Abstract
Objective
To examine market competition and facility characteristics that can be related to technical efficiency in the production of multiple dialysis outputs from the perspective of the industrial organization model.
Study Setting
Freestanding dialysis facilities that operated in 1997 submitted cost report forms to the Health Care Financing Administration (HCFA), and offered all three outputs—outpatient dialysis, dialysis training, and home program dialysis.
Data Sources
The Independent Renal Facility Cost Report Data file (IRFCRD) from HCFA was utilized to obtain information on output and input variables and market and facility features for 791 multiple-output facilities. Information regarding population characteristics was obtained from the Area Resources File.
Study Design
Cross-sectional data for the year 1997 were utilized to obtain facility-specific technical efficiency scores estimated through Data Envelopment Analysis (DEA). A binary variable of efficiency status was then regressed against its market and facility characteristics and control factors in a multivariate logistic regression analysis.
Principal Findings
The majority of the facilities in the sample are functioning technically inefficiently. Neither the intensity of market competition nor a policy of dialyzer reuse has a significant effect on the facilities' efficiency. Technical efficiency is significantly associated, however, with type of ownership, with the interaction between the market concentration of for-profits and ownership type, and with affiliations with chains of different sizes. Nonprofit and government-owned facilities are more likely than their for-profit counterparts to become inefficient producers of renal dialysis outputs. On the other hand, that relationship between ownership form and efficiency is reversed as the market concentration of for-profits in a given market increases. Facilities that are members of large chains are more likely to be technically inefficient.
Conclusions
Facilities do not appear to benefit from joint production of a variety of dialysis outputs, which may explain the ongoing tendency toward single-output production. Ownership form does make a positive difference in production efficiency, but only in local markets where competition exists between nonprofit and for-profit facilities. The increasing inefficiency associated with membership in large chains suggests that the growing consolidation in the dialysis industry may not, in fact, be the strategy for attaining more technical efficiency in the production of multiple dialysis outputs.
Keywords: Dialysis market, efficiency, ownership, consolidation
In the health-care sector, the existence of conflicts of interest between the payers and the providers of health-care services are not surprising. The situation may take even more serious form in price-regulated health-care markets. The Medicare end-stage renal disease (ESRD) program, as a virtually monopsonistic buyer of ESRD-related services, offers an example of this phenomenon (Farley 1994).
Medicare has provided coverage to approximately 93 percent of those with ESRD, regardless of age, since its inception in 1973. As of 1997, the ESRD population consisted of more than three hundred thousand people, a disproportionate majority of whom received dialysis treatments (USRDS 1999). The total ESRD payments made by Medicare add up to over $14 billion (USRDS 1999). Given the incomplete control over program enrollment and the changing patient mix, cost-containment policies have been integral to the program. Major cost-cutting policies have included a fixed fee structure for dialysis services, bundling once separately billable services into the composite rate, shifting program costs to the private sector, and a reduction in real payments over time (Levinsky 1993; Iglehart 1993; Nissenson and Rettig 1999; Rettig 1996; Farley 1994).
Such policies have forced providers to search for every possible mean of economizing in providing dialysis treatment. Some of the well-known facility cost-saving efforts are reuse of dialyzers, using technological advancements to allow shorter dialysis sessions, and staffing changes. Considering the dominant presence of for-profit units and the growing consolidation, ownership form and affiliation with dialysis chains can be seen as other facility strategies to reduce costs and generate revenue. Overall, such facility responses have given rise to the consensus that dialysis facilities are operated by efficient companies/persons (Fox 1993; Kendix 1997; Levinsky 1993).
This study assesses the relationships between competition and facility features and efficiency in producing multiple dialysis outputs in an integrated model. The next section reviews the research literature that has assessed the effects of market and facility features on production efficiency. The following section develops a conceptual framework, drawing from an industrial organization model, and presents hypotheses to be tested. The subsequent two sections describe the data and analysis techniques used to measure efficiency and to test the hypotheses, and present the results from efficiency measurement and the efficiency-related multivariate model. The last section presents a discussion of the findings, limitations of the study, and suggestions for future study.
Background
Current knowledge on factors related to efficiency is limited to only a few studies. Held and Pauly (1983), analyzing the relationship between competition and production efficiency, showed that facilities in competitive markets produced more dialysis treatments. The study also addressed the issue of “competitive amenity bias,” indicating that as competition increases, the level of amenity delivered to patients is affected, which may result in varying levels of cost or productivity. Since the study used data from before the implementation of Medicare composite rate payment in 1983, which was expected to change provider incentives toward providing more home dialysis treatment, there is a need to verify the findings from that study by utilizing more recent data.
Using national data to study 1,224 Medicare-certified, freestanding dialysis units, the study by Griffiths et al. (1994) found for-profit units to produce more dialysis treatments as compared to their nonprofit counterparts, adjusting for resource inputs consumed and facility case-mix characteristics. The study failed, however, to include factors that can further reveal ownership-related differences in the efficiency of dialysis production, such as ownership mix in the market, competition, and dialyzer re-use.
Hirth et al. (1999) addressed the impact on costs of ownership type, dialyzer reuse, and engagement in consolidation. The study showed no statistical difference in the costs of dialysis between for-profit and nonprofit units, after controlling for type of membrane and reuse as quality dimensions, and for case mix. Units that reused dialyzers were found to have lower costs than units that did not do so. The study also found significant benefits of scale economies for units affiliated with one of the largest national chains, as compared to independent units. However, the results of this study did not include measures of competition and mixed-ownership markets.
In addition to not addressing some potential determinants of efficiency, the previous research on efficiency/cost examined dialysis units regardless of whether they engaged in single or multiple output production. Thus, little is known about whether the observed relationships between efficiency and its predictors vary in multiple output markets. Nor is it clear to what extent current cost-cutting policies provided incentives for efficiency for facilities with different dialysis modalities. Given that most facilities have offered only one type of modality, usually outpatient hemodialysis, evaluating efficiency in the production of multiple dialysis outputs may shed light on why units are reluctant to offer multiple modalities.
Theoretical Framework
In industrial organization theory, the traditional approach for analysis is based on the market structure–conduct–performance paradigm (Scherer 1980). In light of that theory, this study assumes that market competition and a variety of facility characteristics affect a facility's technical efficiency, and that all those factors are influenced strongly by government payment policy. Facility characteristics here are a policy of reusing dialyzer as a product differentiation strategy, interorganizational affiliations, and type of ownership.
Market Competition and Efficiency
According to the model, the more intense the competition, the greater the technical efficiency firms will exhibit. The model also recognizes efficient production from a profit-maximizing monopolist that produces the output at lowest possible cost. The former assumption may not always be valid in health-care markets that are nonprice competitive. Numerous studies have consistently found that before the prospective payment system, nonprice competition among hospitals increased costs and decreased efficiency (Wilson and Jadlow 1982; Robinson and Luft 1985; Joskow 1980).
Since the federal government is virtually a monopsonist buyer of dialysis services and pays fixed prices for them, competition on price is no longer relevant (Farley 1996), which gives rise to nonprice competitive strategies. In the face of increased nonprice competition, facilities may apply strategies that raise costs: holding more backup capacity (Held and Pauly 1983), adopting newer technology (Hirth and Chernew 1997), accepting older and sicker patients (Farley 1993), or competing for physicians through consulting fees and bonuses for service volumes (Bovbjerg, Held, and Diamond 1987; Farley 1996). In light of current research, the following hypothesis can be postulated:
H1. Dialysis facilities that are located in less competitive markets will be more likely to be technically efficient in producing dialysis treatments than are dialysis facilities located in more competitive markets.
Facility Characteristics and Efficiency
From the theoretical standpoint, although under nonprice competition facilities may differentiate their products to position themselves favorably in the market, fixed-payment policy restricts their capabilities for doing so (Tirole 1988). That may explain why outpatient dialysis, especially hemodialysis, has remained a mainstay product for most facilities. Rather than by the scope of their products, units may apply differentiation by the quality of their dialysis care. Not reusing dialyzers, for example, may be seen as a measure of better quality care, since research shows that reuse is associated with adverse outcomes such as inadequate dialysis and higher mortality rates (Held et al. 1994; Feldman et al. 1996). Once again, in a fixed-price dialysis industry, one can expect units to be less likely to provide better quality of medical care (i.e., no to reuse dialyzers). Despite the demonstrated detrimental effects on patient outcomes, reuse of dialyzers has long been practiced, mainly for economical reasons (Iglehart 1993; Ogden and Friedl 1984). Reprocessing and reusing the same dialyzer for the same patient saves a facility money by reducing supply costs, which are an important input item (Hirth et al. 1999).
To deal with fixed prices and competition, facilities may also involve in a corporate strategy, to enhance efficiency through the benefits of economies of scale such as more coordinated activities, standardized labor staffing, volume discounts on purchasing, and reduced unit costs (Zuckerman 1979; Mason 1980). As of 1998, approximately 61 percent of dialysis facilities were owned or managed by the two largest national chains (Nephrology News and Issues 1998). In addition to the steady growth of dialysis chains, the market has witnessed the continued profitability of large chains (Burns 1992; Nissenson and Rettig 1999). Under financial pressure, however, members of smaller chains as well as independent units may not perform as well as do members of large chains (Nissenson and Rettig 1999). Thus, efficient production of dialysis may be affected by the size of the chain with which the unit affiliates (Hirth et al. 1999).
From the viewpoint of property rights theory, the pursuit of profit maximization leads to divergent behavior between for-profit and nonprofit units in improving efficiency. However, the existing literature on this issue yields mixed results (Griffiths 1994; Hirth et al. 1999). Given the ongoing dominance of for-profit entities in the dialysis industry (HCFA 1999), the notion of greater efficiency from for-profit facilities is adopted in this study.
The distinctive behavior of for-profit and nonprofit units in controlling costs and in enhancing efficiency may, on the other hand, converge in mixed-ownership markets. According to Hirth (1997), competition from nonprofit firms may exert pressure on for-profit firms to provide socially desirable but unprofitable services. Similarly, competition from for-profit firms can increase the efficiency of nonprofit firms. The growth of for-profit dialysis units has raised questions about whether profit seeking behavior leads to the selection of treatment modes that were more profitable but not necessarily socially desirable. Previous research has shown that nonprofit units provide more home dialysis (Schlesinger, Cleary, and Blumental 1989) and more referrals for renal transplants than for-profit units do (Garg et al. 1999; Port, Wolfe, and Held 2000). Furthermore, Cleary, Schlesinger, and Blumental (1991) revealed that units in areas with higher percentages of for-profit units were more likely to favor in-center dialysis over home dialysis and transplants. Thus, in a given market with a higher proportion of for-profit units, nonprofit units may tend to “act like” for-profit enterprises and pursue efficiency.
Based on the foregoing discussion, this study posits four additional hypotheses about the relationship between the characteristics of facilities and technical efficiency.
H2. Dialysis facilities that reuse dialyzers may appear to be more technically efficient than dialysis facilities that do not reuse dialyzers.
H3. Dialysis facilities that are members of large dialysis chains will be more likely than independent dialysis facilities to be technically efficient.
H4. For-profit dialysis facilities will be more likely than nonprofit facilities to be technically efficient,
H5. Nonprofit dialysis facilities will be likely to be technically efficient as the percentage of for-profit dialysis facilities in a given market grows.
METHODOLOGY
Study Population and Sample
Using the 1997 IRFCRD file maintained by HCFA, the study included 840 Medicare-certified freestanding dialysis facilities that submitted cost report forms to HCFA and produced three pre-specified dialysis outputs jointly.1 The selection of facilities was restricted to those that reported nonzero operating costs (797, or 95 percent of 840 facilities). Among those, facilities that had zero labor inputs were included in the sample, given the fact that a positive dialysis output may be produced with the absence of some labor inputs (e.g., physicians) (Held and Pauly 1983). Facilities with outlier information on capital and labor inputs were excluded from the sample: four facilities with zero information on capital input and two facilities that had extreme labor inputs (2,325 registered nurses and 4,425 other medical staff). As a result, the study consisted of a final sample of 791 freestanding dialysis facilities (94 percent of the total 840 three-output facilities).
The study excluded hospital-based dialysis facilities to rule out the variations between freestanding and hospital-based facilities in case mix (Plough et al. 1984; Radecki et al. 1988; Held et al. 1994; Held, Pauly, and Diamond 1987), organizational structure, and reimbursement rates. Consequently, the study examines a relatively homogenous study group in making confident comparisons across “like” dialysis facilities.
Data Sources
This study is a cross-sectional study of freestanding dialysis facilities for the year 1997. Information on dialysis treatments produced by each treatment modality, quantities of labor, operating expenses, and statistical data on the characteristics of the facilities were obtained from the 1997 IRFCRD file. The Area Resource File, a database of county-aggregated statistics, was used to draw a number of characteristics of the population living in the local market area.
Variable Construction
A binary dependent variable of efficiency versus inefficiency in the multivariate analysis of efficiency-related factors was constructed, based on the efficiency scores estimated through several variables that were believed to accurately reflect dialysis production. Various types of dialysis modalities that are considered the products of the dialysis facility (Dor, Held, and Pauly 1992) were disaggregated into three output categories: outpatient dialysis, dialysis training, and home dialysis treatments. Each output variable was measured by the additive sum of the modality-specific dialysis treatments produced. For example, the total number of outpatient dialysis treatments was the sum of the number for outpatient hemodialysis and the number for intermittent peritoneal dialysis. To have a uniform unit of measurement, the total for home program continuous ambulatory/continuous cycling peritoneal dialysis patient-week treatments was added into the total home program outputs as outpatient hemodialysis equivalents, by multiplying three (Dor, Held, and Pauly 1992; Hirth et al. 1999; Griffiths et al. 1994).
Labor inputs consisted of the number of full-time equivalent (FTE) physicians, FTE registered nurses (RNs), and other FTE medical staff—licensed nurses, licensed practical nurses, aides, technicians, dieticians, and social workers (Griffiths et al. 1994; Held and Pauly 1983). Capital input was calculated by the total number of dialysis machines (Griffiths et al. 1994; Held and Pauly 1983). Operating expenses comprised the costs of administrative and general (A & G), supplies, drugs (including erytropoetin—EPO costs), laboratory, and equipment and machines maintenance, which all are covered in the composite rate and are reimbursed by Medicare. The only exception is for EPO costs that are outside the composite rate but reimbursed by Medicare as separately billable expenses. Each of the cost items was measured by the sum of total costs allocated to each dialysis modality.
Independent variables in the multivariate model included market competition and a set of facility characteristics as described below.
Market competition
The Hirschman-Herfindahl index (HHI) was utilized as a measure of market competitiveness to test Hypothesis 1. The index was constructed by summing the squared market shares of all facilities in a given Metropolitan Statistical Area (MSA), or county for non-MSA facilities (Held and Pauly 1983). Market share for each facility was measured as the proportion of total dialysis treatments produced by a facility to the total number of dialysis treatments furnished by all other facilities, including hospital-based facilities, in a given market.
Facility Characteristics
A binary indicator representing dialyzer reuse was constructed to test Hypothesis 2. To test Hypothesis 3, facilities were divided into six classes, using the categories of chain organizations by which facilities were owned or managed: (1) independent, (2) affiliated with a small chain, (3) affiliated with a midsized chain, (4) affiliated with a large chain, (5) affiliated with the largest national chain (largest1), and (6) affiliated with the second largest national chain (largest2). It should be noted that since the study was unable to obtain information on chain affiliation directly from chain offices, this classification was based on the total 2,274 freestanding dialysis facilities in the 1997 IRFCRD file. Thus, assignment of facilities to categories of affiliated with small and midsized chains may have been underrepresented. Facilities were categorized into (1) for-profit facilities, (2) nonprofit facilities, and, (3) government/other facilities, to test Hypothesis 4. The cross-product term between percentage of for-profit facilities in a given market and ownership type was constructed to test Hypothesis 5. An exclusively nonprofit market was represented by a value of zero, a for-profit market by a value of one, and a mixed market by values between zero and one.
The study also included general population characteristics of age, race, education, and population density, and geographic location and ruralness, to control for differences in the market characteristics of external demand and supply across dialysis providers.
Analytical Methods
The Data Envelopment Analysis (DEA) technique was used to measure the relative technical efficiency scores of each facility. DEA is a nonparametric frontier technique used to search for optimal combinations of outputs and inputs based on the actual performance of comparable units—in this study, dialysis facilities. Application of DEA provided the current study with several advantages in comparison to previous studies of efficiency/costs in dialysis care that used regression-based techniques modeled as parametric functions (Griffiths et al. 1994; Held and Pauly 1983; Hirth et al. 1999). First, in regression-based models, estimates of a facility's efficiency are based on average output generated from a set of resources. By contrast, in DEA the maximum output that a facility should generate from a set of inputs is estimated from the best performers tracing out the frontier, which can be viewed as the appropriate benchmarking for evaluating the efficiency of facilities (Bryce, Engberg, and Wholey 2000). Facilities that lie on the best-practice frontier are assigned an efficiency score of one and are technically efficient, and all other facilities are assigned a score of less than one, but greater than zero, and are relatively technically inefficient (Cooper, Seiford, and Tone 2000). Second, unlike regression-based techniques, DEA does not make explicit assumptions about the form of the production function under investigation (i.e., parameter-free), thereby reducing potential specification error. Regression-based method, on the other hand, would be valid as long as the production function of interest is specified adequately (Grosskopf and Valdmanis 1987). The measures of efficiency used here are similar to those in previous studies of physicians, hospitals, and organ procurement organizations (Chilingerian and Sherman 1990; Ozcan and Luke 1993; Ozcan 1998; Ozcan, Begun, and McKinney 1999; Ozcan, Jiang, and Pai, 2000), so that it is reasonable to expect the efficiency measurements of the study to encompass lower specification error than those in the previous research.
Third, DEA, in comparison to regression-based techniques, is capable of evaluating the efficiency of facilities that produce multiple outputs by given multiple inputs (Cooper, Seiford, and Tone 2000). Specification of multiple outputs instead of a single output is suggested to reduce measurement error resulting from the variation in input requirements (Grosskopf and Valdmanis 1987; Kooreman 1994). However, the reduction in measurement error depends largely on the extent of within-group homogeneity or between-groups heterogeneity. Incorporating different types of dialysis modalities into common output categories, this study further investigated this issue. Hemodialysis accounted for 99.99 percent of average total outpatient dialysis treatments produced; CAPD and CCPD training treatments accounted for 69 percent and 25 percent, respectively, of the average total training treatments produced: home program CAPD and CCPD accounted for 73 percent and 24 percent, respectively, of the average total home dialysis treatments produced. Moreover, the resource consumption for each modality distributed homogeneously within specified output groups. For instance, within the dialysis training category, CAPD and CCPD dialysis training accounted for the largest drug, supply, laboratory, A & G, and maintenance costs. Thus, this study should reduce measurement error and permit the variation in case mix.
Despite all these widely recognized advantages, DEA is known to have a major weakness. In contrast to regression-based techniques, because of its deterministic nature DEA does not impose the error term in the efficiency model, and thus observed inefficiency is attributed to poor managerial decisions (Bryce, Engberg, and Wholey 2000). Thus, there may be measurement error with the efficiency measurements here because of factors such as unobserved variables.
In DEA, efficiency measurements vary by the DEA model selected and also by the model orientation (Charnes et al. 1994). Two major models identify the efficiency frontier: the constant-returns-to-scale model (CRS) and the variable-returns-to-scale (VRS) model (Cooper, Seiford, and Tone 2000). A CRS model assumes that an increase in the input(s) yields a proportional change in the output(s), whereas a VRS model assumes increasing or decreasing change in the output(s) (Norman and Stoker 1991). The two models also differ in the efficiency measure that they provide: A CRS model produces a global efficiency measure (technical and scale efficiency) whereas a VRS model yields only a pure technical efficiency measure (Banker, Charnes, and Cooper 1984). This study uses a VRS DEA model in examining the technical efficiency of dialysis facilities, assuming that the average productivity at the most productive scale size may not be attainable for the other scale sizes at which a given dialysis facility may be operating (Banker, Charnes, and Cooper 1984). Thus, the study generates only pure technical efficiency measurements of dialysis production. The type of orientation of the DEA model means specification of the type of strategy that must to be used to enhance efficiency. Since managers of dialysis facilities can be assumed to have more opportunity to reduce the inputs used to produce dialysis outputs than discretion over increases in dialysis outputs, an input-oriented model was used.
An input-oriented VRS DEA model used to compute efficiency scores can be expressed in the following linear programming problem (dual multiplier form) (adapted from Cooper, Seiford, and Tone 2000):
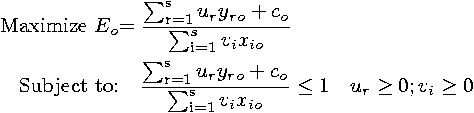 |
where Eo denotes the efficiency score for each facility in the set of o=1,…,n facilities, yro the selected output “r” produced by each facility in the set “o,” xio the selected input “i” used by each facility in the set “o,” yrj the selected output “r” produced by facility “j,” xij the selected input “i” used by facility “j.” In this formulation, ur and vi are the weights assigned respectively to output “r” and input “i,” both obtained from DEA. The constant is represented by co.
The DEA methodology assumes that facilities are to be identical with respect to organizational and environmental operating conditions (Sexton et al. 1989). Since this is not necessarily true, there may be variation in efficiency measurements across facilities with different characteristics. On the other hand, this drawback can easily be overcome by a second-stage statistical analysis in which efficiency scores derived from DEA are used to construct an index of efficiency that can serve as the dependent variable in examining the determinants of efficiency (Sexton 1986).
Multivariate logistic regression analysis was performed to analyze the probability of efficiency, using a binary dependent variable of technical efficiency to regress against the independent variables and control factors. The individual dialysis facility was the unit of analysis. To test the robustness of the model, one can alternatively conduct sensitivity analyses by altering the cutoff points of efficiency from 1 to .95, .90 and so on. Our analyses showed that the significance of the independent variables stayed at the same level until the efficiency cutoff was about .90. Hence, the predictors of efficiency are well described by the logistic regression model.
Results
Table 1 presents descriptive statistics for the variables used in the analysis of efficiency and the multivariate logistic regression. The total of outpatient treatments produced is consistent with the overall tendency of facilities to produce outpatient dialysis most, relative to dialysis training and home dialysis. The large number of nonphysician and non-RN medical staff employed, relative to the number of physicians and RNs, is the cost-cutting strategy that dialysis facilities use to reduce labor inputs and their corresponding costs. Among the operating costs included here, drug costs were the largest operating expense (35 percent of total average cost of $1,268,956.39), most of which was accounted for by EPO costs (95 percent of total drug costs). Following drug costs, an average A & G cost of $361,670 implies that substantial costs were devoted to areas other than dialysis treatment itself. Laboratory tests, on average, accounted for the least cost in the dialysis process (0.69 percent of total average cost).
Table 1.
Characteristics of Freestanding Dialysis Facilities
| Variable | Number (n=791) | Mean (%) | SD |
|---|---|---|---|
| Outputs | |||
| Outpatient dialysis | 11,595.02 | 6,612.11 | |
| Dialysis training | 105.47 | 552.56 | |
| Home dialysis | 2,285.25 | 8,848.56 | |
| Inputs | |||
| Labor inputs | |||
| Physicians | 0.23 | 1.17 | |
| Registered nurses | 7.33 | 5.27 | |
| Other medical staff | 12.89 | 8.44 | |
| Capital input | |||
| Dialysis machines | 23.03 | 10.20 | |
| Operating expenses (in $) | |||
| A&G costs | 361,670.27 | 232,002.50 | |
| Supply costs | 350,372.89 | 251,340.72 | |
| Drug costs | 444,589.45 | 291,259.80 | |
| Laboratory costs | 8,803.52 | 11,682.84 | |
| Maintenance costs | 103,520.26 | 66,849.13 | |
| Market Competition | |||
| Hirschman-Herfindahl index | 791 | 0.30 | 0.33 |
| Dialysis Facility | |||
| Reused dialyzers | 690 | (87.2) | |
| Not reused | 101 | (12.8) | |
| Not affiliated–independent | 155 | (19.6) | |
| Affiliated with small chain | 67 | (8.5) | |
| Affiliated with mid-sized chain | 52 | (6.6) | |
| Affiliated with large chain | 159 | (20.1) | |
| Affiliated with largest chain | 197 | (24.9) | |
| Affiliated with second largest chain | 161 | (20.4) | |
| For-profit | 678 | (85.7) | |
| Nonprofit | 82 | (10.4) | |
| Government/other | 31 | (3.9) | |
| % for-profits | 791 | 0.75 | 0.25 |
| Control Factors | |||
| % age 65+ | 784 | 0.13 | 0.02 |
| % African American | 784 | 0.16 | 0.15 |
| % persons <9-year education | 784 | 0.11 | 0.01 |
| Population density | 784 | 153,60.38 | 34,647.99 |
| Northeast | 120 | (15.2) | |
| South | 384 | (48.5) | |
| West | 149 | (18.8) | |
| Midwest | 131 | (16.6) | |
| Rural | 110 | (13.9) | |
| Urban | 681 | (86.1) |
The majority of the facilities reprocessed and reused hemodialyzers. Of 636 chain facilities, nearly one-fourth were members of the largest national chain, followed by members of the second largest national chain, and of large chains, small chains, and midsized chains. For-profit facilities were the largest proportion of freestanding dialysis facilities; government-owned facilities were represented least. The average degree of market competition measured by HHI was 0.30. The percentage of for-profit facilities averaged 75 percent, indicating that a nonprofit and/or government facility is operating in a local market where for-profit facilities are dominant. Specifically, the majority of the facilities in each ownership category operated in mixed-ownership markets (69 percent of the for-profit facilities, 88 percent of the nonprofit facilities, and 74 percent of the government facilities). The average profile of the general population in a freestanding dialysis facility's area can be depicted as 13 percent 65 years or older, 16 percent African-American, 11 percent with less than a 9-year education, 15,360 people per square mile in a county. A little less than one-half of the facilities are in the South, and the majority is in urban areas.
Technical Efficiency
According to the facility-specific efficiency scores derived through an input-orientated VRS DEA model, 167 facilities (21.1 percent) were classified as technically efficient. The remaining 624 facilities (78.9 percent) were classified as technically inefficient as compared to facilities on the efficiency frontier. The average efficiency score for inefficient facilities was 0.79, with a minimum efficiency of 0.33 and a maximum efficiency of 0.99, which means that inefficient providers should have been able to produce outputs using 21 percent less inputs than they did.
Factors Related to Technical Efficiency
Table 2 presents the results of the multivariate logistic regression analysis. Overall, the model fits the data well, according to goodness-of-fit statistics. The model chi-square was 83.416 with 19 degrees of freedom (p = .000). Comparing the predicted probabilities and observed responses, 80.23 percent of the facilities were correctly classified, which indicates high prediction accuracy.
Table 2.
Multivariate Logistic Regression Results (n = 784)
| Variable | Beta Coefficient | p-Value | Odds Ratio | 95% CI |
|---|---|---|---|---|
| Market Competition | ||||
| Hirschman-Herfindahl index | 0.313 | 0.442 | 1.37 | 0.62, 3.04 |
| Facility Characteristics | ||||
| Reuse | −0.086 | 0.770 | 0.92 | 0.52, 1.63 |
| Independent | Reference | |||
| Affiliated with small chain | 0.337 | 0.302 | 1.40 | 0.74, 2.66 |
| Affiliated with mid-sized chain | 0.161 | 0.681 | 1.18 | 0.55, 2.53 |
| Affiliated with large chain | −0.951 | 0.001 | 0.39 | 0.22, 0.68 |
| Affiliated with largest chain | −1.992 | 0.000 | 0.14 | 0.07, 0.27 |
| Affiliated with second largest chain | −1.053 | 0.001 | 0.35 | 0.20, 0.62 |
| For profit ownership | Reference | |||
| Nonprofit ownership | −1.721 | 0.031 | 0.18 | 0.04, 0.85 |
| Government ownership | −1.563 | 0.078 | 0.21 | 0.04, 1.19 |
| Nonprofit * % for-profits | 2.885 | 0.043 | 17.89 | 1.10, 291.16 |
| Government * % for-profits | 2.816 | 0.060 | 16.71 | 0.89, 314.21 |
| Control Factors | ||||
| Ruralness | −0.056 | 0.886 | 0.95 | 0.44, 2.02 |
| Midwest | −0.508 | 0.114 | 0.60 | 0.32, 1.13 |
| West | 0.279 | 0.337 | 1.32 | 0.75, 2.34 |
| Northeast | 0.098 | 0.766 | 1.10 | 0.58, 2.09 |
| South | Reference | |||
| % persons aged 65 + | −3.170 | 0.227 | 0.04 | 0.00, 7.21 |
| % African-American | −0.654 | 0.410 | 0.52 | 0.11, 2.46 |
| Population density | 2.484 | 0.341 | 11.99 | 0.07, 20.67 |
| % persons <9-year education | 3.727 | 0.067 | 41.57 | 0.78, 23.92 |
| Intercept | −0.535 | 0.356 | ||
| Log-Likelihood=−357.71 | ||||
| Goodness of Fit Statistic | ||||
| Chi-square (19df)=83.416 (p=0.000) | ||||
| CorrectClassificationRate=80.23% | ||||
Note: All variables were kept in the analysis regardless of their significance, in order to control confounding effects among variables as much as possible within the data set.
No support is found for Hypothesis 1: Market competition measured by HHI does not enhance technical efficiency. The parameter estimate is positive but insignificant. There is also no support for Hypothesis 2: Dialyzer reuse is not a significant determinant of efficiency in the production of dialysis outputs. Counter to Hypothesis 3, membership in large chains, in the largest national chain (largest1), and in the second largest national chain (largest2) (p = .001, p = .000, p = .001, respectively) show negative associations with efficiency, as compared to independent status. Affiliations with small and with midsized chains are positively associated with technical efficiency, but the relationships are not significant.
Hypothesis 4 receives strong support: Nonprofit ownership, as compared with for-profit facilities, is significantly and negatively associated with the probability of efficiency (p = .031). Although of marginal significance, government ownership is also significantly and negatively associated with efficiency (p = .078). In support of Hypothesis 5, the interactions between the percentages of for-profit facilities, nonprofit facilities, and government-owned facilities are positively significant predictors of technical efficiency (p = .043, p = .06, respectively). The results show that the higher the percent of for-profit facilities in a mixed market, the greater the likelihood that nonprofit and government freestanding facilities will be technically efficient.
Among control variables, estimates for only one of the variables have statistical significance. Facilities located in markets with higher percentages of people with fewer than nine years of education are more likely to be efficient at the marginal significance level (p = .067).
Discussion and Limitations
The study provides insights about the extent of technical efficiency in the production of multiple dialysis outputs and about the potential predictors of efficiency, across freestanding dialysis units operating in a nonprice competitive market. In general, facilities seem to be actively seeking and practicing the most cost-efficient ways to provide dialysis and related services. As the first study to introduce the DEA technique to the literature on dialysis, this study found substantial numbers of freestanding facilities in multiple output dialysis markets to be relatively inefficient. This may come about at least partially through the fact that DEA makes no allowance for the possibility of random noise, as pointed out previously.
According to the findings of the study, the major factors significantly associated with the level of technical efficiency are facilities' ownership form, affiliation with dialysis systems of different sizes, and operating in mixed-ownership markets. The finding of greater inefficiency from nonprofit facilities is consistent with the findings by Griffiths et al. (1994), but inconsistent with Hirth et al. (1999). To provide further insight into this issue, the study also tested the model without interaction terms and found no significant difference in efficiency among nonprofit and government-owned facilities as compared to for-profit ones.The implications of these findings apply to both the dialysis and the overall health-care industry. The effects of the growing presence of for-profit providers in health-care markets in general and dialysis markets in particular have continued to be a focus of studies. As Hirth (1997) emphasized, to make unbiased inferences about the effects of type of ownership, health-care researchers should take into account the interaction between local mixed-ownership markets and ownership form.
Although the legal ownership form itself does not improve the efficient operation of facilities, in mixed markets the relationship between ownership and efficiency is reversed, as presumed by Hirth (1997). That is, competition with for-profit facilities appears to enhance the technical efficiency of nonprofit and government providers. This may be because rivalry from for-profit facilities restricts the nonprofit facilities' competitive strategies. In this study, nonprofit units, on average, produced more outputs while using more RNs and incurring higher operating costs than the for-profit units did. We also looked at whether the behavior of nonprofit units in output production and input use varied with the ownership mix of the market. On average, nonprofit units in mixed markets produced outpatient dialysis the most, used fewer RNs, and spent more money, whereas those in nonprofit-only markets produced home dialysis the most, used more RNs, and incurred higher costs. Such a portrait of nonprofit units appears to substantiate the results of the Cleary et al. (1991) study with respect to choice of a particular dialysis mode. These results suggest that the issue of how a mixed-ownership market can affect performance indicators (e.g., efficiency, quality, and access), as areas of interest common to the entire health-care system, should receive particular attention from future research. The findings from future studies on this issue could clarify whether competition between health-care organizations with different types of ownership in local markets may provide effective incentives to improve overall provider performance.
The findings of the insignificant relationships between affiliations with both small and midsized chains confirm those from the Hirth et al. study (1999). On the other hand, unlike the previous study, the results from this study show that affiliation with large-sized chains, as compared to independent facilities, increases inefficiency for facilities that produce multiple dialysis outputs. The fact that the largest dialysis systems have more incentive to report higher costs because future Medicare payments may depend partially on nationwide averages of costs of dialysis treatment (Dor, Held, and Pauly 1992; Hirth et al. 1999) may serve as a general explanation for this inconsistent finding. Another possible reason may be that being part of large-sized chains does not actually contribute efficiently to joint production of dialysis outputs. In summary, the absence of enhanced efficiency through involvement in any type of chain suggests that growing consolidation in the dialysis industry may not be the strategy to enhance technical efficiency in the production of multiple dialysis outputs.
In the face of nonprice competition, external pressure from competition does not provide incentives for freestanding facilities to operate efficiently. This finding is not consistent with the finding from the Held and Pauly study (1983), which found increasing efficiency as competition increases. One major reason for this inconsistency is that the previous study used data from the late 1970s. The second reason may be the methodology employed in the previous study, which used a traditional regression technique to examine efficiency in the production of a single variable: total number of dialysis outputs.
Reusing dialyzers does not reduce facilities' costs and does not enhance the level of technical efficiency in the production of multiple dialysis outputs. A comparison of facilities' operating costs showed that facilities that reused dialyzers had no cost advantages over those that did not, particularly in supply costs. This may be due to the reuse of higher-cost dialyzer membranes. As pointed out by Hirth et al. (1999), when expensive dialyzers are used, the savings from the reuse may not be sufficient to recover the higher supply costs for the expensive dialyzers.
The study has several limitations. First, it is limited in its generalizability by sample selection bias. Because we were able to include only Medicare-approved freestanding dialysis units that submitted cost report forms to HCFA, the results from the study may not be generalizable to the entire population of freestanding dialysis facilities. Second, the study cannot make causal inferences about relations among the study variables because of the use of a cross-sectional study design.
Third, although the findings of the study provide useful information on the issue of interest, the results should be interpreted cautiously. A facility may have been deemed efficient through providing a lower quality of care. For example, this study found that RN employment, a structural measure of the quality of dialysis care (Held et al. 1990), was statistically significantly lower in the efficient facilities than in their inefficient counterparts. However, since the study did not capture the explicit process or outcome measures for quality, differences found in efficiency across units may not necessarily indicate that efficient facilities produced their quality–quantity output mix by using minimum inputs, but rather may show an unobserved variable bias. Therefore, how efficiency is achieved in a nonprice-competitive dialysis market while nevertheless maintaining quality remains a prominent issue. Measures such as mortality rates, hospitalization rates, adequacy of dialysis, and the quality of life of people who undergo dialysis should be included in an efficiency analysis if differences in the quality care in the production of dialysis outputs are to be ruled out.
A final limitation is the absence of measures to adjust for variability in case mix across facilities. Since this study examined a homogenous study sample of facilities that produce basically one type of output (dialysis treatments) to patients with the same disease (chronic renal failure), and used the DEA technique that allows reduction in the variation in case mix, incorporation of case-mix variables in the efficiency model may be considered less necessary. Indeed, this presumption is further supported by the existing dialysis-related research. For example, the Griffiths et al. study (1994) found only African-American identity to be a significant variable in the efficiency model. In addition, evaluating the effects of inclusive case-mix measures on facility costs, Hirth and his colleagues (1999) revealed that most case-mix measures showed no statistically significant associations with dialysis costs. However, all the reasonable presumptions and empirical support may still not free the results in this study from being biased. It is worth noting that the insignificant relationship between case mix and efficiency/cost in dialysis that has been found in previous research may either be true or reflect the failure to include sufficient case-mix variables. To elucidate this issue, future study should analyze efficiency in dialysis with more comprehensive case-mix measures.
Notes
In the IRFCRD file, a total of 1,090 facilities were identified as those that produced more than one dialysis output. We included only three-output facilities because the technique used to measure efficiency is sensitive to zeros. Two hundred fifty facilities out of 1,090 facilities were two-output producers of dialysis, indicating zero-output values for approximately one-fourth of facilities and potential inefficiency for such units. To elaborate this, we also evaluated efficiency with a total sample of 1,041 (791+250=1,041) and found a 3 percent difference in the number of efficient units between the two models.
References
- Banker RD, Charnes A, Cooper WW. “Some Models for Estimating Technical and Scale Inefficiencies in Data Envelopment Analysis.”. Management Science. 1984;30(9):1078–92. [Google Scholar]
- Bovbjerg RR, Held PJ, Diamond LH. “Provider-Patient Relations and Treatment Choice in the Era of Fiscal Incentives: The Case of the End-Stage Renal Disease Program.”. Milbank Quarterly. 1987;65(2):177–202. [PubMed] [Google Scholar]
- Bryce CL, Engberg JB, Wholey DR. “Comparing the Agreement Among Alternative Models in Evaluating HMO Efficiency.”. Health Services Research. 2000;35(2):509–28. [PMC free article] [PubMed] [Google Scholar]
- Burns J. “Dialysis Providers Cope with Dwindling Reimbursement.”. Modern Healthcare. 1992:56–7. [PubMed] [Google Scholar]
- Charnes A, Cooper WW, Lewin AY, Seiford LM. Data Envelopment Analysis: Theory, Methodology, and Applications. Boston: Kluwer Academic Publishers; 1994. [Google Scholar]
- Chilingerian J, Sherman DH. “Managing Physician Efficiency and Effectiveness in Providing Hospital Services.”. Health Service Management Research. 1990;3(1):3–15. doi: 10.1177/095148489000300101. [DOI] [PubMed] [Google Scholar]
- Cleary PD, Schlesinger M, Blumental D. “Factors Affecting the Availability and Use of Hemodialysis Facilities.”. Health Care Financing Review. 1991;13(2):49–55. [PMC free article] [PubMed] [Google Scholar]
- Cooper WW, Seiford LM, Tone K. Data Envelopment Analysis: A Comprehensive Text with Models, Applications, References, and DEA-Solver Software. Boston: Kluwer Academic Publishers; 2000. pp. 87–90. [Google Scholar]
- Dor A, Held PJ, Pauly M. “The Medicare Costs of Renal Dialysis: Evidence from a Statistical Cost Function.”. Medical Care. 1992;30(10):879–91. doi: 10.1097/00005650-199210000-00001. [DOI] [PubMed] [Google Scholar]
- Farley DO. “Effects of Competition on Dialysis Service Levels and Patient Selection.”. Doctoral dissertation Rand Graduate School Santa Monica. 1993 [Google Scholar]
- Farley DO. “Financing of End-Stage Renal Disease Care: Past, Present, and Future.”. Advances in Renal Replacement Therapy. 1994;1(1):24–31. doi: 10.1016/s1073-4449(12)80019-7. [DOI] [PubMed] [Google Scholar]
- Farley DO. “Competition under Fixed Prices: Effects on Patient Selection and Service Strategies by Hemodialysis Providers.”. Medical Care Research and Review. 1996;53(3):330–49. doi: 10.1177/107755879605300307. [DOI] [PubMed] [Google Scholar]
- Feldman HI, Kinosian M, Bilker WB, Simmons C, Holmes JH, Pauly MV, Escarce JJ. “Effect of Dialyzer Reuse on Survival of Patients Treated with Hemodialysis.”. Journal of the American Medical Association. 1996;276:620–5. [PubMed] [Google Scholar]
- Fox MP. “Facility Reimbursement: A Critical Comparison between Hemodialysis and Peritoneal Dialysis.”. American Journal of Kidney Diseases. 1993;22(2):32–4. doi: 10.1016/0272-6386(93)70179-3. [DOI] [PubMed] [Google Scholar]
- Garg PP, Frick KD, Marie DW, Powe NR. “Effect of the Ownership of Dialysis Facilities on Patients' Survival and Referral for Transplantation.”. New England Journal of Medicine. 1999;341(22):1653–60. doi: 10.1056/NEJM199911253412205. [DOI] [PubMed] [Google Scholar]
- Griffiths RI, Powe NR, Gaskin DJ, Anderson GF, de Lissovoy GV, Whelton PK. “The Production of Dialysis by For-Profit versus Not-For-Profit Freestanding Renal Dialysis Facilities.”. Health Services Research. 1994;29(4):473–87. [PMC free article] [PubMed] [Google Scholar]
- Grosskopf S, Valdmanis VG. “Measuring Hospital Performance: A Non-Parametric Approach.”. Journal of Health Economics. 1987;6:89–107. doi: 10.1016/0167-6296(87)90001-4. [DOI] [PubMed] [Google Scholar]
- Growth in the ESRD Provider Market. Nephrology News & Issues. 1998:19. [Google Scholar]
- Health Care Financing Administration. National Listing of Medicare Providers Furnishing Kidney Dialysis and Transplant Services. Washington DC: Health Care Financing Administration; 1999. pp. 5–5. [Google Scholar]
- Held PJ, Wolfe RA, Gaylin DS, Port FK, Levin NW, Turenne MN. “Analysis of the Association of Dialyzer Reuse Practices and Patient Outcomes.”. American Journal of Kidney Diseases. 1994;23(5):692–708. doi: 10.1016/s0272-6386(12)70280-9. [DOI] [PubMed] [Google Scholar]
- Held PJ, Pauly MV. “Competition and Efficiency in the End Stage Renal Disease Program.”. Journal of Health Economics. 1983;2:95–118. doi: 10.1016/0167-6296(83)90001-2. [DOI] [PubMed] [Google Scholar]
- Held PJ, Pauly MV, Diamond L. “Survival Analysis of Patients Undergoing Dialysis.”. Journal of the American Medical Association. 1987;257(5):645–50. [PubMed] [Google Scholar]
- Held PJ, Garcia JR, Pauly MV, Cahn MA. “Price of Dialysis, Unit Staffing, and Length of Dialysis Treatments.”. American Journal of Kidney Diseases. 1990;15(5):441–50. doi: 10.1016/s0272-6386(12)70362-1. [DOI] [PubMed] [Google Scholar]
- Hirth RA, Held PJ, Orzol SM, Dor A. “Practice Patterns, Case Mix, Medicare Payment Policy, and Dialysis Facility Costs.”. Health Services Research. 1999;33(6):1567–92. [PMC free article] [PubMed] [Google Scholar]
- Hirth RA. “Competition Between For-Profit and Nonprofit Health Care Providers: Can It Help Achieve Social Goals?”. Medical Care Research and Review. 1997;54(4):414–38. doi: 10.1177/107755879705400402. [DOI] [PubMed] [Google Scholar]
- Hirth RA, Chernew ME. “Adoption of New Technologies and Cost-Saving Practices in a Fixed Price Environment.”. Abstract Book for Association of Health Services Research. 1997;14:127. [Google Scholar]
- Iglehart JK. “The American Health Care System: End Stage Renal Disease Program.”. The New England Journal of Medicine. 1993;328(5):366–71. doi: 10.1056/NEJM199302043280528. [DOI] [PubMed] [Google Scholar]
- Joskow PL. “The Effects of Competition and Regulation on Hospital Bed Supply and Reservation Quality of the Hospital.”. The Bell Journal of Economics. 1980;11:421–47. [Google Scholar]
- Kendix M. “Dialysis Modality Selection among Patients Attending Freestanding Dialysis Facilities.”. Health Care Financing Review. 1997;18(4):3–21. [PMC free article] [PubMed] [Google Scholar]
- Kooreman P. “Data Envelopment Analysis and Parametric Frontier Estimation: Complementary Tools.”. Journal of Health Economics. 1994;13:345–6. [Google Scholar]
- Levinsky NG. “The Organization of Medical Care: Lessons from the Medicare End-Stage Renal Disease Program.”. New England Journal of Medicine. 1993;329(19):1395–9. doi: 10.1056/NEJM199311043291907. [DOI] [PubMed] [Google Scholar]
- Mason SA. “Greater Access, Lower Costs with Multi-Hospital Systems.”. Hospital Financial Management. 1980;10(4):56–64. [PubMed] [Google Scholar]
- Maxwell JH, Sapolsky HM. “The First DRG: Lessons from the End Stage Renal Disease Program for the Prospective Payment System.”. Inquiry. 1987;24:57–67. [PubMed] [Google Scholar]
- Nissenson AR, Rettig RA. “Medicare's End-Stage Renal Disease Program: Current Status and Future Prospects.”. Health Affairs. 1999;18(1):161–79. doi: 10.1377/hlthaff.18.1.161. [DOI] [PubMed] [Google Scholar]
- Norman M, Stoker B. Data Envelopment Analysis: The Assessment of Performance. New York: Wiley; 1991. [Google Scholar]
- Ozcan YA. “Physician Benchmarking: Measuring Variation in Practice Behavior in Treatment of Otitis Media.”. Health Care Management Science. 1998;1(1):5–17. doi: 10.1023/a:1019026114859. [DOI] [PubMed] [Google Scholar]
- Ozcan YA, Begun JW, McKinney MM. “Benchmarking Organ Procurement Organizations (OPOs): A National Study.”. Health Services Research. 1999;34(4):853–72. [PMC free article] [PubMed] [Google Scholar]
- Ozcan YA, Jiang HJ, Pai CW. “Physician Efficiency in Treatment of Sinusitis: Do Primary Care Physicians or Specialists Provide More Efficient Care?”. Health Services Management Research. 2000;13(2):90–6. doi: 10.1177/095148480001300203. [DOI] [PubMed] [Google Scholar]
- Ozcan YA, Luke RD. “A National Study of the Efficiency of Hospitals in Urban Markets.”. Health Services Research. 1993;28(6):719–39. [PMC free article] [PubMed] [Google Scholar]
- Ogden DA, Friedl MM. “Simultaneous Reprocessing of Hollow Fiber Dialyzers and Blood Tubing Sets for Multiple Use.”. Dialysis Transplant. 1984;13:366–75. [Google Scholar]
- Plough AL, Salem SR, Schwartz JM, Ferguson CW. “Case Mix in the End Stage Renal Disease: Differences between Patients in Hospital-Based and Freestanding Treatment Facilities.”. New England Journal of Medicine. 1984;310(22):1432–6. doi: 10.1056/NEJM198405313102205. [DOI] [PubMed] [Google Scholar]
- Port FK, Wolfe RA, Held PJ. “Ownership of Dialysis Facilities and Patients' Survival.”. New England Journal of Medicine. 2000;342(14):1053. doi: 10.1056/NEJM200004063421415. [DOI] [PubMed] [Google Scholar]
- Radecki SE, Mendenhall RC, Nissenson AR, Freeman RB, Blagg CR, Capelli JP, Gentile DE, Feinstein EI. “Case-mix and Treatment in End-stage Renal Disease: Hemodialysis versus Peritoneal Dialysis.”. American Journal of Kidney Diseases. 1988;11(1):7–14. doi: 10.1016/s0272-6386(88)80167-7. [DOI] [PubMed] [Google Scholar]
- Rettig RA. “The Social Contract and the Treatment of Permanent Kidney Failure.”. Journal of the American Medical Association. 1996;275(14):1123–6. [PubMed] [Google Scholar]
- Rettig RA, Levinsky NG. Kidney Failure and the Federal Government. Washington DC: National Academy Press; 1991. [PubMed] [Google Scholar]
- Robinson JC, Luft HS. “The Impact of Hospital Market Structure on Patient Volume, Average Length of Stay, and Cost of Care.”. Journal of Health Economics. 1985;4:333–56. doi: 10.1016/0167-6296(85)90012-8. [DOI] [PubMed] [Google Scholar]
- Scherer FM. Industrial Market Structure and Economic Performance. Chicago: Rand McNally; 1980. [Google Scholar]
- Schlesinger M, Cleary PD, Blumental D. “The Ownership of Health Facilities and Clinical Decisionmaking The Case of the ESRD Industry.”. Medical Care. 1989;27(3):244–57. doi: 10.1097/00005650-198903000-00003. [DOI] [PubMed] [Google Scholar]
- Sexton TR, Silkman RH. Measuring Efficiency: An Assessment of Data Envelopment Analysis New Directions for Program Evaluation. Vol. 32. San Francisco: Jossey-Bass; 1986. “Methodology of Data Envelopment Analysis”; pp. 7–29. [Google Scholar]
- Sexton T, Leiken A, Nolan A, Liss S, Hogan A, Silkman RH. “Evaluating Managerial Efficiency of Veterans Administration Medical Center Using Data Envelopment Analysis.”. Medical Care. 1989;27(12):1175–89. doi: 10.1097/00005650-198912000-00009. [DOI] [PubMed] [Google Scholar]
- Tirole J. The Theory of Industrial Organization. Cambridge MA: MIT Press; 1988. [Google Scholar]
- United States Renal Data System 1999 Annual Data Report. National Institute of Diabetes and Digestive and Kidney Diseases. Bethesda MD: National Institutes of Health; 1999. [Google Scholar]
- Wilson GW, Jadlow JM. “Competition, Profit Incentives, and Technical Efficiency in the Provision of Nuclear Medicine Services.”. The Bell Journal of Economics. 1982:472–82. [Google Scholar]
- Zuckerman HS. “Multi-Institutional Systems: Promise and Performance.”. Inquiry. 1979;16(4):291–314. [PubMed] [Google Scholar]


