Abstract
Background
Patients who leave hospital against medical advice (AMA) may be at risk of adverse health outcomes and readmission. In this study we examined rates of readmission and predictors of readmission among patients leaving hospital AMA.
Methods
We prospectively studied 97 consecutive patients who left the general medicine service of an urban teaching hospital AMA. Each patient was matched according to age, sex and primary diagnosis with a control patient who was discharged routinely. Readmission rates were examined using Kaplan–Meier analysis. Regression models were used to test the hypothesis that readmissions among patients discharged AMA followed a biphasic curve.
Results
Patients who left AMA were much more likely than the control patients to be readmitted within 15 days (21% v. 3%, p < 0.001). Readmissions occurred at an accelerated pace during the first 15 days, followed by a 75-day period during which readmissions occurred at a rate comparable to that among the control patients. Among the patients who left AMA, being male and having a history of alcohol abuse were significant predictors of readmission within 15 days; however, these characteristics were common among the patients who left AMA. In the Cox proportional hazard models, leaving AMA was the only significant predictor of readmission (adjusted hazard ratio 2.5, 95% confidence interval 1.4–4.4).
Interpretation
The significantly increased risk of readmission among general medicine patients who leave hospital AMA is concentrated in the first 2 weeks after discharge. However, it is difficult to identify which patients will likely be readmitted.
Patients who leave hospital against medical advice (AMA) account for 0.8%–2.2% of discharges from medical services at various teaching and acute care hospitals in the United States.1,2,3,4 The rate of AMA discharge may be inversely correlated with socioeconomic status: a relatively low rate (0.8%) was observed at a hospital serving a primarily middle- and upper-class population,1 whereas a higher rate (2.2%) was seen at a hospital serving a disadvantaged urban area.3 In the United States 2 characteristics strongly linked to low socioeconomic status — lack of health insurance and Medicaid eligibility — are associated with an approximately 2-fold increase in the likelihood of leaving AMA.1,3 Our experience at a hospital providing care in a low-income urban area suggested that rates of discharge AMA were much higher than those reported in the literature.
Physicians may fear that premature discharge will lead to adverse health effects and readmission. A recent Canadian study found that HIV-positive patients leaving AMA were more likely to be readmitted with a related diagnosis within 30 days than those formally discharged (odds ratio [OR] 5.0, 95% confidence interval [CI] 3.0–8.2).5 However, little information is available on outcomes after discharge AMA among general medical patients. We therefore conducted this case–control study (a) to determine the rate of discharge AMA from a general medical ward at a hospital serving a disadvantaged urban Canadian population, (b) to compare readmission rates among patients leaving AMA and matched controls discharged formally and (c) to identify predictors of early readmission among patients leaving AMA.
Methods
St. Michael's Hospital is a teaching hospital in Toronto that serves many low-income neighbourhoods and a large concentration of homeless people. We defined patients as leaving AMA if they signed a standard hospital form acknowledging that they were discharging themselves contrary to the advice of their physician or if they left the hospital in an unscheduled manner without informing hospital staff. Between March 1997 and August 1998, there were 1874 discharges from the general medicine service; this number does not include 205 deaths. A total of 100 patients accounted for 113 discharges AMA (6.0% of total discharges). For patients who left AMA more than once during the study period, we included only the first time they left AMA.
Each patient who left AMA was paired with a control patient discharged routinely from the general medicine service between January 1997 and September 1998. Control patients and AMA patients were matched according to sex and Case Mix Group (CMG), which identifies the primary reason for the hospital stay. Case and control patients were also matched by age decade or, if this was not possible, within 10 years of the case patient's age. When multiple potential control subjects were identified, one was selected at random. Case and control patients differed by a mean of 3.7 years in age and 3.5 months in date of discharge. Three patients who left AMA were excluded because no other patient of the same sex and CMG had been discharged from the general medicine service during the study period. Patients who were deemed incompetent and compelled to remain in the hospital were excluded from the study.
Clinical data were obtained by chart review performed by 2 investigators (S.W.H. and R.E.M.). Whenever possible, patients leaving AMA were interviewed before or shortly after leaving the hospital and asked “What is your main reason for leaving the hospital today?” More than one reason could be coded for each patient. These reasons were recorded verbatim and categorized independently by the 2 investigators. Disagreements were examined, and a consensus was reached by the 2 investigators.
Readmissions during a 90-day follow-up period were ascertained through review of databases at St. Michael's Hospital and 4 nearby hospitals (Wellesley Hospital, Toronto General Hospital, Toronto Western Hospital and Toronto East General Hospital) that provide care to patients from the catchment area of St. Michael's Hospital. The charts of all patients who left AMA and were subsequently readmitted to St. Michael's Hospital were reviewed, as were records at the other hospitals if the patient had given consent for release of their information. The Research Ethics Board at all involved hospitals approved the study protocol.
For analysis, we used χ2 tests to compare characteristics of the case and control patients and to examine characteristics associated with readmission among patients who left AMA. Kaplan–Meier curves were used to examine time to readmission. Cox regression models were used to identify variables associated with readmission among all patients. The slope of the Kaplan–Meier curve for patients who left AMA appeared to be steep during the first 2 weeks after leaving hospital and then appeared to level off. We therefore conducted a post-hoc analysis using stepwise regression models to test whether the Kaplan–Meier curves of case and control patients consisted of a single curve or multiple-phase joined curve with different slopes.6
Results
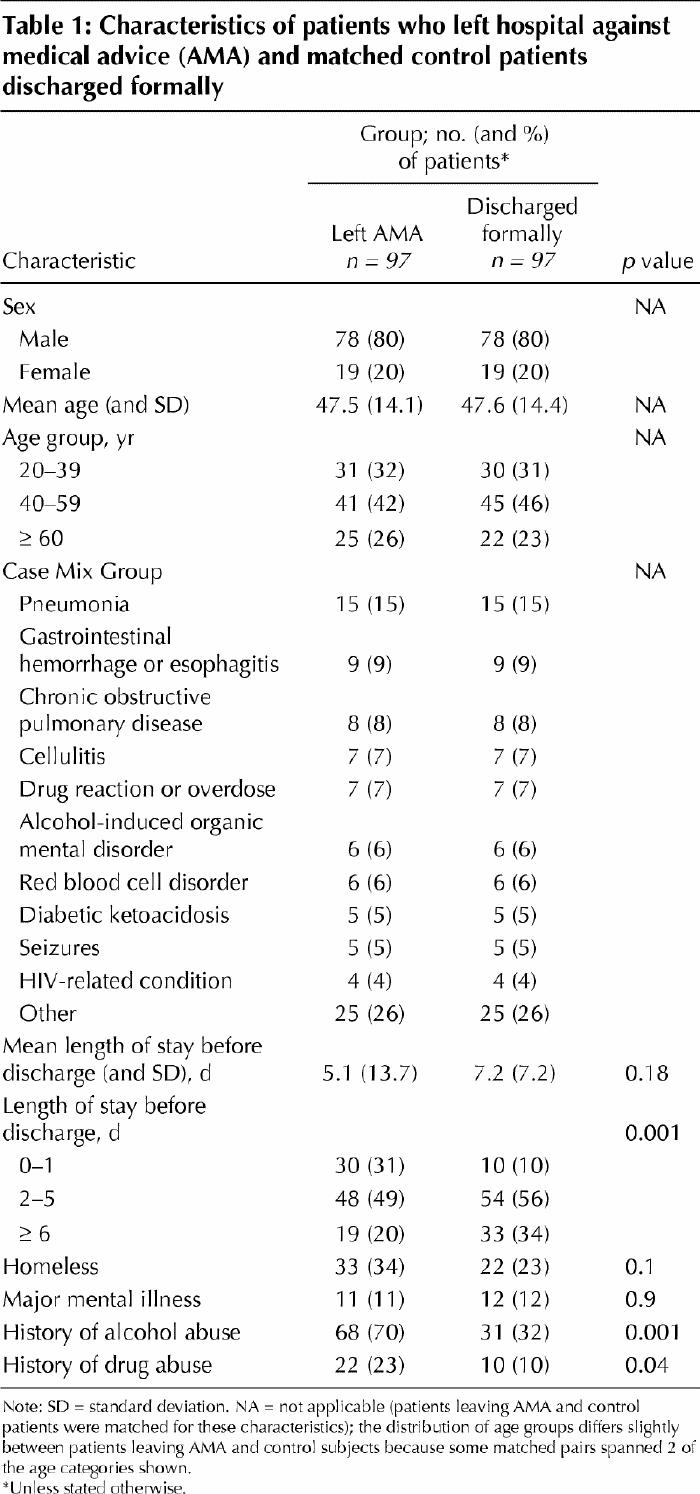
Characteristics of the patients are shown in Table 1. Patients who left AMA were significantly more likely than the control patients to have a history of alcohol or drug abuse and to have had shorter hospital stays. Interviews were completed with 57 (59%) of the patients who left AMA. The most commonly cited reasons for leaving the hospital were personal or family matters (16 patients), feeling well enough to leave (16), dissatisfaction with treatment received (16), feeling bored or fed up (11), dislike of hospitals in general (8) and miscellaneous other reasons (7). Although 70% of the patients who left AMA had a history of alcohol abuse, none cited a desire to drink as their reason for leaving.
Table 1
By 15 days, readmission rates were significantly higher in the AMA group than in the control group (21% v. 3%, p < 0.001). During the 90-day follow-up period, there were 65 readmissions among patients who left AMA, as compared with 21 among the control patients; 28% of the readmissions occurred at hospitals other than St. Michael's Hospital. Among the patients who left AMA, 95% of the readmissions within 15 days of leaving hospital and 69% of the readmissions within 90 days were for the same diagnosis as the initial one.
Kaplan–Meier analysis (Fig. 1) demonstrated that the patients who left AMA were significantly more likely than the control patients to be readmitted during the follow-up period (p < 0.001 by the log-rank test). The regression models revealed that the Kaplan–Meier plot for the control patients consisted of a single curve but that the Kaplan–Meier plot for the patients discharged AMA consisted of 2 curves, with a joint point at 15 days (p < 0.001). After adjustment for the difference in readmission rates between the AMA and control groups at 15 days, there was no significant difference in the Kaplan–Meier curves of these 2 groups between 15 and 90 days after discharge (p = 0.18 by the log-rank test). Thus, patients who left AMA were readmitted at an accelerated pace during the first 15 days, followed by a 75-day period during which their readmission rate was comparable to that of the control patients.
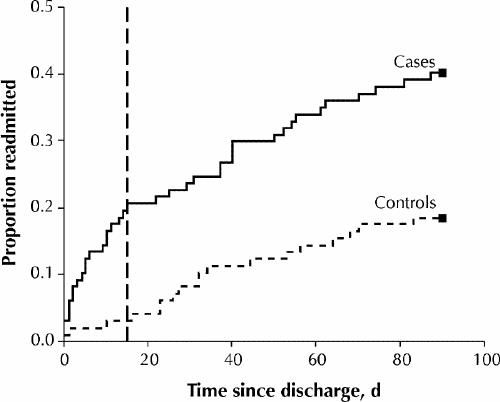
Fig.1: Proportion of patients readmitted to hospital from time of discharge against medical advice (cases) or formal discharge (controls). Vertical broken line indicates 15 days after discharge.
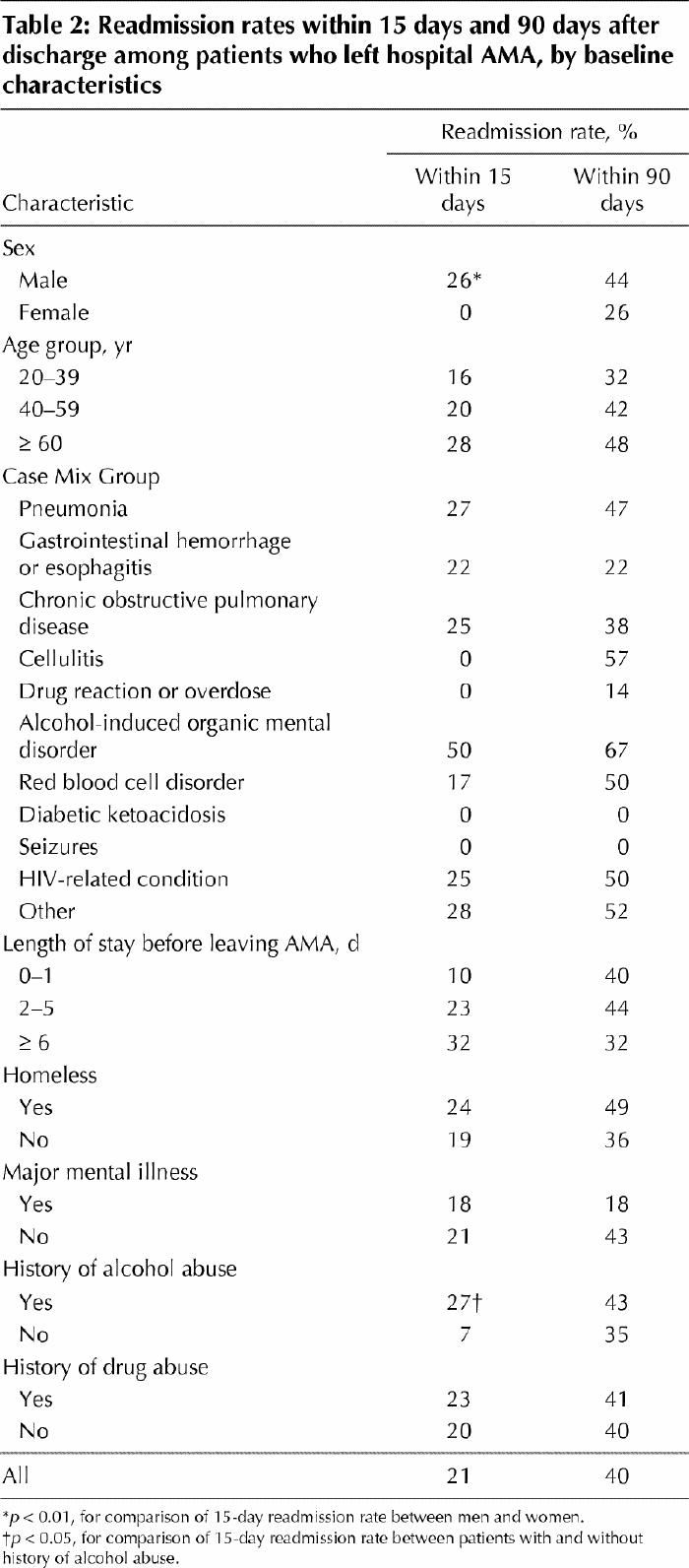
The relation between characteristics of AMA patients and subsequent readmission are shown in Table 2. Being male and having a history of alcohol abuse were significantly associated with a likelihood of readmission within 15 days. Patients initially seen because of a drug reaction or overdose, diabetic ketoacidosis or seizures were rarely readmitted during the follow-up period, but these trends did not reach statistical significance. Age, homelessness, mental illness and substance abuse were not correlated with readmission.
Table 2
In the Cox proportional hazards models, which included all 194 subjects, leaving AMA was the only characteristic found to be significantly associated with readmission (adjusted hazard ratio 2.5, 95% CI 1.4–4.4). Three patients who left AMA and 1 control patient died during the follow-up period (p = 0.61). A review of the charts suggested that none of the deaths among the patients who left AMA was directly related to the premature departure.
Interpretation
Patients leaving hospital AMA represent a problem of considerable importance. Based on an average AMA discharge rate of about 1%, more than 20 000 such discharges occur each year in Canada.7 Although our observation of a 20% higher readmission rate within 90 days among patients leaving AMA than among those discharged formally cannot be assumed to be applicable to all hospitals, a conservative estimate of a 10% excess readmission rate would translate into 2000 additional readmissions per year in Canada.
The 6% rate of discharge AMA observed in our study is far higher than that reported in other studies.1,2,3,4 One possible explanation is the high prevalence of alcohol and drug abuse in our patient population, as both these factors were associated with discharge AMA. Although our hospital serves a low-income urban area, our data do not permit an analysis of the independent effect of low socioeconomic status on the likelihood of leaving AMA. Length of stay may be another factor contributing to a high rate of discharge AMA. Previous studies were conducted in US hospitals, where the average length of stay is 7.3 days,8 as compared with 10.0 days in Canadian hospitals.9 Longer hospital stays may increase the likelihood that patients with a strong desire to leave the hospital do so AMA.
In our study, patients leaving AMA had a much higher risk of readmission within 15 days than patients discharged formally. This finding is consistent with a previous study from Boston, in which 7-day readmission rates were 14% among patients leaving AMA and 7% among control patients.1 This increased risk of readmission could reflect either the effect of leaving AMA or simply a high level of comorbidity among patients leaving AMA. Our data support the former hypothesis, since readmission rates were similar among AMA patients and controls after the first 15 days. Although patients leaving AMA were more likely than control patients to have a history of alcohol and drug abuse, leaving AMA was the only characteristic significantly associated with readmission in a Cox proportional hazards model.
If physicians could accurately identify which patients leaving AMA are at greatest risk of readmission, these individuals could be targeted for more aggressive follow-up. Although being male and having a history of alcohol abuse were significant predictors of readmission within 15 days, these characteristics would be of little value in selecting individuals for intervention because of their high prevalence among AMA patients. Our ability to identify other predictors of readmission was limited by insufficient statistical power.
How can physicians minimize the risk of adverse outcomes among patients leaving AMA? Existing research does not specifically address this question, although our findings suggest that efforts should focus on the first 2 weeks after departure. Reasonable recommendations would include giving the patient a specific follow-up appointment at the time of departure, ensuring that the patient receives appropriate prescriptions (or, preferably, the medications themselves) and providing the patient with a written summary of his or her hospital stay to assist health care providers in the event the patient presents to a different hospital. Follow-up by telephone would be desirable, since patients who leave AMA often lack a primary care provider1,3 and are likely to miss follow-up appointments; however, many of these patients may not have a telephone or may be difficult to contact. In our experience, follow-up with homeless people leaving AMA is feasible if it is known which homeless shelters and drop-in centres the person frequents; health care workers who provide outreach services at these sites can provide invaluable assistance.
This study has certain limitations. Patients leaving AMA were identified at a single urban hospital, and the characteristics and outcomes of such patients may vary at different hospitals. Our study did not identify readmissions to distant hospitals. However, unlike previous studies that ascertained only readmissions to a single hospital,1,3 we searched the records of multiple hospitals in a given area. Finally, sample size considerations limited the power of our study to identify characteristics predictive of readmission, and the significance of the associations we did identify were not adjusted for multiple comparisons. Confirmation of our findings in a larger study would be useful.
In this study of general medicine patients at an urban teaching hospital, those who left AMA were at greatly increased risk of readmission within the first 2 weeks after departure, but it was difficult to predict which patients would be readmitted. Future research is needed to focus on whether leaving AMA is associated with poorer health outcomes or increased health care costs, or if readmissions simply represent clinical care for “unfinished business” from a prematurely interrupted episode of care. Future research could also evaluate whether intervention strategies to improve follow-up of patients who leave AMA provide any benefit in terms of outcomes or costs.
Acknowledgments
This study was funded by a grant from the Physicians Services Incorporated Foundation. Dr. Hwang is the recipient of a Career Scientist Award from the Ontario Ministry of Health and Long-Term Care. The Inner City Health Research Unit is supported in part by a grant from the Ontario Ministry of Health and Long-Term Care. The results and conclusions are those of the authors, and no official endorsement by the Ontario Ministry of Health and Long-Term Care is intended or should be inferred. Preliminary reports of this study were presented at the 24th annual meeting of the Society of General Internal Medicine, held in San Diego in May 2001, and at the Congress of Epidemiology, held in Toronto in June 2001.
Footnotes
This article has been peer reviewed.
Contributors: Drs. Hwang and Li contributed to the conception and design of the study, the acquisition, analysis and interpretation of data, and the preparation of the initial draft of the article. Drs. Gupta and Chien contributed to the acquisition and interpretation of data and revised the article critically for important intellectual content. Ms. Martin contributed to the acquisition, analysis and interpretation of data and revised the article critically for important intellectual content. All of the authors approved the final version.
Competing interests: None declared.
Correspondence to: Dr. Stephen W. Hwang, Inner City Health Research Unit, St. Michael's Hospital, 30 Bond St., Toronto ON M5B 1W8; hwangs@smh.toronto.on.ca
References
- 1.Weingart SN, Davis RB, Phillips RS. Patients discharged against medical advice from a general medicine service. J Gen Intern Med 1998;13:568-71. [DOI] [PMC free article] [PubMed]
- 2.Smith DB, Telles JL. Discharges against medical advice at regional acute care hospitals. Am J Public Health 1991;81:210-3. [DOI] [PMC free article] [PubMed]
- 3.Jeremiah J, O'Sullivan P, Stein MD. Who leaves against medical advice? J Gen Intern Med 1995;10:403-5. [DOI] [PubMed]
- 4.Saitz R, Ghali WA, Moskowitz MA. The impact of leaving against medical advice on hospital resource utilization. J Gen Intern Med 2000;15:103-7. [DOI] [PMC free article] [PubMed]
- 5.Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O'Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ 2002;167(6):633-7. [PMC free article] [PubMed]
- 6.Smith PL. Splines as a useful and convenient statistical tool. Am Stat 1979;33: 57-62.
- 7.Hospital discharges by leading diagnoses and gender, Canada, 1999/00 [Table 4]. Ottawa: Canadian Institute for Health Information. Available: http://secure.cihi.ca/cihiweb/en/media_26sep2001_tab4_e.html (accessed 2003 Jan 21).
- 8.Health, United States, 2001. [table 96]. Hyattsville (MD): National Center for Health Statistics; 2001.
- 9.Average length of stay in hospital, by selected diagnostic group, 1996–1997. Ottawa: Statistics Canada; 1997. Available: www.statcan.ca/english/Pgdb/health20a.htm (accessed 2003 Jan 14).


