980 to 1996”; p. 123. [Google Scholar]
- Health Care Financing Administration (HCFA) U.S. Health Care Financing Administration Office of Information Systems Statistical Abstract of the United States: 1998. Washington DC: U.S. Bureau of the Census; 1999. “Medicaid—Selected Utilization Measures: 1980 to 1997”; p. 124. [Google Scholar]
- Health Care Financing Administration (HCFA) “National Health Expenditures Aggregate and Per Capita Amounts Percent Distribution and Average Annual Percent Growth by Source of Funds: Selected Calendar Years 1960–1998.”. [June 15 2001];2000a http://www.hcfa.gov/stats/nhe-oact/tabkes/tablist.asp.
- Health Care Financing Administration (HCFA) “Home and Community-Based Services 1915 (c). Waivers.”. [June 15 2001];2000b http://www.hcfa.gov/medicaid/hpg4.htm.
- Health Care Financing Administration (HCFA) “Figure 64. Distribution of Medicaid Vendor Payments by Eligibility Group: FY 1997”. Medicare and Medicaid Statistical Supplement 1999 p 82 Health Care Financing Review. 2000c [Google Scholar]
- Heckman JJ, Ichimura H, Smith J, Todd P. “Sources of Selection Bias in Evaluating Social Programs: an Interpretation of Conventional Measures and Evidence on the Effectiveness of Matching as a Program Evaluation Method.”. Proceedings of the National Academy of Sciences in the United States of America. 1996;93(23):13416–20. doi: 10.1073/pnas.93.23.13416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschman C. “Home Health Care Booms as Hospital Stays Shorten.”. Business First—Columbus 20 December. 1993;10(16)(1):13. [Google Scholar]
- Hughes SL, Ulasevich A, Weaver FM, Henderson W, Manheim L, Kubal JD, Bonarigo F. “Impact of Home Care on Hospital Days: A Meta-analysis.”. Health Services Research. 1997;32(4):415–32. [PMC free article] [PubMed] [Google Scholar]
- Joffe MM, Rosenbaum PR. “Invited Commentary: Propensity Scores.”. American Journal of Epidemiology. 1999;150(4):327–33. doi: 10.1093/oxfordjournals.aje.a010011. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Iezzoni LI. Risk Adjustment for Measuring Healthcare Outcomes. Chicago: Health Administration Press; 1997. “Data Sources and Implications: Administrative Databases.”; pp. 169–242. [Google Scholar]
- Kenney GM. “Understanding the Effects of PPS on Medicare Home Health Use.”. Inquiry. 1991;28(2):129–39. [PubMed] [Google Scholar]
- Kramer AM, Shaughnessy PW, Pettigrew ML. “Cost-effectiveness Implications Based on a Comparison of Nursing Home and Home Health Case Mix.”. Health Services Research. 1985;20(4):387–405. [PMC free article] [PubMed] [Google Scholar]
- Legoretta AP, Leung KM, Berkbigler D, Evens R, Liu X. “Outcomes of a Population-Based Asthma Management Program: Quality of Life Absenteeism and Utilization.”. Annals of Allergy Asthma and Immunology. 2000;85(1):28–34. doi: 10.1016/S1081-1206(10)62430-1. [DOI] [PubMed] [Google Scholar]
- Leutz W. “Policy Choices for Medicaid and Medicare Waivers.”. Gerontologist. 1999;39(1):86–93. doi: 10.1093/geront/39.1.86. [DOI] [PubMed] [Google Scholar]
- Miettinen O. “Stratification of a Multivariate Confounder Score.”. American Journal of Epidemiology. 1976;104(6):609–21. doi: 10.1093/oxfordjournals.aje.a112339. [DOI] [PubMed] [Google Scholar]
- National Association for Home Care (NAHC) “Basic Statistics about Home Care.”. [June 15 2001];2000 http://www.nahc.org/Consumer/hcstats.html.
- Nyman JA, Svetlik MA. “Does the Average Cost of Home Health Care Vary with Case Mix?.”. Public Health Reports. 1989;104(4):335–41. [PMC free article] [PubMed] [Google Scholar]
- Payne SMC, DiGiuseppe DL, Tilahun N. Medicaid Technical Assistance and Policy Program (MEDTAPP) of the Ohio Department of Human Services and the Ohio Board of Regents. Cleveland OH: Case Western Reserve University; 1999. “Use of Home- and Community-based Health Services by Disabled Ohio Medicaid Recipients”. [Google Scholar]
- Pear R. “Medicare Spending for Care at Home Plunges by 45%.”. New York Times. 2000 [Google Scholar]
- Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. “A Multidisciplinary Intervention to Prevent the Readmission of Elderly Patients with Congestive Health Failure.”. New England Journal of Medicine. 1995;333(18):1190–5. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- Riley T. “State Health Reform and the Role of 1115 Waivers.”. Health Care Financing Review. 1995;16(3):139–49. [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum P. “Discussing Hidden Bias in Observational Studies.”. Annals of Internal Medicine. 1991;115:901–5. doi: 10.7326/0003-4819-115-11-901. [DOI] [PubMed] [Google Scholar]
- Rosenbaum P, Rubin D. “The Central Role of the Propensity Score in Observational Studies for Causal Effects.”. Biometrika. 1983a;70:41–55. [Google Scholar]
- Rosenbaum P, Rubin D. “Assessing Sensitivity to an Unobserved Binary Covariate in an Observational Study with Binary Outcome.”. Journal of the Royal Statistical Society. 1983b;45:212–18. [Google Scholar]
- Rosenbaum P, Rubin D. “Reducing Bias in Observational Studies Using Subclassification on the Propensity Score.”. Journal of the American Statistical Association. 1984;79(387):516–24. [Google Scholar]
- Rosenthal GE, Harper DL. “Cleveland Health Quality Choice: A Model for Collaborative Community-Based Outcomes.”. Journal on Quality Improvement. 1994;20(8):425–42. doi: 10.1016/s1070-3241(16)30088-8. [DOI] [PubMed] [Google Scholar]
- Rosenthal GE, Hammar PJ, Way LE, Shipley SA, Doner D, Wojtala B, Miller J, Harper DL. “Using Hospital Performance Data in Quality Improvement: The Cleveland Health Quality Choice Experience.”. Joint Commission Journal on Quality Improvement. 1998;24(7):347–60. doi: 10.1016/s1070-3241(16)30386-8. [DOI] [PubMed] [Google Scholar]
- Rubin DB. “Estimating Causal Effects from Large Data Sets Using Propensity Scores.”. Annals of Internal Medicine. 1997;127(8):757–63. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. Cary NC: SAS Institute Inc; 1989–1996. [Google Scholar]
- Smith NL, Reiber GE, Psaty BM, Heckbert SR, Siscovick DS, Ritchie JL, Every NR, Koepsell TD. “Health Outcomes Associated with Beta-blocker and Diltiazem Treatment of Unstable Angina.”. Journal of the American College of Cardiology. 1998;32(5):1305–11. doi: 10.1016/s0735-1097(98)00408-2. [DOI] [PubMed] [Google Scholar]
- Stone RA, Obrosky DS, Singer DE, Kapoor WN, Fine MJ. “Propensity Score Adjustment for Pretreatment Differences between Hospitalized and Ambulatory Patients with Community-acquired Pneumonia. Pneumonia Patient Outcomes Research Team (PORT) Investigators.”. Medical Care. 1995;33(4):AS56–66. [PubMed] [Google Scholar]
- Tai-Seale M, Croghan TW, Obenchain R. “Determinants of Antidepressant Treatment Compliance: Implications for Policy.”. Medical Care Research and Review. 2000;57(4):491–512. doi: 10.1177/107755870005700405. [DOI] [PubMed] [Google Scholar]
- Welch HG, Wennberg DE, Welch WP. “The Use of Medicare Home Health Care Services.”. New England Journal of Medicine. 1996;335(5):324–9. doi: 10.1056/NEJM199608013350506. [DOI] [PubMed] [Google Scholar]
- Weissert WE. “Seven Reasons Why It Is So Difficult to Make Community-based Long-term Care Cost-Effective.”. Health Services Research. 1985;20(4):423–33. [PMC free article] [PubMed] [Google Scholar]
- Wiener JM, Hanley RJ, Shortell S, Reinhardt U. Improving Health Policy and Management. Ann Arbor MI: Health Administration Press; 1992. “Caring for the Disabled Elderly: There's No Place Like Home”; pp. 75–110. [Google Scholar]
- Wiener JM, Campbell JC, Ikegami N. Long-term Care for Frail Older People: Reaching for the Ideal System. Tokyo Japan: Springer-Verlag; 1999. “Balancing Institutional and Home and Community-Based Care”; pp. 215–218. [Google Scholar]