Abstract
Safe induction of autoantigen-specific long-term tolerance is the “holy grail” for the treatment of autoimmune diseases. In animal models of type 1 diabetes, oral or i.n. immunization with islet antigens induces Tregs that are capable of bystander suppression. However, such interventions are only effective early in the prediabetic phase. Here, we demonstrate that a novel combination treatment with anti-CD3ε–specific antibody and i.n. proinsulin peptide can reverse recent-onset diabetes in 2 murine diabetes models with much higher efficacy than with monotherapy with anti-CD3 or antigen alone. In vivo, expansion of CD25+Foxp3+ and insulin-specific Tregs producing IL-10, TGF-β, and IL-4 was strongly enhanced. These cells could transfer dominant tolerance to immunocompetent recent-onset diabetic recipients and suppressed heterologous autoaggressive CD8 responses. Thus, combining a systemic immune modulator with antigen-specific Treg induction is more efficacious in reverting diabetes. Since Tregs act site-specifically, this strategy should also be expected to reduce the potential for systemic side effects.
Introduction
Type 1 diabetes (T1D) is one of the most common autoimmune diseases, affecting almost 20 million people worldwide. During pathogenesis, insulin-producing pancreatic β cells are progressively destroyed by autoreactive CD4+ and CD8+ T cells. A destruction of approximately 80% of β cells occurs before type 1 patients become symptomatic. Importantly, insulin has been shown to be a major autoantigen in NOD mice as well as in humans (1, 2). In the past 2 decades, immunomodulatory approaches to prevent or cure T1D have been developed and tested, with some encouraging recent results. Development of a cure for T1D has been particularly difficult, because insulin substitution affords a reasonable life quality and expectancy, the disease frequently affects young adults and children, and therefore, the ethical window for any treatment is rather small, and long-term side effects have to be avoided. Thus, the risk-benefit ratio for future clinical trials has to be carefully weighed. On the other hand, insulin cannot prevent all of the late complications of diabetes, and life expectancy can be reduced by 10 to 15 years due to serious complications including retinopathy, nephropathy, cardiovascular diseases, or neuropathy (3).
It is known that systemic immunosuppression, for example with cyclosporin, can halt β cell destruction (4). However, the protection only lasted as long as the drug was present; long-term immunological tolerance to β cell antigens was not achieved, and extended therapy was not feasible due to side effects. In contrast, one much more promising intervention tested clinically during the past 5 years is the application of non–Fc-binding anti-CD3ε Ab, engineered as an F(ab′)2 fragment of hamster anti-CD3ε (145-2C11) for preclinical studies (5) or as a fully humanized IgG1 (hOKT3γ1[Ala-Ala]) for human trials (6). Although, its mechanism of action is not fully known yet, a decrease in the number of autoaggressive T cells together with an expansion of a CD4+ Treg population expressing the α-chain of the IL-2 receptor (CD25) relying on TGF-β have both been demonstrated following short-course treatment with anti-CD3 in NOD mice (7). Thus, the increase in the number of such Tregs might explain the long-term protection observed in mice treated with anti-CD3 after recent onset, as well as the slowing of the progressive decline in C-peptide levels over an 18-month period following short-course treatment in 2 independent trials in humans (8, 9). However, the level of C-peptide began to decline after 18 months, indicating that permanent tolerance to β cell antigens had not been achieved. Therefore, efficacy needs to be enhanced. Safety concerns will prevent us from increasing the human anti-CD3 dose, since temporary EBV reactivation was seen in most individuals in the recent European anti-CD3 trial, and other options will need to be explored. One promising avenue is the β cell antigen–specific induction of Tregs.
In the 1990s, several groups including ours reported that immunization with islet autoantigens by various means and routes can induce islet antigen–specific Tregs and prevent T1D (10–16). Those autoreactive Tregs can act as bystander suppressors and suppress site-specifically heterologous autoreactive immune responses (16). For example, transferred insulin B-chain–induced (insB-induced) Tregs selectively proliferated in the pancreatic draining LNs (PLNs), where their cognate antigen is being presented by APCs during development of diabetes. There, they were capable of dampening autoaggressive CD8 responses (16). This suppressive effect was associated with IL-4 and IL-10 production by the Tregs. Thus, antigen-specific induction of Tregs can result in long-lasting tolerance to β cell antigens mediated by local immune modulation in the PLNs, which makes this intervention safe, with low potential for side effects. However, from many tests in animal models, we know that the efficacy is limited, because prevention of T1D is only seen when the immunization is given during the prediabetic phase. Therefore, antigen-specific interventions will need “help” to be used successfully in humans, especially in recent-onset diabetics (17).
We hypothesized that anti-CD3 would create a systemic immunomodulatory milieu to facilitate the islet antigen–specific induction of Tregs. As described previously, anti-CD3 treatment induces a shift in the cytokine profile (mainly from Th1 toward Th2) as well as an expansion of T cells with regulatory properties in mice (7, 18) and in humans (6, 19). Thus, one could envision that upon immunization with islet autoantigen, a combination therapy with anti-CD3 will expand islet-specific Tregs more forcefully. In addition, depletion of autoaggressive T cells following anti-CD3 administration would allow us to create a suitable window in recent-onset diabetes that would give newly activated Tregs enough time to proliferate and traffic to the PLNs to suppress further generation of autoaggressive cells.
To test this idea, we administered islet antigens and peptides through various routes in conjunction with anti-CD3. Here we report that a peptide derived from the human proinsulin II exhibited the best synergy and strongly enhanced Treg induction. Efficacy of this combination treatment was found in 2 animal models, and mechanistic analyses are presented herein.
Results
Enhanced efficacy in curing recent-onset T1D by combining i.n. proinsulin peptide immunization with anti-CD3 in NOD and RIP-LCMV mice.
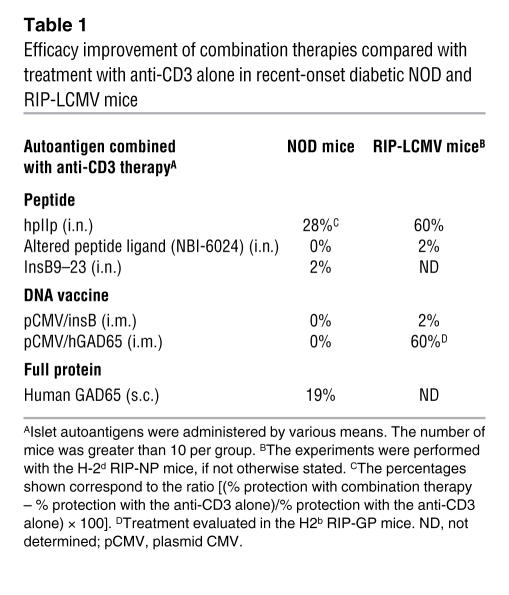
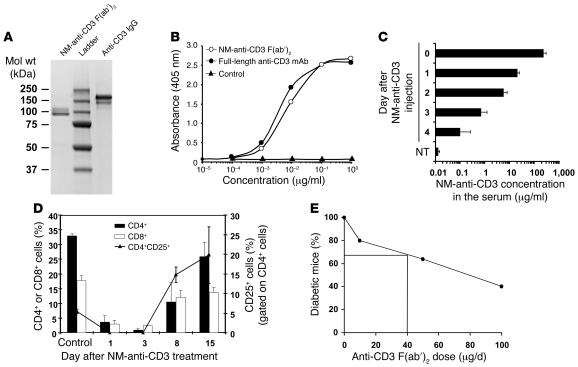
In past studies in various animal models, immunization with islet antigens resulting in the induction of Tregs has been effective in preventing T1D without systemic immunosuppression but incapable of reverting recent-onset diabetes (20). Since it had been described that treatment with anti-CD3 Ab can promote expansion of CD25+ Tregs in NOD mice (7), we investigated whether codelivery of various islet antigens could enhance reversion of hyperglycemia in recent-onset T1D (Table 1). We first evaluated the purity and activity of our anti-CD3 F(ab′)2. As shown in Figure 1, A–C, the Ab was functional, with a half-life of 2 days in vivo. Although a rapid and short-term lymphodepletion was observed after anti-CD3 treatment, the proportion of CD25+ cells strikingly increased, as compared with the untreated control mice, to reach systemically 20% of the CD4+ T cells 2 weeks after CD3 therapy (Figure 1D). In order to create a suitable window for therapeutic improvement with the combination therapy, we determined an anti-CD3 dosage leading to partial reversion of recent-onset T1D in NOD and rat insulin promoter–lymphocytic CMV (RIP-LCMV) models (Figures 1E and 2A).
Table 1 .
Efficacy improvement of combination therapies compared with treatment with anti-CD3 alone in recent-onset diabetic NOD and RIP-LCMV mice
Figure 1. Purity and functionality of the anti-CD3 F(ab′)2 .
(A) The purity of anti-CD3 was assessed by staining with Coomassie blue brilliant. (B) ELISA experiment to compare the binding capacities of the purified nonmitogenic (NM) F(ab′)2 and full-length anti-CD3. (C) The half-life of the CD3 was evaluated in vivo. After i.v. injection of 200 μg into mice (n = 6), 50 μl blood was taken daily and the presence of anti-CD3 F(ab′)2 in the serum assessed by ELISA. NT, nontreated. (D) In vivo activity of the NM anti-CD3 F(ab′)2 was evaluated in RIP-LCMV mice (n = 6). Blood samples were analyzed days 1, 3, 8, and 15 after treatment with anti-CD3 alone and their contents in CD4+, CD8+, and CD25+ T cells compared with those of untreated and uninfected RIP-LCMV mice (control). (E) The efficacy of our commercial anti-CD3 F(ab′)2 was controlled by treating NOD mice after new-onset diabetes with 3 Ab doses (10, 50, and 100 μg/d, 5 consecutive days). The percentage of mice showing long-term remission was calculated and is shown in the figure.
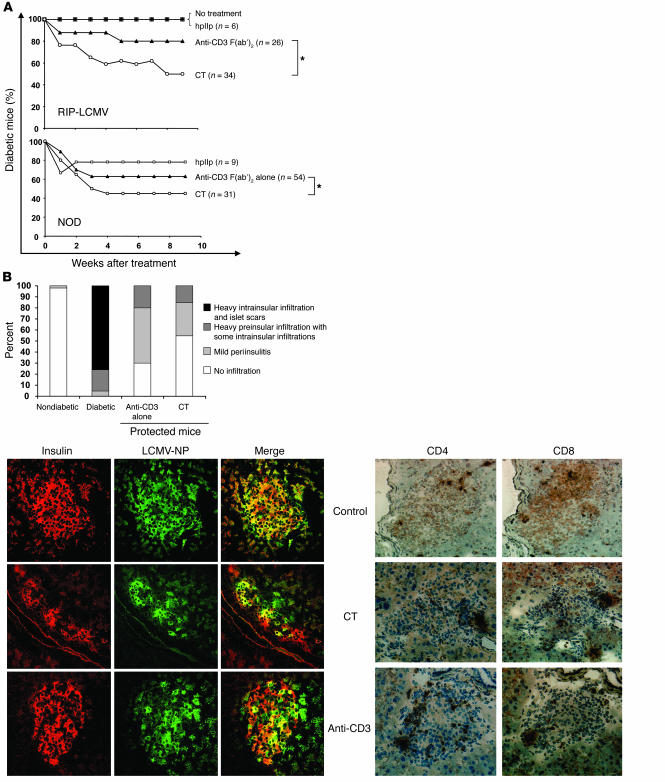
Figure 2. Synergy between non–Fc-binding anti-CD3 and hpIIp in treating NOD and RIP-LCMV mice after overt diabetes.
Mice were treated with either the anti-CD3 or peptide alone [suboptimal dose of anti-CD3 F(ab′)2 i.v. or hpIIp i.n., both 40 μg/injection] or a combination of both (combination therapy [CT]). (A) In the H-2d RIP-LCMV model (upper panel), the efficacy of the combination treatment reached 50% (n = 34) compared with 20% with anti-CD3 alone (n = 26) or 0% with hpIIp alone (n = 6). In the NOD model (lower panel), the efficacy reached 55% with the combination treatment (n = 31), compared with 37% with anti-CD3 alone (n = 54) or 22% with the hpIIp alone (n = 9). At week 9 after treatment, the statistical significance was evaluated between the anti-CD3 alone and the combination therapy groups (*P < 0.05). (B) Pancreatic islets were scored for the presence of mononuclear infiltration (upper left panel). The average percentage shown was determined from at least 8 mice per group. Shown are histological stainings of pancreata from RIP-LCMV-NP mice (lower panels). At week 5 after treatment with anti-CD3 alone or in conjunction with the proinsulin peptide (CT), pancreata from protected animals were harvested. Six-micrometer tissue sections were cut and collected for immunochemistry. Sections were costained for insulin and NP expression (lower left panel). Sections were probed for cellular infiltration by CD4+ and CD8+ T cells (lower right panel). Representative sections are shown in each panel. Original magnification, ×20.
We treated recent-onset T1D in 2 animal models (NOD and H-2d RIP-LCMV-nucleoprotein [RIP-LCMV-NP] mice), combining anti-CD3 with various islet antigens given by various means. Intranasal administration of human proinsulin II B24–C36 peptide (hpIIp) exhibited best synergy (Table 1). Thus, we focused on this antigenic modality and delivery throughout our investigation here. This peptide contains a mutation of Val to Ala in position C34 disabling a cytotoxic T cell epitope as described previously (12). After injecting anti-CD3 alone i.v. (40 μg/d for 5 consecutive days), we observed partial protection, ranging from 20% in the RIP-LCMV mice to 37% in the NOD model (Figure 2A). After recent onset, hpIIp alone showed low efficiency with a maximum of 22% protection in NOD mice. In contrast, when administered in combination, the efficacy strikingly increased. Long-term reversion of diabetes for at least 9 weeks was seen in both models (from 50% to 55% remission in RIP-LCMV and NOD mice respectively; Figure 2A). As expected, for the RIP-LCMV model, several islets expressing high insulin levels were found in the pancreas of noninfected (control) as well as cured mice (Figure 2B, lower panel). Last, we analyzed the degree of cellular infiltration in the islets of Langerhans of protected RIP-LCMV mice 5 weeks after treatment. Mice treated with anti-CD3 showed a mild periinsulitis, mainly CD4+ but also CD8+ (Figure 2B, upper panel) around 30–50% of their islets, similar to previous observations in the NOD model or after oral insulin administration (10, 21). It is noteworthy that comparing combination therapy versus anti-CD3 monotherapy, the overall degree of periinsulitis is not much further reduced in protected animals, but the number of protected animals is increased (Figure 2A).
Induction of Tregs and proinsulin-specific T cells expressing regulatory cytokines following combination therapy.
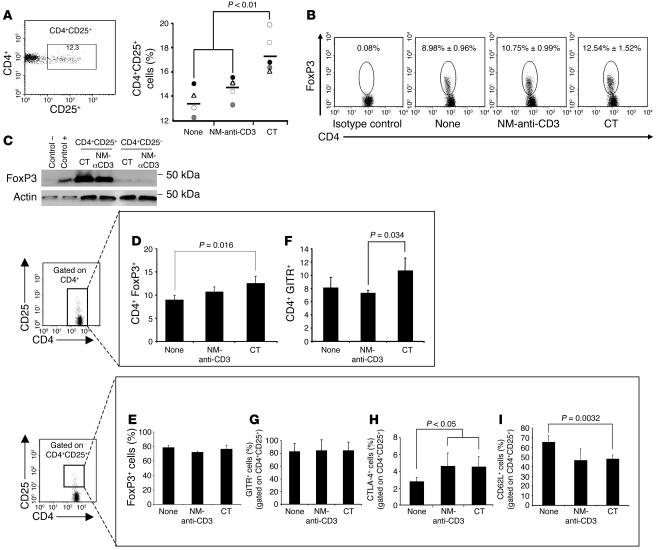
We investigated whether the combination treatment had promoted hpIIp-specific or other Tregs. We used cells pooled from spleens and PLNs of RIP-LCMV mice 5–6 weeks after treatment. First, we defined the percentage of CD4+ lymphocytes expressing 2 major Treg markers: CD25 and the transcription-repressor protein Foxp3. For this purpose, the CD4+ populations were gated on the CD25+ or Foxp3+ subpopulations as compared with the isotype control. The level of CD4+CD25+ lymphocytes significantly increased after combination therapy compared with nontreated control or anti-CD3–treated mice (Figure 3A). This expansion also correlated with a higher number of CD4+Foxp3+ cells (Figure 3, B and D). Moreover, in all groups, most of the CD4+CD25+ cells (~75%) were found to coexpress high levels of Foxp3, while the CD4+CD25– cells did not (Figure 3, C and E). Thus, in this regard, the CD4+CD25+ population obtained in our study could be compared with the Foxp3-expressing CD4+CD25high T population described in humans (22). The glucocorticoid-induced TNF receptor (GITR) is an activation marker that also appeared to characterize the suppressor phenotype of CD4+CD25+ Tregs in vivo (23, 24). The CD4+GITR+ population expanded only somewhat after combination therapy to reach 10.7% of the CD4+ cells compared with 7.3% after anti-CD3 alone (P = 0.034; Figure 3F). As previously observed with Foxp3, with or without treatment, the vast majority of the CD4+CD25+ T cells also expressed the GITR marker (Figure 3G). Since T1D is modulated by triggering CTL antigen–4 (CTLA-4) (25) and anti-CD3 therapy increased the CD4+CD25+CTLA-4+ population in the NOD mice (26), we analyzed the CD4+CD25+CTLA-4+ compartment. After both therapies, the level of CTLA-4–expressing CD4+CD25+ cells significantly increased compared with untreated controls (P < 0.05; Figure 3H). Conversely, the proportion of CD4+CD25+CD62L+-expressing cells decreased after both treatments, especially after combination therapy (P = 0.0032; Figure 3I).
Figure 3. Treatment with a combination of anti-CD3 and hpIIp increases the number of CD4+ T cells with a regulatory phenotype.
The data are from euglycemic animals treated with anti-CD3 (n = 5 experiments with 3–5 mice per experiment) or with the combination therapy (n = 5 experiments with 3–5 mice per experiment). As control, nontreated animals were used (n = 4 experiments with 4–6 mice per experiment). (A) The percentage of CD4+CD25+ cells is shown. (B) After intracellular staining, the percentage of CD4+Foxp3+ cells was evaluated. For each group, the mean ± SD is given, with P = 0.016 for the combination treatment group and P = 0.089 for the NM anti-CD3–treated group as compared with the untreated control group (None). (C) CD4+CD25+ cells expressed high levels of Foxp3. For each sample, cells were lysed in loading buffer containing SDS and β-mercaptoethanol and used in the Western blotting experiment. 5 × 105 purified CD4+CD25+ and CD4+CD25– cells were obtained from mice protected by treatment with anti-CD3 (α-CD3) alone or in combination with the hpIIp. As positive and negative controls (control+ and control–, respectively), 105 HeLa cells stably expressing or not, respectively, the mouse Foxp3 protein were loaded. Actin was used to evaluate the amount of loaded proteins. (D–I) Long-term protected RIP-LCMV mice were sacrificed and the percentage of Treg markers in pooled splenocytes and PLNs cells determined. The percentages of GITR+ and Foxp3+ cells was measured in the CD4+ population (D and E). The percentage of GITR+, Foxp3+, CTLA-4+, and CD62L+ cells were measured in the CD4+CD25+ population (F–I).
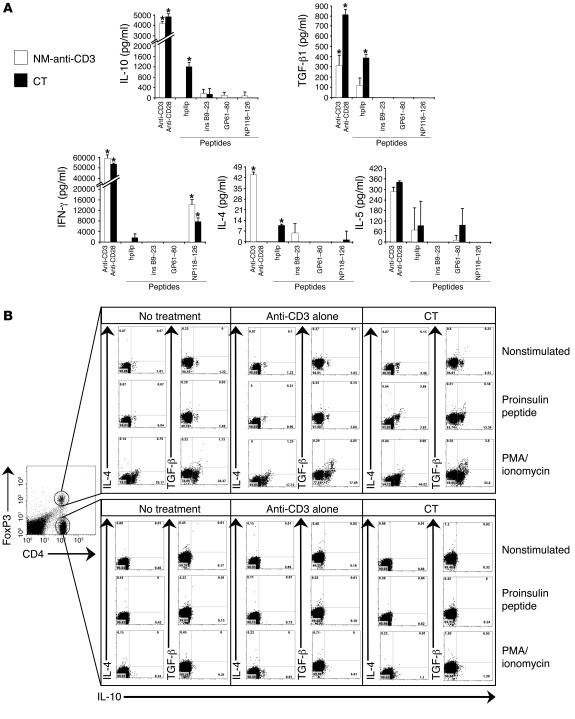
We further analyzed the capacity of hpIIp-specific T cells to produce regulatory cytokines or IFN-γ after hpIIp-specific in vitro stimulation. Splenocytes and PLNs cells of treated animals were stimulated with the hpIIp or nonspecifically with a CD3/CD28 Ab mixture. First, we analyzed the cytokine content in culture supernatants. Interestingly, the hpIIp-induced T cells mainly produced “regulatory” cytokines, with a significant increase, as compared with the background levels, in IL-10 (1,204 ± 254 pg/ml) and TGF-β (393 ± 39.5 pg/ml) in the combination therapy group following hpIIp stimulation (P < 0.05; Figure 4A), while the control peptides (insB9–23, GP61–90, or NP118–126) did not. We also observed a significant but lower increase in IL-4 secretion (10.1 ± 0.45 pg/ml). In contrast, IFN-γ production remained at the background level when stimulated under the same conditions but significantly increased when the LCMV-specific NP118–126 control peptide was used for stimulation in both nonmitogenic–anti-CD3 and combination therapy groups (Figure 4A). Additionally, we used intracellular cytokine staining after gating on CD4+Foxp3+ cells. The number of IL-10– and TGF-β–producing CD4+Foxp3+ cells was augmented selectively in this subset when stimulated with hpIIp (Figure 4B). After hpIIp stimulation, the percentage of IL-10–producing hpIIp-specific Tregs ranged, on average, from 6% to 10% in the CD4+Foxp3+ population as compared with the anti-CD3 and nontreated groups (Figure 4B, upper panel). It is worth noting that 50% of the hpIIp-specific CD4+Foxp3+ Tregs produced both IL-10 and IL-4 cytokines.
Figure 4. hpIIp–specific T cells from mice treated with anti-CD3 and i.
. proinsulin peptide exhibit a regulatory cytokine profile after in vitro stimulation. (A) Splenocytes and PLNs from animals treated and cured by the anti-CD3 alone or in combination with the hpIIp were used in vitro in a cytokine secretion assay. Cells were stimulated with a mixture of anti-CD3 and anti-CD28 Abs, various peptides (hpIIp, insB9–23, and LCMV-specific GP61–80 and NP118–126) or remained nonstimulated. After 72 hours, the supernatants were analyzed by ELISA as well as using the Luminex 100 LabMAP System. The data represent the levels of cytokine above the background observed without stimulation (NM-anti-CD3 [IL-4: 17 pg/ml, IL-5: 430 pg/ml, IL-10: 10 pg/ml, TGF-β1: 530 pg/ml, and IFN-γ: 2,500 pg/ml] or combination therapy [IL-4: 41.5 pg/ml, IL-5: 380 pg/ml, IL-10: 200 pg/ml, TGF-β1: 580 pg/ml, and IFN-γ: 3,000 pg/ml]). Data for an average of 4 mice per group are shown. *P < 0.05 compared with the nonstimulated control. (B) To confirm the cytokine profile found in the supernatants, intracellular cytokine stainings were performed. The cells were stimulated specifically with the hpIIp or unspecifically with a mixture PMA/ionomycin or remained unstimulated (nonstimulated) for 6 hours in the presence of an inhibitor of intracellular protein transport (monensin). The cells were recovered and stained at the surface for CD4 and intracellularly for Foxp3 and the cytokines TGF-β, IL-10, and IL-4. The cytokine expression was analyzed in the CD4+Foxp3+ (upper panel) and CD4+Foxp3neg (lower panel) populations.
A similar increase in the cytokine profiles was not observed with the controls: CD4+Foxp3neg cells (Figure 4B, lower panel) or 2 irrelevant peptides, NP118–126 and GP61–80 (data not shown).
Thus, combination therapy increases the level of CD4+CD25+Foxp3+ Tregs and also strongly enhances their proinsulin-specific IL-10, IL-4, and TGF-β production.
Suppression of autoaggressive CD8 responses in RIP-LCMV and NOD mice treated with combination therapy.
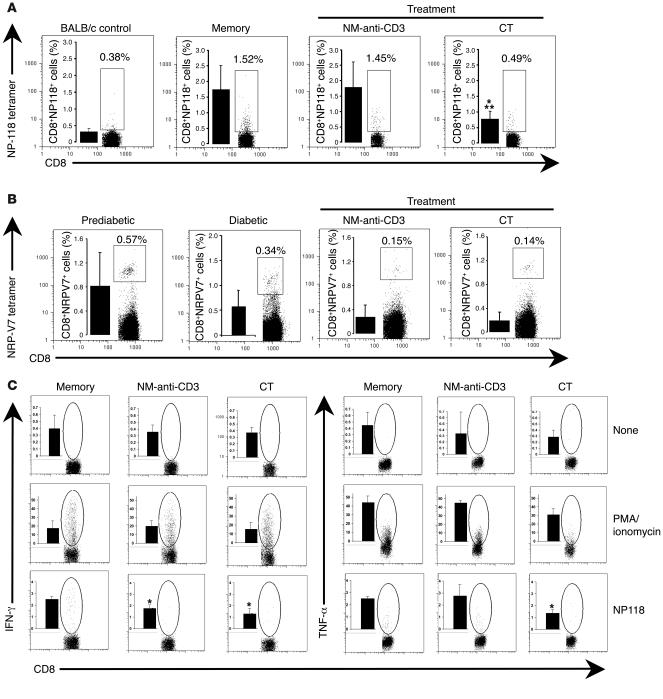
Our group previously showed that insulin-induced Treg cells are capable of modulating diabetes by bystander suppressive mechanisms (16, 27). To examine whether our combination approach induced Tregs with such suppressive capacities, we analyzed the effect on CD8 autoaggressive T cells. As depicted in Figure 5, A and B, the percentage of antigen-specific autoaggressive memory CD8+ cells was strongly reduced after combination therapy in both NOD (0.27% ± 0.19%) and RIP-LCMV (0.79% ± 0.24%) models using the NRP-V7 and NP118 tetramers, respectively. Interestingly, in the NOD model, CD8+NRP-V7+ cells were already reduced after anti-CD3 alone. In the more stringent RIP-LCMV model, where much larger numbers of autoaggressive CD8+ T cells are triggered by the virus, CD8+NP118+ T cells were only reduced after combination therapy. This also correlated well with their decreased capacity to secrete Th1 cytokines after in vitro stimulation (Figure 5C). Furthermore, the percentage of CD8+NP118+ T cells expressing IFN-γ (1.29% ± 0.46%) and TNF-± (1.38% ± 0.28%) significantly decreased compared with nontreated LCMV-immune control mice (P = 0.016; Figure 5C).
Figure 5. Reduced autoaggressive CD8+ T cell responses after combination treatment.
(A) The percentage of NP118 tetramer–positive CD8+ T cells in nondiabetic LCMV-infected RIP-NP mice (5 weeks after infection) or after treatment (anti-CD3 alone or combination therapy). Numbers above the gated cells correspond to the percentage of tetramer-positive CD8+ T cells found in the individual mice represented in the figure. Histograms, shown as insets, represent the average of n = 6–9 mice per group. As control, BALB/c mice were used. *P = 0.0036 compared with mice that have been infected but are in the memory phase of viral clearance (memory mice) and **P = 0.0057 compared with mice treated with NM-anti-CD3 alone. (B) The percentage of NRP-V7 tetramer–positive CD8+ T cells is shown for prediabetic NOD mice (10-week-old mice), for diabetic NOD mice, and for cured NOD mice after treatment (anti-CD3 alone or combination therapy). Numbers in the upper-right corner correspond to the percentage of tetramer-positive CD8+ T cells found in the individual mice shown in the figure. Histograms, shown as insets, represent the average of n = 5 mice per group. (C) The percentage of IFN-γ– and TNF-α–expressing CD8+ T cells was measured by intracellular staining in nondiabetic LCMV-infected RIP-NP mice, either nontreated (memory) or treated (anti-CD3 or combination therapy). Rows correspond to 3 different in vitro stimulations. Splenocytes and PLN cells were pooled and stimulated with either PMA/ionomycin or NP118 peptide or remained unstimulated (None). Histograms, shown as insets, correspond to the mean ± SD of IFN-γ– or TNF-α–positive CD8+ T cells (n = 3–5 mice per group). *P < 0.05 compared with the LCMV memory control.
Antigen-induced Tregs following combination therapy can transfer protection from diabetes in vivo.
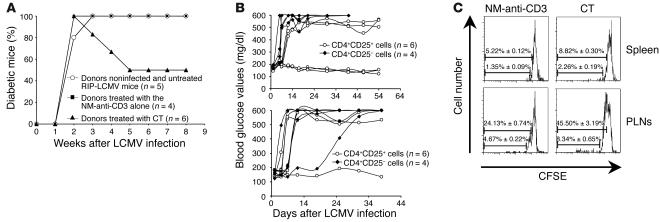
To address the question of whether the antigen-induced Tregs were capable of transferring active, dominant tolerance, we performed adoptive transfer studies. We used immunocompetent RIP-LCMV-NP recipients. Three-day antigenic stimulation of splenocytes derived from protected mice was performed to expand the hpIIp-specific Tregs prior to adoptive transfers. This expansion was required, since direct ex vivo transfers did not result in protection from diabetes (data not shown and ref. 16). We observed 50% protection in recipients receiving cells from mice protected by the combination therapy (Figure 6A). Importantly, the cells reverted recent-onset diabetes as efficaciously as the combination therapy did in the donors. As previously reported by our group with immunocompetent RIP-LCMV mice, no protection was seen with CD4+ cells from mice protected with anti-CD3 alone (18). Next, we tested whether our antigen-induced Tregs were contained within the CD4+CD25+ compartment. Transfer of 106 CD4+CD25+ cells purified from the same source was sufficient to reduce diabetes development by 50% (Figure 6B, upper panel).
Figure 6. CD4+ CD25+ T lymphocytes generated by combination therapy exert dominant tolerance and block autoimmune diabetes after adoptive transfer.
(A) Adoptive transfer of 5 × 106 CD4+ T cells from nondiabetic donors, either nontreated RIP-LCMV mice (control, n = 5 mice) or mice treated with the anti-CD3 alone (n = 4 mice) or in combination with the proinsulin peptide (n = 6 mice). A 3-day antigenic stimulation of splenocytes derived from protected mice was performed for each group (treated as well as control) to expand the proinsulin-specific Treg population prior to adoptive transfers. The putative Tregs were transferred into nonimmunodeficient RIP-LCMV-NP recipient mice day 5 after LCMV infection. (B) CD4+CD25+ and CD4+CD25– T cells were purified from treated RIP-LCMV mice protected by the anti-CD3 alone (lower panel) or in combination with the proinsulin peptide (upper quadrant). Those cells (106) were transferred into nonimmunodeficient RIP-LCMV-NP recipient mice 5 days after LCMV infection (n = 6 mice per group). (C) Proliferation of CD4+CD25+ lymphocytes in the spleens and PLNs of RIP-LCMV recipient mice. CD4+CD25+ T lymphocytes were purified from treated RIP-LCMV mice protected by the anti-CD3 alone (left panels) or in combination with the hpIIp (right panels). These cells were CFSE labeled and transferred into wild-type RIP-LCMV recipient mice day 5 after infection. Spleens and PLNs were removed from recipients 2 days after transfer and stained with a CD4-specific antibody. The data are representative of 2 independent experiments. Numbers correspond to the mean ± SD of CFSE-diluted CD4+CD25+ lymphocytes (n = 2 mice per group).
Furthermore, the severity of the disease was reduced in the nonprotected recipient mice after transfer with Tregs from mice cured by the combination therapy. Indeed, the recipient mice transferred with CD4+CD25– T cells rapidly died, with blood glucose values above 600 mg/dl, while the blood glucose values of the 3 nonprotected mice transferred with CD4+CD25+ Tregs (Figure 6B, upper panel) were stabilized around 500 mg/dl for more than 50 days. At 54 days after transfer, apart from the higher blood glucose values, those diabetic mice appeared clinically as healthy as the nondiabetic control mice. In contrast, only 1 recipient mouse transferred with CD4+CD25+ cells from anti-CD3–cured mice was stabilized at 500 mg/dl. Thus, the severity of the disease was reduced for 6 of the 6 recipient mice (100%) transferred with Tregs from donors cured with the combination therapy, as compared with 2 of 6 mice (33.3%) with Tregs from donors cured with anti-CD3 alone.
Last, we used CFSE labeling to track the CD4+CD25+ cells after transfer. Although, a similar proportion of the transferred cells was found in the spleens and PLNs of the hosts, only the CD4+CD25+ cells in the PLNs started to proliferate (Figure 6C). Two days after transfer, 24.13% ± 0.74% of the cells from CD3-treated mice divided in the PLNs of recipients, while, under similar conditions, 2-fold more (45.50% ± 3.19%) cells from mice protected with the combination therapy underwent their first division in the PLNs (Figure 6C, lower panels). As we previously reported (16), a majority of the cells completed only 1 round of division. This proliferation profile might be explained by the fact that we transferred into immunocompetent nonirradiated syngeneic recipients, which have a lower capacity than NOD-SCID mice to expand adoptively transferred CD4+ cells (28, 29).
Thus, CD25+ Tregs induced by combination therapy with hpIIp peptide and anti-CD3 but not anti-CD3 alone are capable of mediating active, dominant tolerance in syngeneic recipients.
Discussion
We found that efficacy of antigen-specific therapy to induce Tregs and long-term tolerance can be greatly enhanced when combined with anti-CD3 in recent-onset diabetes. Whereas antigen administration alone had no efficacy in late-stage disease, in particular following onset of hyperglycemia, the coadministration of non–Fc-binding anti-CD3 doubled the reversion of diabetes compared with anti-CD3 alone. This protection, observed in 2 laboratories, was long lasting and was seen in 2 different diabetes models. We believe that our observation is highly relevant for shaping future clinical strategies in T1D prevention and intervention in several aspects.
First, although anti-CD3 has shown great promise in 2 human recent-onset diabetes trials by delaying decline of C-peptide over an 18-month period, there is still need for improvement, especially in extending duration of the beneficial effect and also efficacy. Increasing the anti-CD3 dose is not a good option, because side effects such as cytokine release and EBV activation would likely be increased (8). Although the drug might be given more frequently, a more ideal scenario would be induction of antigen-specific tolerance without repeated or longer-lasting systemic immune modulation.
Second, induction of Tregs with insulin or other islet antigens with the goal of establishing long-term tolerance has shown great promise in animal models, but has, so far, had little efficacy in human trials such as the Diabetes Prevention Trial — Type 1, where only a subfraction of treated patients showed a beneficial effect (30). In addition, antigen-specific therapies were only effective during the prediabetic phase in animal models, but it would be highly desirable to apply them later on, after overt hyperglycemia, which is more practical and would provide benefit for patients with manifested hyperglycemia. The attractive aspect of generating islet antigen–specific Tregs by immunization is that such cells can act as bystander suppressors, circumventing the need to identify all autoantigenic targets, and operate locally in the PLNs and islets, where they recognize their cognate antigens, without systemically affecting the immune system and compromising host defense.
Based on these considerations, the promise for combination therapy presented in this report is highly relevant, since it would circumvent the need to increase anti-CD3 dose or frequency of administration and shows operational induction of Tregs late during disease, which to our knowledge had never been achieved before. Our current data point toward i.n. hpIIp as one of the best antigenic modalities (Table 1).
How can the synergy after combination therapy be explained mechanistically? An obvious interpretation of our data is that anti-CD3 will create a temporal window that allows proinsulin-induced Tregs to develop.
This is achieved because anti-CD3 directly decreases numbers of autoaggressive T cells in mice, as described previously (18, 31). This lymphodepleting effect is short in duration and correlates well with the half-life of the drug in serum, as shown by us in mice and the recent human trials (8, 9, 31). The resulting transient release of “pressure” on the remaining β cells might be essential to allow Tregs to still become operational during advanced stages of diabetogenesis, where only a small number of islets are left. Based on unpublished data from our laboratory, it is less likely that Tregs can directly affect already activated effector CD4 and CD8 lymphocytes, because coculture of activated effector CTLs with CD25+ or insB Tregs did not affect their ability to lyse targets or secrete IFN-γ (M. von Herrath and colleagues, unpublished observations). Therefore, a more likely mechanism is the modulation of APCs in PLNs that will render them tolerogenic and prevent further generation of effector lymphocytes, thus disrupting the cycle that eventually leads to complete loss of all β cells. Indeed, data from several groups support this concept (32, 33), and, if true, this means that Tregs will be unable to suppress already-activated autoaggressive T cells within the islets and PLNs. This task would be managed by the anti-CD3 in the combination regimen, and without anti-CD3, induction of Tregs will have no impact on disease in late stages, where too many armed effector cells are already within the islets.
In addition, anti-CD3 has been shown in some settings (7, 34) but not all (18) to directly promote the generation of Tregs. This property is less well understood, and it is still unclear whether this is a direct effect on T cells during their activation. In NOD studies by Chatenoud and others, anti-CD3 increased the number of CD4+CD25+ cells as well as systemic TGF-β production (35), which was required for therapeutic efficacy. In humans, in contrast, increased IL-10 generation was observed, and CD8 cells were increased after therapy (6, 9). In the RIP-LCMV model, anti-CD3 induced systemic cytokine shifts to Th2, but not a CD4+CD25+ population that could transfer protection (18). In conjunction with our present findings, where proinsulin-induced CD25+Foxp3+ Tregs were augmented, produced regulatory cytokines, and could transfer protection to recent-onset diabetic recipients, anti-CD3 might induce a systemic cytokine release that favors overall and insulin-specific Treg induction. In addition, antigenic responses that are primed while anti-CD3 is present might become more likely regulatory or IL-10, TGF-β, and/or IL-4 producers. Reversion of hyperglycemia is achieved, because the combination therapy induces larger numbers of islet-specific Tregs, whereas anti-CD3 or proinsulin alone would prime insufficient amounts of Tregs.
There are some intriguing differences between the NOD and RIP-LCMV models concerning Treg induction and function in our studies. First, in previous studies, anti-CD3 alone induced increased numbers of CD25+CD62L+ Tregs in the NOD mice that can transfer protection to NOD/SCID recipients (36), whereas no such Tregs were found in the RIP model. We have to keep in mind that our mechanistic analyses were done 5–6 weeks after treatment in order to study animals with long-lasting disease remission. We thus would argue that a majority of the induced Tregs already contracted and entered into the memory phase with lower CD62L expression, explaining why, before adoptive transfer, antigen-induced Tregs had to be activated and expanded by in vitro stimulation to be fully functional (ref. 16 and present data). Similarly, expression of CD62L was also reduced on the CD4+CD25+ T cells in a majority of patients treated with the hOKT3γ1(Ala-Ala) Ab (6).
Second, in the NOD model in the present investigation, suppression of autoaggressive CD8 responses following anti-CD3 was more efficient. In RIP mice, such suppression was seen only immediately following anti-CD3 administration (18), but not long term, as evidenced in this report (Figure 5). The reason for this divergence is likely differences in immune regulation between the 2 mouse models, since it is known that NOD but not RIP mice exhibit multiple abnormalities in immune function (37). Furthermore, CD8 responses initiated by the virus are much higher in frequency compared with NRP-V7 cells found in the NOD mice, which might account for the fact that their long-term suppression was only observed after combination therapy but not treatment with anti-CD3 alone. The fact that the combination treatment was able to reverse established diabetes in the RIP-LCMV model at all is by itself encouraging (Figure 6A), since it points toward rather strong efficacy that would hopefully also apply to the human disease. Furthermore, humans do not exhibit all of the immune defects seen in the NOD model, and therefore the data from the RIP-LCMV model provide increased confidence in the general applicability of our novel combination approach.
In summary, based on our current investigation, one can expect several advantages from combining antigen-specific induction of Tregs with a suitable systemically acting drug such as anti-CD3 for the treatment of recent-onset diabetes and maybe other autoimmune disorders. Efficacy is enhanced, the risk for side effects is reduced, and the need for further increasing the systemic drug is obviated. This will allow for safely establishing antigen-specific therapy that should be a central component when establishing long-term tolerance, because Tregs can exert bystander suppression and act site-specifically, wherever their cognate autoantigen is expressed.
Methods
Mice and virus.
Generation of H-2d RIP-LCMV-NP transgenic mice has been previously described (38). Mice were genotyped by PCR as previously described (38). NOD/LtJ mice were purchased from the Jackson Laboratory. We used LCMV strain Armstrong (Arm) to trigger diabetes in the RIP-LCMV-NP model. Seven- to 10-week-old RIP-LCMV-NP mice were infected with a single i.p. dose of 103 PFU of LCMV-Arm. In this diabetes model, the LCMV NP is transgenically expressed under control of the rat insulin promoter. The H-2d RIP-LCMV-NP strain also shows thymic expression of the NP antigen, and diabetes development depends on both CD4 and CD8 T cells. Although the autoaggressive response and process in the islets is initiated exclusively following immunization with LCMV, autoantibodies to other islet antigens such as insulin and glutamic acid decarboxylase arise prior to onset of T1D and evidence antigenic spreading. The RIP model has been utilized by many investigators in situations where the autoaggressive response needs to be tracked precisely and resembles, in many aspects, human autoimmune diabetes development as far as we understand it. This study was approved by the La Jolla Institute for Allergy and Immunology Animal Care Committee.
Blood glucose monitoring.
Blood glucose was monitored with the blood glucose monitoring system OneTouch Ultra (LifeScan Inc.). Diabetes was defined as 2 consecutive blood glucose values superior to 250 mg/dl in both animal models.
Treatments.
After recent-onset diabetes, mice were treated 5 consecutive days i.v. (days 0–4, 40 μg/d) with the non–Fc-binding anti-CD3ε F(ab′)2 (anti-CD3) obtained from Bio Express. This treatment was given alone or in combination with hpIIp without CTL epitope (amino acid sequence: AAAFFYTPKTRREAEDA [amino acid residues corresponding to the hpIIp are underlined]; obtained from Auspep). The hpIIp diluted in PBS at 4 mg/ml was administered i.n. on days 0, 2, 7, and 12 after recent onset (40 μg/d). As control, a group of mice was treated with the peptide alone using the same regimen.
Immunohistochemistry.
To detect insulin, NP, CD4, and CD8 expression in pancreatic β cells, primary Abs (guinea pig anti-swine insulin from Dako [dilution 1:300], anti-CD4 RM4.5 and anti-CD8a IHC from BD Biosciences [dilution 1:50]), and rabbit polyclonal anti-LCMV (dilution 1:1,000) from Michael Bruns (Heinrich-Pette-Institute for Experimental Virology and Immunology, University of Hamburg, Hamburg, Germany) were applied to frozen tissue sections as previously described (39).
Abs and tetramers used for in vitro experiments.
mAbs specific for CD3 (clone 145-2C11), CD4, CD8, CD25, CD28, CTLA-4, CD62L, IL-10, IL-4, IL-5, IFN-γ, and all the control isotypes were purchased from BD Biosciences. Purified anti–TGF-β1 (detected with an APC-labeled anti-mouse Ab) and anti-GITR/TNFRSF18-FITC Abs were obtained, respectively, from IQ Products and R&D Systems. Rabbit polyclonal anti-mouse Foxp3 as well as mouse Foxp3 cDNA were kindly provided by Alexander Rudensky (University of Washington, Seattle, Washington, USA). The NP118-H-2Kd tetramers were generated in our laboratory, while the NRP-V7-H-2Kd tetramers (40) were generously provided by Pere Santamaria and Rusung Tan (University of Calgary, Calgary, Alberta, Canada, and University of British Columbia, Vancouver, British Columbia, Canada).
Flow cytometry.
Single-cell suspensions were prepared from the spleens and PLNs of protected animals or untreated mice as controls. A fraction of the cells were stained for 1 hour at 4°C (dilution 1:20) with either the NRP-V7-H-2Kd or NP118-H-2Kd tetramers (for the NOD and the RIP-LCMV-NP mice, respectively). The rest of the cells were cultured and stimulated in vitro with 10 μg/ml of hpIIp for 10 hours or a mixture of PMA (25 ng/ml) and ionomycin (500 ng/ml) for 6 hours in presence of Golgi-stop (cytofix/cytoperm kit; BD) or remained unstimulated as controls. Then cells were stained with the conjugated Abs specific for cell-surface markers. After permeabilization with the cytofix/cytoperm kit, cells were incubated first with the purified anti–TGF-β Ab. After washings, the labeled Abs were added to the cells (a series of APC-conjugated cytokine-specific antibodies, the PE-labeled anti-mouse Foxp3, as well as the APC-labeled anti-mouse Ab directed against the anti–TGF-β Ab) for 30 minutes at 4°C. Next the cells were fixed with a 4% paraformaldehyde solution, acquired, and analyzed on a FACScalibur flow cytometer (BD Biosciences).
ELISA experiments
Detection of nonmitogenic anti-CD3 F(ab′)2 .
The microtiter plates were coated with recombinant purified CD3εγ protein (41) generously provided by E.L. Reinherz (Harvard Medical School, Boston, Massachusetts, USA) at 1 μg/ml in PBS overnight at 4°C. Plates were washed with 0.05% Tween-20 in PBS (PBS-T) and blocked with 2% BSA in PBS-T (blocking buffer) for 1 hour at 37°C. Then, anti-CD3 F(ab′)2 as well as full-length anti-CD3 Abs (10-fold dilution from 1 to 10–5 μg/ml in blocking buffer) were incubated for 2 hours at 37°C. To assess the in vivo half-life of anti-CD3, several blood samples (days 0–4 after injection of 200 μg anti-CD3 into RIP-LCMV-NP mice) were obtained. The sera from treated or control mice (dilution 1:100 in blocking buffer) as well as purified anti-CD3 as a standard (10-fold dilution from 10 to 10–4 μg/ml in blocking buffer) were incubated for 2 hours at 37°C. After washing, a biotinylated anti-hamster IgG (heavy + light chains) (diluted 1:1,000; Vector Laboratories) was added for 1 hour at 37°C. Then, an HRP-conjugated avidin (dilution 1:2,000; Vector Laboratories) was used for 30 minutes at 37°C. The reactivity was revealed using the ABTS (2,2’-Azino-bis-[3-ethylbenzthiazoline-6-sulfonic acid]) substrate (Sigma-Aldrich).
Cytokine measurements.
Single-cell suspensions were prepared from the spleens and PLNs of protected animals or untreated mice as controls. Cells were cultured and stimulated in vitro (a) antigen-specifically with 10 μg/ml hpIIp, insB9–23, GP61–80 (LCMV-specific CD4+ epitope) or 2 μg/ml of NP118 peptide for 72 hours or (b) nonspecifically with an anti-CD3/anti-CD28 mixture (1 μg/ml each) for 24 hours; (c) or they remained unstimulated as control for 72 hours. The supernatants were harvested, and capture ELISA experiments were used to assess IL-4, IL-5, IL-10, TGF-β1, and IFN-γ levels. Cytokine analysis was conducted as proposed by BD Biosciences — Pharmingen for IL-4, IL-5, IL-10, and IFN- γ, and the Quantikine kit (R&D Systems) was used to detect TGF-β1. The data obtained by ELISA were confirmed using a commercially available multiplexed kit (Beadlyte Mouse Multi-Cytokine Detection System; Upstate USA Inc.) and the Luminex 100 LabMAP System, with cytokine concentrations interpolated using the Softmax Pro program (Molecular Devices Corp.) against the linear range on the standard curves.
Adoptive transfers.
Single-cell suspensions were prepared from the spleens and PLNs of protected animals or untreated mice as control. Cells were cultured in complete RPMI-1640 medium supplemented with rhIL-2 (200 U/ml). In vitro stimulation was performed by adding 10 μg/ml hpIIp for 72 hours (and anti-CD3 Abs for the last 12 hours only when the bulk of CD4+ cells were transferred). After in vitro culture, the CD4+CD25+ cells were purified using the mouse CD4+CD25+ Treg isolation kit from Miltenyi Biotec. To obtain only a pure CD4+ population, the isolation protocol was stopped after the depletion step. The cells were counted, labeled with CFSE (Invitrogen Corp.) if necessary, and transferred into immunocompetent male recipient RIP-LCMV-NP mice day 5 after infection (200 μl PBS containing 5 × 106 CD4+ or 106 CD4+CD25+ or CD4+CD25– cells were injected i.v.).
Statistics.
Data are expressed as a mean ± SD. The statistical significance of the difference between means was determined using the 2-tailed Student’s t test or the log-rank test. Differences were considered significant at P < 0.05.
Acknowledgments
The authors would like to thank Mark Atkinson and Clive Wasserfall for the Luminex analyses. This work was supported by the NIH (grants DK69872 to K.C. Herold and M. von Herrath, DK51091 and AI51973 to M. von Herrath). D. Bresson was successfully recipient of a Juvenile Diabetes Research Foundation International postdoctoral fellowship (2004–2005) and a European Marie-Curie Outgoing fellowship (2005–2008).
Footnotes
Nonstandard abbreviations used: CTLA-4, CTL antigen–4; GITR, glucocorticoid-induced TNF receptor; hpIIp, human proinsulin II B24–C36 peptide; insB, insulin B-chain; NP, nucleoprotein; PLN, pancreatic draining LN; RIP-LCMV, rat insulin promoter–lymphocytic CMV; T1D, type 1 diabetes.
Conflict of interest: Jeffrey A. Bluestone has a financial interest in the mAb hOKT3g1 (Ala-Ala) consisting of a patent application and a commercial agreement with Centocor and Johnson and Johnson Pharmaceuticals.
Citation for this article: J. Clin. Invest. 116:1371–1381 (2006). doi:10.1172/JCI27191.
References
- 1.Kent S.C., et al. Expanded T cells from pancreatic lymph nodes of type 1 diabetic subjects recognize an insulin epitope. Nature. 2005;435:224–228. doi: 10.1038/nature03625. [DOI] [PubMed] [Google Scholar]
- 2.Nakayama M., et al. Prime role for an insulin epitope in the development of type 1 diabetes in NOD mice. Nature. 2005;435:220–223. doi: 10.1038/nature03523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu E., Eisenbarth G.S. Type 1A diabetes mellitus-associated autoimmunity. Endocrinol. Metab. Clin. North Am. 2002;31:391–410, vii–viii. doi: 10.1016/s0889-8529(01)00017-2. [DOI] [PubMed] [Google Scholar]
- 4.Mahon J.L., Dupre J., Stiller C.R. Lessons learned from use of cyclosporine for insulin-dependent diabetes mellitus. The case for immunotherapy for insulin-dependent diabetics having residual insulin secretion. Ann. N. Y. Acad. Sci. 1993;696:351–363. doi: 10.1111/j.1749-6632.1993.tb17171.x. [DOI] [PubMed] [Google Scholar]
- 5.Chatenoud L., Primo J., Bach J.F. CD3 antibody-induced dominant self tolerance in overtly diabetic NOD mice. J. Immunol. 1997;158:2947–2954. [PubMed] [Google Scholar]
- 6.Herold K.C., et al. Activation of human T cells by FcR nonbinding anti-CD3 mAb, hOKT3γ1(Ala-Ala). J. Clin. Invest. 2003;111:409–418. doi: 10.1172/JCI200316090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belghith M., et al. TGF-beta-dependent mechanisms mediate restoration of self-tolerance induced by antibodies to CD3 in overt autoimmune diabetes. Nat. Med. 2003;9:1202–1208. doi: 10.1038/nm924. [DOI] [PubMed] [Google Scholar]
- 8.Keymeulen B., et al. Insulin needs after CD3-antibody therapy in new-onset type 1 diabetes. . N. Engl. J. Med. 2005;352:2598–2608. doi: 10.1056/NEJMoa043980. [DOI] [PubMed] [Google Scholar]
- 9.Herold K.C., et al. A single course of anti-CD3 monoclonal antibody hOKT3{gamma}1(Ala-Ala) results in improvement in C-peptide responses and clinical parameters for at least 2 years after onset of type 1 diabetes. Diabetes. 2005;54:1763–1769. doi: 10.2337/diabetes.54.6.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Von Herrath M.G., Dyrberg T., Oldstone M.B. Oral insulin treatment suppresses virus-induced antigen-specific destruction of β cells and prevents autoimmune diabetes in transgenic mice. J. Clin. Invest. 1996;98:1324–1331. doi: 10.1172/JCI118919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alleva D.G., et al. Immunological characterization and therapeutic activity of an altered-peptide ligand, NBI-6024, based on the immunodominant type 1 diabetes autoantigen insulin B-chain (9-23) peptide. Diabetes. 2002;51:2126–2134. doi: 10.2337/diabetes.51.7.2126. [DOI] [PubMed] [Google Scholar]
- 12.Martinez N.R., et al. Disabling an integral CTL epitope allows suppression of autoimmune diabetes by intranasal proinsulin peptide. J. Clin. Invest. 2003;111:1365–1371. doi: 10.1172/JCI200317166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daniel D., Wegmann D.R. Intranasal administration of insulin peptide B:9-23 protects NOD mice from diabetes. Ann. N. Y. Acad. Sci. 1996;778:371–372. doi: 10.1111/j.1749-6632.1996.tb21146.x. [DOI] [PubMed] [Google Scholar]
- 14.Coon B., An L.L., Whitton J.L., von Herrath M.G. DNA immunization to prevent autoimmune diabetes. J. Clin. Invest. 1999;104:189–194. doi: 10.1172/JCI7209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mukherjee R., Wagar D., Stephens T.A., Lee-Chan E., Singh B. Identification of CD4+ T cell-specific epitopes of islet-specific glucose-6-phosphatase catalytic subunit-related protein: a novel beta cell autoantigen in type 1 diabetes. . J. Immunol. 2005;174:5306–5315. doi: 10.4049/jimmunol.174.9.5306. [DOI] [PubMed] [Google Scholar]
- 16.Homann D., Dyrberg T., Petersen J., Oldstone M.B., von Herrath M.G. Insulin in oral immune “tolerance”: a one-amino acid change in the B chain makes the difference. J. Immunol. 1999;163:1833–1838. [PubMed] [Google Scholar]
- 17.Harlan D.M., von Herrath M. Immune intervention with anti-CD3 in diabetes. Nat. Med. 2005;11:716–718. doi: 10.1038/nm0705-716. [DOI] [PubMed] [Google Scholar]
- 18.Von Herrath M.G., Coon B., Wolfe T., Chatenoud L. Nonmitogenic CD3 antibody reverses virally induced (rat insulin promoter-lymphocytic choriomeningitis virus) autoimmune diabetes without impeding viral clearance. J. Immunol. 2002;168:933–941. doi: 10.4049/jimmunol.168.2.933. [DOI] [PubMed] [Google Scholar]
- 19.Bisikirska B., Colgan J., Luban J., Bluestone J.A., Herold K.C. TCR stimulation with modified anti-CD3 mAb expands CD8+ T cell population and induces CD8+CD25+ Tregs. J. Clin. Invest. 2005;115:2904–2913. doi: 10.1172/JCI23961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larche M., Wraith D.C. Peptide-based therapeutic vaccines for allergic and autoimmune diseases. Nat. Med. 2005;11:S69–S76. doi: 10.1038/nm1226. [DOI] [PubMed] [Google Scholar]
- 21.Chatenoud L., Thervet E., Primo J., Bach J.F. Anti-CD3 antibody induces long-term remission of overt autoimmunity in nonobese diabetic mice. Proc. Natl. Acad. Sci. U. S. A. 1994;91:123–127. doi: 10.1073/pnas.91.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lundgren A., et al. Mucosal FOXP3-expressing CD4+ CD25high regulatory T cells in Helicobacter pylori-infected patients. Infect. Immun. 2005;73:523–531. doi: 10.1128/IAI.73.1.523-531.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McHugh R.S., et al. CD4(+)CD25(+) immunoregulatory T cells: gene expression analysis reveals a functional role for the glucocorticoid-induced TNF receptor. Immunity. 2002;16:311–323. doi: 10.1016/s1074-7613(02)00280-7. [DOI] [PubMed] [Google Scholar]
- 24.Shimizu J., Yamazaki S., Takahashi T., Ishida Y., Sakaguchi S. Stimulation of CD25(+)CD4(+) regulatory T cells through GITR breaks immunological self-tolerance. Nat. Immunol. 2002;3:135–142. doi: 10.1038/ni759. [DOI] [PubMed] [Google Scholar]
- 25.Boden E., Tang Q., Bour–Jordan H., Bluestone J.A. The role of CD28 and CTLA4 in the function and homeostasis of CD4+CD25+ regulatory T cells. Novartis Found. Symp. 2003;252:55–63; discussion 63–56, 106–114. doi: 10.1002/0470871628.ch5. [DOI] [PubMed] [Google Scholar]
- 26.Chatenoud L. CD3 antibody treatment stimulates the functional capability of regulatory T cells. Novartis Found. Symp. 2003;252:279–286; discussion 286–290. [PubMed] [Google Scholar]
- 27.Homann D., et al. Autoreactive CD4+ T cells protect from autoimmune diabetes via bystander suppression using the IL-4/Stat6 pathway. Immunity. 1999;11:463–472. doi: 10.1016/s1074-7613(00)80121-1. [DOI] [PubMed] [Google Scholar]
- 28.Ploix C., Lo D., Carson M.J. A ligand for the chemokine receptor CCR7 can influence the homeostatic proliferation of CD4 T cells and progression of autoimmunity. J. Immunol. 2001;167:6724–6730. doi: 10.4049/jimmunol.167.12.6724. [DOI] [PubMed] [Google Scholar]
- 29.Maury S., Salomon B., Klatzmann D., Cohen J.L. Division rate and phenotypic differences discriminate alloreactive and nonalloreactive T cells transferred in lethally irradiated mice. Blood. 2001;98:3156–3158. doi: 10.1182/blood.v98.10.3156. [DOI] [PubMed] [Google Scholar]
- 30.Skyler J.S., et al. Effects of oral insulin in relatives of patients with type 1 diabetes: the Diabetes Prevention Trial — Type 1. Diabetes Care. 2005;28:1068–1076. doi: 10.2337/diacare.28.5.1068. [DOI] [PubMed] [Google Scholar]
- 31.Herold K.C., et al. Anti-CD3 monoclonal antibody in new-onset type 1 diabetes mellitus. . N. Engl. J. Med. 2002;346:1692–1698. doi: 10.1056/NEJMoa012864. [DOI] [PubMed] [Google Scholar]
- 32.Nagler-Anderson C., Bhan A.K., Podolsky D.K., Terhorst C. Control freaks: immune regulatory cells. Nat. Immunol. 2004;5:119–122. doi: 10.1038/ni0204-119. [DOI] [PubMed] [Google Scholar]
- 33.Tarbell K.V., Yamazaki S., Olson K., Toy P., Steinman R.M. CD25+ CD4+ T cells, expanded with dendritic cells presenting a single autoantigenic peptide, suppress autoimmune diabetes. . J. Exp. Med. 2004;199:1467–1477. doi: 10.1084/jem.20040180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kohm A.P., et al. Treatment with nonmitogenic anti-CD3 monoclonal antibody induces CD4+ T cell unresponsiveness and functional reversal of established experimental autoimmune encephalomyelitis. J. Immunol. 2005;174:4525–4534. doi: 10.4049/jimmunol.174.8.4525. [DOI] [PubMed] [Google Scholar]
- 35.Chatenoud L. CD3-specific antibody-induced active tolerance: from bench to bedside. Nat. Rev. Immunol. 2003;3:123–132. doi: 10.1038/nri1000. [DOI] [PubMed] [Google Scholar]
- 36.Chatenoud L., Salomon B., Bluestone J.A. Suppressor T cells — they’re back and critical for regulation of autoimmunity! Immunol. Rev. 2001;182:149–163. doi: 10.1034/j.1600-065x.2001.1820112.x. [DOI] [PubMed] [Google Scholar]
- 37.Anderson M.S., Bluestone J.A. The NOD mouse: a model of immune dysregulation. Annu. Rev. Immunol. 2005;23:447–485. doi: 10.1146/annurev.immunol.23.021704.115643. [DOI] [PubMed] [Google Scholar]
- 38.Von Herrath M.G., Dockter J., Oldstone M.B. How virus induces a rapid or slow onset insulin-dependent diabetes mellitus in a transgenic model. Immunity. 1994;1:231–242. doi: 10.1016/1074-7613(94)90101-5. [DOI] [PubMed] [Google Scholar]
- 39.Christen U., et al. A viral epitope that mimics a self antigen can accelerate but not initiate autoimmune diabetes. J. Clin. Invest. 2004;114:1290–1298. doi: 10.1172/JCI200422557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lieberman S.M., et al. Identification of the beta cell antigen targeted by a prevalent population of pathogenic CD8+ T cells in autoimmune diabetes. . Proc. Natl. Acad. Sci. U. S. A. 2003;100:8384–8388. doi: 10.1073/pnas.0932778100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim K.S., Sun Z.Y., Wagner G., Reinherz E.L. Heterodimeric CD3epsilongamma extracellular domain fragments: production, purification and structural analysis. J. Mol. Biol. 2000;302:899–916. doi: 10.1006/jmbi.2000.4098. [DOI] [PubMed] [Google Scholar]