Abstract
Objectives: An observational study describes on-duty nurses' informative behaviors from the perspective of library and information science, rather than patient care,. It reveals their information sources, the kinds of information they seek, and their barriers to information acquisition.
Methods: Participant observation and in-context interviews were used to record in detail fifty hours of the information behavior of a purposive sample of on-duty critical care nurses on twenty-bed critical care unit in a community hospital. The investigator used rigorous ethnographic methods—including open, in vivo, and axial coding—to analyze the resulting rich textual data.
Results: The nurses' information behavior centered on the patient, seeking information from people, the patient record, and other systems. The nurses mostly used patient-specific information, but they also used some social and logistic information. They occasionally sought knowledge-based information. Barriers to information acquisition included illegible handwriting, difficult navigation of online systems, equipment failure, unavailable people, social protocols, and mistakes caused by people multitasking while working with multiple complex systems. Although the participating nurses understood and respected evidence-based practice, many believed that taking time to read published information on duty was not only difficult, but perhaps also ethically wrong. They said that a personal information service available to them at all hours of the day or night would be very useful.
Conclusions: On-duty critical care nursing is a patient-centric information activity. A major implication of this study for librarians is that immediate professional reference service—including quality and quantity filtering—may be more useful to on-duty nurses than do-it-yourself searching and traditional document delivery are.
INTRODUCTION
This study presents evidence of on-duty critical care nurses' information behavior. It describes the kinds of information they seek, their information sources, and their barriers to information acquisition at the point of care. As Dalrymple writes,
Observation of information-gathering behaviors … contributes to developing delivery systems that actually work. Understanding the information behaviors of clinicians—how they seek information and how they apply it to practice—is a crucial first step in designing information delivery systems. [1]
Hospital librarians decry practicing nurses' lack of use of traditional library services [2–9]. They are perplexed when service, marketing, and teaching strategies developed for libraries in large university health sciences centers do not work well in libraries in community hospitals. It is unreasonable to expect working nurses to use hospital libraries in the same manner that they used academic libraries when they were in school or to assume that the on-duty hospital nurses' information ecology is similar to that of the nursing student. With the exception of the rare clinical librarians, informationists, and clinical information specialists in context (all of whom practice in teaching hospitals), most hospital librarians have spent little, if any, time with nurses on a hospital unit.
To provide effective library services for practicing hospital nurses, librarians need to understand the nurses' on-the-job information behavior. Many research studies of the information seeking of faculty and students, and of practicing physicians in teaching hospitals, have been conducted, but few have been conducted of community hospital nurses. Existing studies of nurses seeking knowledge-based information rely on post hoc self-report data gathered through surveys and interviews, not direct observation in a naturalistic context.
BACKGROUND
Registered nurses (RNs) are the largest group of professional health care providers [10]. The Statistical Abstract of the United States: 2004–2005 reports 2,449,000 registered nurses in 2003, almost 3 times as many as the next largest group, physicians (819,000), in the United States [11].
Most nurses work in hospitals [12], and the majority of hospital employees are nurses [13]. They are responsible not only for following physician orders and performing routine duties, but also for maintaining a constant surveillance of their patients, especially in a critical care unit. Nurses also gather and transmit information from the patient's family to other health care providers and sometimes even between the patient and the patient's family [14]. Hospital nurses, especially critical care nurses, are responsible for coordinating all care for the patients in their charge [15]. Their on-duty information behavior in this information ecology [16] can literally be a matter of life and death.
Nurses work with people and information sources in an information ecology built by tradition and rituals from a pre-digital era [17]. Their tools for gathering and recording information are rapidly changing from paper systems to digital systems.
The Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) specifies “information management” as one of the major hospital functions. JCAHO has standards and guidelines for (a) “patient specific information,” (b) “aggregate information,” and (c) “knowledge based information” [18].
In support of the nursing process, most nursing educators and librarians advocate evidence-based practice (more specifically, evidence-based nursing), which requires extensive use of knowledge-based information. This approach uses overlapping principles from the older practice of nursing research utilization and that of evidence-based medicine [19].
LITERATURE REVIEW
Most studies of nurses' (and other health care providers') knowledge-based information seeking have been done in academic contexts [20]. Indeed, some medical librarianship literature treats hospital libraries as if they were academic medical libraries in miniature [21].
Most studies of health care providers' information behavior are studies of physicians, and few of those are observational [21–24]. Most hospitals are community hospitals and not teaching hospitals; most studies of the information behavior of health care providers have been done in teaching hospitals. McKnight and Peet [20] have demonstrated that some, purporting to be studies of health care providers, are actually studies of students.
Hospital librarians report that even though nurses are the largest group of hospital employees, they are not the largest group of hospital library users. There is little literature about hospital nurses seeking knowledge-based information from any source. Most are library-centric surveys that ask nurses to report their use of library materials [3–10, 25]. Bunyan, Lutz, and DuMont [2] have noted that hospital library services are usually designed more for physicians' information-seeking behavior than nurses'. They conducted a small ethnographic study of nurses on duty in several types of hospital units. The nurses they studied sought information to help them care for individual patients. However, they used research literature very rarely and then only used what was available on the unit, because they could not leave their patients. This research is more extensively reviewed elsewhere [26].
METHODOLOGY
This study used participant observation and in-context interview techniques for ethnographic rich data collection and the constant comparison method for analysis. In such fieldwork, the investigator and people work so closely together that they are all considered participants, not researcher and subjects. The holistic research questions are open and seek evidence inductively from the observation data rather than deductively from hypothesis testing.
Forsythe [27] explains that asking people to describe their information behavior is less trustworthy than direct observation, because (a) self-report (like eyewitness testimony in court) is often neither accurate nor complete; (b) respondents may believe that their answers reflect their level of professional competence; and (c) investigators may not understand the context of respondents' answers.
For this study, the author selected a 20-bed critical care unit in a 275-bed community, nonteaching hospital. This unit was chosen because (a) I could concentrate my observations on individual RNs who did not work with nurses' aids and (b) my experience was that critical care nurses were some of the most frequent library users of nurses in the hospital where I worked at the time. The hospital was chosen because it had an institutional review board (IRB). Research is rarely conducted in community hospitals, so most do not have an IRB. This hospital had recently instituted an IRB so oncology physicians could enter their patients in clinical trials. This nonprofit hospital is in a suburban city in United States Census Division 7, West South Central. The hospital's city has a university campus, but the hospital has no affiliation with that university.
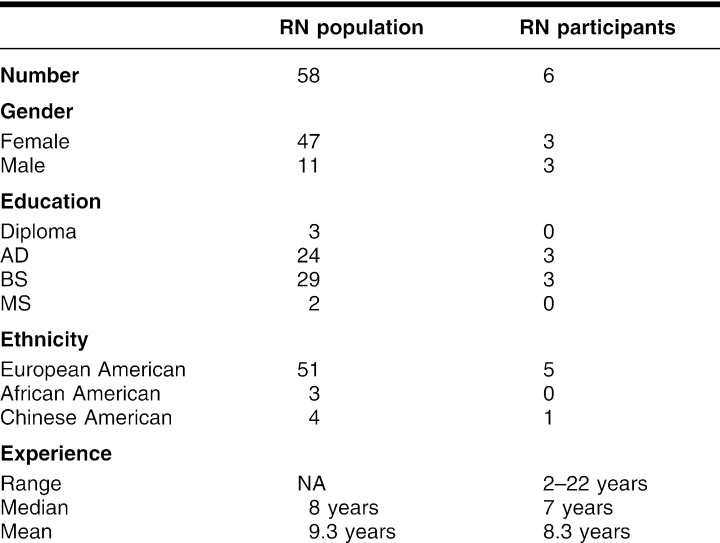
The six RN participants in this study constituted a purposeful sample of the staff in gender, education, and experience, as presented in Table 1. As the participant-observer-researcher, I accompanied each RN participant for one shift (from 4 to 13 hours) for a total of fifty hours of field work. I made observations on weekdays (7:00 a.m. to 7:00 p.m.), weekday nights (7:00 p.m. to 7:00 a.m.), weekend days, and weekend nights. No shift was on a holiday. My conceptual stance, a belief in the importance of published literature for health care providers, derived from my eighteen years of experience as a hospital librarian. I was significantly familiar with health care vocabulary and hospital culture, at least from the viewpoint of an ancillary professional service. I previously experienced nurses' knowledge-based information seeking in a hospital library setting. During the observations, I dressed as a hospital employee (my badge identified me as a librarian) but not as a nurse.
Table 1 Unit nurse population and participants
The hospital's administration, vice president of nursing, director of critical care, and manager of the critical care unit supported the study and were aware of how rarely research is conducted in community hospitals. They understood that they would not pick or be told who the participants were. The participants were recruited through flyers, departmental meetings, and word of mouth. I emphasized to the participants that (a) I was not a nurse and would not be judging anyone's professional competence, (b) I would protect participants' confidentiality as much as possible (except that during observations other staff might notice me accompanying the participant), and (c) I was in no way a change agent for the institution. Furthermore, I told the nurses that, if at any time, they perceived my presence as interfering with patient care, they should give a hand sign (a quick flash of the palm with all fingers spread) and I would leave immediately. I left the patient room during some intimate procedures, but the signal was never used during the study. Each of the participants volunteered privately at different times. At least one nurse volunteered after having seen me accompanying another nurse on the unit and expressed a belief that I should observe a nurse different from the one she had seen me observing.
The institutional review boards of both the University of North Texas and the hospital approved the research plan, the informed consent forms, and all of the privacy and confidentiality procedures for participants, patients, and other people. The hospital, the unit, and all of the individuals involved (except the researcher) are not named in any publications of this study.
I used the EasyScript speedwriting method for my field notes while I accompanied each on-duty participant. Earlier studies of physicians had determined that taking any kind of audio- or video-recording equipment into a patient care area was too intrusive [28, 29]. I recorded observed actions, conversations, and some on-the-scene memos. From time to time, I asked questions in context. As a participant observer, I frequently helped the nurse participant with small tasks such as moving a patient or unwrapping components of a patient's meal, while the nurse participant was present. At one point, I noticed and alerted the nurse participant to a change in a cardiac rhythm on an electrocardiogram monitor.
Sometime toward the end of the shift, when the nurse could take a short break, I engaged the participant in a private, audio-recorded interview. The interview usually lasted twenty to twenty-five minutes.
As soon as possible (within 24 hours), I transcribed all of the observation notes and the recorded interview. I used a member check technique [30] to verify the accuracy and validity of my observations. I gave each participant a copy of the transcript within hours of its completion and asked the participant for revisions.
I immediately began open coding, in vivo coding, and axial coding of the transcribed field notes and interviews [31]. I developed axial (hierarchical) codes in four conceptual tree structures (including information behaviors, information sources, information uses, and information kinds) with open codes for concepts that emerged during the data gathering. An example of an open code was “nurse's personal notes” and an example of an in vivo code (based on participants' own words) was “reading on duty.” By the end of the post-observation analysis, I used fifty-five open or in vivo and sixty-four axial codes for paragraphs of data. I used Non-numerical Unstructured Data Indexing Searching and Theorizing (NUDIST) qualitative research software and its later version, N6, to record my concurrent coding and to index the data for later retrieval.
The data were 4,236 paragraphs of text, each indexed with 1 or more codes. Fewer than 250 of these paragraphs described activities that were not information behavior. The concurrent memos constitute another 406 paragraphs. Analysis continued after the end of the observations with selective coding, triangulation from other sources (e.g., critical care nursing textbooks and conversations with nurses, nurse educators, and nurse managers who were not study participants), and grounded theory development [26].
FINDINGS
Observable information-seeking behavior and sources of information
The on-duty critical care nurses constantly sought information from people, patient record systems, monitoring and other computer systems, and notice boards but very rarely from published sources of information. They sought information verbally (in both oral and text media) and through their senses of sight, smell, sound, and touch. They did not use the sense of taste for on-duty information seeking. These nurses frequently used patient assessment protocols during the shift, and they checked and rechecked the contents of the chart many times. Occasionally, they asked questions, but much of their information seeking could be described as monitoring or scanning the environment. In general, they did not seek any information unrelated to their current patients.
The nurse participants sought information from people, including patients, other nurses, family members, physicians, and other health care workers. Of their informative interactions with people, most were with patients and patients' real-time physiological monitoring devices. Sometimes when they asked the patients questions, they were seeking only a factual answer, but more often they were also establishing a relationship with the patient and assessing the patient's cognitive, emotional, and psychosocial state.
The nurses sought information from other nurses less often than they did from patients. They read nurses' notes in the patients' charts, but most of their informative interaction with other nurses was oral—usually in person but occasionally on the telephone. They “took report” from their patients' previous nurses, “gave report” to the nurses who were about to care for their patients, and often asked other nurses for social and logistic information.
The nurses asked physicians questions during the brief periods of time when the physicians were on the unit. On the occasions when they tried to contact a physician by telephone, the process required a series of calls, pages, and messages.
They communicated frequently with the unit secretary, a gatekeeper who directed many kinds of information flow in the unit and with other hospital departments and patient care units. The nurses frequently asked questions of other health care providers (or health care workers) who came on the unit, particularly the clinical pharmacists.
Their typical conversations with doctors of pharmacy were longer than their conversations with doctors and doctors of osteopathy. As Byrd has written, health information professionals could well take the change in pharmacists' practice from the pharmacy to the clinical unit as a model for transforming “its professional training and practice roles for more effective work in clinical health care settings” [32].
The nurses sought some information from the people who knew the patient best, the patient's family and friends. Often, the patient's visitors were eager to do whatever they could to help the patient, and that included telling the nurse more about the patient.
The paper and digital elements of the patient's record, collectively and colloquially called “the chart” by the nurses, were the critical care nurses' largest source of information. The nurses sought information from the chart immediately after receiving an oral report from the patient's previous nurse, even before seeing the patient. The nurses returned to different parts of the chart many times during a shift.
The participants sought information from many different computer systems. They appeared to be comfortable with and skilled in the technology. Most of the participants used computers at home, and some even had their own Websites. In contrast, the physicians rarely paid much attention to the online functions of the systems, preferring to read printouts. Some computer systems on the unit were for patient records, others were for monitor systems and administrative functions.
They used other sources for information, including white boards and bulletin boards. Only twice in the fifty hours of observation did any of the participants independently seek information from published print sources. One used a telephone book, and another read part of the instruction manual for a monitor system. The participant nurses checked readings on various pieces of equipment, including thermometers, glucometers, bed scales, and ventilators. They read the time from their watches and clocks. They paid attention to the television sets in the patients' rooms only to make conversation with a patient about what the patient was watching.
Kinds of information and choice of questions to pursue
The critical care nurses' information seeking often did not take the form of a syntactic question or an articulated query. The process of acquiring new information, very broadly described as questioning, could also be browsing or scanning the environment, monitoring, encountering, and being aware of new information. It had a quality of vigilant surveillance. While the nurse was charting, she was also aware of people in her vicinity and of sounds from equipment alarms and patients' rooms. When a nurse entered a patient's room, she was aware of anything that was out of the ordinary in the room, even while performing a routine assessment.
The kinds of information that health care providers use could be classified according to the categories of information Gorman [33] observed physicians using: (a) patient data, corresponding to JCAHO's patient-specific information [18]; (b) population statistics or epidemiological information, generally corresponding to JCAHO's “aggregate information” [18]; (c) medical knowledge, generally corresponding to JCAHO's “knowledge based information” [18]; (d) logistic information; and (e) social information.
In addition to patient-specific information, these nurses sought and used some social and logistic information to help them care for their patients and do their jobs. They were observed seeking, using, and passing on only a small amount of knowledge-based information. In no instance were they observed in any activity involving epidemiologic information.
The participant nurses' chose to pursue questions based on their sense of responsibility to the patient and the patient's chart. They pursued social and logistic questions that they believed were necessary for the care of the patient. Other kinds of questions always had a much lower priority for these nurses.
The critical care nurse had questions not only about social information about the patient, but also about other health care workers. For instance, some physicians did not want a nurse to call during the night with patient information, the same information that other physicians would definitely want a nurse to call in at any time. The nurses discussed with each other what pleased and displeased different physicians.
Sometimes nurses had logistic questions. Procedures and contacts changed, especially as automated systems replaced manual ones. Logistic questions might be as simple as where something was kept or as complicated as how to use a particular program. Critical care nurses might work at more than one hospital, and some processes were different at one hospital from what they were at another.
The nurses very rarely sought knowledge-based information on duty, and, when they did, they most often asked colleagues rather than “looked it up.” Although the unit had some reference books and Internet access from one of the computers, I only once observed (and participated in) seeking knowledge-based information from those sources. Surprised by this, I frequently asked about it in the interviews. The participants knew, of course, that I was a librarian and, in the interviews, might have inflated their use of knowledge-based information to seek my approval. Even so, a common theme was that there simply was not enough time to read (from a book or from a computer) on the job. Some expressed the opinion that it was ethically and morally wrong for on-duty nurses to take time away from patient care “to read.” It did not matter whether the reading was from a book or an online source, it was still perceived as taking time away from their duties. They said that a personal information service available to them at all hours of the day or night would be very useful.
Barriers to information acquisition
Major observed barriers to information acquisition included illegible handwriting, difficult navigation of computer systems, equipment failure, unavailable people who had information, and social protocol barriers. Some confusion resulted from busy peoples' mistakes during interactions with multiple complex systems, creating other barriers to information acquisition. Sometimes the nurses could not find the information they needed because (a) they could not figure out how to get to the part of the system they expected to have the information; (b) it was not recorded where they expected it to be; or (c) it had never been recorded at all. As mentioned above in the discussion of kinds of information, the nurses did not have time to read knowledge-based information sources even if they could easily find them.
The nurses encountered barriers to information acquisition in both manual and computer systems. The most common problem in manual systems was illegible handwriting. Electronic records systems eliminated the difficulties of handwriting interpretation. However, navigability of electronic systems presented another set of barriers to finding information. Nurses often needed to look back over a patient's record for a period of time so that they could be aware of any important changes. I saw nurses on the night shift reminding each other to print-out vital signs records before midnight. The system would only allow access to the current day, but a nurse working 7:00 p.m. to 7:00 a.m. needed data from 2 different calendar days.
One person wholly concentrating on using one complex system was one thing; many people dealing with several complex systems at once was quite another. Something might be different in one information system from what was in another. Someone who was interacting with one information system (human, paper, or automated) might be interrupted with another and not complete the task begun in the first system. The resulting ambiguous, conflicting, or missing messages could create barriers to information the nurse needed.
Other observed barriers to information acquisition included library hours, misplaced papers, inaccurate telephone numbers, delayed results of lab tests, and forgotten information.
Other relevant observations
While most of the participant nurses showed or expressed a high regard for their continuing education and for practice based on good research, they had no way to follow the formal steps of evidence-based nursing on duty. Any research that they might do had to be done off duty and off the pay clock. Their vigilant surveillance of their patients precluded any reading on duty.
All nurses displayed and expressed frustration with their on-duty time management challenges, especially charting. They were skilled at multitasking but feared making serious mistakes by missing something important. Most believed that their data recording systems (both on paper and online) had too many redundancies that wasted their time.
SUMMARY, RELIABILITY, AND LIMITATIONS
The observable on-duty information behavior of the participant nurses was patient centric. They sought information from people, from the patient's chart, from computer systems, and from other information sources. The information they used was patient specific, social, and logistic. They occasionally sought knowledge-based information but were not observed seeking epidemiological information. Their decisions to pursue questions were based on their judgment of how important the answer would be to the care of the patient. They encountered barriers to information acquisition in both paper and online systems. Equipment failure, unavailable people, social protocols, and mistakes caused by simultaneously using multiple complex systems hampered their information-seeking efforts.
Member checking, the participant's review of my transcript of my field notes, helped verify the accuracy of the data. After reading the transcripts, the participants often commented that they had not realized how often they had some interactions. The use of thick description enriched the credibility of the data and the reliability of the findings.
The fact that I, as researcher and participant observer in this study, was not a nurse was both a limitation and a strength of the study. This study did not begin with a particular nursing theory or formal process, but rather with observation of nurses' information behavior. I did not consider how best the nurse should care for a patient, but focused on the observed information behavior.
The participant nurses could, of course, have altered their behavior because of my presence. While I occasionally detected some “performance” behavior at the beginning of a shift, I believe that the nurses' work was so constant and intense that they could not keep that up very long. Observational qualitative research requires the researcher to refine and improve observations with experience. At the beginning of a particular pilot observation, my perception of the exotic drama of a critical care unit prompted the participant to recount stories that fit that perception. The stories ceased, however, when the nurse and I focused on current events rather than the nurse's memories of events on other shifts.
This study described the behavior of one group of people at one time in one setting, and the results are not generalizable to all settings. The participants were all volunteers who expressed pride in their profession but did not appear to restrain themselves from expressing their frustrations. It was possible that some of the nurses in the unit who did not volunteer were not as happy with their jobs.
Just because none of these nurses were observed reading knowledge-based information or pursuing epidemiologic information, one cannot assume that that never happens—just that it did not happen during these observations. Likewise, it would not be unusual for critical care nurses' patients to die, but none did during these observations.
Replication of this study or other studies that quantitatively measure nurses' observed information behaviors could be very useful.
IMPLICATIONS FOR PRACTICE
Librarians serving schools of nursing usually teach nursing students how to use information-retrieval resources for their schoolwork and research papers. Frequently, they teach nurses skills for evidence-based practice. These activities require time not only for information gathering, but also for thoughtful reflection. No one can retrieve reliable literature and systematically review it while watching monitors, checking on patients, administering and verifying therapies, and answering telephone calls.
The intelligent and educated nurses who participated in this study are all passionate about giving their patients the best care possible. They respect research-informed practice and want the best of what academia and libraries can give them to support the care of their patients. However, their duties leave little room for such pursuits. These critical care nurses have neither time nor opportunity to use most of their academic skills on duty. Given the economic realities of health care, hospital administrators are unlikely to pay nurses for off-duty time for such pursuits. What research that nurses do, they have to do on their own time.
Librarians serving working nurses in hospitals must be wary of using academic models for delivery of their information services. On-call ready reference service (an expert reference interview followed by information retrieval incorporating literature and filtering and highlighting pertinent passages) would provide these nurses with more reliable knowledge-based information than they currently get by asking other people. It does not matter whether the knowledge-based information is delivered on paper or online; nurses still do not have time to read more than a few paragraphs on the job.
Hospital-based pharmacists are providing limited knowledge-based information services [26]. Librarians, with their broader knowledgebase and professional information-retrieval skills, can provide better on-demand information services than pharmacists can.
In light of the nurses' observed and expressed preference for a professional presence in their unit as an information source, it would appear that a clinical informationist [34–36] could be very valuable to them. Such a person would provide the reliable knowledge-based information they do not have time to gather while on duty.
Footnotes
This article has been approved for the Medical Library Association's Independent Reading Program.
REFERENCES
- Dalrymple PW. Improving health care through information: research challenges for health sciences librarians. In: Lynch MJ, ed. Research questions for the twenty-first century. Libr Trends. 2003 Spring; 51(4):525–40. [Google Scholar]
- Bunyon L, Lutz E, and DuMont R. Application of the “sense-making” model in designing library services for nurses. In: Medical libraries: keys to health information: Proceedings of the 6th International Congress on Medical Librarianship; New Delhi, India; 24–28 Sep 1990. New Delhi, India: Medical Library Association of India, 1990. [Google Scholar]
- Bunyon L, Lutz EM. Marketing the hospital library to nurses. Bull Med Libr Assoc. 1991 Apr; 79(2):223–5. [PMC free article] [PubMed] [Google Scholar]
- Gonnerman K. The health sciences library and professional librarians: important resources for busy ED nurses and nurse managers. J Emerg Nurs. 2003 Apr; 29(2):183. [DOI] [PubMed] [Google Scholar]
- Layton B, Hahn K. The librarian as a partner in nursing education. Bull Med Libr Assoc. 1995 Oct; 83(4):499–502. [PMC free article] [PubMed] [Google Scholar]
- Royle JA, Blythe J, DiCenso A, Bauman A, and Fitzgerald D. Do nurses have the information resources and skills for research utilization? Can J Nurs Admin. 1997 Sep; 10(3):9–30. [PubMed] [Google Scholar]
- Spath M, Buttlar L. Information and research needs of acute-care clinical nurses. Bull Med Libr Assoc. 1996 Jan; 84(1):112–6. [PMC free article] [PubMed] [Google Scholar]
- Wakeham M. Nurses—their information needs and use of libraries: the views of some librarians. Health Libr Rev. 1993 Jun; 10(2):85–94. [DOI] [PubMed] [Google Scholar]
- Wakeham M. What nurses think of library services: a research study. Nurs Stand. 1996 Apr 3; 10(28):40–3. [DOI] [PubMed] [Google Scholar]
- Blythe J, Royle JA. Assessing nurses' information needs in the work environment. Bull Med Libr Assoc. 1993 Oct; 81(4):433–5. [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau. Statistical abstract of the United States: 2004–2005 the national data book (table 597). 124th ed. [Web document]. The Bureau. [rev. 8 Dec 2004; cited 27 Dec 2004] <http://www.census.gov/statab/www/>. [Google Scholar]
- Marriott J, Mable AL. Opportunities and potential: a review of international literature on primary health care reform and models. Ottawa, ON, Canada: Health Human Resource Strategies Division, Health Policy and Communications Branch, Health Canada, 2000. [Google Scholar]
- Mayer G. The impact of managed care on hospital nursing. Best Pract Benchmarking Healthc. 1997 Jul/Aug; 2(4):162–7. [PubMed] [Google Scholar]
- Clarke SP, Aiken LH. Failure to rescue: needless deaths are prime examples of the need for more nurses at the bedside. Am J Nurs. 2003 Jan; 103(1):42–7. [DOI] [PubMed] [Google Scholar]
- Thelan LA, Lough ME, Urden LD, and Stacy KM. Critical care nursing diagnosis and management. 3rd ed. St. Louis, MO: Mosby, 1998. [Google Scholar]
- Nardi BA, O'Day VL. Information ecologies: using technology with heart. Cambridge, MA: The MIT Press, 1999. [Google Scholar]
- Brewer CS, Frazier P. The influence of structure, staff type, and managed-care indicators on registered nurse staffing. J Nurs Adm. 1998 Sep; 28(9):28–36. [DOI] [PubMed] [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations. CAMH: comprehensive accreditation manual for hospitals: the official handbook. Oakbrook Terrace, IL: The Commission, 2004. [Google Scholar]
- McKibbon KA. Evidence-based practice. Bull Med Libr Assoc. 1998 Jul; 86(3):396–401. [PMC free article] [PubMed] [Google Scholar]
- McKnight M, Peet M. Health care providers' information seeking: recent research. Med Ref Serv Q. 2000 Summer; 19(2):27–50. [DOI] [PubMed] [Google Scholar]
- McKnight M. Building a useful hospital library book collection. National Network. 1996 Aug; 21(1):10–1. [PubMed] [Google Scholar]
- Detlefsen EG. The information behaviors of life and health scientists and health care providers: characteristics of the research literature. Bull Med Libr Assoc. 1998 Jul; 86(3):385–90. [PMC free article] [PubMed] [Google Scholar]
- Case DO. Looking for information: a survey of research on information seeking, needs, and behavior. Amsterdam, The Netherlands: Academic Press, 2002. [Google Scholar]
- Dawes M, Sampson U. Knowledge management in clinical practice: a systematic review of information seeking behavior in physicians. Int J Med Inform. 2003 Aug; 71(1):9–15. [DOI] [PubMed] [Google Scholar]
- Pettengill MM, Gillies DA, and Clark CC. Factors encouraging and discouraging the use of nursing research findings. Image J Nurs Sch. 1994 Summer; 26(2):143–7. [DOI] [PubMed] [Google Scholar]
- McKnight M. An observational investigation of on-duty critical care nurses' information behavior in a nonteaching community hospital. Diss Ab Int 2004;65/03,740A. (UMI no.: AAT 3126579.). [Google Scholar]
- Forsythe DE. Using ethnography to investigate life scientists' information needs. Bull Med Libr Assoc. 1998 Jul; 86(3):402–9. [PMC free article] [PubMed] [Google Scholar]
- Forsythe DE, Buchanan BG, Osheroff JA, and Miller RA. Expanding the concept of medical information: an observational study of physicians' information needs. Comput Biomed Res. 1992 Apr; 25(2):181–200. [DOI] [PubMed] [Google Scholar]
- Osheroff JA, Forsythe DE, Buchanan BG, Bankowitz RA, Blumenfeld BH, and Miller RA. Physicians' information needs: analysis of questions posed during clinical teaching. Ann Intern Med. 1991 Apr 1; 114(7):576–81. [DOI] [PubMed] [Google Scholar]
- Glesne C. Becoming qualitative researchers: an introduction. New York, NY: Longman, 1999. [Google Scholar]
- Cresswell JW. Qualitative inquiry and research design: choosing among five traditions. Thousand Oaks, CA: Sage, 1998. [Google Scholar]
- Byrd GD. Can the profession of pharmacy serve as a model for health informationist professionals? J Med Libr Assoc. 2002 Jan; 90(1):68–75. [PMC free article] [PubMed] [Google Scholar]
- Gorman PN. Information needs of physicians. J Am Soc Inf Sci. 1995 Dec; 46(10):729–36. [Google Scholar]
- Davidoff F, Florance V. The informationist: a new health profession? Ann Intern Med. 2000 Jun 20; 132(12):996–8. [DOI] [PubMed] [Google Scholar]
- Lyon J, Giuse NB, Williams A, Koonce T, and Walden R. A model for training the new bioinformationist. J Med Libr Assoc. 2004 Apr; 92(2):188–95. [PMC free article] [PubMed] [Google Scholar]
- Shipman JP, Cunningham DJ, Holst R, and Watson LA. The informationist conference: report [special report]. J Med Libr Assoc. 2002 Oct; 90(4):458–64. [PMC free article] [PubMed] [Google Scholar]