Abstract
THIS ARTICLE CONCISELY DESCRIBES the more common epilepsy conditions and will enable physicians to efficiently evaluate and manage these disorders. Salient aspects of the history and examination, together with electroencephalography, will usually determine the epilepsy syndrome (category), forming the basis for any further investigation and possible antiepileptic therapy. Imaging may be required in some circumstances.
Epilepsy and stroke are the 2 most common neurological disorders: at any one time 7 in 1000 people in the general population have epilepsy. Epilepsy usually begins in childhood, potentially impeding education, employment, social relationships and development of a sense of self-worth. Prompt, accurate diagnosis with appropriate social and medical management will optimize the situation. A family physician, in conjunction with a neurologist, can ascertain (a) if the episodes represent epileptic seizures and (b) if so, which epileptic syndrome they represent.
A harmonized partnership between family physician and neurologist will facilitate the recognition and care of epileptic disorders. As the role of the family physician in the care of patients with epilepsy increases, the principles delineated in this article will be ever more utilized.
Differential diagnoses
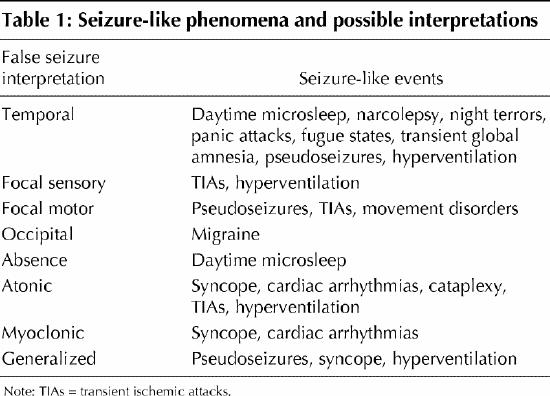
Before determining whether paroxysmal events represent an epileptic disorder, one must consider 2 alternatives: (a) nonepileptic events mimicking epileptic seizures (Table 1) and (b) true epileptic seizures caused by a nonneurological condition (Box 1). Three conditions are common imitators of epilepsy: syncope, excessive daytime sleep and pseudoseizures.
Table 1
Box 1.
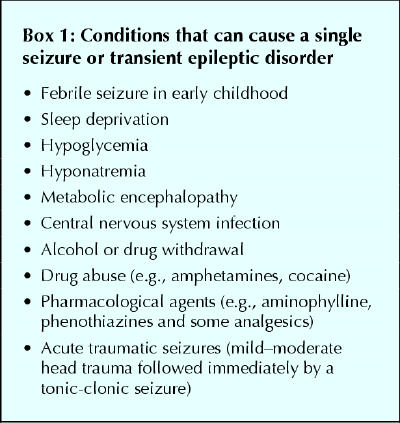
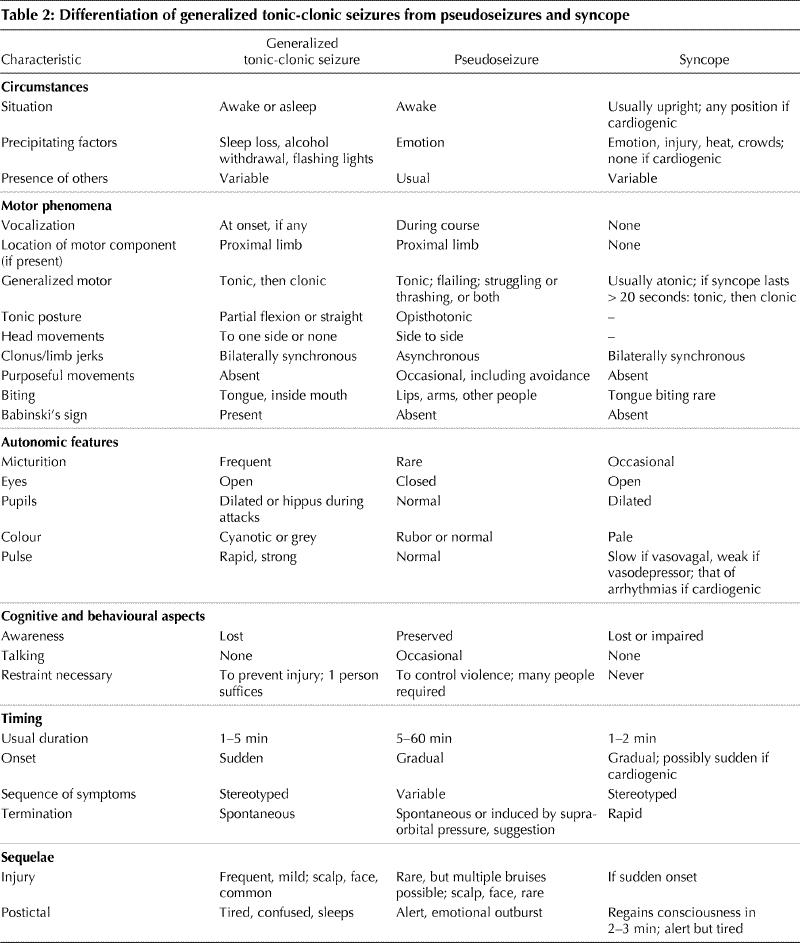
Table 2 lists several distinguishing manifestations of syncope, which resembles a generalized tonic-clonic (GTC) seizure in the middle of the attack but not at its onset or termination. Almost always while in an erect sitting or standing position, the patient feels faint, vision may blur, the face becomes pale, sweating may occur, and the patient falls atonically with occasional bilaterally synchronous tonic or myoclonic phenomena followed by rapid recovery, albeit with fatigue. The principal differential diagnosis is a treatable cardiac arrhythmia, and this should be strongly suspected if syncope-like attacks occur in other circumstances, particularly upon exercise.
Table 2
Excessive daytime sleep, as episodes of microsleep, occurs in children at school and in adults; it superficially resembles temporal lobe seizures or absence attacks. The patient stares without specific warning or appears inattentive; automatisms may occur. Unlike seizures, episodes of microsleep can be reliably and instantly aborted with an afferent stimulus. Evidence of sleep deprivation includes less than 7 hours of sleep, hypnic jerks in drowsiness, frequent dreaming, prominent snoring, morning arousal only with stimuli, morning irritability, excessive caffeine intake and prolonged sleeping on weekends.
Psychogenic nonepileptic events may be defined as “a paroxysmal behavioural pattern mimicing epileptic seizures and initiated by psychological mechanisms”.1 Diagnosis depends principally on symptomatology (Table 2). A physician should suspect such events in any patient with an apparently intractable cryptogenic “seizure disorder,” except in infants or elderly people. Psychogenic events may mimic any type of epileptic seizure and may occur as a pseudostatus epilepticus. Distinguishing between psychogenic and frontal lobe epileptic seizures may be difficult although the latter are shorter and occur principally at night. Psychogenic events may supervene in some truly epileptic patients. Electroencephalogram (EEG) monitoring may be required. However, epileptic seizures that arise from mesial or inferior cortical surfaces may demonstrate no interictal or ictal EEG abnormality. At the Epilepsy Programme in London, Ont., we have developed a system for identifying suspected psychogenic attacks that consists of taking a detailed description of the attack, 24-hour telemetered EEG recordings over 2–3 days and a clinical psychological consultation including the Minnesota Multiphasic Personality Inventory-2 (MMPI-2). The MMPI-2 contains profiles of significant sensitivity and specificity for anxiety, somatization and hysteria, components that predispose a person to pseudoseizures. The evaluation concludes with an interview with the patient, one or more close relatives, the clinical psychologist and the neurologist.
An erroneous diagnosis of epilepsy carries serious consequences. Missing a cardiac arrhythmia could be fatal. The patient could be unnecessarily exposed to side effects of antiepileptic medications; this occurs principally in emergent situations with pseudostatus epilepticus. Potentially treatable psychiatric conditions could be overlooked. The patient could unnecessarily lose his or her driver's licence and occupation.
Principal epilepsy syndromes
The first step in epilepsy management is identification of the syndrome. A syndrome is a constellation of factors that defines each epileptic disorder and influences management. Syndrome determination hinges on seizure description and frequency, age at onset, neurological history and functional enquiry, neurological examination and one or more EEGs. The neurological functional enquiry (review of systems) seeks areas of cognitive and other neurological dysfunctions that may lead to syndrome identification. Neuroimaging may aid in evaluation, but most syndromes are defined by the afore-mentioned means. Most epileptic disorders that a general physician will see will be manifestations of a syndrome. The following describes the most common ones.
Absence seizures
Absence seizures begin in childhood or early adolescence, with 5–20-second episodes of sudden arrest of activity, staring straight ahead or upward, occasionally with myoclonic activity of the eyelids, face or upper extremities, and ending abruptly without postictal confusion. Generalized tonic-clonic (GTC; “grand mal”) seizures occur in about one-third of such patients, usually in adolescence. Findings from the neurological functional enquiry and examination, including cognition, are normal. Prognosis varies such that “growing out of it” cannot be assured.
Management
The EEG shows sudden bursts of bilaterally synchronous 3-Hz spike-waves, whose quantity usually reflects the frequency of absence seizures.
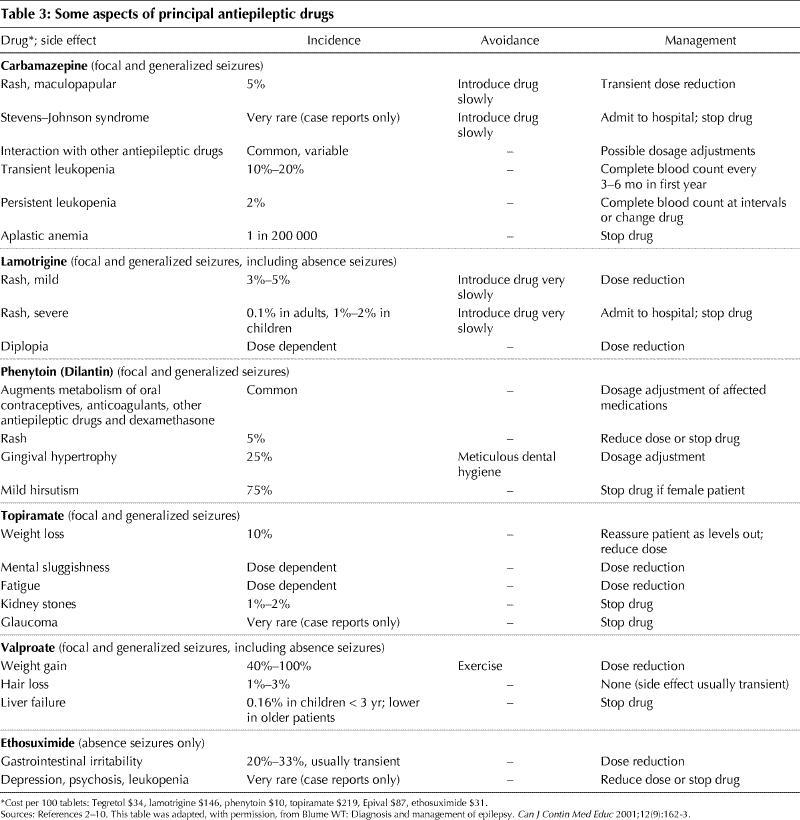
Complete eradication of absence attacks may require excess medication, and therefore a compromise between adequate dosage and attack frequency may be required. Valproate and lamotrigine act against absence and GTC seizures, whereas ethosuximide, although equally effective, only acts against absence seizures (Table 3).2,3,4,5,6,7,8,9,10
Table 3
Juvenile myoclonic epilepsy and generalized tonic-clonic seizures upon awakening
These adolescents usually present with a history of GTC seizures in sleep, within 1 hour of awakening or late in the evening. Anxiety, sleep loss and alcohol ingestion are precipitants. Absence attacks occur in about 30% of such patients. Myoclonus of the arms may occur shortly after awakening or in the evening. The history of myoclonus is often difficult to obtain, leaving one with a diagnosis of GTC seizures on awakening.11 Otherwise the syndromes are identical.
Management
The EEGs may show 3–4-Hz bisynchronous spike-waves but may be normal.
Treatment options are (a) none, if precipitants can be avoided, (b) valproate, the most effective, (c) lamotrigine, if valproate gives side effects, or (d) phenytoin, at a low dose (e.g., about 200 mg/d) (Table 3).
Benign focal epilepsy of childhood with “rolandic spikes”
This benign focal epilepsy has no identifiable brain lesion. It accounts for 10%–16% of all patients with seizures under the age of 15 years and is 3–4 times more common than childhood absence seizures.12,13 An otherwise healthy child has episodes of a unilateral unusual sensation in the mouth, face or one arm, with hypersalivation. Focal tonic or clonic phenomena involving the mouth, tongue or arm may occur, and speech may arrest. Most of such attacks begin during sleep, awakening the patient. This syndrome may present as nocturnal GTC seizure followed by a brief Todd's paresis and may be the most common cause of an idiopathic nocturnal GTC seizure in children between 5 and 10 years of age.
Management
This benign syndrome cannot be diagnosed without demonstration of typical “rolandic” spikes on an EEG of a nonsedated patient, whether awake or asleep, but 2 EEGs may be required to disclose their presence. Lack of such spikes draws into question this diagnosis and may prompt further evaluation, including imaging. The seizure tendency ends by adolescence in 98% of cases, and medication can then be omitted.
No treatment may be necessary if the seizures occur rarely and do not disrupt the child's activities. Alternatively, a low dose of carbamazepine, lamotrigine, valproate or phenytoin will often suffice.
Temporal lobe seizures
The temporal lobe is the most common site of focal seizures, and the seizures most often begin in childhood or adolescence. Aurae include an epigastric sensation, fear and various types of visual, olfactory or auditory experiential phenomena. Cognition may be impaired during the seizure, manifesting as confusion, a receptive or expressive dysphasia, apraxia, distraction by an experiential phenomenon or amnesia. Thus, the term “dyscognitive” will replace “complex partial” for this seizure type.
Unilateral or bilateral manual automatisms may occur when cognition is impaired. Dystonic posturing should be sought by observation or history-taking, as it almost always occurs in the arm contralateral to seizure origin. Chewing and swallowing may occur. Ictal speech, even if nonsensical, suggests involvement of the temporal lobe nondominant for language. A GTC seizure may evolve immediately from a dyscognitive one and is often heralded by contralateral head and eye deviation. Alternatively, GTC seizures may appear independently.
Prolonged febrile seizures may have occurred in infancy. Memory may be impaired if the epilepsy and pathology reside in both temporal lobes or principally in the temporal lobe dominant for language. Subtle or overt signs of unilateral motor dysfunction in the face, hand or leg should be sought on neurological examination.
Management
Temporal lobe interictal EEG spikes should be sought to confirm the clinical diagnosis, but more than one EEG may be required. The lack of temporal lobe epileptiform activity on about 3 routine EEGs suggests the need to reassess the diagnosis. MRI scanning is clearly warranted to determine the side and nature of the abnormality and its cause.
Generally favoured medications include carbamazepine, phenytoin, lamotrigine and topiramate.14 However, temporal lobe epilepsy may not respond adequately to antiepileptic drugs. In fact, the need to use a second medication either as monotherapy or dual therapy reflects the severity of the disorder, reducing somewhat the chances that adequate control will ever be obtained. In this instance, epilepsy surgery should be considered.
Special issues
The first seizure
Management of a patient with a first epileptic seizure depends primarily on clinical analysis and EEG findings. Imaging may be required for (a) seizures not associated with a benign syndrome, (b) focal seizures, (c) nonprecipitated attacks, (d) an associated central nervous system disorder and (e) subsequent unexpectedly refractory seizures.
Look for avoidable precipitants. Sleep loss, stress and alcohol withdrawal may provoke GTC seizures.15 Only about 3% of patients with such “stress-induced” attacks will develop spontaneous seizures.
About 8% of patients with a first seizure may have a brain tumour.16 This drops to 1% among patients with a normal neurological functional enquiry. Such would include any personality or cognitive change, or newly acquired motor, somatosensory or visual change. In this group the chance diminishes to 0.6% if the findings on neurological examination are normal, and to 0.3% if the EEG shows no focal abnormality.
In both adults and children, the following augment the risk of recurrence from about 33% to at least 50%: focal seizures, abnormal findings on neurological examination, pre-existing neurological disorder and focal spikes or generalized spike-waves on EEG.17,18,19
Although antiepileptic drugs reduce the risk of early seizure recurrence, their early use apparently does not affect longer term remission rates.20,21 Moreover, compliance with antiepileptic drug therapy after a single seizure varies among patients.
Women's issues
Catamenial epilepsy
Catamenial epilepsy refers to the appearance or worsening of seizures in the perimenstrual period or, rarely, in the entire second half of the menstrual period if no progesterone is secreted (“inadequate luteal phase” syndrome).22 This relates to a shift of the ratio between estrogen (pro-epileptogenic) and progesterone (anti-epileptogenic). Serum levels of antiepileptic drugs may drop perimenstrually, at which time a slight dose increase may be required.
Contraception
Enzyme-inducing drugs such as carbamazepine, oxcarbazepine, phenytoin, phenobarbital, primidone and topiramate may accelerate the metabolism of both estrogen and progesterone, thereby reducing their concentrations by up to 50%. This increases the risk of pregnancy in patients taking oral contraceptives23 and suggests the need to increase the dose of estradiol from 35 μg to 50 μg if an enzyme-inducing antiepileptic drug is given. Midcycle bleeding may indicate that estrogen levels are too low to block ovulation. Drugs that do not increase the risk of oral contraceptive failure include valproate, lamotrigine and gabapentin. Oral contraceptives do not impair seizure control.
Pregnancy
The following considerations derive from 2 fundamental questions: Do seizures or antiepileptic drugs harm the fetus?
A prolonged GTC seizure may produce fetal distress or death.24 However, nonconvulsive seizures are apparently innocuous.25 There is no evidence that seizures create deformities. Seizures remain unchanged in 60%, are increased in 30% and decreased in 10% of pregnancies.23 Poor preconception seizure control predicts incomplete control in pregnancy.
In preparing a patient with an apparent seizure disorder for pregnancy, the treating physician should ask 3 questions: Are the events epileptic seizures? Does the epilepsy still require treatment? Can any polytherapy be changed to monotherapy?
Antiepileptic medication levels may decline during pregnancy because of increases in drug metabolism, excretion and volume of distribution, and decreases in absorption, protein binding and compliance. It is prudent to measure antiepileptic serum levels before conception, at the beginning of each trimester and during the last month in patients with moderately severe seizure disorders.
Teratogenic effects
The risk of major malformations in babies of mothers taking antiepileptic drugs is about 4%–8% as compared with a baseline of 1%–3%.25 Most of this increased risk can be attributed to unfavourable lifestyle, inadequate nutrition, high antiepileptic drug levels and polypharmacy.24,25 Therefore, if possible, change gradually to monotherapy, which is usually a safe procedure.
As no single antiepileptic drug has been shown to be more teratogenic than another, a pregnant woman should keep taking her current drug, which is presumably the best antiepileptic drug for her epilepsy. Barbiturates, phenytoin and ethosuximide have been associated with congenital heart, cleft lip and palate abnormalities.24 Valproate and carbamazepine may produce neural tube defects and hydrocephalus, with an incidence of neural tube defects of 1%–2% for valproate and 0.5%–1% for carbamazepine.24,25 Effects of oxcarbazepine, topiramate and lamotrigine are unknown. Minor malformations such as hypertelorism, low-set ears and nail-bed hypoplasia may occur, but these usually do not cause serious medical or cosmetic effects.23
Adequate nutrition and folic acid supplementation by about 4–5 mg/d in any sexually active woman of childbearing age lowers the risk of major fetal malformations, especially neural tube defects in babies of young women taking antiepileptic drugs.23,24,26 As neural tube and cardiac malformations occur during the first 5 weeks of pregnancy, adequate folic acid levels should be established before conception.
Because of high fetal demand, folic acid levels decline in pregnancy, reaching a nadir at term.23 Women who smoke have lower folic acid levels than those who do not smoke. High folic acid levels do not appear to exacerbate a seizure disorder.
An expert obstetric opinion is needed to monitor for congenital defects. This may involve α-fetoprotein screening: that of amniotic fluid is apparently more reliable than that of maternal serum.24 Ultrasonography at 16–18 weeks' gestation may be necessary as well.
Hemorrhagic disease of the newborn may occur in an infant whose mother has lower than normal levels of vitamin K–dependent clotting factors. This can be prevented with 10–20 mg per day of vitamin K orally in the last month of pregnancy23,25 (Dr. Renato Natale, Associate Chief, St. Joseph's Health Centre and London Health Sciences Centre — University Campus, London, Ont.: personal communication, 2002). Oral vitamin K can be obtained in Canada through the Special Access Programme.27,28
Postpartum considerations
Although antiepileptic drugs are detectable in breast milk, their concentrations are usually lower than those in maternal serum. Breast-feeding should not be discouraged in women with epilepsy, because its advantages appear to outweigh the rare (5%–10%) adverse effects to the baby of sedation, hypotonia and feeding difficulty. Drug withdrawal symptoms have been reported sporadically.23 Antiepileptic drug levels may gradually increase over the first few weeks after birth as enzymatic induction will have decreased.
Mothers with incompletely controlled seizures should avoid bathing an infant in the bathtub without another person present and should change the infant on the floor.
Epilepsy in elderly patients
Unfortunately, the incidence and prevalence of epilepsy increases in elderly people because hemorrhagic and ischemic stroke, primary or secondary tumours, trauma, dementia and metabolic disorders occur commonly in this population. Fortunately, such epilepsy is seldom intractable. The consequences of uncontrolled seizures may be greater in elderly patients: a fall may fracture a hip or create a subdural hematoma, whereas a GTC seizure may crush a vertebra, giving back pain. A postictal state may manifest as memory loss, cognitive impairment, or an increase in a hemiparesis or dysphasia.
The principal differential diagnoses are syncope, sudden falls of elderly people, transient ischemic attacks or even sleep disturbances. Nonconvulsive status epilepticus appears more often in elderly people, manifesting as mild confusion and forgetfulness or total unresponsiveness for hours or days.
Management
Diagnostic tests include EEG, CT scanning and metabolic studies. The need for antiepileptic drugs and ongoing medication should be reviewed to diminish polypharmacy and its complications. The choice of any needed antiepileptic drug is guided by efficacy, ease of introduction and administration, potential drug interactions and likelihood of significant side effects. As most seizure disorders in elderly patients are focal with possible secondary generalization, carbamazepine and phenytoin would be appropriate drugs.14,29
Driving
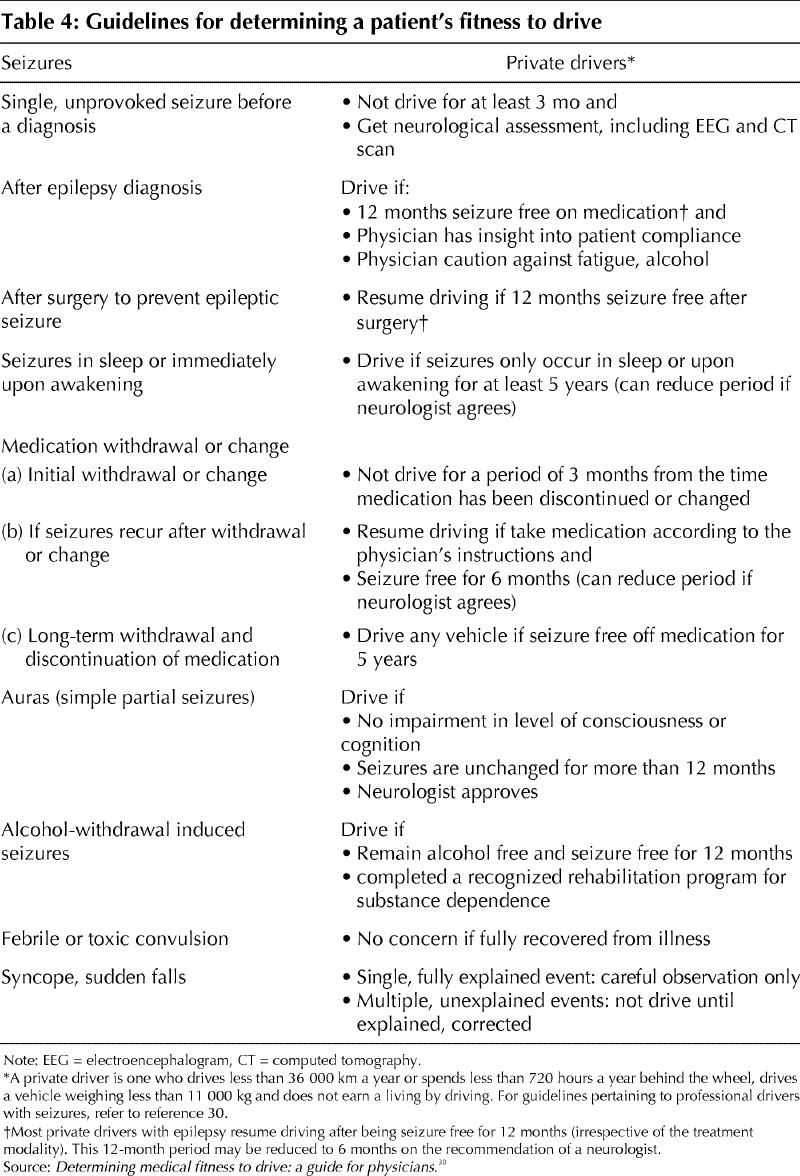
The loss or suspension of a driving licence significantly disrupts life, but the medical, emotional and legal impacts of a medically related driving injury to others or self potentially produce greater anguish. These opposing considerations have led to the development by the Canadian Medical Association of guidelines for physicians (Table 4).30 Although studies have shown the risk of motor vehicle crashes to be only equal or one-third greater among drivers with epilepsy as compared with the general population,31 this near equality may have been achieved by the implementation of the CMA's guidelines. Risk assessment should include seizure frequency and loss of awareness or other faculty during the events. Legal responsibility for failing to report possibly incapable drivers is being placed ever more upon physicians.
Table 4
Antiepileptic drug therapy: key points .
Monotherapy suffices for most seizure disorders.
Twice-daily dosing is most practical except in pregnancy, when dosing 4 times daily prevents a serum level surge and therefore has less effect on the fetus.
The severity of the seizure disorder, not the laboratory numbers, determines the “therapeutic range.” Whatever serum drug level renders the patient seizure free is adequate for that patient, even if it is below the laboratory range.
Dual therapy with most antiepileptic drugs at serum levels in the middle of the laboratory range impairs cognition.
Effectiveness and side effects both depend on dosage. Small changes in dosage can produce dramatic effects.
Traditional antiepileptic drugs may be as effective as new ones.
Fatigue is the most common side effect of most antiepileptic drugs.
Phenytoin is the only antiepileptic drug that can be started at full dose.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. Warren T. Blume, London Health Sciences Centre — University Campus, 339 Windermere Rd., London ON N6A 5A5; fax 519 663-3753; warren.blume@lhsc.on.ca
References
- 1.Kuyk J, Leijten F, Meinardi H, Spinhoven, Van Dyck R. The diagnosis of psychogenic non-epileptic seizures: a review. Seizure 1997;6:243-53. [DOI] [PubMed]
- 2.Canadian Pharmacists Association. Tegretol. Compendium of pharmaceuticals and specialties. Ottawa: The Association; 2002. p. 1666-8.
- 3.Canadian Pharmacists Association. Lamictal. Compendium of pharmaceuticals and specialties. Ottawa: The Association; 2002. p. 866-70.
- 4.Canadian Pharmacists Association. Dilantin. Compendium of pharmaceuticals and specialties. Ottawa: The Association; 2002. p. 509-12.
- 5.Canadian Pharmacists Association. Topamax. Compendium of pharmaceuticals and specialties. Ottawa: The Association; 2002. p. 1709-13.
- 6.Canadian Pharmacists Association. Epival. Compendium of Pharmaceuticals and Specialties. Ottawa: The Association; 2002. p. 582-6.
- 7.Canadian Pharmacists Association. Zarontin. Compendium of Pharmaceuticals and Specialties. Ottawa: The Association; 2002. p. 1899.
- 8.Levy RH, Dreifuss FE, Mattson RH, Meldrum BS, Penry JK. Antiepileptic drugs. 3rd ed. New York: Raven Press; 1989.
- 9.Levy RH, Mattson RH, Meldrum BS. Antiepileptic drugs. 4th ed. New York: Raven Press; 1995.
- 10.Wyllie E. The treatment of epilepsy, principles & practice. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2001.
- 11.Blume WT. Epilepsy with generalised tonic-clonic seizures on awakening and other idiopathic generalised epilepsies. In: Meinardi H, editor. The epilepsies, Part II. Vol 73(29) of Handbook of clinical neurology series. Amsterdam: Elsevier Science; 2000. p. 175-82.
- 12.Van Huffelen AC, van der Meij W. Idiopathic partial epilepsies. In: Meinardi H, editor. The epilepsies, Part II. Vol 73(29) of Handbook of clinical neurology series. Amsterdam: Elsevier Science; 2000. p. 5-35.
- 13.Loiseau P. Idiopathic and benign partial epilepsies. In: Wyllie E, editor. The treatment of epilepsy. Principles and practice. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 475-84.
- 14.Karceski S, Morrell M, Carpenter D. The expert consensus guideline series. Treatment of epilepsy. Epilepsy Behav 2001;(Suppl 2):A1-50.
- 15.Friis ML, Lund M. Stress convulsions. Arch Neurol 1974;31:155-9. [DOI] [PubMed]
- 16.Bardy AH. Decisions after first seizure. Acta Neurol Scand 1991;83:294-6. [DOI] [PubMed]
- 17.Berg AT, Shinnar S. The risk of seizure recurrence following a first unprovoked seizure: a quantitative review. Neurology 1991;41:965-72. [DOI] [PubMed]
- 18.Shinnar S, Berg AT, Moshe SL, Petix M, Maytal J, Kang H, et al. Risk of seizure recurrence following a first unprovoked seizure in childhood: a prospective study. Pediatrics 1990;85:1076-85. [PubMed]
- 19.Camfield PR, Camfield CS, Dooley JM, Tibbles JA, Fung T, Garner B. Epilepsy after a first unprovoked seizure in childhood. Neurology 1985;35:1657-60. [DOI] [PubMed]
- 20.Camfield C, Camfield P, Gordon K, Dooley J. Does the number of seizures before treatment influence ease of control or remission of childhood epilepsy? Not if the number is 10 or less. Neurology 1996;46:41-4. [DOI] [PubMed]
- 21.First Seizure Trial Group. Randomized clinical trial on the efficacy of anti-epileptic drugs in reducing the risk of relapse after a first unprovoked tonic-clonic seizure. Neurology 1993;43:478-83. [DOI] [PubMed]
- 22.Klein P, Herzog AG. Hormones and epilepsy. In: Schmidt D, Schachter SC, editors. Epilepsy: problem solving in clinical practice. London: Martin Dunitz; 2000. p. 413-33.
- 23.Foldvary N. Treatment of epilepsy during pregnancy. In: Wyllie E, editor. The treatment of epilepsy principles and practice. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 775-86.
- 24.Lindhout D. Pregnancy and epilepsy. In: Schmidt D, Schachter SC, editors. Epilepsy: problem solving in clinical practice. London: Martin Dunitz; 2000. p. 241-52.
- 25.Sadler RM. Women's issues and epilepsy. Mississauga (ON): The Medicine Group; 2002. Merritt-Putnam Neurology Residents' Course.
- 26.Canadian Pharmacists Association. Folic acid. Compendium of pharmaceuticals and specialties. Ottawa: The Association; 2002. p. 658-9.
- 27.Canadian Pharmacists Association. Vitamin K. Compendium of pharmaceuticals and specialties. Ottawa: The Association; 2002. p. 1842-3.
- 28.Canadian Pharmacists Association. Special Access Programme. Compendium of pharmaceuticals and specialties. Ottawa: The Association; 2002. p. A7.
- 29.Parker BM, Vestal RE. Pharmacokinetics of anticonvulsant drugs in the elderly. In: Wyllie E, editor. The treatment of epilepsy, principles and practice. Philadelphia: Lea & Febiger; 1993. p. 769-74.
- 30.Canadian Medical Association. Determining medical fitness to drive. 6th ed. Ottawa: The Association; 2000.
- 31.McLachlan R. Epilepsy and driving. Mississauga (ON): The Medicine Group; 2002. p. 44-7. Merritt-Putnam Neurology Residents' Course.


