Abstract
Bile acids (BAs), a group of structurally diverse molecules that are primarily synthesized in the liver from cholesterol, are the chief components of bile. Besides their well-established roles in dietary lipid absorption and cholesterol homeostasis, it has recently emerged that BAs are also signaling molecules, with systemic endocrine functions. BAs activate mitogen-activated protein kinase pathways, are ligands for the G-protein-coupled receptor TGR5, and activate nuclear hormone receptors such as farnesoid X receptor α. Through activation of these diverse signaling pathways, BAs can regulate their own enterohepatic circulation, but also triglyceride, cholesterol, energy, and glucose homeostasis. Thus, BA-controlled signaling pathways are promising novel drug targets to treat common metabolic diseases, such as obesity, type II diabetes, hyperlipidemia, and atherosclerosis.
Keywords: bile acids, gene expression, metabolism, nuclear receptors, signaling
Introduction
Bile consists of bile acids (BAs), cholesterol, phosphatidylcholine, and bilirubin, and is secreted from the hepatocytes into the bile canaliculi. BA synthesis from cholesterol is the prime pathway for cholesterol catabolism. BAs are amphipathic molecules, which contain a sterol nucleus with hydroxyl groups and a side chain that terminates in a carboxyl group. Their amphipathic nature is essential to solubilize dietary lipids, which subsequently promotes their absorption in the digestive tract. The principal BAs include in humans the primary BAs cholic acid and chenodeoxycholic acid (CDCA), their glycine and taurine conjugates, and the secondary BAs deoxycholic acid and lithocholic acid (Figure 1A). In mice, CDCA is efficiently converted into muricholic acid and BAs are almost exclusively conjugated to taurine. Most of the BAs are present within the enterohepatic organs. Usually BAs are stored in the gallbladder; however, when a meal is ingested, they flow into the duodenum and intestine. The BAs are efficiently (95%) absorbed again by passive diffusion and active transport in the terminal ileum, and transported back to the liver via the portal vein. In the liver, the BAs are taken up at the basolateral (sinusoidal) membrane and exported again at the apical (canalicular) membrane of the hepatocytes into the bile canaliculus (transhepatic BA flux). This completes their enterohepatic circulation. Each BA molecule may complete 4–12 cycles between the liver and intestine per day (Cohen, 2003). Owing to this efficient recirculation, only a small amount of the BA pool size is derived from de novo biosynthesis. Several reviews describe BA biosynthesis with its enzymes, genetics, and regulation in detail (Chiang, 2002; Russell, 2003).
Figure 1.
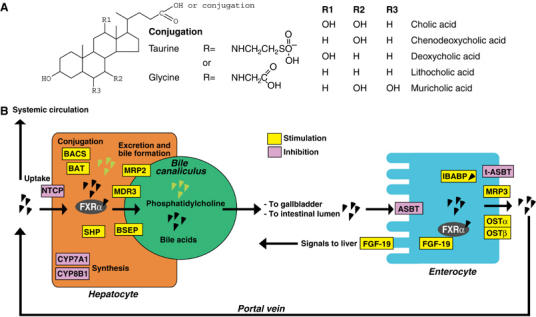
(A) Structure of selected BAs. (B) FXRα target genes involved in the enterohepatic recycling and detoxification of BAs. Genes whose expression is directly induced by BAs and FXRα are in yellow rectangles; those in pink rectangles are inhibited by BAs. BACS, BA-CoA synthetase; BAT, BA-CoA: amino acid N-acetyltransferase; BSEP, bile salt export pump; MDR3, multidrug resistance 3 p-glycoprotein; MRP2, multidrug resistance-associated protein 2; IBABP, ileal BA-binding protein; CYP8B1, sterol 12α-hydroxylase; NTCP, sodium taurocholate cotransporting polypeptide; ASBT, apical sodium-dependent bile salt transporter.
Besides its roles in dietary lipid absorption and cholesterol homeostasis, it has become clear that BAs are also signaling molecules. Three major signaling mechanisms have been identified. BAs activate mitogen-activated protein kinase (MAPK) pathways (Gupta et al, 2001; Qiao et al, 2003), are ligands for the G-protein-coupled receptor (GPCR) TGR5 (Maruyama et al, 2002; Kawamata et al, 2003), and activate nuclear hormone receptors such as farnesoid X receptor α (FXRα; NR1H4) (Makishima et al, 1999; Parks et al, 1999; Wang et al, 1999). The discovery of BAs as the endogenous FXRα ligands suggested a function for them in the enterohepatic recycling of BAs and the feedback regulation of BA biosynthesis, which is in line with the reported expression pattern of FXRα in liver and intestine (Forman et al, 1995). In these tissues, FXRα activation protects against accumulation of BAs, which is toxic, via mechanisms that have been reviewed recently (Chiang, 2002; Russell, 2003; Houten and Auwerx, 2004). To summarize (Figure 1B), FXRα activation in the liver leads to increased conjugation of BAs, followed by the excretion of BAs from the hepatocyte into the bile canaliculus, leading to an increase in the formation of bile. In the intestine, FXRα activation leads to increased expression of a protective BA-binding protein and the basolateral BA transporters (organic solute transporter (OST) α and β). Of particular interest is the FXRα-mediated induction of short heterodimer partner expression (SHP, NR0B2). SHP is an atypical nuclear hormone receptor that only has a ligand-binding domain and no DNA-binding domain and inhibits the activity of several nuclear receptors. The SHP induction underlies the negative feedback regulation of BA biosynthesis and uptake via a mechanism that will be described below. In this review, we will focus on the recent interest in BAs as general regulators of metabolic homeostasis and the mechanisms by which BAs can exert these functions.
BAs regulate lipid metabolism
Besides its roles in BA homeostasis, increasing evidence is emerging for an important role of FXRα in lipid metabolism. BAs decrease their own biosynthesis from cholesterol, through an elaborate feedback inhibitory circuit, which starts by BA-mediated activation of FXRα, which will in turn induce the expression of SHP. In rodents, SHP then binds and interferes with the activity of two nuclear receptors, liver X receptor α (LXRα, NR1H3) and liver receptor homolog-1 (LRH-1, NR5A2) (Goodwin et al, 2000; Lu et al, 2000; Brendel et al, 2002), both necessary for transcriptional activation of the cholesterol 7α-hydroxylase (CYP7A1), the rate-limiting enzyme in BA biosynthesis from cholesterol. Significant differences exist in BA homeostasis of rodents, humans, and other model organisms. Most notably, differences have been documented in the regulation of CYP7A1 promoter activity by LXRα. The regulation of other key pathways such as the FXRα-mediated induction of SHP, however, is well conserved between species. Therefore, a high transhepatic BA flux, which translates in FXRα activation, positively correlates with hepatic and LDL-cholesterol levels, since cholesterol is not eliminated via its conversion to BAs. HDL levels are negatively correlated with transhepatic BA flux (Figure 2; Schoenfield and Lachin, 1981; Leiss and von Bergmann, 1982). Several genes with a role in HDL metabolism are FXRα targets and have been reviewed recently (Francis et al, 2003).
Figure 2.
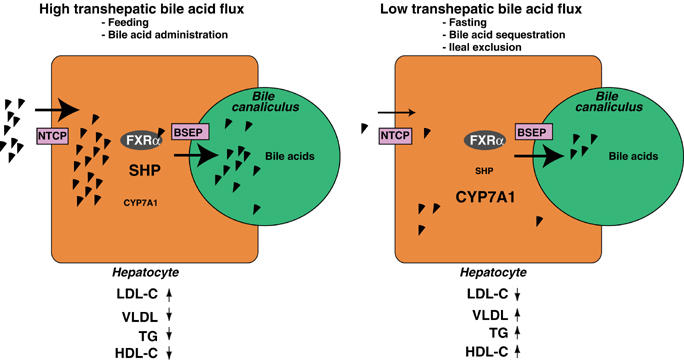
Respective situations that cause high (left panel) and low (right) transhepatic flux of BAs and their principle functional consequences.
Interestingly, BAs also affect triglyceride homeostasis. In fact, for a long time it has been known that in man there is an inverse relationship between the transhepatic BA flux and hepatic VLDL production. Treatment with BA-binding resins, ileal exclusion, or bile withdrawal interrupts the enterohepatic circulation, decreasing transhepatic BA flux (Figure 2). All these interventions induce the production of VLDL (Grundy et al, 1971; Nestel and Grundy, 1976; Angelin et al, 1978). Conversely, treatment of cholesterol gallstones with the BA CDCA increases the BA pool and consequently the transhepatic BA flux, and reduces hypertriglyceridemia (Figure 2) (Miller and Nestel, 1974; Angelin et al, 1978).
The direct ability of BAs to modify gene expression by activating FXRα can explain these effects. Indeed, FXRα was shown to induce human and rodent apolipoprotein C-II (apoC-II) expression (Kast et al, 2001). ApoC-II is a coactivator of lipoprotein lipase and its induction lowers serum triglycerides. During fasting in rodents, FXRα mRNA levels are increased by two nuclear hormone receptors, peroxisome proliferator-activated receptor γ (PPARγ, NR1C3) and hepatic nuclear factor 4α (HNF4α, NR2A1) (Zhang et al, 2004). FXRα is furthermore coactivated by PPARγ coactivator-1α (PGC-1α) in a ligand-dependent or -independent way (Kanaya et al, 2004; Zhang et al, 2004; Savkur et al, 2005). PGC-1α is an important activator of hepatic gluconeogenesis, whereas in other tissues such as muscle and brown adipose tissue (BAT) it induces mitochondrial biogenesis and thermogenesis. These authors speculated that, during fasting, FXRα and PGC-1α cooperate to maintain energy homeostasis by decreasing serum TG levels via effects on VLDL clearance (Zhang et al, 2004).
We have shown that the induction of SHP via FXRα activation, which causes feedback inhibition of BA synthesis, also underlies the feedback regulation of hepatic fatty acid and triglyceride biosynthesis and VLDL production (Watanabe et al, 2004). In fact, SHP interferes with the expression of sterol regulatory element-binding protein-1c (SREBP-1c). SREBPs are transcription factors that are activated by proteolytic processing and are mainly known for their control of genes involved in cholesterol homeostasis, effects mainly mediated by SREBP-2 (Horton et al, 2002). SREBP-1c is the master regulator of fatty acid and triglyceride biosynthesis and controls the expression of genes involved in various aspects of lipogenesis, such as acetyl-CoA carboxylase 1 (ACC1), ACC2, fatty acid synthase, glucose-6-phosphate dehydrogenase, and malic enzyme (Horton et al, 2002). Importantly, expression of SREBP-1c is enhanced by insulin, which explains why insulin enhances the conversion of glucose to fatty acid (Foretz et al, 1999; Shimomura et al, 1999). Activation of LXRα and LXRβ by agonists has also been shown to induce SREBP-1c, accounting for the triglyceride-raising effects of LXR agonists (Repa et al, 2000; Schultz et al, 2000). We propose a mechanism by which SREBP-1c, LXRα, LRH-1, FXRα and SHP cooperate in regulating lipid homeostasis (Figure 3). SREBP-1c and CYP7A1 expression is elevated by oxysterol-induced LXRα activation in cooperation with LRH-1, which increases triglyceride and BA biosynthesis. FXRα-mediated induction of SHP interferes with the activity of LXRα and LRH-1 to induce SREBP-1c and CYP7A1, and hence will inhibit lipogenesis and BA biosynthesis.
Figure 3.
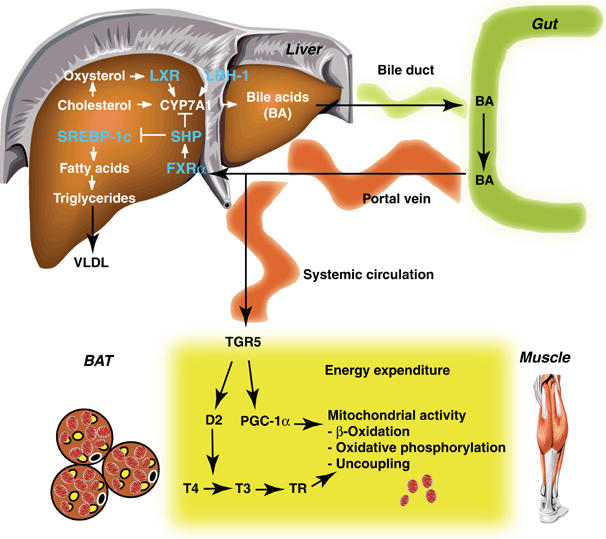
Schematic representation of the control of BAs on BA, triglyceride and energy homeostasis. TR, thyroid hormone receptor.
SHP expression levels are controlled by FXRα and as a consequence positively correlated with transhepatic BA flux. Interruption of the enterohepatic circulation will decrease transhepatic BA flux and consequently decrease SHP expression and thus increase BA biosynthesis. An increase in the BA pool will have the opposite effect (Figure 2). Therefore, SHP seems to be a pivotal factor in linking BA pool size with triglyceride levels. Consistent with this, SHP expression levels will be inversely correlated with serum triglyceride levels, a prediction confirmed by several studies. Hypertriglyceridemia and mild obesity have been associated with mutations in the SHP gene in Japanese patients (Nishigori et al, 2001). Later studies confirmed that genetic variation in SHP can influence birth weight and BMI, although it seems not to be a common cause of obesity (Hung et al, 2003; Mitchell et al, 2003). In contrast to humans with mutations in the SHP gene, SHP−/− mice have no hypertriglyceridemia and obesity; however, the study of these mice did show that the profound lowering of hepatic triglycerides observed with a CA diet was significantly attenuated in the SHP−/− mice (Kerr et al, 2002; Wang et al, 2002). FXRα−/− mice show increased serum and hepatic triglyceride levels due to an increase in the production of VLDL, which coincides with a decreased SHP expression (Sinal et al, 2000).
Several other genes, including apolipoproteins A-V, C-III, E, PPARα, syndecan-1, and VLDL receptor, that directly affect lipid and lipoprotein metabolism, have also been reported as FXRα target genes (reviewed in Claudel et al (2005) and references herein). Taken together, all these genes enhance triglyceride and VLDL metabolism and consequently lower serum VLDL and triglyceride levels, consistent with the described effect of BAs. In view of the atypical nature of the FXRα response elements identified in this set of genes, additional experiments are necessary to dissect whether they are physiologically relevant FXRα targets and to carefully define their exact contributions in the triglyceride-lowering effects of BAs.
BAs and energy homeostasis
BAs have been reported to inhibit diet-induced obesity and prevent the development of insulin resistance (Ikemoto et al, 1997), suggesting effects on energy homeostasis. We have recently shown that administration of BAs to mice increases energy expenditure in BAT, preventing obesity and insulin resistance (Figure 3; Watanabe et al, 2006). This metabolic effect of BAs is critically dependent on induction of the cAMP-dependent thyroid hormone activating enzyme type 2 iodothyronine deiodinase (D2), since it is lost in mice with a targeted disruption of D2 (D2−/−). BA treatment of brown adipocytes, but also human skeletal myocytes, increases D2 activity and oxygen consumption. These effects are independent of FXRα, and instead are mediated by increased cAMP production, that stems from the binding of BAs with the GPCR TGR5. TGR5 is a novel GPCR which responds to BAs by inducing receptor internalization, activation of MAPK pathways, and cAMP production (Maruyama et al, 2002; Kawamata et al, 2003). The most thermogenically important tissues of rodents (BAT) and humans (skeletal muscle) are specifically targeted by this mechanism because they coexpress D2 and TGR5 (Watanabe et al, 2006).
FXRα has been shown to regulate directly the expression of fibroblast growth factor-19 (FGF-19, mouse ortholog FGF-15). This secreted growth factor signals from the intestine to the liver through the cell-surface FGF receptor 4 (FGFR4) tyrosine kinase, resulting in an alternative pathway that potently suppresses CYP7A1 expression in a SHP-independent fashion (Figure 1B; Holt et al, 2003; Inagaki et al, 2005). Interestingly, transgenic mice which overexpress human FGF-19 display improved metabolic rate and decreased adiposity. This was attributed to increased BAT mass and enhanced liver β-oxidation due to decreased ACC2 expression (Tomlinson et al, 2002). A decreased ACC2 expression reduces the levels of malonyl-CoA that inhibit carnitine palmitoyl transferase 1 enzyme activity, the rate-limiting enzyme involved in the import of fatty acids into the mitochondrial matrix prior to their β-oxidation. Thus, the FXRα-mediated FGF-19 induction could also signal in an endocrine manner, mediating in part the effects of BAs on energy homeostasis.
SHP was recently also reported to inhibit PGC-1α expression and energy production in BAT, as concluded from the resistance of SHP−/− mice to diet-induced obesity (Wang et al, 2005). Further studies are, however, required to define whether this effect is directly due to the absence of SHP in BAT in the SHP−/− mice (normally SHP is expressed to very low levels in BAT) or perhaps to an indirect mechanism, subsequent to altered whole body BA homeostasis. It is expected that the characterization of tissue-specific SHP deficient animals will shed light on this issue in the near future.
BAs and glucose metabolism
An assessment of the efficacy and tolerability of cholestyramine in patients with dyslipidemia and type 2 diabetes, unexpectedly revealed that glycemic control was also improved with cholestyramine therapy (Garg and Grundy, 1994). Recently several studies addressed an eventual role of BAs in glucose metabolism, however, the contribution of FXRα in mediating the effects of BAs on glucose homeostasis is still highly debated. Whereas hepatic FXRα expression was reported to be increased by fasting, suggesting an inhibitory role of insulin levels on FXRα gene expression (Zhang et al, 2004), another study indicated that FXRα levels are decreased in animal models of diabetes and could be normalized by insulin addition (Duran-Sandoval et al, 2004). The role of FXRα in the regulation of gluconeogenesis is also unclear at present. BAs have been reported to inhibit gluconeogenesis via downregulation of phosphoenolpyruvate carboxykinase (PEPCK) mRNA levels in a FXRα-dependent and -independent manner (De Fabiani et al, 2003; Yamagata et al, 2004). In another paper, however, FXRα activation was shown to activate PEPCK via a mechanism that involved induction of PPARα and TRB3 (Stayrook et al, 2005). TRB3 is a fasting inducible inhibitor which prevents activation of the serine/threonine kinase Akt/PKB and mediates activation of gluconeogenesis during fasting and insulin resistance (Koo et al, 2004). Two recent studies indicated that FXRα activation might increase hepatic glycogen levels (Duran-Sandoval et al, 2005; Zhang et al, 2006). The control of FXRα on whole body glucose homeostasis, however, seems rather small and is limited to specific timepoints in the fasting/(re)feeding cycle.
The concept that the impact of BAs on whole body glucose homeostasis is indirect and the consequence of their major effects on body weight has gained support recently. In fact, via activation of the TGR5-D2 signaling pathway, BAs robustly increase mitochondrial activity and oxidative phosphorylation in BAT (in rodents) and skeletal muscle cells (in humans), which was associated with a remarkable insulin sensitization both in genetic and diet-induced models of diabesity (Watanabe et al, 2006). The effects of BAs on FGF-19 production could also contribute to enhanced mitochondrial activity (Tomlinson et al, 2002). In line with this, a number of independent and converging observations in animal models and humans have linked reduced mitochondrial function and oxidative phosphorylation with the development of type 2 diabetes (Lowell and Shulman, 2005). Finally, activation of TGR5 was also shown to induce the production of glucagon-like peptide-1, in vitro which improves insulin secretion, and also via this way could ameliorate whole body glucose homeostasis (Katsuma et al, 2005). This effect warrants further investigation in vivo.
BA signaling pathways as therapeutic targets to treat metabolic disease
As described in the previous sections, BAs have evolved over the last years from regulators of BA homeostasis to general metabolic integrators. It is therefore not too surprising that a number of BA-activated signaling pathways have become attractive targets in our fight against common metabolic diseases, such as obesity, type 2 diabetes, hyperlipidemia, and atherosclerosis.
FXR agonists
GW4064, the first reported high-affinity synthetic nonsteroidal FXRα agonist, was identified using high-throughput screening and combinatorial chemistry. GW4064 protects against cholestatic liver damage (Liu et al, 2003) and cholesterol gallstone disease (Moschetta et al, 2004), and lowers also serum triglyceride levels in KK-Ay and ob/ob mice (Watanabe et al, 2004) and in Fisher rats (Maloney et al, 2000). 6α-ethyl-CDCA (6-ECDCA), a high affinity steroidal FXRα agonist, has anticholestatic properties and protects the liver against LCA-induced necrosis and fibrosis (Pellicciari et al, 2005).
FXR antagonists and modulators
Guggulsterone, fexaramine and AGN34 are gene-selective FXRα modulators, which means that they can affect the expression of various FXRα target genes in different ways (antagonists or agonists) (Cui et al, 2003; Downes et al, 2003; Dussault et al, 2003). This phenomenon offers the possibility to develop FXRα modulators in which therapeutic effects are separated from undesired side effects. Most data are available for guggulipid, a plant extract containing the sterol guggulsterone, which is used to lower LDL cholesterol. This beneficial effect was attributed to its FXRα antagonizing activities (Urizar et al, 2002; Wu et al, 2002). In a recent clinical trial, however, guggulipid slightly but significantly increased LDL cholesterol (Szapary et al, 2003). In addition, guggulsterone lacks specificity for FXRα, since it interacts with numerous other nuclear receptors ((Meyer et al, 2005) and references herein).
TGR5 agonists
Activation of TGR5 induces energy expenditure in vivo and in cultured cells (Watanabe et al, 2006) and increases GLP-1 expression in cell lines (Katsuma et al, 2005). Due to these properties, synthetic TGR5 agonists could curb weight gain and improve glucose homeostasis, as claimed in the recent patent literature (Hinuma et al, 2005). Further in vivo work will be required to test whether these pharmacological compounds have the same efficacy as BAs, natural TGR5 agonists.
BAs as endocrine signaling factors, perspectives for the future
It is clear that BAs can affect metabolism, one question that remains is under which physiological conditions BAs exert this function. For this, it might be helpful to recapitulate where and when BAs can be found. BAs are together with other metabolites secreted from hepatocytes into the bile canaliculi. Usually bile is stored in the gallbladder, however, when a meal is ingested, it flows into the duodenum. The BAs are absorbed again by passive diffusion and active transport from the terminal ileum, and transported back to the liver via the portal vein, which completes their enterohepatic recirculation (Cohen, 2003). The first pass extraction of BAs by the liver is remarkably efficient (70–90%). Thus after a meal, BA levels in the hepatocyte will increase. The hepatic extraction rate of BAs usually remains constant during the fasting state and during digestion (Cohen, 2003). Consequently, a significant amount of BAs can spill over into the systemic circulation. Therefore, after a meal, BA levels will not only increase in the portal vein and the liver but also in the systemic circulation (Ho, 1976; Engelking et al, 1980). Indeed fasting serum BAs are usually below 5μM, whereas postprandial levels rise up to 15 μM (Everson, 1987). As a consequence of this phenomenon, serum BA levels vary during the day following a rhythm dictated by the ingestion of meals.
Based on these physiological observations it makes sense that BAs will exert their signaling functions mainly during feeding and active digestion. Under these conditions BAs are present in the intestine, return to the liver and spill over in the systemic circulation. BAs could hence be a signal to the liver and other organs that a meal has been ingested and that nutrients such as triglycerides will become available. BAs will then elicit a physiological response that is composite of FXRα-dependent (e.g. increased secretion of FGF-19) and -independent signaling (e.g. activation of the GPCR TGR5). A good example of such composite and converging signaling activities is given by the fact that BAs decrease hepatic VLDL production via the induction of the FXR–SHP–SREBP-1c pathway (Watanabe et al, 2004) and increase the (extra-)hepatic metabolism of VLDL and fatty acids through stimulation of β-oxidation via activation of the TGR5–cAMP–D2 pathway (Figure 3) (Watanabe et al, 2006).
This new hormonal signaling role for BAs also forces us to think about the potential role of FXRα in non-enterohepatic tissues. Indeed, FXRα is also expressed at a high level in the kidney and the adrenal cortex (Forman et al, 1995). However, to activate FXRα, an intracellular receptor, BAs need specific transporters such as OSTα/β to cross the cell membrane in these tissues (Lee et al, 2006). Since evidence of such transport has not been demonstrated in vivo, one needs to consider the existence of novel natural FXRα agonists in these tissues.
Acknowledgments
We acknowledge support by grants of CNRS, INSERM, ULP, Hôpital Universitaire de Strasbourg, NIH (DK59820 and DK067320), AFM, FRM, and the EU (QLRT-2001-00930 and LSHM-CT-2004-512013) and by fellowships from EMBO and FRM (to SMH). We apologize to those authors whose original work could not be quoted due to space restrictions.
References
- Angelin B, Einarsson K, Hellstrom K, Leijd B (1978) Effects of cholestyramine and chenodeoxycholic acid on the metabolism of endogenous triglyceride in hyperlipoproteinemia. J Lipid Res 19: 1017–1024 [PubMed] [Google Scholar]
- Brendel C, Schoonjans K, Botrugno OA, Treuter E, Auwerx J (2002) The small heterodimer partner interacts with the liver X receptor alpha and represses its transcriptional activity. Mol Endocrinol 16: 2065–2076 [DOI] [PubMed] [Google Scholar]
- Chiang JY (2002) Bile acid regulation of gene expression: roles of nuclear hormone receptors. Endocr Rev 23: 443–463 [DOI] [PubMed] [Google Scholar]
- Claudel T, Staels B, Kuipers F (2005) The farnesoid X receptor. A molecular link between bile acid and lipid and glucose metabolism. Arterioscler Thromb Vasc Biol 25: 2020–2030 [DOI] [PubMed] [Google Scholar]
- Cohen DE (2003) Pathogenesis of gallstones. In Hepatology: A Textbook of Liver Disease, Zakim D, Boyer TD (eds) pp 1713–1743. Philadelphia: Saunders [Google Scholar]
- Cui J, Huang L, Zhao A, Lew JL, Yu J, Sahoo S, Meinke PT, Royo I, Pelaez F, Wright SD (2003) Guggulsterone is a farnesoid X receptor antagonist in coactivator association assays but acts to enhance transcription of bile salt export pump. J Biol Chem 278: 10214–10220 [DOI] [PubMed] [Google Scholar]
- De Fabiani E, Mitro N, Gilardi F, Caruso D, Galli G, Crestani M (2003) Coordinated control of cholesterol catabolism to bile acids and of gluconeogenesis via a novel mechanism of transcription regulation linked to the fasted-to-fed cycle. J Biol Chem 278: 39124–39132 [DOI] [PubMed] [Google Scholar]
- Downes M, Verdecia MA, Roecker AJ, Hughes R, Hogenesch JB, Kast-Woelbern HR, Bowman ME, Ferrer JL, Anisfeld AM, Edwards PA, Rosenfeld JM, Alvarez JG, Noel JP, Nicolaou KC, Evans RM (2003) A chemical, genetic, and structural analysis of the nuclear bile acid receptor FXR. Mol Cell 11: 1079–1092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duran-Sandoval D, Cariou B, Percevault F, Hennuyer N, Grefhorst A, van Dijk TH, Gonzalez FJ, Fruchart JC, Kuipers F, Staels B (2005) The farnesoid X receptor modulates hepatic carbohydrate metabolism during the fasting–refeeding transition. J Biol Chem 280: 29971–29979 [DOI] [PubMed] [Google Scholar]
- Duran-Sandoval D, Mautino G, Martin G, Percevault F, Barbier O, Fruchart JC, Kuipers F, Staels B (2004) Glucose regulates the expression of the farnesoid X receptor in liver. Diabetes 53: 890–898 [DOI] [PubMed] [Google Scholar]
- Dussault I, Beard R, Lin M, Hollister K, Chen J, Xiao JH, Chandraratna R, Forman BM (2003) Identification of gene-selective modulators of the bile acid receptor FXR. J Biol Chem 278: 7027–7033 [DOI] [PubMed] [Google Scholar]
- Engelking LR, Dasher CA, Hirschowitz BI (1980) Within-day fluctuations in serum bile-acid concentrations among normal control subjects and patients with hepatic disease. Am J Clin Pathol 73: 196–201 [DOI] [PubMed] [Google Scholar]
- Everson GT (1987) Steady-state kinetics of serum bile acids in healthy human subjects: single and dual isotope techniques using stable isotopes and mass spectrometry. J Lipid Res 28: 238–252 [PubMed] [Google Scholar]
- Foretz M, Pacot C, Dugail I, Lemarchand P, Guichard C, Le Liepvre X, Berthelier-Lubrano C, Spiegelman B, Kim JB, Ferre P, Foufelle F (1999) ADD1/SREBP-1c is required in the activation of hepatic lipogenic gene expression by glucose. Mol Cell Biol 19: 3760–3768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman BM, Goode E, Chen J, Oro AE, Bradley DJ, Perlmann T, Noonan DJ, Burka LT, McMorris T, Lamph WW, Evans RM, Weinberger C (1995) Identification of a nuclear receptor that is activated by farnesol metabolites. Cell 81: 687–693 [DOI] [PubMed] [Google Scholar]
- Francis GA, Fayard E, Picard F, Auwerx J (2003) Nuclear receptors and the control of metabolism. Annu Rev Physiol 65: 261–311 [DOI] [PubMed] [Google Scholar]
- Garg A, Grundy SM (1994) Cholestyramine therapy for dyslipidemia in non-insulin-dependent diabetes mellitus. A short-term, double-blind, crossover trial. Ann Intern Med 121: 416–422 [DOI] [PubMed] [Google Scholar]
- Goodwin B, Jones SA, Price RR, Watson MA, McKee DD, Moore LB, Galardi C, Wilson JG, Lewis MC, Roth ME, Maloney PR, Willson TM, Kliewer SA (2000) A regulatory cascade of the nuclear receptors FXR, SHP-1, and LRH-1 represses bile acid biosynthesis. Mol Cell 6: 517–526 [DOI] [PubMed] [Google Scholar]
- Grundy SM, Ahrens EH Jr, Salen G (1971) Interruption of the enterohepatic circulation of bile acids in man: comparative effects of cholestyramine and ileal exclusion on cholesterol metabolism. J Lab Clin Med 78: 94–121 [PubMed] [Google Scholar]
- Gupta S, Stravitz RT, Dent P, Hylemon PB (2001) Down-regulation of cholesterol 7alpha-hydroxylase (CYP7A1) gene expression by bile acids in primary rat hepatocytes is mediated by the c-Jun N-terminal kinase pathway. J Biol Chem 276: 15816–15822 [DOI] [PubMed] [Google Scholar]
- Hinuma S, Fujii R, Kawamata Y, Komatsu H, Ueshima M, Ito F (2005) Screening method (method for the screening of agonists or antagonists of TGR5). 2003-380574[P2005-21151A (JP)]
- Ho KJ (1976) Circadian distribution of bile acid in the enterohepatic circulatory system in hamsters. J Lipid Res 17: 600–604 [PubMed] [Google Scholar]
- Holt JA, Luo G, Billin AN, Bisi J, McNeill YY, Kozarsky KF, Donahee M, Wang da Y, Mansfield TA, Kliewer SA, Goodwin B, Jones SA (2003) Definition of a novel growth factor-dependent signal cascade for the suppression of bile acid biosynthesis. Genes Dev 17: 1581–1591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton JD, Goldstein JL, Brown MS (2002) SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest 109: 1125–1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houten SM, Auwerx J (2004) The enterohepatic nuclear receptors are major regulators of the enterohepatic circulation of bile salts. Ann Med 36: 482–491 [DOI] [PubMed] [Google Scholar]
- Hung CC, Farooqi IS, Ong K, Luan J, Keogh JM, Pembrey M, Yeo GS, Dunger D, Wareham NJ, O'Rahilly S (2003) Contribution of variants in the small heterodimer partner gene to birthweight, adiposity, and insulin levels. Diabetes 52: 1288–1291 [DOI] [PubMed] [Google Scholar]
- Ikemoto S, Takahashi M, Tsunoda N, Maruyama K, Itakura H, Kawanaka K, Tabata I, Higuchi M, Tange T, Yamamoto TT, Ezaki O (1997) Cholate inhibits high-fat diet-induced hyperglycemia and obesity with acyl-CoA synthetase mRNA decrease. Am J Physiol 273: 37–45 [DOI] [PubMed] [Google Scholar]
- Inagaki T, Choi M, Moschetta A, Peng L, Cummins CL, McDonald JG, Luo G, Jones SA, Goodwin B, Richardson JA, Gerard RD, Repa JJ, Mangelsdorf DJ, Kliewer SA (2005) Fibroblast growth factor 15 functions as an enterohepatic signal to regulate bile acid homeostasis. Cell Metab 2: 217–225 [DOI] [PubMed] [Google Scholar]
- Kanaya E, Shiraki T, Jingami H (2004) The nuclear bile acid receptor FXR is activated by PGC-1alpha in a ligand-dependent manner. Biochem J 382: 913–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kast HR, Nguyen CM, Sinal CJ, Jones SA, Laffitte BA, Reue K, Gonzalez FJ, Willson TM, Edwards PA (2001) Farnesoid X-activated receptor induces apolipoprotein C-II transcription: a molecular mechanism linking plasma triglyceride levels to bile acids. Mol Endocrinol 15: 1720–1728 [DOI] [PubMed] [Google Scholar]
- Katsuma S, Hirasawa A, Tsujimoto G (2005) Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem Biophys Res Commun 329: 386–390 [DOI] [PubMed] [Google Scholar]
- Kawamata Y, Fujii R, Hosoya M, Harada M, Yoshida H, Miwa M, Fukusumi S, Habata Y, Itoh T, Shintani Y, Hinuma S, Fujisawa Y, Fujino M (2003) A G protein-coupled receptor responsive to bile acids. J Biol Chem 278: 9435–9440 [DOI] [PubMed] [Google Scholar]
- Kerr TA, Saeki S, Schneider M, Schaefer K, Berdy S, Redder T, Shan B, Russell DW, Schwarz M (2002) Loss of nuclear receptor SHP impairs but does not eliminate negative feedback regulation of bile acid synthesis. Dev Cell 2: 713–720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo SH, Satoh H, Herzig S, Lee CH, Hedrick S, Kulkarni R, Evans RM, Olefsky J, Montminy M (2004) PGC-1 promotes insulin resistance in liver through PPAR-alpha-dependent induction of TRB-3. Nat Med 10: 530–534 [DOI] [PubMed] [Google Scholar]
- Lee H, Zhang Y, Lee FY, Nelson SF, Gonzalez FJ, Edwards PA (2006) FXR regulates organic solute transporters {alpha} and {alpha} in the adrenal gland, kidney, and intestine. J Lipid Res 47: 201–214 [DOI] [PubMed] [Google Scholar]
- Leiss O, von Bergmann K (1982) Different effects of chenodeoxycholic acid and ursodeoxycholic acid on serum lipoprotein concentrations in patients with radiolucent gallstones. Scand J Gastroenterol 17: 587–592 [DOI] [PubMed] [Google Scholar]
- Liu Y, Binz J, Numerick MJ, Dennis S, Luo G, Desai B, MacKenzie KI, Mansfield TA, Kliewer SA, Goodwin B, Jones SA (2003) Hepatoprotection by the farnesoid X receptor agonist GW4064 in rat models of intra- and extrahepatic cholestasis. J Clin Invest 112: 1678–1687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowell BB, Shulman GI (2005) Mitochondrial dysfunction and type 2 diabetes. Science 307: 384–387 [DOI] [PubMed] [Google Scholar]
- Lu TT, Makishima M, Repa JJ, Schoonjans K, Kerr TA, Auwerx J, Mangelsdorf DJ (2000) Molecular basis for feedback regulation of bile acid synthesis by nuclear receptors. Mol Cell 6: 507–515 [DOI] [PubMed] [Google Scholar]
- Makishima M, Okamoto AY, Repa JJ, Tu H, Learned RM, Luk A, Hull MV, Lustig KD, Mangelsdorf DJ, Shan B (1999) Identification of a nuclear receptor for bile acids. Science 284: 1362–1365 [DOI] [PubMed] [Google Scholar]
- Maloney PR, Parks DJ, Haffner CD, Fivush AM, Chandra G, Plunket KD, Creech KL, Moore LB, Wilson JG, Lewis MC, Jones SA, Willson TM (2000) Identification of a chemical tool for the orphan nuclear receptor FXR. J Med Chem 43: 2971–2974 [DOI] [PubMed] [Google Scholar]
- Maruyama T, Miyamoto Y, Nakamura T, Tamai Y, Okada H, Sugiyama E, Itadani H, Tanaka K (2002) Identification of membrane-type receptor for bile acids (M-BAR). Biochem Biophys Res Commun 298: 714–719 [DOI] [PubMed] [Google Scholar]
- Meyer U, Costantino G, Macchiarulo A, Pellicciari R (2005) Is antagonism of E/Z-guggulsterone at the farnesoid X receptor mediated by a noncanonical binding site? A molecular modeling study. J Med Chem 48: 6948–6955 [DOI] [PubMed] [Google Scholar]
- Miller NE, Nestel PJ (1974) Triglyceride-lowering effect of chenodeoxycholic acid in patients with endogenous hypertriglyceridaemia. Lancet 2: 929–931 [DOI] [PubMed] [Google Scholar]
- Mitchell SM, Weedon MN, Owen KR, Shields B, Wilkins-Wall B, Walker M, McCarthy MI, Frayling TM, Hattersley AT (2003) Genetic variation in the small heterodimer partner gene and young-onset type 2 diabetes, obesity, and birth weight in UK subjects. Diabetes 52: 1276–1279 [DOI] [PubMed] [Google Scholar]
- Moschetta A, Bookout AL, Mangelsdorf DJ (2004) Prevention of cholesterol gallstone disease by FXR agonists in a mouse model. Nat Med 10: 1352–1358 [DOI] [PubMed] [Google Scholar]
- Nestel PJ, Grundy SM (1976) Changes in plasma triglyceride metabolism during withdrawal of bile. Metabolism 25: 1259–1268 [DOI] [PubMed] [Google Scholar]
- Nishigori H, Tomura H, Tonooka N, Kanamori M, Yamada S, Sho K, Inoue I, Kikuchi N, Onigata K, Kojima I, Kohama T, Yamagata K, Yang Q, Matsuzawa Y, Miki T, Seino S, Kim MY, Choi HS, Lee YK, Moore DD, Takeda J (2001) Mutations in the small heterodimer partner gene are associated with mild obesity in Japanese subjects. Proc Natl Acad Sci USA 98: 575–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks DJ, Blanchard SG, Bledsoe RK, Chandra G, Consler TG, Kliewer SA, Stimmel JB, Willson TM, Zavacki AM, Moore DD, Lehmann JM (1999) Bile acids: natural ligands for an orphan nuclear receptor. Science 284: 1365–1368 [DOI] [PubMed] [Google Scholar]
- Pellicciari R, Costantino G, Fiorucci S (2005) Farnesoid X receptor: from structure to potential clinical applications. J Med Chem 48: 5383–5403 [DOI] [PubMed] [Google Scholar]
- Qiao L, Han SI, Fang Y, Park JS, Gupta S, Gilfor D, Amorino G, Valerie K, Sealy L, Engelhardt JF, Grant S, Hylemon PB, Dent P (2003) Bile acid regulation of C/EBPbeta, CREB, and c-Jun function, via the extracellular signal-regulated kinase and c-Jun NH2-terminal kinase pathways, modulates the apoptotic response of hepatocytes. Mol Cell Biol 23: 3052–3066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repa JJ, Liang G, Ou J, Bashmakov Y, Lobaccaro JM, Shimomura I, Shan B, Brown MS, Goldstein JL, Mangelsdorf DJ (2000) Regulation of mouse sterol regulatory element-binding protein-1c gene (SREBP-1c) by oxysterol receptors, LXRalpha and LXRbeta. Genes Dev 14: 2819–2830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell DW (2003) The enzymes, regulation, and genetics of bile acid synthesis. Annu Rev Biochem 72: 137–174 [DOI] [PubMed] [Google Scholar]
- Savkur RS, Thomas JS, Bramlett KS, Gao Y, Michael LF, Burris TP (2005) Ligand-dependent coactivation of the human bile acid receptor FXR by the peroxisome proliferator-activated receptor gamma coactivator-1alpha. J Pharmacol Exp Ther 312: 170–178 [DOI] [PubMed] [Google Scholar]
- Schoenfield LJ, Lachin JM (1981) Chenodiol (chenodeoxycholic acid) for dissolution of gallstones: the National Cooperative Gallstone Study. A controlled trial of efficacy and safety. Ann Intern Med 95: 257–282 [DOI] [PubMed] [Google Scholar]
- Schultz JR, Tu H, Luk A, Repa JJ, Medina JC, Li L, Schwendner S, Wang S, Thoolen M, Mangelsdorf DJ, Lustig KD, Shan B (2000) Role of LXRs in control of lipogenesis. Genes Dev 14: 2831–2838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimomura I, Bashmakov Y, Ikemoto S, Horton JD, Brown MS, Goldstein JL (1999) Insulin selectively increases SREBP-1c mRNA in the livers of rats with streptozotocin-induced diabetes. Proc Natl Acad Sci USA 96: 13656–13661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinal CJ, Tohkin M, Miyata M, Ward JM, Lambert G, Gonzalez FJ (2000) Targeted disruption of the nuclear receptor FXR/BAR impairs bile acid and lipid homeostasis. Cell 102: 731–744 [DOI] [PubMed] [Google Scholar]
- Stayrook KR, Bramlett KS, Savkur RS, Ficorilli J, Cook T, Christe ME, Michael LF, Burris TP (2005) Regulation of carbohydrate metabolism by the farnesoid X receptor. Endocrinology 146: 984–991 [DOI] [PubMed] [Google Scholar]
- Szapary PO, Wolfe ML, Bloedon LT, Cucchiara AJ, DerMarderosian AH, Cirigliano MD, Rader DJ (2003) Guggulipid for the treatment of hypercholesterolemia: a randomized controlled trial. JAMA 290: 765–772 [DOI] [PubMed] [Google Scholar]
- Tomlinson E, Fu L, John L, Hultgren B, Huang X, Renz M, Stephan JP, Tsai SP, Powell-Braxton L, French D, Stewart TA (2002) Transgenic mice expressing human fibroblast growth factor-19 display increased metabolic rate and decreased adiposity. Endocrinology 143: 1741–1747 [DOI] [PubMed] [Google Scholar]
- Urizar NL, Liverman AB, Dodds DT, Silva FV, Ordentlich P, Yan Y, Gonzalez FJ, Heyman RA, Mangelsdorf DJ, Moore DD (2002) A natural product that lowers cholesterol as an antagonist ligand for FXR. Science 296: 1703–1706 [DOI] [PubMed] [Google Scholar]
- Wang H, Chen J, Hollister K, Sowers LC, Forman BM (1999) Endogenous bile acids are ligands for the nuclear receptor FXR/BAR. Mol Cell 3: 543–553 [DOI] [PubMed] [Google Scholar]
- Wang L, Lee YK, Bundman D, Han Y, Thevananther S, Kim CS, Chua SS, Wei P, Heyman RA, Karin M, Moore DD (2002) Redundant pathways for negative feedback regulation of bile acid production. Dev Cell 2: 721–731 [DOI] [PubMed] [Google Scholar]
- Wang L, Liu J, Saha P, Huang J, Chan L, Spiegelman B, Moore DD (2005) The orphan nuclear receptor SHP regulates PGC-1alpha expression and energy production in brown adipocytes. Cell Metab 2: 227–238 [DOI] [PubMed] [Google Scholar]
- Watanabe M, Houten SM, Mataki C, Christoffolete MA, Kim BW, Sato H, Messaddeq N, Harney JW, Ezaki O, Kodama T, Schoonjans K, Bianco AC, Auwerx J (2006) Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature 439: 484–489 [DOI] [PubMed] [Google Scholar]
- Watanabe M, Houten SM, Wang L, Moschetta A, Mangelsdorf DJ, Heyman RA, Moore DD, Auwerx J (2004) Bile acids lower triglyceride levels via a pathway involving FXR, SHP, and SREBP-1c. J Clin Invest 113: 1408–1418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J, Xia C, Meier J, Li S, Hu X, Lala DS (2002) The hypolipidemic natural product guggulsterone acts as an antagonist of the bile acid receptor. Mol Endocrinol 16: 1590–1597 [DOI] [PubMed] [Google Scholar]
- Yamagata K, Daitoku H, Shimamoto Y, Matsuzaki H, Hirota K, Ishida J, Fukamizu A (2004) Bile acids regulate gluconeogenic gene expression via small heterodimer partner-mediated repression of hepatocyte nuclear factor 4 and Foxo1. J Biol Chem 279: 23158–23165 [DOI] [PubMed] [Google Scholar]
- Zhang Y, Castellani LW, Sinal CJ, Gonzalez FJ, Edwards PA (2004) Peroxisome proliferator-activated receptor-gamma coactivator 1alpha (PGC-1alpha) regulates triglyceride metabolism by activation of the nuclear receptor FXR. Genes Dev 18: 157–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Lee FY, Barrera G, Lee H, Vales C, Gonzalez FJ, Willson TM, Edwards PA (2006) Activation of the nuclear receptor FXR improves hyperglycemia and hyperlipidemia in diabetic mice. Proc Natl Acad Sci USA 103: 1006–1011 [DOI] [PMC free article] [PubMed] [Google Scholar]


