Abstract
Reactivation of the polyomavirus BK (BKV) causes polyomavirus nephropathy (PVN) in kidney transplant (KTx) recipients and may lead to loss of the renal allograft. We have identified two HLA-A*0201-restricted nine-amino-acid cytotoxic T lymphocyte (CTL) epitopes of the BKV major capsid protein VP1, VP1p44, and VP1p108. Using tetramer staining assays, we showed that these epitopes were recognized by CTLs in 8 of 10 (VP1p44) and 5 of 10 (VP1p108) HLA-A*0201+ healthy individuals, while both epitopes elicited a CTL response in 10 of 10 KTx recipients with biopsy-proven PVN, although at variable levels. After in vitro stimulation with the respective peptides, CTLs directed against VP1p44 were more abundant than against VP1p108 in most healthy individuals, while the converse was true in KTx recipients with PVN, suggesting a shift in epitope immunodominance in the setting of active BKV infection. A strong CTL response in KTx recipients with PVN appeared to be associated with decreased BK viral load in blood and urine and low anti-BKV antibody titers, while a low or undetectable CTL response correlated with viral persistence and high anti-BKV antibody titers. These results suggest that this cellular immune response is present in most BKV-seropositive healthy individuals and plays an important role in the containment of BKV in KTx recipients with PVN. Interestingly, the BKV CTL epitopes bear striking homology with the recently described CTL epitopes of the other human polyomavirus JC (JCV), JCV VP1p36 and VP1p100. A high degree of epitope cross-recognition was present between BKV and corresponding JCV-specific CTLs, which indicates that the same population of cells is functionally effective against these two closely related viruses.
BK virus (BKV) is the etiologic agent of polyomavirus nephropathy (PVN), an infection of the kidney occurring in up to 8% of kidney transplant (KTx) recipients (38). BKV infects 90% of adults (20) but does not cause any disease in healthy individuals. Viral reactivation in renal transplant recipients occurs in the setting of pharmacologic immunosuppression. This reactivation leads to a lytic infection of renal tubular epithelial cells of the transplanted kidney, which was responsible for renal allograft loss in as high as 45 to 67% of cases in early experiences and is currently responsible for 10 to 30% of renal allograft losses (29, 35, 38). There is no specific antiviral treatment for PVN. Therefore, this disease is a growing medical problem as the population of KTx recipients continues to increase. The only currently available therapeutic option for PVN consists of reduction of chemical immunosuppression, which allows reconstitution of the immune system to clear the virus (4) but which may also be associated with an increased risk of transplant rejection. Hence, prognostic markers of disease evolution and a better understanding of the immune response against BKV are urgently needed for the appropriate management of patients with PVN.
BKV has 75% homology with JC virus (JCV), the causative agent of progressive multifocal leukoencephalopathy (PML). We have previously characterized two HLA-A*0201-restricted epitopes of JCV major capsid protein VP1 recognized by CD8+ cytotoxic T lymphocytes (CTL) and studied the role of these cells in PML patients and control subjects (12, 23). The presence of JCV-specific CTL was associated with a favorable outcome of PML (13), and these cells could be detected in the blood of 73% of healthy individuals (14), suggesting that the cellular immune response against the JCV VP1 protein may be important in the containment of JCV and the prevention of PML (10, 11, 13, 21, 23, 24).
We therefore hypothesized that the BKV VP1 protein may play a similar role. Indeed, in parallel to our studies on the cellular immune response to BKV (5), Krymskaya et al. (26) also recently independently reported that the BKV VP1-specific epitope p108 (VP1p108) cross-reacted with JCV VP1p100 in healthy subjects and in two KTx recipients. In the present study, we have confirmed the cross-reactivity between BKV VP1p108 and JCV VP1p100 and identified an additional A*0201-restricted BKV VP1 CTL epitope p44, which cross-reacts with JCV VP1p36. Both the BKV VP1p44 and VP1p108 epitopes were naturally processed by cells infected with a recombinant vaccinia virus (rVV) expressing the entire BKV VP1 protein. We constructed tetrameric staining complexes with these peptides and the HLA-A*0201 molecule and used these reagents as a tool to detect BKV-specific CTL in healthy individuals and explore their role in KTx recipients with PVN. In addition, we compared the effects of the cellular and humoral immune responses on BKV viral load in the blood and urine samples of these patients. We found that these CTL play a critical role in control of BKV infection in KTx recipients with PVN and that a high degree of epitope cross-recognition exists between BKV and JCV-specific CTL.
MATERIALS AND METHODS
Selection of study subjects.
To determine whether healthy individuals are able to mount a cellular immune response against BKV, we enrolled 10 HLA-A*0201+ healthy individuals, from 23 to 43 years of age (mean ± standard deviation, 34.4 ± 6.63 years), in this Institutional Review Board-approved study and 10 KTx patients, 41 to 68 years of age (57 ± 8.79), with biopsy-proven PVN who were part of an ongoing Institutional Review Board-approved study on PVN at the Division of Transplantation, University of Cincinnati, between December 2000 and October 2005. Informed consent was obtained according to institutional guidelines. Allograft biopsies were performed on KTx recipients at the University of Cincinnati who experienced an unexplained rise in serum creatinine (SCr). PVN was diagnosed by light microscopic viral cytopathic changes suspicious for PVN such as the presence of nuclear viral inclusions, interstitial inflammation with lymphocytes present, and sloughed epithelial cells with slightly enlarged nuclei containing occasional viral inclusions. PVN diagnosis was confirmed by in situ hybridization for BKV on paraffin-embedded sections of renal allograft biopsies with light microscopic viral cytopathic changes suspicious for PVN (7, 8).
All KTx recipients with PVN were managed with a reduction of chemical immunosuppression after PVN diagnosis. At the time of PVN diagnosis, patients underwent a 30 to 40% reduction in their calcineurin inhibitor dose (all patients were on tacrolimus) and a 50% reduction in their azathioprine, mycophenolate mofetil, or sirolimus dose. If a decrease of 2 to 3 logs in BKV urine and serum loads or an increase in anti-BKV antibody titers was not observed within 4 to 6 weeks, a further reduction of immune suppression was undertaken, consisting of discontinuation of the azathioprine or mycophenolate mofetil dose and a 25% reduction in the prednisone dose (37). Blood and urine samples were collected prospectively for monitoring of BK viral load, cellular and humoral immune responses, and renal function.
MHC-I typing.
The major histocompatibility complex class I (MHC-I) alleles expressed by the study subjects and organ donors were determined using standard serologic tissue typing procedures. In addition, molecular analyses to determine HLA-A*02 subtypes were performed on all study subjects.
Hemagglutination inhibition assay.
Human serum antibody titers against BKV and JCV were determined by hemagglutination inhibition assays (HAI) as described elsewhere (31).
Peptide selection.
Two computer algorithms (http://bimas.cit.nih.gov/molbio/hla_bind/ and http://www.syfpeithi.de) were used to predict nine-amino-acid peptides from BKV VP1 protein for their likely ability to bind to the HLA-A*0201 molecule (32, 33). A total of six nonamer peptides with a high score in both predictive analyses methods were selected and synthesized (Table 1). Peptides were dissolved in dimethyl sulfoxide at a concentration of 10 mg/ml and stored at −80°C until use.
TABLE 1.
Nonamer peptides from BKV VP1 protein predicted to bind to the HLA-A*0201 allele
| Peptide | Sequence | BIMAS scorea | Syfpeithi scoreb |
|---|---|---|---|
| VP1p108 | LLMWEAVTV | 437 | 27 |
| VP1p27 | LLIKGGVEV | 118 | 30 |
| VP1p84 | KMLPCYSTA | 70 | 19 |
| VP1p128 | NLHAGSQKV | 69 | 24 |
| VP1p44 | AITEVECFL | 66 | 21 |
| VP1p259 | SLYVSAADI | 33 | 23 |
BIMAS: BioInformatics and molecular analysis section, National Institutes of Health, Bethesda, Md.
Syfpeithi: Department of Immunology, Heidelberg BMI, Germany.
Construction of rVV BKV VP1.
Construction of rVV BKV VP1 was performed as previously described (24). Briefly, the BKV VP1 gene was subcloned from BKV reference strain Dunlop into the plasmid pAbt 4587 (a generous gift from Therion Biologics, Cambridge, MA), and the nucleotide sequences of the recombinant clones were verified by automated sequencing. Molecular clones containing the entire BKV VP1 gene were inserted into vaccinia virus (NYCBH strain A) as previously described (24). The presence in the rVV BKV VP1 of a full-length DNA insert was demonstrated by DNA PCR amplification from infected BSC40 cells and by expression of the BKV VP1 protein by Western blotting using polyclonal rabbit antisera against simian virus 40 capsid, which cross-reacts against BKV (Lee Biomolecular Research, San Diego, CA).
Functional lysis assay.
Functional lysis assays using BKV CTL epitope peptides were performed as previously described (14, 23). Briefly, peripheral blood mononuclear cells (PBMC) were isolated from fresh blood (nine samples) or from buffy coat (one sample) using a Ficoll-diatrizoate gradient. These PBMC were cultured in aliquots of 7 × 106 cells in RPMI 1640 medium in 12-well plates with individual BKV VP1 peptides, at a concentration of 2 μg/ml for each peptide, and after 3 days, 25 U of recombinant human interleukin-2 per ml was added. After 10 to 14 days, the presence of CTL specific for these peptides was determined in a 51Cr release assay. Autologous Epstein-Barr virus-transformed or heterologous A*0201-matched only B-lymphoblastoid cell lines (B-LCL) were used as target cells. Aliquots of 106 B-LCLs were incubated overnight with peptide at a concentration of 2 μg/ml. Peptide p11B (ALSEGCTPYDIN) from simian immunodeficiency virus was used as a negative control. After a 16-h incubation period, target cells were labeled with 100 μCi of 51Cr in a 100-μl volume for 90 min. These cells were washed, and 104 cells were added to the peptide-stimulated PBMC in a 96-well U-bottom plate in a final volume of 200 μl/well. The assays were performed in duplicate. Cross-killing experiments were performed similarly using the JCV VP1p36 and VP1p100 peptides. Assays were considered positive when the specific lysis was ≥10% at an effector-to-target ratio (E:T) of 20:1.
Functional lysis assays using rVV BKV VP1 were performed as previously described (24). Briefly, PBMC were stimulated with the BKV CTL epitope peptides as described above, and autologous B-LCLs infected with this rVV were made to serve as target cells. B-LCLs similarly transformed with wild-type vaccinia virus (vABT33) were used as control target cells. Aliquots of 106 B-LCLs were incubated overnight with the respective vaccinia viruses at a multiplicity of infection of 10 PFU/cell. The rest of the procedure is the same as described above.
Construction of the tetrameric HLA-A*0201/VP1p44 and HLA-A*0201/VP1p108 complexes.
Construction of BKV tetramers was performed as previously described (12, 23). The HLA-A*0201 protein was expressed in vitro from the plasmid HLA-A*0201/glyser/BirA substrate peptide (1) and refolded in vitro with human β2-microglobulin in the presence of the BKV VP1p44 or VP1p108 peptides. The HLA-A*0201/BKV VP1p44 and HLA-A*0201/VP1p108 monomers were purified by gel filtration and biotinylated with the BirA enzyme (Avidity, Denver, CO). The biotinylated monomers were then mixed with phycoerythrin (PE)- or allophycocyanin (APC)-labeled streptavidin (Prozyme, San Leandro, CA) at a molar ratio of 4:1 to generate the HLA-A*0201/BKV VP1p44 and HLA-A*0201/VP1p108 tetramers.
Staining and phenotypic analysis of BKV VP1p44- and VP1p108-specific CD8+ T cells and JCV VP1p36- and VP1p100-specific CD8+T cells.
Flow cytometry analysis of tetramer-stained samples was performed as previously described (23). For cross-staining experiments, BKV and JCV tetramers were labeled with different fluorochromes. Results were considered positive when tetramer-stained CD8αβ+ T cells formed a distinct population and their number was ≥0.1%.
Qualitative PCR amplification of BKV and JCV DNA in healthy individuals.
The presence of BKV or JCV DNA in urine samples was determined by PCR. Three microliters of DNA solution extracted from a 5-ml urine sample was added into a 50-μl reaction mixture consisting of Platinum PCR supermix (Invitrogen) and 10 pmol of each oligonucleotide primer. Primers JP23 and JP25 were used to specifically amplify a JCV DNA fragment. The sequences of these two primer are as follows: JP25, 5′-CTG GTG AAT TTA TAG AAA GAA GTA TTG CA-3′ (nucleotides [nt] 1343 to 1372); JP23, 5′-GGG CCA TCT TCA TAT GCT TCA A-3′ (nt 1475 to 1454). This primer pair is specific to the JCV VP2 protein gene and yields a 133-bp PCR product. Similarly, BK2217F and BK2320R were used to specifically amplify BKV DNA from the urine DNA samples and yield a 104-bp PCR product. The sequence of primer BKV2217F is 5′-TGC TAG GTA TTT TGG GAC TTT CAC A-3′ (nt 2217 to 2241), and the sequence for BKV2320R is 5′-GCC CCA CAC CCT GTT CAT C-3′ (nt 2320 to 2302). The amplification was carried out in a GeneAmp PCR System 9700 (PE Applied Biosystems) with a first denaturing step of 2 min at 94°C, followed by 40 cycles consisting of 30 s of denaturation at 94°C, 1 min of annealing at 60°C, 1 min of elongation at 72°C, and a final elongation period of 7 min at 72°C. The PCR products were analyzed by electrophoresis on a 1% agarose gel.
QPCR detection for BKV and JCV DNA in KTx recipients with PVN.
Real-time quantitative PCR (QPCR) was used to measure BK (15) and JC (34) viral loads in the serum and urine of KTx recipients with PVN, as previously described (15, 28). DNA extracted from serum or urine using a QiaAmp DNA Mini Kit (QIAGEN) was analyzed in triplicate using primers which represent nt 2511 to 2531 and nt 2586 to 2605 of the VP1 sequence (Dunlop strain) of BKV. Each 50-μl reaction mixture contained 200 nM and 400 nM of forward (5′-AGTGGATGGGCAGCCTATGTA-3′) and reverse primers (5′-TCATATCTGGGTCCCCTGGA-3′), respectively, and 200 nM of BKV-specific probe (nt 2546 to 2578) (5′-FAM-AGGTAGAAGAGGTTAGGGTGTTTCATGGCACA-BHQ1-3′) in 1× TaqMan Universal Master Mix (Perkin Elmer). Cycling conditions were 45 cycles of annealing at 60°C for 60 s and denaturation at 95°C for 15 s. Plasmid DNA containing the BKV genome served to generate a standard curve against which samples were analyzed using iCycler software (Bio-Rad). All QPCR results were calculated as copies per ml. The detection cutoff of the assay was 5,000 copies/ml in urine and 100 copies/ml in the serum.
RESULTS
Characterization of two HLA-A*0201-restricted CTL epitopes of BKV VP1 protein.
In this study, we explored the possibility that a CTL response might exist that recognizes a dominant BKV epitope presented to CD8+ T lymphocytes by a common MHC-I allele. Using a similar approach, we have previously characterized two epitopes of the JCV VP1 protein, JCV VP1p36 and JCV VP1p100, using a computerized predictive algorithm and an epitope mapping study (10, 12, 13, 23, 24). VP1 is the major capsid protein of the polyomaviruses, and BKV VP1 has a 75% homology at the amino acid level with the JCV VP1 protein. We therefore hypothesized that the BKV and JCV CTL epitopes could be identical. Using two computerized algorithms (Biomas and SYFPEITHI) (32, 33), we selected six nonamer peptides derived from BKV VP1 protein that are predicted to bind to the HLA-A*0201 molecule: BKV VP1p108, BKV VP1p27, BKV VP1p84, BKV VP1p128, BKV VP1p44, and BKV VP1p259 (Table 1). The six peptide sequences are identical in the BKV strains WW, AS, DIK, Dunlop, JL, MM, MT, and SB and in 15 novel BKV full-length clones sequenced by our laboratory, except for one amino acid change in BKV VP1p44 at position 4 of BKV MJu-5 (6).
PBMC from HLA-A*0201+ healthy individuals were stimulated with these peptides and assessed as effector cells in a 51Cr release assay using as target cells autologous B-LCLs pulsed with each of these peptides. The BKV VP1p44 AITEVECFL was recognized by CTL from three of the six HLA-A2+ healthy individuals and BKV VP1p108 LLMWEAVTV was recognized by CTL from two of six of the study subjects. No other peptide was recognized by CTL from any of the six subjects. These results suggested that BKV VP1p44 and VP1p108 are two epitopes recognized by CTL of healthy individuals.
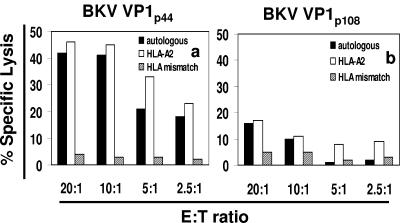
To confirm that CTL recognition of these two epitopes was HLA-A*0201-restricted, target cells that were fully MHC-I mismatched and target cells that shared only the A*0201 allele were selected from a panel of previously characterized B-LCLs. The selected allogeneic B-LCLs pulsed with BKV VP1p44 or BKV VP1p108 were assessed as targets in a standard 51Cr release assay. The A*0201+ cells, but not the fully allogeneic target cells, were lysed by the A*0201+ effector cells. These experiments, therefore, confirmed that the VP1p44- and VP1p108-specific CTL were HLA-A*0201-restricted in their target cell recognition (Fig. 1).
FIG. 1.
The BKV VP1p44 and VP1p108 peptides are recognized by CTL from an HLA-A*0201+ healthy individual. Autologous and HLA-A*0201-matched only target cells sensitized with BKV VP1 peptides p44 AITEVECFL (a) or p108 LLMWEAVTV (b) were lysed by peptide-stimulated PBMC from a healthy study subject. No significant lysis was observed using fully MHC-I-mismatched target cells. The percentage of specific lysis indicates the difference in specific 51Cr release between target cells pulsed with the BKV VP1 peptides and those pulsed with the control peptide. Effector target (E:T) ratios are shown.
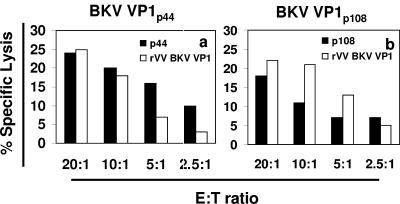
To examine whether VP1p44- and VP1p108-specific CTL were able to recognize naturally processed epitopes, PBMC of a healthy BKV-seropositive individual were stimulated separately with VP1p44 and VP1p108 in the presence of recombinant interleukin-2 as described above. After 2 weeks, these peptide-stimulated PBMC were used as effector cells in a 51Cr release assay, using as target cells autologous B-LCLs that were either infected with the rVV BKV VP1 expressing the entire VP1 protein or pulsed with the respective epitope peptide. Both rVV BKV VP1-infected and peptide-pulsed target cells were lysed by effector cells (Fig. 2). These results demonstrate that VP1p44- and VP1p108-specific CTL from a healthy individual were able to recognize the corresponding epitope after it had been processed from the full-length VP1 protein by virus-infected cells.
FIG. 2.
The BKV VP1p44 and VP1p108 epitopes are naturally processed and presented from the intact VP1 protein. PBMC from a healthy individual were stimulated in vitro with the peptides VP1p44 (a) and VP1p108 (b) and were assessed for their ability to destroy autologous B-LCLs that were either pulsed with the respective peptide or infected with a recombinant vaccinia virus expressing the entire VP1 protein (rVV BKV VP1). Lysis of target cells (T) by effector cells (E) was observed using both conditions. The irrelevant peptide p11b (23) was used as control for VP1p44 and VP1p108, while wild-type vaccinia virus (24) was used as control for rVV BKV VP1.
Detection of CTL recognizing BKV VP1p44 and BKV VP1p108 in A*0201+ healthy individuals using tetrameric complexes and functional lysis assays.
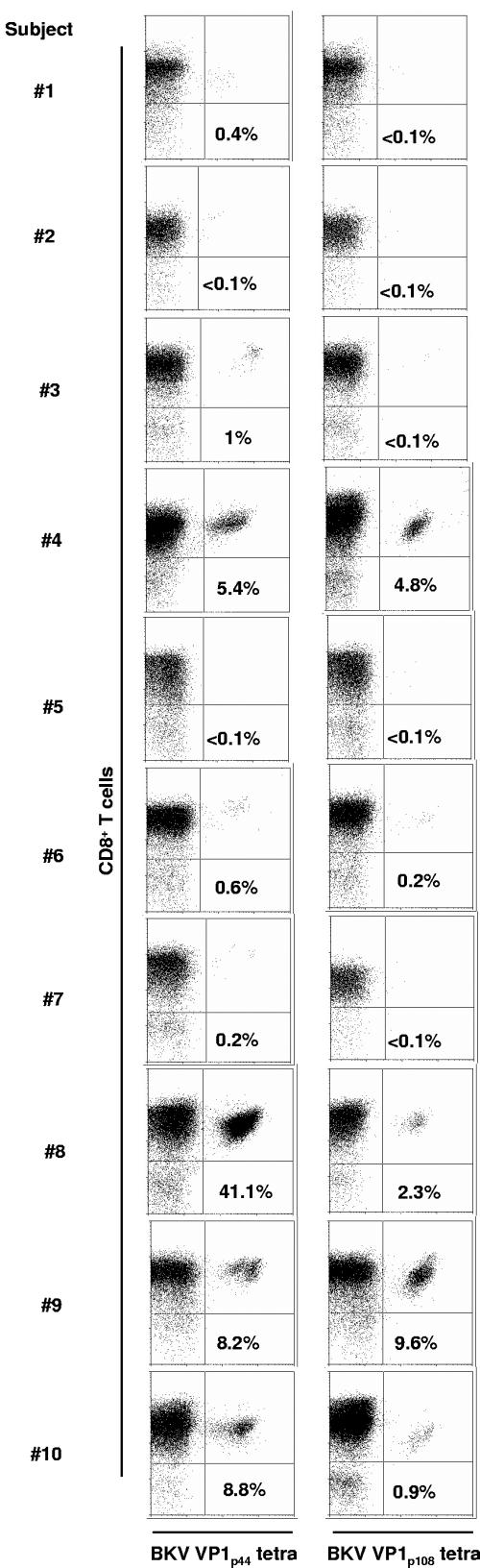
Since our goal was to create an easily performed and quantitative assay for BKV-specific CTL, we used the knowledge of the VP1 epitope peptides presented to CTL by HLA-A*0201 to create tetrameric HLA-A*0201/BKV VP1p44 and HLA-A*0201/BKV VP1p108 complexes. Fresh blood and cultured lymphocyte specimens from 10 HLA-A*0201+ healthy individuals were stained with the tetrameric HLA-A*0201/VP1p44 and HLA-A*0201/VP1p108 complexes and analyzed by flow cytometry, gating on the CD3+ CD8αβ+ T cells. No tetramer staining of CD8αβ+ T cells from any of the fresh blood samples was observed (data not shown). However, the lymphocytes of 8 of 10 A*0201+ healthy individuals had between 0.2% and 41.1% BKV VP1p44-specific CD8+ T cells, whereas 5 of 10 had between 0.2% and 9.6% BKV VP1p108-specific CD8+ T cells, after in vitro stimulation with the respective peptides (Fig. 3).
FIG. 3.
Staining of PBMC from 10 HLA-A*0201+ healthy individuals with tetrameric HLA-A*0201/BKV VP1p44 and HLA-A*0201/BKV VP1p108 complexes after in vitro stimulation with the respective peptides for 10 to 14 days. The percentages of CD8αβ+ T cells that bind the tetramers (right upper quadrant of each panel) are indicated in each panel. BKV VP1p44 tetramer-positive cells were detected in 8 of 10 healthy individuals (left column), while BKV VP1p108-positive cells were present in 5 of 10 individuals of the same group (right column). Results were considered positive if the percentage of tetramer-staining cells was equal or greater than 0.1% of CD8αβ+ T cells and formed a distinct population of cells on the dot plot.
To confirm that tetramer-staining cells were functionally active effectors, we performed a 51Cr assay using the same peptide-stimulated PBMC in seven healthy individuals for which sufficient numbers of cells were available (Fig. 3, subjects 2 to 6, 8, and 9). Positive results, determined by a percent specific lysis greater than or equal to 10 at an E:T ratio of 20:1, were found whenever the percent tetramer-staining cells was >4%, consistent with the fact that the tetramer staining assay is much more sensitive than the 51Cr assay (23) (data not shown).
BKV antibody titers and detection of BKV in urine of healthy individuals.
To determine whether an association existed between the presence of BKV-specific CTL and polyomavirus antibody titers or viruria, we measured serum antibody titers for BKV, as well as the presence of BKV DNA by qualitative PCR in the urine of the healthy individuals (Table 2). BKV antibodies were detected in nine of nine subjects tested. (The untested sample came from a buffy coat from an anonymous A*0201+ donor, and therefore serum or plasma was not available.) Of eight urine samples tested, two had detectable BKV DNA. No significant relationship was found between tetramer staining results, urine BKV detection, or serum antibody titers.
TABLE 2.
Serological, qualitative PCR, and immunological results in healthy individualsa
| Study subject | BKV HAI titer | Urine BKV DNA PCR | JCV HAI titer | Urine JCV DNA PCR | Cultured cells tetramer staining
|
|
|---|---|---|---|---|---|---|
| VP1p44 | VP1p108 | |||||
| 1 | 1/512 | − | 1/32 | − | + | − |
| 2 | 1/1024 | + | 1/32 | − | − | − |
| 3 | 1/512 | − | 1/32 | − | + | − |
| 4 | 1/256 | − | 1/32 | − | + | + |
| 5 | 1/512 | − | 1/32 | − | − | − |
| 6 | 1/256 | − | 1/32 | + | + | + |
| 7 | 1/2,048 | NA | 1/16 | NA | + | − |
| 8 | 1/512 | − | 1/64 | + | + | + |
| 9 | 1/256 | + | 1/64 | + | + | + |
| 10 | NA | NA | NA | NA | + | + |
NA, not available.
Correlation of humoral and cellular immune responses against BKV with blood and urine BK viral load in A*0201+ kidney transplant recipients with PVN.
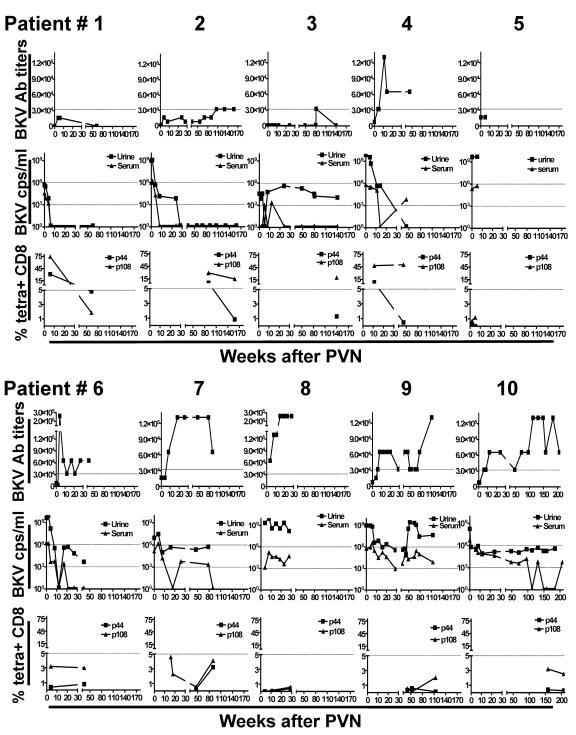
We then tested the 10 HLA-A*0201 KTx recipients with biopsy-proven PVN. CTL specific for BKV VP1p44 and VP1p108 were detectable in the blood of all patients tested (100%), although at variable levels and only transiently in some cases. To determine the temporal relationship between the emergence of the cellular and humoral immune responses against BKV and their effect on BK viremia and viruria in KTx recipients with PVN, we correlated the results of the tetramer staining assay, BKV antibody titers, and viral load in urine and in serum over time after the development of PVN (Fig. 4). Based on the experience at our transplantation center and the sensitivity of our QPCR assay, we used cutoffs of 1,000 BKV copies/ml or greater in the serum and 1,000,000 BKV copies/ml in the urine or greater as being consistent with active disease. These cutoffs are lower than recently reported BK viral load values in PVN (17).
FIG. 4.
Temporal relationship between BKV-specific cellular immune response, viral load, and BKV-specific antibody titers in 10 HLA-A*0201+ kidney transplant recipients in the weeks following PVN diagnosis. (Top rows) Anti-BKV antibody (Ab) titers determined by HAI. Values above 32,768 represented by the horizontal dotted line have only been reported in KTx recipients with PVN (J. Gordon et al., unpublished observations). (Middle rows) BKV viral load in urine and serum. Values above 106 copies/ml in urine, represented by the upper horizontal dotted line, and 103 copies/ml in serum, represented by the lower horizontal dotted line, have only been reported in KTx recipients with PVN. Because of the sensitivity of our assay, these cutoffs are lower than recently reported values for BK viral load in PVN (17) (see text for details). (Bottom rows) Percentage of CD8+ T cells specific for the VP1p44 or VP1p108 epitopes by tetramer staining assay. The horizontal dotted line at 5% separates high from low responders.
Tetramer staining assays were performed at one time point in one patient (no. 3), twice in six patients (no. 1, 2, 4 to 6, and 10), three times in two patients (no. 8 and 9) and four times in one patient (no. 7). The first tetramer staining assay was performed within the first 3 months following PVN diagnosis in five patients (no. 1, 4 to 6, and 8), between 3 months and 1 year in two patients (no. 7 and 9), and between 1 to 4 years in three patients (no. 2, 3, and 10).
Patients 1 to 4 had a high CTL response (above 5% tetramer-staining CD8+ T cells) for both CTL epitopes (Fig. 4, bottom row, patients 1, 2, and 4) or the p108 epitope only (Fig. 4, bottom row, patient 3) at their first testing. These patients had a decreased BK viral load in blood and urine (middle row), except for patient 3, who kept a stable BK viral load in the urine over time of around 106 copies/ml. Interestingly, this patient had a strong CTL response for only one of the two epitopes. The BKV-specific antibody titers of these patients are shown in Fig. 4 (top row). Despite initially high levels of viremia and viruria, patients 1 to 3 never mounted a strong antibody response to BKV, with titers remaining below 32,768, while patient 4 developed an initial spike followed by a decrease in antibody titers. These results suggest that a strong CTL response tends to be associated with decreasing levels of BK viremia and viruria, and in this context, the humoral immune response against BKV may remain low.
Conversely, patients 5 to 10 had a low or undetectable CTL response for both epitopes (less than 5% tetramer-staining CD8+ T cells) (Fig. 4, bottom row). Of these six patients, all except patient 6 had persistently elevated viruria, above the diagnostic cutoff of 106 copies/ml, and four of them had a viremia oscillating usually above the diagnostic cutoff of 103 copies/ml (Fig. 4, middle row, patients 5, and 8 to 10). Patients 6 to 10 had elevated antibody titers (above 32,768) (Fig. 4, top row), which persisted for up to 4 years after PVN diagnosis in one patient (patient 10). These results suggest that a low or absent CTL response against BKV tends to be associated with maintenance of high BK viral loads in urine and, in some patients, in the blood, and in this context, the humoral immune response against BKV may be elevated.
All patients underwent a similar reduction in immunosuppression, and general renal function was assessed by measuring serum creatinine (SCr) levels. SCr levels returned to pre-PVN baseline values in three of four patients with a high CTL response (patients 1 to 3). In contrast, SCr levels remained high in four of six patients with lower CTL responses (patients 6 to 9), which is attributed to ongoing active disease. Note that follow-up of patient 5 was limited to 6 weeks post-PVN, and therefore a reduction in SCr would not be expected during this time period.
HLA-A*0201-restricted CTL in A*0201+ KTx recipients developing PVN in a kidney allograft from A2+ or A2− donors.
Whether CTL can efficiently recognize and destroy virus-infected cells in HLA class I-mismatched allografts is unclear. The composition of class I A and B alleles of donors and recipients is shown in Table 3. Of five KTx recipients with PVN who had a renal allograft from an A2-positive donor, three had a strong CTL response and satisfactory control of BKV (patients 2, 3, and 4) while two had a low CTL response (patients 6 and 7). Of the five patients who received an allograft from an A2-negative donor, four (patients 5 and 8 to 10) had low CTL responses and incomplete control of BKV in blood and urine while one (patient 1) exhibited a strong CTL response against both of these A*0201-restricted epitopes associated with satisfactory viral clearance. These results suggest that a CTL response directed against A*0201-restricted epitopes may still occur in A*0201+ KTx recipients with PVN, despite the absence of the A2 allele in the infected graft.
TABLE 3.
HLA class I alleles in recipients and donors of renal allograftsa
| Patient no. | HLA recipient (allele no.)
|
HLA donor (allele no.)
|
||||||
|---|---|---|---|---|---|---|---|---|
| A | B | A | B | |||||
| 1 | 2 | 3 | 7 | 44 | 1 | 23 | 8 | 44 |
| 2 | 2 | 2 | 52 | 44 | 2 | 31 | 52 | 60 |
| 3 | 2 | 3 | 7 | 14 | 2 | 11 | 57 | 62 |
| 4 | 2 | 18 | 35 | 53 | 2 | 11 | 35 | 44 |
| 5 | 2 | 26 | 38 | 44 | 1 | 32 | 44 | 44 |
| 6 | 1 | 2 | 8 | 44 | 1 | 2 | 8 | 44 |
| 7 | 2 | 23 | 35 | 44 | 2 | 3 | 7 | 44 |
| 8 | 2 | 3 | 7 | 15 | 1 | 11 | 44 | 53 |
| 9 | 2 | 11 | 13 | 62 | 30 | 31 | 42 | 60 |
| 10 | 2 | 11 | 44 | 62 | 1 | 3 | 8 | 39 |
Bold underlined alleles are present in both donor and recipient.
CTL epitope immunodominance in healthy individuals and KTx recipients with PVN.
Interestingly, the healthy individuals and KTx recipients with PVN had different tetramer staining patterns. Of five healthy individuals with double-positive staining, four (Fig. 3, subjects 4, 6, 8, and 10) had a higher percentage of VP1p44- than VP1p108-specific CD8+ T cells, and in two of them (subjects 8 and 10), the difference was equal or greater than one log. Only in one subject, (subject 9) were VP1p108-specific CD8+ T cells slightly more abundant than VP1p44-specific CD8+ T cells. These results suggest than the VP1p44 epitope is more frequently recognized in healthy individuals than the VP1p108 epitope. Conversely, KTx recipients with PVN all had a higher percentage of VP1p108- than VP1p44-specific CD8+ T cells (Fig. 4). Only one patient (Fig. 4, patient 1, bottom row), who initially had the highest CTL response for both VP1p108 and VP1p144 epitopes (74.3% and 31%, respectively), inverted this ratio upon further testing and then had a higher percentage of VP1p44- than VP1p108-specific CD8+ T cells at the time when BKV replication was under control in blood and urine and antibody titers were low. The difference between the p44/p108 tetramer staining ratio of healthy individuals and KTx recipients with PVN is shown in Fig. 5.
FIG. 5.
Shift in BKV CTL epitope immunodominance in PVN patients compared to healthy individuals. The log of p44 tetramer staining result divided by the p108 tetramer staining result at the same time point was calculated for each individual in all experiments where both of these results were different than zero (see the legend of Fig. 4). A positive number indicates that the percentage of p44 tetramer-staining cells is higher than the percentage of p108 tetramer-staining cells at a given time point, which is the case of most healthy individuals. Conversely, a negative value indicates that the percentage of p108 tetramer-staining cells is higher than the percentage of p44-staining cells, which is the case of most KTx recipients with PVN. TSR, tetramer staining results; HI, healthy individuals.
Functional cross-reactivity between BKV and JCV VP1 CTL epitopes.
BKV shares 75% amino acid sequence with JCV. We have previously identified two A*0201-restricted CTL epitopes of JCV, JCV VP1p36 (12) and JCV VP1p100 (23), in immunosuppressed patients with PML (13) and healthy control subjects (14). BKV VP1p44 AITEVECFL has only one amino acid different (underlined) from the sequence of JCV VP1p36 SITEVECFL at position 1, whereas BKV VP1p108 LLMWEAVTV has two amino acid differences with JCV VP1p100 ILMWEAVTL, at positions 1 and 9. These three amino acid changes are conservative. To determine whether there is cross-reactivity between BKV VP1p44 and JCV VP1p36, as well as between BKV VP1p108 and JCV VP1p100, we stimulated PBMC from the same subject in parallel experiments with an identical concentration of either the BKV or JCV VP1 corresponding peptide. After 10 to 14 days of culture, the cells were stained with either corresponding BKV or JCV tetramers and double-stained with both tetramers (Fig. 6). The results showed that the same population of CD8+ CTL reacted with either BKV VP1p44 or JCV VP1p36 (Fig. 6 A, frames a to c and e to g), and this was also the case for BKV VP1p108 and JCV VP1p100 CTL epitopes (Fig. 6.B, frames a to c and e to g).
FIG. 6.
Cross-staining and cross-killing between BKV VP1 peptide-stimulated CD8+ T lymphocytes and JCV VP1 peptide-stimulated CD8+ T lymphocytes in PBMC of two HLA-A*0201+ healthy individuals. (A) Cross-reactivity between BKV VP1p44 and JCV VP1p36 peptides in study subject 8. In cross-staining, both BKV VP1p44 and JCV VP1p36 tetramers bind to a population of CD8αβ+ T lymphocytes stimulated with either VP1p44 or JCV VP1p36 peptides. The percentages of all CD8 αβ+ T cells that bind to these tetramers are indicated in each frame. An equal percentage of BKV VP1p44-stimulated CD8 αβ+ T lymphocytes was stained with the BKV VP1p44 tetramer (frame a) or the JCV VP1p36 tetramer (frame b). A double staining experiment showed that the majority of these cells stained with both tetramers (frame c). The mirror experiment is shown in frames e to g. An equal percentage of JCV VP1p36-stimulated CD8 αβ+ T lymphocytes was stained with the BKV VP1p44 tetramer (frame e) or the JCV VP1p36 tetramer (frame f). A double staining experiment showed that the majority of these cells stained with both tetramers (frame g). In a cross-killing experiment, both BKV VP1p44- and JCV VP1p36-stimulated PBMC lyse autologous target cells pulsed with either peptide. BKV VP1p44-stimulated PBMC induced lysis of BKV VP1p44-pulsed target cells more efficiently than JCV VP1p36-pulsed target cells (frame d). Conversely, JCV VP1p36-stimulated cells induced a greater lysis of JCV VP1p36-pulsed target cells than BKV VP1p44-pulsed target cells (frame h). (B) Cross-reactivity between BKV VP1p108 and JCV VP1p100 peptides in study subject 4. In cross-staining experiments, both BKV VP1p108 and JCV VP1p100 tetramers bind to a population of CD8αβ+ T lymphocytes stimulated with either BKV VP1p108 or JCV VP1p100 peptides. The percentages of all CD8 αβ+ T cells that bind to these tetramers are indicated in each frame. An equal percentage of BKV VP1p108-stimulated CD8 αβ+ T lymphocytes was stained with the BKV VP1p108 tetramer (frame a) or the JCV VP1p100 tetramer (frame b). A double staining experiment showed that the majority of these cells stained with both tetramers (frame c). A mirror experiment is shown in frames e to g. An equal percentage of JCV VP1p100-stimulated CD8 αβ+ T lymphocytes was stained with the BKV VP1p108 tetramer (frame e) or the JCV VP1p100 tetramer (frame f). A double staining experiment showed that the majority of these cells stained with both tetramers (frame g). In a cross-killing experiment, both BKV VP1p108- and JCV VP1p100-stimulated PBMC lyse autologous target cells pulsed with either peptide. As expected, BKV VP1p108-stimulated PBMC induced lysis of BKV VP1p108-pulsed target cells more efficiently than JCV VP1p100-pulsed target cells (frame d). Interestingly, JCV VP1p100-stimulated cells induced a greater lysis of BKV VP1p108-pulsed target cells than JCV VP1p100-pulsed target cells (frame h). Flow cytometry experiments were performed with PE-tagged tetramers (A, frames a, b, and f; B, frames a, b, e, and f), or APC-tagged tetramer (A, frame e). Double staining experiments were performed with a combination of PE- and APC-tagged tetramers (A, frames c and g; B, frames c and g).
Since these tetramer staining experiments showed a high level of cross-reactivity between corresponding BKV and JCV CTL epitopes, we sought to determine whether cells stimulated with the epitope peptide of one virus could efficiently lyse target cells presenting the corresponding epitope from the other virus. PBMC stimulated in vitro for 10 to 14 days with BKV or JCV VP1 peptides were used as effector cells in a 51Cr release assay, using autologous B-LCLs pulsed with BKV or corresponding JCV peptides as target cells (Fig. 6). Effectors stimulated with either BKV VP1p44 or JCV VP1p36 demonstrated a clear cytolytic activity with targets pulsed with either epitope peptide (Fig. 6A, frames d and h). We made the same observation for BKV VP1p108 and JCV VP1p100 CTL epitopes (Fig. 6B, frames d and h). These results indicate that cross-killing exists between corresponding BKV and JCV CTL epitopes.
Detection of JCV antibody titers and JCV DNA in healthy individuals and KTx recipients with PVN.
To determine whether an active JCV infection was present in our study subjects, we measured the antibody titers for JCV, as well as the presence of JCV DNA in the urine of the healthy individuals (Table 2). Low titers of JCV antibodies were detected in nine of nine subjects tested. Of eight urine samples tested, three were positive for JCV DNA. These results demonstrated that the BKV-seropositive healthy individuals enrolled in this study were JCV seropositive as well, and JC viruria could be detected in 38%, consistent with the results of previous studies (22). All KTx recipients with PVN were JCV seropositive, and eight had titers below 512, while two had titers going up to a maximum of 1,024 and 2,048, respectively. It should be noted that the HAI and PCR assays are highly specific for BKV versus JCV with no cross-reactivity between the two viruses (15, 40). Of six KTx recipients for whom the JCV viral load was available, four had undetectable JCV in serum (patients 2, 6, 7, and 10) while two had transient JCV viremia (patients 1 and 9); four had undetectable JCV in urine (patients 6, 7, 9, and 10); one had transient viruria (patient 2), and one had low-level persistent viruria at <100 cps/ml (patient 1). These results suggest that the KTx recipients with PVN did not have active ongoing JCV infection.
DISCUSSION
Like JCV, BKV infects most healthy adults and remains quiescent in the kidneys, without causing any disease. Since anti-BKV antibodies do not prevent viral reactivation in immunosuppressed patients, we hypothesized that the cellular immune response was likely to have a crucial role in containing the replication of this virus. Indeed, the two HLA-A*0201-restricted CTL epitopes, BKV VP1p44 and VP1p108 were naturally processed and presented by cells expressing the full-length BKV VP1 protein. They are the exact counterpart of the previously defined JCV VP1p36 and VP1p100 CTL epitopes (12, 23), with only one and two amino acid differences, respectively. In addition, cross-staining experiments with BKV and JCV tetramers showed that the population of cells recognizing both corresponding BKV and JCV epitopes was identical. Furthermore, cross-killing experiments demonstrated that CTL specific for one virus were able to destroy target cells presenting the corresponding epitope of the other virus.
Since BKV and JCV have 75% amino acid homology, it is therefore advantageous for the body to mount a cellular immune defense against epitopes common to both viruses. Although we have recently detected a higher intrastrain genetic diversity in BKV sequences (6) than previously reported for JCV (16), the two BKV CTL epitopes identified in this study are conserved among all 23 different BKV strains, including the 15 complete genomes sequenced by our group, except for a single amino acid change in one epitope of one strain (6), and among 445 JCV sequences available in GenBank. These results suggest that generation of JCV or BKV CTL epitope escape mutants may be unlikely to occur. This was confirmed in our group of KTx recipients with PVN, where sequence analysis of BKV isolates showed no evidence of amino acid substitutions in the p44 and p108 epitopes (data not shown).
Krymskaya et al. (26) recently independently reported cross-tetramer staining results between one of the CTL epitopes defined in our study, the BKV VP1p108 and JCV VP1p100 in healthy subjects, and in two KTx recipients who did not have biopsy evidence of PVN; they claim that our previous studies on JCV-specific CTL in PML should be reappraised (13, 14, 23). In fact, how can one determine whether CTL against the JCV or cross-reactive BKV VP1 epitopes we have defined are directed against one or the other virus in a given individual, especially since most adults have antibodies against both JCV and BKV? To answer this question, it is key to consider the clinical context of the subject. First, PML patients have, by definition, active central nervous system infection with JCV, and 63 to 89% of them have detectable JC viremia (22, 36). Most PML patients reported in our previous studies had AIDS as a predisposing illness, while the others either had hematologic malignancies, were on chronic steroid treatment, or were bone marrow transplant recipients, but none were KTx recipients (25). Since PVN almost exclusively occurs in the latter group, an occult BKV infection could not have been overlooked in our PML patients. In addition, a clear correlation existed not only between the presence of JCV VP1p100- and VP1p36-specific CTL in the blood and a favorable clinical outcome with stabilization of PML and prolonged survival but also with CTL against the whole JCV VP1 protein expressed by recombinant vaccinia virus (24) or pools of overlapping peptides encompassing the entire JCV VP1 protein (12). Furthermore, we have recently detected the same CTL in the cerebral spinal fluid of PML survivors (9), and we have seen evidence that CD8+ T cells are the principal lymphocyte cell type present in PML lesions where they colocalize with JCV-infected glial cells (41). Taken together, these results clearly indicate that the CTL response detected in our previous studies on PML patients was directed against JCV and not against BKV (12, 13, 23, 24).
Similarly, KTx recipients with PVN in the present study had active ongoing BK infection of the renal allograft, which was proven by biopsy, and all had very elevated BK viral load in blood and urine at the time of disease onset. Although all those tested were also JCV seropositive, they had low levels of JCV-specific antibody titers, and their JCV viral load in blood and urine was either undetectable or low and, in most cases, transient. Therefore, the CTL response in these patients appeared clearly directed against BKV, and not JCV. This was not necessarily the case in the single KTx recipient reported by Krymskaya et al. (26), who had CTL recognizing the BKV VP1p108 epitope in the context of BK viruria but who had neither BK viremia nor biopsy evidence of PVN, since the investigators did not quantify the BK viral load in urine and did not test this patient for JCV antibody; nor did they assess whether this patient had JC viruria or viremia.
In our study, analysis of the cellular immune response against BKV provides a very important clue on the pathogenesis of PVN. Although all KTx recipients with PVN had detectable BKV-specific CTL at least at one time point, the magnitude of this response was quite variable between patients, from 0.13% to 74.3% of CD8+ T cells. Indeed, the presence of high levels of BKV-specific CTL in KTx recipients with PVN was associated in most cases with a better control of BK viruria and viremia and low BKV antibody titers, while low levels or undetectable BKV-specific CTL were associated in most patients with higher viremia and viruria and a high BKV antibody response, which was then followed by a decrease in viremia. In addition, despite our limited sample size, a trend emerged in that patients who were able to lower their urine and serum BK viral loads were more likely to have their renal function return to pre-PVN baseline values.
Moreover, the cellular immune response in the periphery may be underestimated since many BKV-specific CTL may likely migrate in the allograft in patients with PVN. In this context, it appears that a strong cellular immune response, as detected in the blood, may be able to control BKV replication in the infected kidney, which decreases both BKV shedding in the urine and spilling into the blood. In absence of a viremic phase, the humoral immune response may not need to be activated. Clearance of BKV from the kidney may lead to recovery of the renal function. Conversely, a weak or absent cellular immune response appears to be unable to control BKV replication in the kidney and results in abundant viruria as well as a viremic phase. Presence of the virus in the blood in turn triggers a humoral immune response. Subsequently, high titers of BKV antibody may be able to clear cell-free virus from the blood but not from its site of intracellular replication in the kidney, causing sustained viruria. Persistence of BKV replication in the kidney associated with inflammation may prevent recovery of renal function. These data illustrate the complex interplay between the cellular and humoral immune responses in KTx recipients with PVN.
Furthermore, KTx recipients with PVN had a different pattern of response against the two CTL epitopes compared to healthy individuals. Indeed, 80% of BKV-seropositive healthy individuals had detectable CTL for at least one of the BKV epitopes, which is comparable to our recent finding that 73% of healthy individuals had CTL recognizing the corresponding JCV epitopes (14). As it was the case for JCV VP1p36 and VP1p100, BKV VP1p44 was more frequently recognized and elicited a stronger response than BKV VP1p108 in healthy individuals. Conversely, the CTL response against BKV VP1p108 was always stronger than BKV VP1p44 in all KTx recipients with PVN, regardless of the magnitude of their cellular immune response. The only exception was observed at the second time point of patient 1 (Fig. 5). This patient had the highest CTL response in our entire cohort soon after PVN onset and was successful at controlling BKV replication in the blood and urine. Of note, data from both healthy individuals and KTx recipients with PVN were obtained after in vitro stimulation of PBMC with the respective peptides. Indeed, we could not detect any CTL ex vivo in fresh, unstimulated blood samples. Therefore, we cannot exclude the potential for in vitro selection to confound frequencies of CD8+ T cells specific for each epitope ex vivo. In this context, these results may suggest that a change in epitope immunodominance hierarchy may occur during active BKV infection in KTx recipients, which may revert back to a pattern seen in healthy individuals once the infection is under control.
Due to the relative shortage of available organs, HLA class I alleles are in most cases partially or totally mismatched between donors and recipients. Whether CTL are able to recognize viral epitopes presented by non-self class I alleles in the allograft and efficiently destroy infected cells is unclear. In fact, several studies have shown a trend for an increased incidence of PVN in KTx recipients of HLA class I-mismatched allografts (2, 18, 30), suggesting that the immune response against BKV may be ineffective in this setting. In line with these observations, our study shows that four of five A*0201+ KTx recipients with PVN occurring in a graft from an A2-negative donor had a low or undetectable CTL response against the A*0201-restricted epitopes (Fig. 4, patients 5 and 8 to 10). However, this did not seem to be the case in the remaining patient in this category (Fig. 4, patient 1) who has a very high CTL response against both A*0201-restricted epitopes associated with viral clearance. Although this patient had another allele (B44) in common with the donor which may have participated in the immune response against BKV, it appears that an efficient recall response was generated via the A*0201 allele. Whether this response was elicited by classical antigen presentation in tissues of the recipient or via cross-recognition of BKV VP1p44 and VP1p108 CTL epitopes on other class I molecules in the infected graft deserves further study.
Findings reported in this study may have broader implications outside of the population of KTx recipients. Indeed, two patients with multiple sclerosis recently developed PML after treatment with a combination of interferon β, an immunomodulator, and natalizumab, a monoclonal antibody binding to α4 integrins on the surface of lymphocytes, which prevents their normal trafficking in the tissues (3, 19, 27). In addition, another patient with Crohn's disease treated with natalizumab also died from PML (39). According to our present data, since the CTL populations that failed to prevent JCV reactivation in these patients may also be responsible for the containment of BKV, patients treated with such a combination of immunomodulatory medications may need to be monitored for BKV reactivation as well as for potential development of kidney disease.
Acknowledgments
We are grateful to Michele Lifton and Darci Gorgone for technical assistance and to Norman Letvin and Dan Barouch for helpful discussion.
This work was supported in part by Public Health Service grant and NS/AI 041198 to I.J.K. and by a grant from the Paul Teschan Research Fund from Dialysis Clinics to J.T.
REFERENCES
- 1.Altman, J. D., P. A. Moss, P. J. Goulder, D. H. Barouch, M. G. McHeyzer-Williams, J. I. Bell, A. J. McMichael, and M. M. Davis. 1996. Phenotypic analysis of antigen-specific T lymphocytes. Science 274:94-96. [DOI] [PubMed] [Google Scholar]
- 2.Awadalla, Y., P. Randhawa, K. Ruppert, A. Zeevi, and R. J. Duquesnoy. 2004. HLA mismatching increases the risk of BK virus nephropathy in renal transplant recipients. Am. J. Transplant. 4:1691-1696. [DOI] [PubMed] [Google Scholar]
- 3.Berger, J. R., and I. J. Koralnik. 2005. Progressive multifocal leukoencephalopathy and natalizumab—unforeseen consequences. N. Engl. J. Med. 353:414-416. [DOI] [PubMed] [Google Scholar]
- 4.Brennan, D. C., I. Agha, D. L. Bohl, M. A. Schnitzler, K. L. Hardinger, M. Lockwood, S. Torrence, R. Schuessler, T. Roby, M. Gaudreault-Keener, and G. A. Storch. 2005. Incidence of BK with tacrolimus versus cyclosporine and impact of preemptive immunosuppression reduction. Am. J. Transplant. 5:582-594. [DOI] [PubMed] [Google Scholar]
- 5.Chen, Y., J. Trofe, J. Gordon, P. Roy-Chaudhury, S. E. Woodle, R. R. Alloway, K. Khalili, and I. J. Koralnik. 2005. Cytotoxic T lymphocytes control BK virus replication in renal transplant recipients with polyomavirus nephropathy. Am. J. Transplant. 5(Suppl. 11):227. [Google Scholar]
- 6.Chen, Y., P. M. Sharp, M. Fowkes, O. Kocher, J. T. Joseph, and I. J. Koralnik. 2004. Analysis of 15 novel full-length BK virus sequences from three individuals: evidence of a high intra-strain genetic diversity. J. Gen. Virol. 85:2651-2663. [DOI] [PubMed] [Google Scholar]
- 7.Drachenberg, C. B., C. O. Beskow, C. B. Cangro, P. M. Bourquin, A. Simsir, J. Fink, M. R. Weir, D. K. Klassen, S. T. Bartlett, and J. C. Papadimitriou. 1999. Human polyoma virus in renal allograft biopsies: morphological findings and correlation with urine cytology. Hum. Pathol. 30:970-977. [DOI] [PubMed] [Google Scholar]
- 8.Drachenberg, R. C., C. B. Drachenberg, J. C. Papadimitriou, E. Ramos, J. C. Fink, R. Wali, M. R. Weir, C. B. Cangro, D. K. Klassen, A. Khaled, R. Cunningham, and S. T. Bartlett. 2001. Morphological spectrum of polyoma virus disease in renal allografts: diagnostic accuracy of urine cytology. Am. J. Transplant. 1:373-381. [PubMed] [Google Scholar]
- 9.Du Pasquier, R. A., P. Autissier, Y. Zheng, J. Jean-Jacques, and I. J. Koralnik. 2005. Presence of JC virus-specific CTL in the cerebrospinal fluid of PML patients: rationale for immune-based therapeutic strategies. AIDS 19:2069-2076. [DOI] [PubMed] [Google Scholar]
- 10.Du Pasquier, R. A., K. W. Clark, P. S. Smith, J. T. Joseph, J. M. Mazullo, U. De Girolami, N. L. Letvin, and I. J. Koralnik. 2001. JCV-specific cellular immune response correlates with a favorable clinical outcome in HIV-infected individuals with progressive multifocal leukoencephalopathy. J. Neurovirol. 7:318-322. [DOI] [PubMed] [Google Scholar]
- 11.Du Pasquier, R. A., S. Corey, D. H. Margolin, K. Williams, L. A. Pfister, U. De Girolami, J. J. Mac Key, C. Wuthrich, J. T. Joseph, and I. J. Koralnik. 2003. Productive infection of cerebellar granule cell neurons by JC virus in an HIV+ individual. Neurology 61:775-782. [DOI] [PubMed] [Google Scholar]
- 12.Du Pasquier, R. A., M. J. Kuroda, J. E. Schmitz, Y. Zheng, K. Martin, F. W. Peyerl, M. Lifton, D. Gorgone, P. Autissier, N. L. Letvin, and I. J. Koralnik. 2003. Low frequency of cytotoxic T lymphocytes against the novel HLA-A*0201-restricted JC virus epitope VP1p36 in patients with proven or possible progressive multifocal leukoencephalopathy. J. Virol. 77:11918-11926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Du Pasquier, R. A., M. J. Kuroda, Y. Zheng, J. Jean-Jacques, N. L. Letvin, and I. J. Koralnik. 2004. A prospective study demonstrates an association between JC virus-specific cytotoxic T lymphocytes and the early control of progressive multifocal leukoencephalopathy. Brain 127:1970-1978. [DOI] [PubMed] [Google Scholar]
- 14.Du Pasquier, R. A., J. E. Schmitz, J. Jean-Jacques, Y. Zheng, J. Gordon, K. Khalili, N. L. Letvin, and I. J. Koralnik. 2004. Detection of JC virus-specific cytotoxic T lymphocytes in healthy individuals. J. Virol. 78:10206-10210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gordon, J., D. Brennan, A. Limaye, P. Randhawa, G. Storch, J. Trofe, K. Weck, and H. H. Hirsch. 2005. Multicenter validation of polyomavirus BK quantification for screening and monitoring of renal transplant recipients. Am. J. of Transplant. 5(Suppl. 11):381-382. [Google Scholar]
- 16.Hatwell, J. N., and P. M. Sharp. 2000. Evolution of human polyomavirus JC. J. Gen. Virol. 81:1191-1200. [DOI] [PubMed] [Google Scholar]
- 17.Hirsch, H. H., D. C. Brennan, C. B. Drachenberg, F. Ginevri, J. Gordon, A. P. Limaye, M. J. Mihatsch, V. Nickeleit, E. Ramos, P. Randhawa, R. Shapiro, J. Steiger, M. Suthanthiran, and J. Trofe. 2005. Polyomavirus-associated nephropathy in renal transplantation: interdisciplinary analyses and recommendations. Transplantation 79:1277-1286. [DOI] [PubMed] [Google Scholar]
- 18.Hirsch, H. H., W. Knowles, M. Dickenmann, J. Passweg, T. Klimkait, M. J. Mihatsch, and J. Steiger. 2002. Prospective study of polyomavirus type BK replication and nephropathy in renal-transplant recipients. N. Engl. J. Med. 347:488-496. [DOI] [PubMed] [Google Scholar]
- 19.Kleinschmidt-DeMasters, B. K., and K. L. Tyler. 2005. Progressive multifocal leukoencephalopathy complicating treatment with natalizumab and interferon beta-1a for multiple sclerosis. N. Engl. J. Med. 353:369-374. [DOI] [PubMed] [Google Scholar]
- 20.Knowles, W. A., P. Pipkin, N. Andrews, A. Vyse, P. Minor, D. W. Brown, and E. Miller. 2003. Population-based study of antibody to the human polyomaviruses BKV and JCV and the simian polyomavirus SV40. J. Med. Virol. 71:115-123. [DOI] [PubMed] [Google Scholar]
- 21.Koralnik, I. J. 2002. Overview of the cellular immunity against JC virus in progressive multifocal leukoencephalopathy. J. Neurovirol. 8(Suppl. 2):59-65. [DOI] [PubMed] [Google Scholar]
- 22.Koralnik, I. J., D. Boden, V. X. Mai, C. I. Lord, and N. L. Letvin. 1999. JC virus DNA load in patients with and without progressive multifocal leukoencephalopathy. Neurology 52:253-260. [DOI] [PubMed] [Google Scholar]
- 23.Koralnik, I. J., R. A. Du Pasquier, M. J. Kuroda, J. E. Schmitz, X. Dang, Y. Zheng, M. Lifton, and N. L. Letvin. 2002. Association of prolonged survival in HLA-A2+ progressive multifocal leukoencephalopathy patients with a CTL response specific for a commonly recognized JC virus epitope. J. Immunol. 168:499-504. [DOI] [PubMed] [Google Scholar]
- 24.Koralnik, I. J., R. A. Du Pasquier, and N. L. Letvin. 2001. JC virus-specific cytotoxic T lymphocytes in individuals with progressive multifocal leukoencephalopathy. J. Virol. 75:3483-3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koralnik, I. J., D. Schellingerhout, and M. P. Frosch. 2004. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 14-2004. A 66-year-old man with progressive neurologic deficits. N. Engl. J. Med. 350:1882-1893. [DOI] [PubMed] [Google Scholar]
- 26.Krymskaya, L., M. C. Sharma, J. Martinez, W. Haq, E. C. Huang, A. P. Limaye, D. J. Diamond, and S. F. Lacey. 2005. Cross-reactivity of T lymphocytes recognizing a human cytotoxic T-lymphocyte epitope within BK and JC virus VP1 polypeptides. J. Virol. 79:11170-11178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Langer-Gould, A., S. W. Atlas, A. J. Green, A. W. Bollen, and D. Pelletier. 2005. Progressive multifocal leukoencephalopathy in a patient treated with natalizumab. N. Engl. J. Med. 353:375-381. [DOI] [PubMed] [Google Scholar]
- 28.Leung, A. Y., C. K. Suen, A. K. Lie, R. H. Liang, K. Y. Yuen, and Y. L. Kwong. 2001. Quantification of polyoma BK viruria in hemorrhagic cystitis complicating bone marrow transplantation. Blood 98:1971-1978. [DOI] [PubMed] [Google Scholar]
- 29.Mathur, V. S., J. L. Olson, T. M. Darragh, and T. S. Yen. 1997. Polyomavirus-induced interstitial nephritis in two renal transplant recipients: case reports and review of the literature. Am. J. Kidney Dis. 29:754-758. [PubMed] [Google Scholar]
- 30.Mengel, M., M. Marwedel, J. Radermacher, G. Eden, A. Schwarz, H. Haller, and H. Kreipe. 2003. Incidence of polyomavirus-nephropathy in renal allografts: influence of modern immunosuppressive drugs. Nephrol. Dial. Transplant. 18:1190-1196. [DOI] [PubMed] [Google Scholar]
- 31.Miller, N. R., E. O. Major, and W. C. Wallen. 1983. Transfection of human fetal glial cells with molecularly cloned JCV DNA. Prog. Clin. Biol. Res. 105:29-40. [PubMed] [Google Scholar]
- 32.Parker, K. C., M. A. Bednarek, and J. E. Coligan. 1994. Scheme for ranking potential HLA-A2 binding peptides based on independent binding of individual peptide side-chains. J. Immunol. 152:163-175. [PubMed] [Google Scholar]
- 33.Parker, K. C., M. Shields, M. DiBrino, A. Brooks, and J. E. Coligan. 1995. Peptide binding to MHC class I molecules: implications for antigenic peptide prediction. Immunol. Res. 14:34-57. [DOI] [PubMed] [Google Scholar]
- 34.Radhakrishnan, S., J. Gordon, L. Del Valle, J. Cui, and K. Khalili. 2004. Intracellular approach for blocking JC virus gene expression by using RNA interference during viral infection. J. Virol. 78:7264-7269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Randhawa, P. S., S. Finkelstein, V. Scantlebury, R. Shapiro, C. Vivas, M. Jordan, M. M. Picken, and A. J. Demetris. 1999. Human polyoma virus-associated interstitial nephritis in the allograft kidney. Transplantation 67:103-109. [DOI] [PubMed] [Google Scholar]
- 36.Tornatore, C., J. R. Berger, S. A. Houff, B. Curfman, K. Meyers, D. Winfield, and E. O. Major. 1992. Detection of JC virus DNA in peripheral lymphocytes from patients with and without progressive multifocal leukoencephalopathy. Ann. Neurol. 31:454-462. [DOI] [PubMed] [Google Scholar]
- 37.Trofe, J., T. Cavallo, M. R. First, P. Weiskittel, V. R. Peddi, P. Roy-Chaudhury, R. R. Alloway, S. Safdar, J. F. Buell, M. J. Hanaway, and E. S. Woodle. 2002. Polyomavirus in kidney and kidney-pancreas transplantation: a defined protocol for immunosuppression reduction and histologic monitoring. Transplant. Proc. 34:1788-1789. [DOI] [PubMed] [Google Scholar]
- 38.Trofe, J., J. Gordon, P. Roy-Chaudhury, I. J. Koralnik, W. J. Atwood, R. R. Alloway, K. Khalili, and E. S. Woodle. 2004. Polyomavirus nephropathy in kidney transplantation. Prog. Transplant. 14:130-140. [DOI] [PubMed] [Google Scholar]
- 39.Van Assche, G., M. Van Ranst, R. Sciot, B. Dubois, S. Vermeire, M. Noman, J. Verbeeck, K. Geboes, W. Robberecht, and P. Rutgeerts. 2005. Progressive multifocal leukoencephalopathy after natalizumab therapy for Crohn's disease. N. Engl. J. Med. 353:362-368. [DOI] [PubMed] [Google Scholar]
- 40.Walker, D. L., and B. L. Padgett. 1983. The epidemiology of human polyomaviruses. Prog. Clin. Biol. Res. 105:99-106. [PubMed] [Google Scholar]
- 41.Wuthrich, C., K. S. Kim, W. K. Williams, K., Gelman, R., Elmeric, D., Girolami, U. D., Joseph, J. T., Hedley-Whyte, T., and Koralnik, I. J. 2005. Characterization of lymphocytic infiltrates in progressive multifocal leukoencephalopathy: Colocalization of CD8+ T cells with JCV-infected glial cells. J. Neurovirol. 11(Suppl. 2):21. [DOI] [PubMed] [Google Scholar]