Systemic lupus erythematosus (SLE) is a multisystem autoimmune connective tissue disorder with various clinical presentations. It is prevalent among young women with a peak age of onset between the late teens and early 40s and a female to male ratio of 9:1. It is more common in certain ethnic groups, such as people with African or Asian ancestry. One study estimated the prevalence of lupus as 27.7/100 000 and as high as 206/100 000 in Afro-Caribbean women.1 SLE is a chronic illness that may be life threatening when major organs are affected but more commonly results in chronic debilitating ill health. No single cause for SLE has been identified, though factors such as sunlight and drugs may precipitate the condition, and there is a complex genetic basis. Autoantibodies may be present for many years before the clinical onset of the disease, and there may be increasing numbers of antibodies just before symptoms develop, pointing to a multi-factorial pathogenesis.2
Sources and selection criteria
I used PubMed to identify references, supplemented by review articles and lectures from the American College of Rheumatology annual conference in 2005. Search terms included systemic lupus erythematosus, antiphospholipid syndrome, lupus nephritis, central nervous system disease in lupus, and fatigue. Articles were selected according to their impact on clinical practice. It is not possible to give a comprehensive guide to the management of all the possible complications of lupus so I have focused on areas where there is a consensus on management or where there have been major new developments.
Clinical presentation
The widely recognised presentation of a young woman with inflammatory arthritis and a butterfly facial rash is uncommon. Non-specific symptoms of fatigue, malaise, oral ulcers, arthralgia, photosensitive skin rashes, lymphadenopathy, pleuritic chest pains, headache, paraesthesiae, symptoms of dry eyes and mouth, Raynaud's phenomenon, and mild hair loss are more likely presentations. It is not surprising therefore that there is often considerable delay before the diagnosis is considered in patients with low grade disease. Patients may present acutely with major organ dysfunction that can affect virtually any organ, and diagnosis hinges on careful and thorough clinical evaluation and recognition of multisystem involvement. Renal involvement (lupus nephritis) presents insidiously, and if it is not detected early, the risk of progression to renal impairment is high.
Summary points
Clinical presentations of systemic lupus erythematosus (SLE) range from chronic debilitating disease to life threatening organ dysfunction
Early diagnosis is central to improving prognosis
The antiphospholipid (Hughes) syndrome is commonly associated with SLE and can lead to recurrent thromboses and loss of pregnancy
Malarial drugs, low dose corticosteroids, and immunosuppressive drugs are effective treatments, and newer agents such as mycophenolate mofetil and biological agents are promising
Exogenous oestrogens may have a lower risk of lupus flares than previously thought but are still associated with a risk of thrombosis
Accelerated atherosclerosis remains a considerable challenge
The key to early diagnosis is clinical evaluation, which should include a complete systems review and examination and investigations guided by the extent of organ involvement. In primary care, a diagnosis of lupus or a related disorder is often apparent after clinical assessment, urinalysis for blood and protein, and basic investigations such as full blood count (often showing anaemia or cytopenia), renal and liver function, and acute phase reactants: a high erythrocyte sedimentation rate (ESR) with a normal C reactive protein (CRP) concentration are characteristic. A search for autoantibodies to nuclear antigens (antinuclear and antiDNA antibodies) and rheumatoid factor are the usual starting points while considering referral to specialist care. Antiphospholipid antibodies (anticardiolipin antibodies and the lupus anticoagulant) should be considered in women with previous morbidity in pregnancy or thrombotic events. In secondary care, more extensive testing is usually considered including detailed assessment of organ dysfunction and further autoantibody testing including complement levels and antibodies to the extractable nuclear antigens (ENA) such as Ro (SS-A), La (SS-B), ribonucleoprotein (RNP), and Sm.
It is difficult to predict which patients will progress to severe multisystem disease with a poor outcome. In general morbidity and mortality is higher in patients with extensive multisystem disease and multiple autoantibodies. Prognosis ultimately depends on the amount of damage (permanent scars or irreversible organ dysfunction) accrued over the course of the disease. Treatment therefore aims to eliminate inflammation and thrombosis, minimising damage. Accelerated atherosclerosis is now recognised as a major contributor to premature death through myocardial infarction and cerebrovascular disease.
Management of SLE
Most stable patients can be managed jointly between primary and secondary care. Primary care can contribute to monitoring patients with regular urinalysis, measurement of blood pressure, and renal, lipid, and glucose profiles, especially in patients on corticosteroids. Blood monitoring of immunosuppressive agents can also be undertaken jointly with shared care protocols. Early identification of disease flares is important, and secondary care facilities should be rapidly accessible for these patients.
Fatigue
Fatigue is a common and debilitating symptom that has proved difficult to evaluate and treat. The pathogenesis of lupus fatigue is complex, and it impacts severely on the quality of life. Factors determining fatigue include depression, pain, poor sleep quality, poor physical fitness, perceived lack of social support, and disease activity.w1 Fatigue can be severe even when lupus is in remission. Identification of contributory factors such as anaemia and hypo-thyroidism are worthwhile as is treatment for depression, a common occurrence in any chronic illness. Two clinical trials of supervised exercise programmes showed benefit in terms of aerobic capacity, quality of life, and depression, and one study showed improvements in fatigue without causing disease flares, though the beneficial effects disappeared when the exercise programmes stopped.w2 3 Anecdotal evidence suggests that treatment with antimalarial drugs may also be useful, though this is controversial and there are no trials to support this.
Arthralgia and skin rashes
Patients with isolated cutaneous lupus, including discoid lupus, are unlikely to progress to systemic disease and often respond to topical therapies. Weak topical steroid preparations in combination with hydroxychloroquine are often useful. More recently, topical preparations of tacrolimus and pimecrolimus have shown benefit in small open case series.w3 w4
Though non-steroidal anti-inflammatory agents (NSAIDs) are widely prescribed for lupus patients with arthralgia, simple analgesics should be used. In particular the COX 2 selective agents are contra-indicated because of the potential cardiovascular risks, and even conventional NSAIDs are not without gastrointestinal, renal, and cardiovascular risks.
Hydroxychloroquine remains the mainstay for patients with mild SLE, especially for those with arthralgia, skin rashes, alopecia, and oral or genital ulceration (fig 1). It should be considered in all patients as it is well tolerated and is disease modifying as well as having other useful properties including a weak antithrombotic action.w5 w6 Other beneficial effects on serum lipids and blood glucose profiles and a lower risk of cataracts make it especially useful in patients who also need long term corticosteroids. Mepacrine is another safe antimalarial widely used in mild lupus, often in small doses and in combination with hydroxychloroquine when the latter has failed to produce a response on its own. Ocular toxicity is rare and, providing there is no major renal impairment and vision is checked annually, long term antimalarial therapy is relatively safe. No blood monitoring is needed, but patients should be warned about the risk of skin rashes, which may occur in 5-10% of patients and resolve on withdrawal.
Fig 1.

33 year old woman with anti-Ro (SS-A) antibodies and subacute cutaneous lupus responding to combination therapy with mepacrine and methotrexate
Lupus nephritis
The most dramatic advances in treatment have been for patients with lupus nephritis—a powerful predictor of prognosis. The established and widely used regimen of long term high dose monthly or quarterly intravenous “pulse” cyclophosphamide pioneered by the National Institutes of Health (NIH) has been challenged on several fronts. Recent studies have shown that short courses of low dose pulse cyclophosphamide followed by azathioprine achieve similar results to the NIH regimen with less toxicity.4 Mycophenolate mofetil, widely used in organ transplantation, is also showing tremendous potential in randomised controlled trials as both induction and maintenance therapy for severe proliferative lupus nephritis and may eventually supersede the use of cyclophosphamide for most patients.5,6
Central nervous system disease
Central nervous system (CNS) disease in lupus remains a challenge in terms of pathogenesis, assessment, and treatment, and it may be better to consider CNS disease in terms of separate syndromes. Indeed the American College of Rheumatology classification criteria for CNS lupus has changed considerably from just seizures and psychosis to 19 different syndromes.w7 There is now a clear distinction between CNS manifestations due to lupus and those due to the antiphospholipid (Hughes) syndrome (APS). Neuropsychiatric manifestations attributable to antiphospholipid syndrome include strokes, seizures, movement disorders, transverse myelopathy, demyelination syndromes, transient ischaemic attacks, cognitive dysfunction, visual loss, and headaches including migraine.7 The differential diagnosis between multiple sclerosis and demyelination associated with APS may be difficult on imaging grounds,w8 though electroencephalography may indicate cerebrovascular insufficiency in antiphospholipid syndrome.8 Seizures are an important feature—in lupus patients these are more likely to be associated with antiphospholipid syndrome than with cerebral vasculitis, which is extremely rare in practice.9
The treatment of CNS lupus varies according to the particular clinical syndrome—for example, organic brain syndromes and psychosis are managed by multidisciplinary teams with corticosteroids, immunosuppression, and antipsychotic medication. There is no consensus on the ideal immunosuppressive agent (there are no clinical trials), though intravenous cyclophosphamide, methotrexate, and azathioprine may be considered. Predominantly thrombotic manifestations such as strokes, transient ischaemic attacks, seizures, and cognitive dysfunction associated with antiphospholipid antibodies may need anticoagulation.
Antiphospholipid (Hughes) syndrome
Though initially described in the context of SLE, it is clear that antiphospholipid syndrome is a syndrome in its own right that may complicate various autoimmune disorders. The hallmarks of arterial and venous thromboses and recurrent morbidity in pregnancy, often with livedo reticularis and thrombocytopenia, have stood the test of time.10 Many clinical features arise from thrombosis in any organ system. Catastrophic antiphospholipid syndrome, characterised by severe widespread thrombosis, occurs in about 1% of patients with antiphospholipid syndrome and remains a serious complication with a poor prognosis. Treatment includes plasma exchange, corticosteroids, and intravenous immunoglobulin but immunosuppression, especially with cyclophosphamide, increases mortality.11
Pulmonary hypertension is a rare complication of lupus and may also be associated with antiphospholipid antibodies.w9 Advances have been made in identifying patients with pulmonary hypertension associated with autoimmune rheumatic diseases. Treatment with agents such as sildenafil and bosentan, as well as the more established epoprostenol (prostacyclin) analogues, is promising.
Primary antiphospholipid syndrome rarely progresses to SLE. Antiphospholipid syndrome in patients who already have SLE, however, considerably increases the risk of damage and death.12 The spectrum of clinical features of antiphospholipid syndrome continues to broaden with descriptions of renal artery stenosis,13 metatarsal fractures,14 avascular necrosis,w10 and abnormalities of vascular function.15 One of the features distinguishing Hughes syndrome from other coagulopathies is the tendency to develop heart valve disease, sometimes progressing rapidly to replacement.
Treatment remains controversial in terms of the level of anticoagulation required to prevent recurrent thromboses. Clinical trials suggest that for most patients with recurrent venous thrombotic events a target international normalised ratio (INR) of 2.0-3.0 provides reasonable protection against further thrombosis with a low risk of bleeding.16,17 Patients at high risk of recurrent arterial thrombosis may continue to need higher target ratios of 3.0-4.5. Precise control is critical in this prothrombotic condition, and we encourage self testing in our unit, which has improved outcome.18
Cardiovascular risk
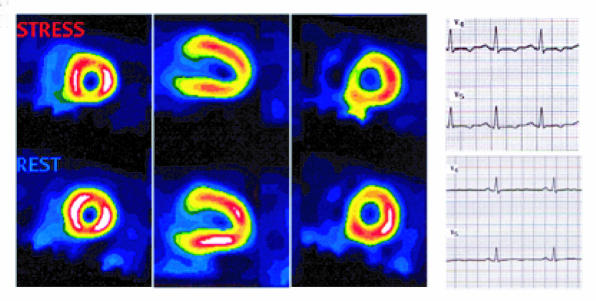
Women with SLE are at a considerably increased risk of premature atherosclerosis (fig 2). This seems to be independent of traditional cardiovascular risk factors, and lupus itself may contribute to the development of atherosclerosis. Inflammatory disease activity over long periods of time probably results in endothelial and vascular damage leading to atherosclerosis. Intensive management of disease activity with aggressive reduction of risk factors will be critical to improving outcome—an approach that is similar to management in diabetes. The role of corticosteroids remains unclear. Corticosteroids, especially in high doses, produce glucose intolerance, hypertension, central obesity, and dyslipidaemia. Low dose corticosteroids and other drugs such as antimalarials and immunosuppressive agents, however, may actually reduce the risk of atherosclerosis by minimising vascular damage.19-21
Fig 2.
Woman aged 43 years with a 20 year history of SLE, lupus nephritis, and antiphospholipid syndrome presenting with angina. Nuclear medicine Myoview scan shows reversible ischaemia with S-T changes on stress. Coronary angiography confirmed diffuse coronary artery disease
Tips for general practitioners
Consider lupus when symptoms arise in several systems, especially in patients with African or Asian ancestry. An increased erythrocyte sedimentation rate with a normal C reactive protein concentration is characteristic of lupus in the absence of infection. Testing for antinuclear antibodies and rheumatoid factor is useful. Consider early referral to a specialist
Antiphospholipid syndrome should be considered in patients with unexplained thrombotic events or losses of pregnancy, or both. Screening includes anticardiolipin antibodies and the lupus anticoagulant
Urinalysis and evaluation of renal function and blood pressure may detect early renal disease, which is treatable
Accelerated atherosclerosis is prevalent in autoimmune rheumatic diseases—intensive modification of risk factors and control of inflammatory disease are essential
Pregnancy, contraceptive pills, and hormone replacement therapy
SLE particularly affects young women, and pregnancy is associated with higher risks of complications. In general, providing that lupus is in remission at conception, the outcomes are good but may still be poorer than in otherwise healthy women.
Morbidity in pregnancy is common, especially if women have antiphospholipid antibodies. Complications include recurrent early loss of pregnancy, fetal death, pre-eclampsia, intrauterine growth restriction, and preterm delivery; and women are at increased risk of maternal thrombosis especially in the puerperium.
Risks of pregnancy increase markedly in the presence of lupus nephritis, hypertension, and active disease, especially at the time of conception, and pregnancy is contraindicated until remission can be achieved. Though pulmonary hypertension in lupus is uncommon, in pregnancy it confers a high risk of maternal death. All women with lupus should receive careful counselling before planning a pregnancy, both in terms of control of the disease and medications potentially toxic to the fetus.w11 Specialist multidisciplinary units may increase the chances of successful outcomes.
Further information for patients
St Thomas Lupus Trust (www.lupus.org.uk)—St Thomas' Lupus Trust, Louise Coote Lupus Unit, Gassiot House, St Thomas' Hospital, London SE1 7EH (tel: 020 7188 3562)
Hughes Syndrome Foundation (www.hughessyndrome.org)—The Hughes Syndrome Foundation, Louise Coote Lupus Unit, Gassiot House, St Thomas' Hospital, London SE1 7EH (tel: 020 7188 8217)
Lupus UK (www.lupusuk.com)—LUPUS UK, St James House, Eastern Road, Romford, Essex RM1 3NH (tel: 01708 731251)
Arthritis Research Campaign (www.arc.org.uk)—Arthritis Research Campaign, Copeman House, St Mary's Court, St Mary's Gate, Chesterfield, Derbyshire S41 7TD (tel: 0870 850 5000 or 01246 558033)
The role of exogenous hormones such as the contraceptive pill and hormone replacement therapy (HRT) in exacerbating or precipitating lupus has been controversial. Oestrogens might increase the risk of a disease flare in women with lupus. Two randomised controlled studies, however, recently suggested that use of the contraceptive pill does not significantly increase the risk of disease activity or disease flares over one year.22,23 A further randomised placebo controlled study of HRT showed significantly more mild to moderate flares (but no increase in major flares) in the HRT group compared with the placebo group.24 All these studies emphasise the risk of thrombosis associated with lupus, especially in the presence of antiphospholipid antibodies.
Novel treatments
There have been major advances in the treatment of SLE, especially with biological agents. Rituximab is a chimeric human-murine monoclonal antibody directed against CD-20 on B cells and their precursors but not against plasma cells. Rituximab is widely used in the management of lymphoma and is relatively safe and well tolerated. Several open studies have shown dramatic and long lasting remissions after only two to four infusions in patients who were previously unresponsive to conventional and even novel immunosuppressive agents such as mycophenolate mofetil.25 w12 The optimum combination of rituximab with methylprednisolone and cyclophosphamide remains unclear.
Intravenous immunoglobulins are increasingly being used in the treatment of resistant lupus, though there have been no large randomised trials. They also have a role in patients who have concomitant infection and active lupus, in whom immunosuppression is risky, and have been used in the treatment of many clinical manifestations in SLE.w13
Clinical trials are currently assessing the potential of various peptides and biological agents such as abatacept (CTLA4 Ig) and epratuzmab in lupus. To date no medications of any class have ever been officially licensed for use in lupus, and these trials offer hope that several agents may be registered specifically for lupus patients.
Conclusion
Lupus was once considered a rare disease with a universally fatal outcome. The past 20 years have shown that this disorder is common and treatable. Most patients now have almost normal life spans. Delay in diagnosis, especially in patients with low grade disease, remains a problem, but the future is promising in terms of potential new treatments. The remaining challenges include improving the quality of life for patients by minimising use of corticosteroids, reducing infections and fatigue, and minimising cardiovascular risks that still claim considerable loss of life.
Supplementary Material
I am grateful to G R V Hughes and M B Y Saldanha for their comments on the manuscript.
Contributor: DPDC is the sole author.
Competing interests: I have received lecture fees and honorariums from Aspreva Pharmaceuticals, and I am participating in clinical trials organised by Bristol Myers Squibb, Teva Pharmaceuticals, Aspreva, and Immunomedics.
Ethical approval: Not required.
 Further references (w1-w13) are on bmj.com.
Further references (w1-w13) are on bmj.com.
References
- 1.Johnson AE, Gordon C, Palmer RG, Bacon PA. The prevalence and incidence of systemic lupus erythematosus in Birmingham, England. Relationship to ethnicity and country of birth. Arthritis Rheum 1995;38: 551-8. [DOI] [PubMed] [Google Scholar]
- 2.Arbuckle MR, McClain MT, Rubertone MV, Scofield RH, Dennis GJ, James JA, et al. Development of autoantibodies before the clinical onset of systemic lupus erythematosus. N Engl J Med 2003;349: 1526-33. [DOI] [PubMed] [Google Scholar]
- 3.Tench CM, McCarthy J, McCurdie I, White PD, D'Cruz DP. Fatigue in systemic lupus erythematosus: a randomized controlled trial of exercise. Rheumatology (Oxford) 2003;42: 1050-4. [DOI] [PubMed] [Google Scholar]
- 4.Houssiau FA, Vasconcelos C, D'Cruz D, Sebastiani GD, de Ramon Garrido E, Danieli MG, et al. Early response to immunosuppressive therapy predicts good renal outcome in lupus nephritis: lessons from long-term follow-up of patients in the Euro-lupus nephritis trial. Arthritis Rheum 2004;50: 3934-40. [DOI] [PubMed] [Google Scholar]
- 5.Ginzler EM, Dooley MA, Aranow C, Kim MY, Buyon J, Merrill JT, et al. Mycophenolate mofetil or intravenous cyclophosphamide for lupus nephritis. N Engl J Med 2005;353: 2219-28. [DOI] [PubMed] [Google Scholar]
- 6.Contreras G, Pardo V, Leclercq B, Lenz O, Tozman E, O'Nan P, et al. Sequential therapies for proliferative lupus nephritis. N Engl J Med 2004;350: 971-80. [DOI] [PubMed] [Google Scholar]
- 7.Sanna G, Bertolaccini ML, Cuadrado MJ, Laing H, Khamashta MA, Mathieu A, et al. Neuropsychiatric manifestations in systemic lupus erythematosus: prevalence and association with antiphospholipid antibodies. J Rheumatol 2003;30: 985-92. [PubMed] [Google Scholar]
- 8.Lampropoulos CE, Koutroumanidis M, Reynolds PP, Manidakis I, Hughes GR, D'Cruz DP. Electroencephalography in the assessment of neuropsychiatric manifestations in antiphospholipid syndrome and systemic lupus erythematosus. Arthritis Rheum 2005;52: 841-6. [DOI] [PubMed] [Google Scholar]
- 9.Shoenfeld Y, Lev S, Blatt I, Blank M, Font J, von Landenberg P, et al. Features associated with epilepsy in the antiphospholipid syndrome. J Rheumatol 2004;31: 1344-8. [PubMed] [Google Scholar]
- 10.Hughes GRV. Thrombosis, abortion, cerebral disease, and the lupus anticoagulant. BMJ 1983;287: 1088-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asherson RA, Cervera R, de Groot PG, Erkan D, Boffa MC, Piette JC, et al. Catastrophic Antiphospholipid Syndrome Registry Project Group. Catastrophic antiphospholipid syndrome: international consensus statement on classification criteria and treatment guidelines. Lupus 2003; 12: 530-4. [DOI] [PubMed] [Google Scholar]
- 12.Ruiz-Irastorza G, Egurbide MV, Ugalde J, Aguirre C. High impact of antiphospholipid syndrome on irreversible organ damage and survival of patients with systemic lupus erythematosus. Arch Intern Med 2004; 164: 77-82. [DOI] [PubMed] [Google Scholar]
- 13.Sangle SR, D'Cruz DP, Jan W, Karim MY, Khamashta MA, Abbs IC, et al. Renal artery stenosis in the antiphospholipid (Hughes) syndrome and hypertension. Ann Rheum Dis 2003;62: 999-1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sangle S, D'Cruz DP, Khamashta MA, Hughes GR. Antiphospholipid antibodies, systemic lupus erythematosus, and non-traumatic metatarsal fractures. Ann Rheum Dis 2004;63: 1241-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baron MA, Khamashta MA, Hughes GR, D'Cruz DP. Prevalence of an abnormal ankle-brachial index in patients with primary antiphospholipid syndrome: preliminary data. Ann Rheum Dis 2005;64: 144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crowther MA, Ginsberg JS, Julian J, Denburg J, Hirsh J, Douketis J, et al. A comparison of two intensities of warfarin for the prevention of recurrent thrombosis in patients with the antiphospholipid antibody syndrome. N Engl J Med 2003;349: 1133-8. [DOI] [PubMed] [Google Scholar]
- 17.Finazzi G, Marchioli R, Brancaccio V, Schinco P, Wisloff F, Musial J, et al. A randomized clinical trial of high-intensity warfarin vs. conventional antithrombotic therapy for the prevention of recurrent thrombosis in patients with the antiphospholipid syndrome (WAPS). J Thromb Haemost 2005;3: 848-53. [DOI] [PubMed] [Google Scholar]
- 18.Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P. Self-monitoring of oral anticoagulation: a systematic review and meta-analysis. Lancet 2006;367: 404-11. [DOI] [PubMed] [Google Scholar]
- 19.Roman MJ, Shanker BA, Davis A, Lockshin MD, Sammaritano L, Simantov R, et al. Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Engl J Med 2003;349: 2399-406. [DOI] [PubMed] [Google Scholar]
- 20.Asanuma Y, Oeser A, Shintani AK, Turner E, Olsen N, Fazio S, et al. Premature coronary-artery atherosclerosis in systemic lupus erythematosus. N Engl J Med 2003;349: 2407-15. [DOI] [PubMed] [Google Scholar]
- 21.El-Magadmi M, Bodill H, Ahmad Y, Durrington PN, Mackness M, Walker M, et al. Systemic lupus erythematosus: an independent risk factor for endothelial dysfunction in women. Circulation 2004;110: 399-404. [DOI] [PubMed] [Google Scholar]
- 22.Petri M, Kim MY, Kalunian KC, Grossman J, Hahn BH, Sammaritano LR, et al. OC-SELENA Trial. Combined oral contraceptives in women with systemic lupus erythematosus. N Engl J Med 2005;353: 2550-8. [DOI] [PubMed] [Google Scholar]
- 23.Sanchez-Guerrero J, Uribe AG, Jimenez-Santana L, Mestanza-Peralta M, Lara-Reyes P, Seuc AH, et al. A trial of contraceptive methods in women with systemic lupus erythematosus. N Engl J Med 2005;353: 2539-49. [DOI] [PubMed] [Google Scholar]
- 24.Buyon JP, Petri MA, Kim MY, Kalunian KC, Grossman J, Hahn BH, et al. The effect of combined estrogen and progesterone hormone replacement therapy on disease activity in systemic lupus erythematosus: a randomized trial. Ann Intern Med 2005;142: 953-62. [DOI] [PubMed] [Google Scholar]
- 25.Leandro MJ, Edwards JC, Cambridge G, Ehrenstein MR, Isenberg DA. An open study of B lymphocyte depletion in systemic lupus erythematosus. Arthritis Rheum 2002;46: 2673-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.