Abstract
Objective
To test whether there is an association between hospital operating conditions such as average length of stays (LOS) and staffing ratio, and elderly patients' risk of readmission.
Data Sources
The main data source was a national patient database of admissions to all acute-care Norwegian hospitals during the year of 1996.
Study Design
It is a cross-sectional study, where Cox' regression analysis was used to test the factors acting on the probability of early unplanned readmission (within 30 days), and later occurring ones. The principal hospital variables included average hospital LOS and staffing ratio (discharges per man-years of personnel). Adjusting patient variables in the model included age, gender, and cost-weights of the Diagnosis Related Groups (DRGs).
Data Extraction Methods
The selected material included discharges from 59 hospitals, and 113,055 elderly patients (≥67 years). Multiple admissions to the same hospital were linked together chronologically, and additional hospital data were matched on. To maximize the association between the index stay and the defined outcome (unplanned readmission), no intervening planned admission was accepted.
Principal Findings
Being admitted to a hospital with relatively short average LOS increased the patient's risk of early readmission significantly. In addition it was found that more intensive care (more staff) could have a compensatory effect. Furthermore, the predictive factors were shown to be time dependent, as hospital variables had much less impact on readmissions occurring late (within 90–180 days).
Conclusions
The results give support to the assumption of a link between hospital operating conditions and patient outcome.
Keywords: Patient readmission, outcome assessment (health care), multivariate analysis, hospitals
Hospitals are faced with an environment of changing policies, resources, and expectations. In recent years the main focus has been upon productivity and cost-containment. This has been a widely distributed trend, acting across differently organized and financed health-care systems. There has been a rising concern that the pressure to increase the productivity might have negative consequences for the patients, or for particularly susceptible groups. In this study the objective was to analyze the association between the hospitals' operating conditions and practice and the patients' outcome, measured as the risk of early readmission.
Methodologically it is essential to ensure valid links between the processes and structures of care and the patients' outcomes (Hammermeister et al. 1995). When using readmission as the outcome measure, the primary question will be if there is a link to the prior hospital stay (Ashton and Wray 1996). A meta-analysis examining the empirical evidence for such a link concluded that early readmission was significantly associated with the medical-care process during the hospital stay (Ashton et al. 1997). The finding of a link to the process was also the result from two studies examining specific conditions for the relationship of readmission to quality of care (Slack and Bucknall 1997; Weissman et al. 1999).
Following the assumption that readmission trends are affected by changes in hospital processes and structures of care, it will be of interest to observe the development of readmission rates over time. Analyses of readmission trends have frequently been used in evaluations of the effects of financial incentives and constraints on the health-care system (Brownell, Roos, and Burchill 1999; Epstein et al. 1991). Studies of readmission in Norway have shown a trend toward steadily increasing rates of early unplanned readmissions in the 1990s (Heggestad and Lilleeng 1995; Magnussen and Kalseth 1998). A parallel tendency has been a decrease in the lengths of hospital stays, where the average LOS in 1996 was 6.4 days. Both these trends have been particularly pronounced for elderly patients.
One of the main challenges facing the hospitals is that the high patient turnover with increasingly shorter stays may affect the quality of care. In practice hospitals have to find strategies to balance between many different and often conflicting demands. The care for inpatients and the planning of their discharge must be balanced against the pressure to admit new patients. Clearly, shortening the lengths of stays and using the bed and personnel resources more efficiently are ways to achieve high patient turnover. It is reasonable to assume that such operating conditions will affect the delivery of care, and the decisions and priorities made. The resources have to be distributed among an increasing number of patients. Some types of tasks may be more easily marginalized. Planning of aftercare and cooperation with the patients' community and the primary health care givers might get a lower priority. Such tendencies would make the elderly patients particularly susceptible for negative consequences.
The aim of this study was to assess the consequences of the hospitals' practice patterns and operating conditions. The primary objective was to analyze whether there is an association between hospital factors indicative of the drive toward high efficiency, and the patients' probability of having an early unplanned readmission. We also wanted to test if the effect of the prior hospital stay is decreasing with time since discharge. As it was assumed that elderly patients are particularly affected, they were the selected study group.
Material and Methods
Patient Material and Hospital Data
The main data source was a national database of discharges from acute-care Norwegian hospitals. In the Norwegian public health-care system the population is covered by local general hospitals where each hospital has an assigned catchment area. There also is a superimposed hierarchy of specialization among the general acute-care hospitals, with regional or university hospitals on top. All such acute-care hospitals were included in the material, excluding other hospitals with more limited and specialized functions.
From the resulting material of 59 acute-care hospitals all elderly patients (67 years of age or older) with one or more hospital stay in the fiscal year of 1996 were extracted. Admissions to psychiatric and rehabilitation departments were excluded, as were specialized departments for diseases of the eye and ear-nose-throat. Patients dying during the index or first hospital stay were excluded. Since it is reported to be a common practice to give cancer patients an arrangement of so-called “open return,” making it difficult to categorize their readmissions as unplanned or not, this group was excluded. The admissions of included patients were classified as emergent or not, as registered in the hospital database. Unplanned readmissions were chosen as the outcome measure, operationalized as emergent ones.
If the patient returned to the same hospital during the year, successive stays were linked together chronologically. The first occurring stay of the year was regarded as the index admission. The pattern of interest was defined if an unplanned admission followed in the chosen time interval after the discharge from the index stay. To maximize the association between the index stay and the defined “positive” outcome, no intervening planned admission was accepted. A readmission was not allowed to reappear as a new index admission. Accordingly, following such definitions each patient was only represented once, either by a single admission or by a pair of admission and successive unplanned readmission.
Only readmissions to the same hospital were observed and counted in our material. In general, we have reason to believe that the proportion of readmitted patients returning to the same hospital is high in Norway. The assumption is based on a supplementary analysis of a subpopulation finding that 95 percent of the unplanned early readmissions occurred to the same hospital as the index admission. This analysis was made possible by access to a person-identified regional database that also enabled identification of readmissions to other hospitals.
The Model and Its Variables
There are multiple factors affecting the patients' probability of readmission, so a multivariate model was constructed. Three main dimensions of influence can be outlined: patient, hospital, and community characteristics. Since the primary study factors were the hospitals' operating conditions, additional hospital data (Kalseth, Solstad, and Rønningen 1997) were matched to the patient datafile so that the index admission of patients discharged from the same hospital were given the same values of the variables. These data on the hospital operating conditions were measures that reflected the average hospital status through the year 1996.
We assumed two main hospital strategies to achieve a relatively high “output” or patient turnover: to have short lengths of stay and to distribute the personnel resources among a high number of patients. These variables were assumed to affect the process and delivery of care, and thus also to have an impact on the patients' probability of readmission. One may also assume that more intensive care could compensate for potentially negative effects of short stays. Having taken the relative quantity of personnel into account, the costs per admission were regarded as a proxy for supplementary ways of applying more intensive care. These main hospital variables were operationalized as the hospital's relative length of stay (average LOS), the staffing ratio (the number of discharges per man-years of personnel), and the costs per admission. As the hospital patient population also affects the measure of these variables, they were adjusted for differences in hospital case-mix. The adjustments were performed using the Diagnosis Related Groups (DRG)-system1, and the relative mean cost-weights of the hospital patient population. For the average LOS, the observed value was related to that expected from the hospital's mix of DRGs and their national average LOS. The type of hospital or level of specialization was also seen as a relevant adjusting factor, assuming the more specialized ones to have more severely ill patients or being more competent. Furthermore, the standardized emergency admission rate of the population in the hospital's catchment area was included to adjust for differences in (re)admission threshold. A standardized measure was estimated as the observed number of emergency admissions per inhabitant related to the expected number, which was calculated from the national average distributed onto their corresponding age and gender strata of the area population. Table 1 lists the main hospital variables.
Table 1.
Categories and Definitions of the Main Hospital Variables Used in the Model
| Scale (quartiles) | Index of Average Hospital LOS§ | Staffing Ratio§§ | Costs per Admission§§§ | Stand. Emerg. Admission Rate§§§§ |
|---|---|---|---|---|
| 1 | 0.824–0.959 | 9.9–13.7 | 17,161–21,380 | 80–93 |
| 2 | 0.960–0.995 | 13.8–14.9 | 21,381–22,414 | 94–99 |
| 3 | 0.996–1.059 | 15.0–16.9 | 22,415–23,754 | 110–106 |
| 4 | 1.060–1.215 | 17.0–21.5 | 23,755–35,230 | 107–143 |
The index reflects a relative measure of average hospital LOS adjusted for differences in patient-population by way of DRGs and the DRG-specific average lengths of stay. The value of 1 represents the national average.
Defined as the annual number of discharges/(man-years of personnel x 365). Adjusted for differences in patient-population by way of DRG and cost-weights.
Costs in NOK per hospital admission, adjusted for differences in patient-population by way of DRG and cost-weights.
An index reflecting the relative number of emergency admissions in the hospital's capture area, (the observed number × 100)/the expected number, (indirectly calculated from the national averages given the age and gender distribution of the area population).
Patient characteristics are strong predictors of readmission. Patient information such as age and gender were included in the modelling as adjusting variables, as were the cost-weights of the patients' DRGs. The cost-weights were assumed to act as a proxy for the type and complexity of illness. To account for differences in severity within a specific DRG, using the conditioned length of the patient's index stay was considered. The observed patient LOS was related to the reference national distribution of the lengths of stays for each specific DRG. Information about type of DRG (medical or surgical), and whether the index admission was emergent or not, was included to further account for differences in patient type of illness and accordingly differences in probability of readmission. Whether the patient was discharged home or to another institution was also assumed to influence the probability of readmission, as was the distance to the hospital. Living near a hospital was defined as those patients living in a municipality with a hospital.
The number of cases or patients included in the final model was 113,055, after 1,050 cases had been excluded for missing data on any of the variables. Fifty-six percent of the patients were women, and patients living in all of the 435 Norwegian municipalities were included. The most frequently occurring DRGs of the index stays were circulatory disorders (DRG 14, 122, and 140), digestive disorders (DRG 183), and procedures of the hip/femur (DRG 211).
Defining Time Intervals
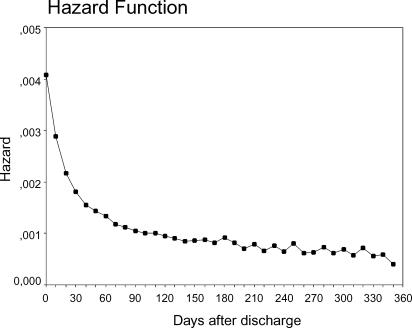
In preparing readmission as a valid measure of outcome, one has to decide what time interval from discharge to observe. A time interval of one month between admission and readmission is commonly used (Ashton and Wray 1996; Chambers and Clarke 1990; Sibbritt 1995). To analyze the distribution of readmissions by time for the study material, the hazard function for emergency readmissions was computed (Figure 1) (SPSS Inc. 1997). It seems as if the occurrence of emergency readmissions levels off or stabilizes after about a month.
Figure 1.
The hazard function of readmissions according to the time interval since discharge
It was assumed that choosing a relatively short interval of time between the discharge and the readmission would strengthen the probability of demonstrating a link with the prior hospital care. Choosing 30 days as the time interval seemed to be a reasonable compromise combining the conditions of a short interval and including a relatively large proportion of the readmissions.
Furthermore, we wanted to test more directly if the effect of the prior hospital stay varied with the time interval since discharge. Accordingly a comparison between early and late readmission was carried out, where readmission within 90–180 days after the index stay was chosen as a secondary outcome indicator.
Having chosen the observation periods, the patients' time at risk of having an unplanned readmission could be calculated. The time at risk was counted from the discharge until the occurrence of a readmission, or until the end of the observation period, or alternatively until the end of the year in the cases that this interval was shorter than the chosen observation period. For example, in the case of a chosen interval of 90–180 days, the patients with an unplanned (or planned) readmission within 30 days would be censored at this time, and not counted as having a “positive” outcome. But the case would be included in the risk population for a period of 30 days. In this way it was possible to maximize the link between the index stay and the defined readmission, and the time-window effect present in our one-year material was accounted for.
Modelling Method
The multivariate statistical modelling was performed by Cox' regression analysis (Kleinbaum 1996; Stata Corp. 1999). The proportional hazard assumption, (multiplicative model), was assessed by plotting log–log survival curves to consider the parallellity. This criterion for using Cox' regression analysis was found to be met. Adjusted hazard functions were estimated. The results of the log-likelihood tests were used to compare different models. P-values below 0.05 were considered to indicate statistical significance.
Because there was no reason to assume a linear relationship between the predictors and the effect measure, categorical variables were generally used. To achieve a scaling of a continuous variable, the values were classified in four different categories according to their distribution in percentiles. A value being lower than the twenty-fifth percentile gave a category of 1, while being above the seventy-fifth percentile gave a category of 4. Generally the first category was chosen as the reference in the model. The main hospital variables are further specified in Table 1.
The variables were entered into the model on the basis of the theoretical assumptions of relevance discussed earlier in the section. In the analyses no variables were dropped due to colinearity. Testing for interaction between variables was performed, both between different hospital variables, and between hospital and patient variables.
There was a clustering effect present because patients admitted to the same hospital were represented by identical values of the hospital variables. As a result the observations could not be considered independent. The use of estimators based on such an assumption may give too small standard errors. To adjust the model estimates for the clustering effect, an alternative and more robust way of calculating standard errors was applied (Lin and Wei 1989; Stata Corp. 1999).
Results
Early Readmissions (within 30 Days)
The results from the multivariate modelling of early readmissions are shown in Table 2. The hypothesis of an association between hospital operating conditions and the probability of early readmission was supported. Admissions to hospitals with the highest relative length of stay were found to give a significantly lower hazard of early readmission (HR 0.87 [95 percent CI=0.80, 0.94]). A low patient–staff ratio did show a tendency toward reducing the patient's risk of early readmission, while admission to a hospital with relatively higher costs per case did not show a clear compensatory effect. The standardized emergency admission rate was also found to have some effect, while the level of specialization of the hospitals turned out to be a nonsignificant factor.
Table 2.
Results from Modelling of Hazard for Unplanned Readmissions within 30 Days after Discharge. Cox' Regression Analysis, with Adjustment for Clustering Effects.§ 113,055 Patients Were Included, of these 9,692 Were Readmitted
| Statistics | |||
|---|---|---|---|
| Hazard Ratio | |||
| Variables§§ | (95% CI) | z or(χ2)§§§ | p |
| Hospital practice | |||
| Index of hospital LOS§§§§ | (23.88, 3 df | <0.0001) | |
| 1 | 1.00 | ||
| 2 | 1.10 (1.02, 1.20) | 2.33 | 0.020 |
| 3 | 0.89 (0.81, 0.96) | −2.79 | 0.005 |
| 4 | 0.87 (0.80, 0.94) | −3.34 | 0.001 |
| Staffing ratio§§§§§ | (31.32, 3 df | <0.0001) | |
| 1 | 1.00 | ||
| 2 | 1.14 (1.06, 1.23) | 3.42 | 0.001 |
| 3 | 1.21 (1.12, 1.31) | 4.67 | <0.0001 |
| 4 | 1.00 (0.89, 1.13) | 0.05 | 0.961 |
| Costs per admission | (10.06, 3 df | 0.018) | |
| 1 | 1.00 | ||
| 2 | 1.12 (1.01, 1.25) | 2.16 | 0.031 |
| 3 | 0.98 (0.88, 1.09) | −0.39 | 0.695 |
| 4 | 1.06 (0.96, 1.16) | 1.18 | 0.239 |
| Stand. emerg. admission rate | (6.12, 3 df | 0.106) | |
| 1 | 1.00 | ||
| 2 | 1.00 (0.92, 1.08) | −0.01 | 0.993 |
| 3 | 1.10 (1.01, 1.20) | 2.13 | 0.034 |
| 4 | 1.05 (0.96, 1.15) | 1.02 | 0.310 |
| Specialization of hospital | (2.70, 2 df | 0.259) | |
| Regional | 1.00 | ||
| County | 0.96 (0.89, 1.04) | −1.05 | 0.294 |
| Local | 1.02 (0.94, 1.10) | 0.40 | 0.690 |
| Patient factors | |||
| Age | |||
| 67−80 years | 1.00 | ||
| >80 years | 1.09 (1.02, 1.15) | 2.74 | 0.006 |
| Gender | |||
| Female | 1.00 | ||
| Male | 1.18 (1.14, 1.22) | 8.80 | <0.0001 |
| Type of index admission | |||
| Elective | 1.00 | ||
| Emergent | 1.91 (1.78, 2.05) | 17.94 | <0.0001 |
| Medical or surgical DRG | |||
| Surgical | 1.00 | ||
| Medical | 1.27 (1.17, 1.37) | 5.73 | <0.0001 |
| Cost-weight of the patient's DRG | (246.38, 3 df | <0.0001) | |
| 1 | 1.00 | ||
| 2 | 1.34 (1.25, 1.43) | 8.25 | <0.0001 |
| 3 | 1.61 (1.52, 1.72) | 15.07 | <0.0001 |
| 4 | 1.24 (1.15, 1.33) | 5.78 | <0.0001 |
| Discharge destination | |||
| To another institution | 1.00 | ||
| Home | 1.03 (0.94, 1.13) | 0.62 | 0.534 |
| Living near hospital | |||
| No | 1.00 | ||
| Yes | 1.31 (1.23, 1.40) | 8.16 | <0.0001 |
The summary results of the model were: log likelihood =−111284.4, Wald χ2(23)=2306.7.
For category-variables scaled into four groups, each category represents one quartile of the distribution, see also Table 1. To unify the format of category-variables, those formatted in quartiles were all kept as four categories even if a simplification seems reasonable.
The overall effect of category-variables was tested using repeated (aggregated) tests (χ2).
The index reflects a relative measure of average hospital LOS adjusted for differences in patient-population by way of DRGs and DRG-specific average LOS.
Defined as the annual number of discharges/(man-years of personnel × 365). Adjusted for differences in patient-population by way of DRG and cost-weights.
As to patient variables, both age and gender had significant effects, with men having a HR of 1.18 compared to women, and those older than 80 years an HR of 1.09 relative to the younger ones. Variables reflecting or adjusting for the type and severity of disease were all significant: such as the cost-weight of the DRG, whether the disease was classified in a surgical or nonsurgical DRG, and whether the index admission was an emergency one. Furthermore, living near to a hospital was found to give an HR of 1.31 relative to those living more distantly, while being discharged home or to another institution showed no significant difference.
Late Readmissions (within 90-180 Days)
The results of Cox' regression analysis with this later time interval are listed in Table 3. Compared to the results from the analysis of early readmissions, there were some fundamental differences. The effect of the hospital variables characterizing the index stay was much greater for early readmission. This is in accordance with our assumption; the impact of the prior admission is decreasing with the time interval since discharge. The conclusion is that a time dependency exists between the predictive factors and the occurrence of readmission.
Table 3.
Results from Modelling of Hazard for Late Readmissions (90-180 Days after Discharge). Cox' Regression Analysis, with Adjustment for Clustering Effects.§) 113,055 Patients Were Included, of these 4,892 Were Readmitted in the Period
| Hazard Ratio | |||
|---|---|---|---|
| Variables§§ | (95% CI) | z or(χ2)§§§ | p |
| Hospital practice | |||
| Index of hospital LOS§§§§ | (3.18, 3 df | 0.365) | |
| Staffing ratio§§§§§ | (2.35, 3 df | 0.502) | |
| Costs per admission | (2.35, 3 df | 0.504) | |
| Stand. emerg. admission rate | (9.35, 3 df | 0.025) | |
| 1 | 1.00 | ||
| 2 | 0.98 (0.88, 1.09) | −0.43 | 0.664 |
| 3 | 1.13 (0.99, 1.28) | 1.85 | 0.064 |
| 4 | 1.09 (0.97, 1.22) | 1.44 | 0.150 |
| Specialization of hospital | (8.28, 2 df | 0.016) | |
| Regional | 1.00 | ||
| County | 1.13 (1.02, 1.26) | 2.27 | 0.023 |
| Local | 1.12 (1.03, 1.21) | 2.64 | 0.008 |
| Patient factors | |||
| Age | |||
| 67–80 years | 1.00 | ||
| >80 years | 1.21 (1.13, 1.30) | 5.54 | <0.0001 |
| Gender | |||
| Female | 1.00 | ||
| Male | 1.04 (0.97, 1.11) | 1.17 | 0.240 |
| Type of index admission | |||
| Elective | 1.00 | ||
| Emergent | 1.51 (1.38, 1.64) | 9.38 | <0.0001 |
| Medical or surgical DRG | |||
| Surgical | 1.00 | ||
| Medical | 1.46 (1.31, 1.63) | 6.91 | <0.0001 |
| Cost-weight of the patient's DRG | (32.63, 3 df | <0.0001) | |
| 1 | 1.00 | ||
| 2 | 1.13 (1.04, 1.21) | 3.08 | 0.002 |
| 3 | 1.24 (1.15, 1.34) | 5.64 | <0.0001 |
| 4 | 1.16 (1.06, 1.27) | 3.14 | 0.002 |
| Discharge destination | |||
| To another institution | 1.00 | ||
| Home | 1.31 (1.21, 1.42) | 6.46 | <0.0001 |
| Living near hospital | |||
| No | 1.00 | ||
| Yes | 1.29 (1.20, 1.40) | 6.56 | <0.0001 |
The summary results of the model were: log likelihood =−54645.6, Wald χ2(23)=829.2.
For category-variables scaled into four, each category represents one quartile of the distribution.
The overall effect of indicator-variables was tested using repeated (aggregated) tests (χ2). When not significant at the aggregated level, values for separate categories were not listed in the table.
The index reflects a relative measure of average hospital LOS adjusted for differences in patient-population by way of DRGs and DRG-specific average LOS.
Defined as the annual number of discharges/(man-years of personnel × 365). Adjusted for differences in patient-population by way of DRG and cost-weights.
The hospital emergency admission rate did have some effect on the probability of late readmission. The hospital threshold of admission with better access to smaller hospitals may also explain why an increased readmission risk was found related to the county and local hospitals. Generally there were many similarities between the effect of patient variables on early and later readmission. However, there were some notable differences. For late readmission gender did not turn out to be of significance. Discharge destination, however, was; patients discharged home were found to have a higher hazard of being readmitted (HR=1.31), than patients transferred to another institution. This is in accordance with other studies (Camberg et al. 1997).
Discussion
The results of this study with many significant variables, and with generally small effect sizes, visualize the complexity of modelling determinants of readmission. The data or variables included in the present study are in no way exhaustive. However, the intention was not to make a complete predictive model. The main objective was to study the association between hospital factors and early readmission. The results indicate that there exists a link between the basic conditions at which the hospitals deliver the care, and the outcome of the patients measured as early readmissions. Furthermore, the results also showed that the effect of the hospital variables on readmission is dependent upon time since the prior stay, since no such link could be demonstrated when increasing the time interval to 90–180 days since discharge.
Shortening stays is a common hospital response to increase productivity, acting across different systems and financial settings. Generally shorter stays can increase the patient turnover and reduce the input of resources per stay. In the model, short relative hospital LOS was found to increase the hazard of early readmission significantly. A relevant question would be if there is a general lower threshold value for LOS where it will no longer be possible to provide good care. To some extent it will be possible to compensate for shorter stays by application of more intensive care. Higher intensity could be achieved by a lower patient/staff ratio. The results give some support to the idea of a compensatory effect of staff, as relatively few discharges per man-years of personnel gave a significantly reduced risk of early readmission. The association was not found to be a monotonic trend, however, as the highest category of patient/staff ratio was not found to give an increased risk of readmission. Neither is the quantity of staffing the only factor that matters. With a given quantity of personnel, more intensive care could also be accomplished by better organization and coordination of tasks, and more efficient use of time. Supplying more sophisticated equipment or procedures would also influence the care. One possibility is that more intensive care would be reflected in higher costs per admission. According to the findings of the model, one may make the deduction that additional increase in costs above the reference level does not seem to act as a compensating factor.
There are additional implications following the tendency toward short lengths of stay. It may put even greater demands on the preparation of the discharge and coordination of the follow-up. And there will be a risk of discharging more patients in an unstabilized condition (Kosecoff et al. 1990). In general, the community and families will receive a greater burden of care. This means that factors reflecting the interplay between hospitals and community should be considered when analyzing readmissions. Insufficient adjustment for differences in community factors may represent a weakness in our study. A separate analysis was performed, however, including only patient and community variables, with adjustment for the clustering effects created for patients living in the same municipality. The model included the same patient variables as in the earlier analyses, and variables indicating supply of community care (the relative number of places in nursing homes, of general practitioners, and of man-years in the community care services) (Statistics Norway 1997). The results from modelling the probability of early readmissions showed a significant impact of the community variables, but the effect sizes were very small. Applying the same predictive factors in modelling readmission within 90–180 days, the community variables showed no significant effects. Weinberger, Oddone, and Henderson (1996) also found no compensating effect of increasing the access to primary care. The apparently small effect of these variables indicating the supply of alternative care seems like a surprising result. In the present study the result may be a reflection of the type of quantitative information included. Different factors, such as indicators of coordination and cooperation between the two levels of care, might be the essential ones. In any case it seems like a logical conclusion to consider readmissions to be indicators of the total chain of care, not only of the hospital performance (Ashton and Wray 1996). Further analyses should be performed including relevant variables at the level of patients, hospitals, and communities by way of multilevel analyzing methods.
As to factors included in the presented model, two of the patient variables can also be regarded as community characteristics: the discharge destination and the proximity to hospital. Living in a municipality with a local hospital gave a higher risk of both early and late readmission. This may be a result of better access, or that the hospitals are willing to take bigger risks with patients living nearby and being able to return within a short time if necessary. Since only readmissions to the same hospital were included in the study, there may be an intervening effect that patients living close by have a higher probability of returning to the same hospital. The general result of a significant association between hospital LOS and early readmission was also found in this subgroup.
The standardized emergency admission rate would, in addition to hospital factors, also depend on the availability of community care, and reflect the admission threshold of the general practitioners of the area. In any case, it can be argued that a high emergency admission rate is one explanation for patients having a high probability of unplanned readmission. This factor of threshold for admission (and re admission) was adjusted for in the model.
The variables that reflect the operating conditions are all measured at hospital level, and are measures that display an average of the status throughout the year. It would have been preferable to have access to information reflecting the actual status at the specific department from where the patient was discharged, and at the exact time it occurred.
The patient factors and characteristics of the illness are strong determinants of readmission. All the patient variables included in the model of early readmission were found to have a significant impact, except discharge destination, which was significant for late readmission. Gender, however, was not a significant variable for late readmission. A possible explanation for this result is that the effect of gender on early readmission may be mediated through hospital practice and a tendency toward earlier discharge of men, related to the fact that elderly men more often have a living spouse at home.
Several patient variables were included to adjust for the type and complexity of illness: the cost-weight of the case, the type of DRG (surgical or not), and whether the admission was emergent or not. For the cost-weight of the cases, patients in category 3 had an HR of 1.61 (95 percent CI=1.52, 1.72) compared to the reference category. This would seem like a reasonable result, the higher the use of hospital resources, the more serious the illness, and the higher the probability of an early readmission. Following this interpretation, a strictly monotonic trend would have been expected. A possible reason for the highest level of cost-weight having a somewhat lower effect size than expected, is that the cost-weights are not exact measures of the complexity or severity of illness; for instance, the costs of surgery tend to weight heavily. With the purpose of achieving a better adjustment for differences in severity of illness, the conditioned LOS of the index stay of the individual patient was included in an alternative model. The results showed that patients with the longest index stays within their DRG had the highest probability of early readmission. Since the patient LOS is also affected by the hospital LOS, the net effects become complex. So to keep the dimensions of influence as clear as possible, the simpler model was preferred here. Furthermore, the general results of this alternative model were very similar to those presented in Table 2, with a significantly increased risk of readmission for patients admitted to hospitals with the shortest LOS. In a study of Scottish hospitals, multilevel modelling methods were used to examine the relationship between LOS and readmission (Leyland 1995). Using crude figures, a slight positive correlation was found between the two measures at the hospital level. But the use of hospital residuals from a length-of-stay model as explanatory variables in a model for readmission rates brought to light the negative association between the LOS and readmission.
Because the adjustment for differences in patient characteristics applied in the model may be insufficient, and since the mechanisms of effect and associations may be condition specific (Thomas and Holloway 1991), an analysis was also performed on a subpopulation. This selection included patients with four different principal diagnoses: chronic obstructive pulmonary disease (DRG 88), angina pectoris (DRG 140), heart failure/shock (DRG 127), and specific cerebrovascular disorders (DRG 14). These four conditions were the most frequently occurring discharge diagnoses of the index admission for early readmitted patients. In this subgroup of patients direct adjustment for differences in diagnoses was performed including the DRG of each case in the model. When computing the model by Cox' regression to this material, the main results were the same as for the total patient population referred in Table 2. The patients admitted to hospitals with the longest stays were found to have a significantly lower risk of early readmission with an HR of 0.78 (0.65, 0.94). So the result of a link between hospital practice of the prior stay and early readmission also applied to this subgroup of patients.
One clear insufficiency of the material is the lack of information about the deaths of patients occurring in the studied time interval after discharge. Generally, one would assume the modelling or prediction of readmission to benefit from an inclusion of more direct measures of clinical elements and quality dimensions of the care process than what is the case in this study. However, even studies of specific conditions including a variety of measures of clinical data and hospital performance can show a low predictive or explanatory power (Kiefe 1999; Zitser-Gurevich et al. 1999), illustrating the complexity of finding good models for predicting readmission.
The question of generalizability of the results and comparability between different health-care systems must be raised. There certainly are many differences in basic conditions and organization, and the incentives toward change vary. However, the strive toward achieving cost-containment and high productivity seems to be general. Obviously short hospital stays is one main way of distributing and rationing the care. The results of this study give further support to the assumption that basic hospital operating conditions do affect the patients' care and outcome. From our cross-sectional study it is difficult to draw any conclusions as to the causal relationships. The study compares the status of different hospitals with different practices and “steady states.” It does not measure the effect of any specific change or intervention over time. Longitudinal studies of trends would be a way of exploring these questions further, which may also bring more knowledge about the trade-off points between cost-containment and quality (DesHarnais et al. 1991).
The question of an optimal status or equilibrium also depends on the time perspective applied, and if one includes the community care in the account. In a short time display an increased risk of readmission can appear as a good solution for the hospital in balancing the need of inpatients against those patients waiting to be admitted. It also results in a high hospital “output,” measured as the number of admissions. In a longer time frame, however, marginally longer or more care-intensive stays might result in fewer readmissions, and thereby fewer resources used all over. It can be discussed how undesirable readmissions are, and how many of them are preventable (Culler, Parchman, and Przybylski 1998; Frankl, Breeling, and Goldman 1991; Oddone et al. 1996; Williams and Fitton 1988). At least one can assume that with optimal hospital care and planning of aftercare, it is possible to prevent some new admissions or prolong the time period from discharge to a readmission. The consequences or costs of readmissions may be experienced differently by individual patients and their families compared with what is the case at the hospital or system level. So when monitoring system performance, readmission measures are relevant, particularly when considering vulnerable groups such as the elderly.
Notes
The DRG-system was first introduced in Norway in the late 1980s, with later modifications. An HCFA-12 grouper was implemented for classification of the 1996 patient-data used in this study. Cost-weights representative for the Norwegian hospitals were also developed (Henriksen and Håkonsen 1993; Nyland 1997).
The work was supported by a grant from The Norwegian Research Council, project no. 116712/330.
References
- Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. “The Association between the Quality of Inpatient Care and Early Readmission. A Meta-analysis of the Evidence.”. Medical Care. 1997;35(10):1044–59. doi: 10.1097/00005650-199710000-00006. [DOI] [PubMed] [Google Scholar]
- Ashton CM, Wray NP. “A Conceptual Framework for the Study of Early Readmission as an Indicator of Quality of Care.”. Social Science and Medicine. 1996;43(11):1533–41. doi: 10.1016/s0277-9536(96)00049-4. [DOI] [PubMed] [Google Scholar]
- Brownell MD, Roos NP, Burchill C. “Monitoring the Impact of Hospital Downsizing on Access to Care and Quality of Care.”. Medical Care. 1999;37(6):JS135–50. doi: 10.1097/00005650-199906001-00013. [DOI] [PubMed] [Google Scholar]
- Camberg LC, Smith NE, Beaudet M, Daley J, Cagan M, Thibault G. “Discharge Destination and Repeat Hospitalizations.”. Medical Care. 1997;35(8):756–67. doi: 10.1097/00005650-199708000-00002. [DOI] [PubMed] [Google Scholar]
- Chambers M, Clarke A. “Measuring Readmission Rates.”. British Medical Journal. 1990;301(6761):1134–6. doi: 10.1136/bmj.301.6761.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culler SD, Parchman ML, Przybylski M. “Factors Related to Potentially Preventive Hospitalizations among the Elderly.”. Medical Care. 1998;36(6):804–17. doi: 10.1097/00005650-199806000-00004. [DOI] [PubMed] [Google Scholar]
- DesHarnais S, Hogan AJ, McMahon LF, Fleming S. “Changes in Rates of Unscheduled Hospital Readmissions and Changes in Efficiency Following the Introduction of the Medicare Prospective Payment System.”. Evaluation of the Health Professions. 1991;14(2):228–52. doi: 10.1177/016327879101400206. [DOI] [PubMed] [Google Scholar]
- Epstein AM, Bogen J, Dreyer P, Thorpe KE. “Trends in Length of Stay and Rates of Readmission in Massachusetts: Implications for Monitoring Quality of Care.”. Inquiry. 1991;28(1):19–28. [PubMed] [Google Scholar]
- Frankl SE, Breeling JL, Goldman L. “Preventability of Emergent Hospital Readmission.”. American Journal of Medicine. 1991;90(6):667–74. [PubMed] [Google Scholar]
- Hammermeister KE, Shroyer AL, Sethi GK, Grover FL. “Why It Is Important to Demonstrate Linkages between Outcomes of Care and Processes and Structures of Care.”. Medical Care. 1995;33(109):OS5–16. doi: 10.1097/00005650-199510001-00002. [DOI] [PubMed] [Google Scholar]
- Heggestad T, Lilleeng SE, Solstad K, Petersen SØ. Reinnleggelser. (Readmissions). In Samdata Hospitals. Comparative data for general hospitals 1994. Trondheim: SINTEF Norwegian Institute for Hospital Research; 1995. [Google Scholar]
- Henriksen B, Håkonsen K. Kostnadsvekter for HCFA-8. (Cost-weights for HCFA-8) Oslo: Ministry of Health and Social Affairs; 1993. [Google Scholar]
- Kalseth B, Solstad K, Rønningen L, editors. Samdata Sykehus. Sammenligningsdata for somatisk fylkeshelsetjeneste 1996. (Samdata Hospitals. Comparative data for general hospitals 1996) Trondheim: SINTEF Norwegian Institute for Hospital Research; 1997. Report June. [Google Scholar]
- Kiefe C. “Predicting Rehospitalization after Bypass Surgery. Can We Do It? Should We Care?”. Medical Care. 1999;37(7):621–4. doi: 10.1097/00005650-199907000-00001. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG. Survival analysis. A self-learning text. New York: Springer-Verlag; 1996. [Google Scholar]
- Kosecoff J, Kahn KL, Rogers WH, Reinisch EJ, Sherwood MJ, Rubenstein LV, Draper D, Roth CP, Chew C, Brook RH. “Prospective Payment System and Impairment at Discharge. The `Quicker-and-sicker' Story Revisited.”. Journal of the American Medical Association. 1990;264:1980–3. [PubMed] [Google Scholar]
- Leyland AH. “Examining the Relationship between Length of Stay and Readmission Rates for Selected Diagnoses in Scottish Hospitals.”. IMA Journal of Mathematics Applied in Medicine and Biology. 1995;12:175–84. doi: 10.1093/imammb/12.3-4.175. [DOI] [PubMed] [Google Scholar]
- Lin DY, Wei LJ. “The Robust Inference for the Cox Proportional Hazard Model.”. Journal of the American Statistical Association. 1989;84:1074–8. [Google Scholar]
- Magnussen J, Kalseth B. Sykehussektoren pa. 90-tallet. Samdata sykehus. (Samdata Hospitals. Comparative data for general hospitals 1997) Trondheim: SINTEF Unimed Norwegian Institute for Hospital Research; 1998. [Google Scholar]
- Nyland K. Midlertidige kostnadsvekter til DRG-versjon HCFA 12. (Preliminary cost-weights for DRG-version HCFA 12) Trondheim: SINTEF Unimed Norwegian Institute for Hospital Research; 1997. [Google Scholar]
- Oddone EZ, Weinberger M, Horner M, Mengel C, Goldstein F, Ginier P, Smith D, Huey J, Farber NJ, Asch DA, Loo L, Mack E, Hurder AG, Henderson W, Feussner JR. “Classifying General Medicine Readmissions. Are They Preventable?”. Journal of General Internal Medicine. 1996;11(10):597–607. doi: 10.1007/BF02599027. [DOI] [PubMed] [Google Scholar]
- Official Statistics of Norway. Nursing and Care Statistics 1996. Oslo: Statistics Norway; 1997. [Google Scholar]
- Sibbritt DW. “Validation of a 28 Day Interval between Discharge and Readmission for Emergency Readmission Rates.”. Journal of Quality in Clinical Practice. 1995;15(4):211–20. [PubMed] [Google Scholar]
- Slack R, Bucknall CE. “Readmission Rates Are Associated with Differences in the Process of Care in Acute Asthma.”. Quality in Health Care. 1997;6(4):194–8. doi: 10.1136/qshc.6.4.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPSS. Advanced Statistics 7.5. Chicago: SPSS Inc; 1997. [Google Scholar]
- Stata. Reference Manual, Release 6. College Station TX: Stata Corporation; 1999. [Google Scholar]
- Thomas JW, Holloway JJ. “Investigating Early Readmission as an Indicator for Quality of Care Studies.”. Medical Care. 1991;29(4):377–94. doi: 10.1097/00005650-199104000-00006. [DOI] [PubMed] [Google Scholar]
- Weinberger M, Oddone EZ, Henderson WG. “Does Increased Access to Primary Care Reduce Hospital Readmissions?”. New England Journal of Medicine. 1996;334(22):1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Ayanian JZ, Chasan-Taber S, Sherwood MJ, Roth C, Epstein AM. “Hospital Readmission and Quality of Care.”. Medical Care. 1999;37(5):490–501. doi: 10.1097/00005650-199905000-00008. [DOI] [PubMed] [Google Scholar]
- Williams EI, Fitton F. “Factors Affecting Early Unplanned Readmission of Elderly Patients to Hospital.”. British Medical Journal. 1988;297(6651):784–7. doi: 10.1136/bmj.297.6651.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zitser-Gurevich Y, Simchen E, Galai N, Braun D. “Prediction of Readmissions after CABG Using Detailed Follow-up Data. The Israeli CABG Study (ISCAB).”. Medical Care. 1999;37(7):625–36. doi: 10.1097/00005650-199907000-00002. [DOI] [PubMed] [Google Scholar]