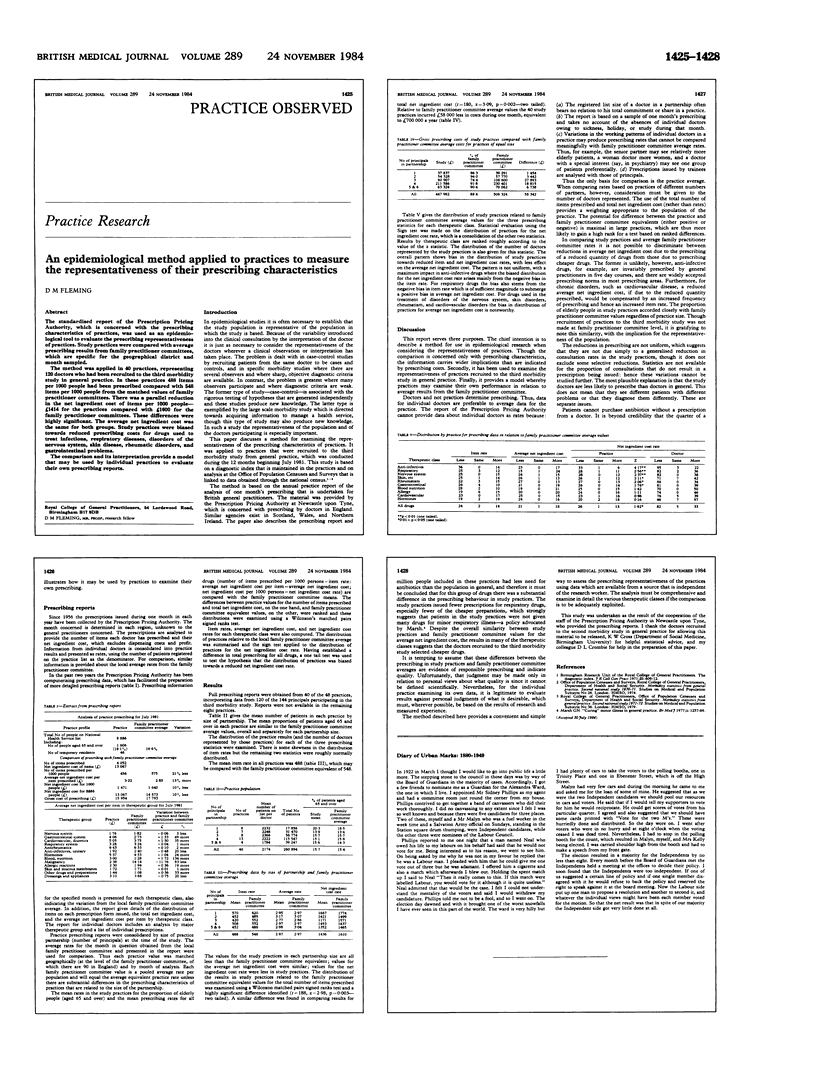
Abstract
The standardised report of the Prescription Pricing Authority, which is concerned with the prescribing characteristics of practices, was used as an epidemiological tool to evaluate the prescribing representativeness of practices. Study practices were compared with average prescribing results from family practitioner committees, which are specific for the geographical district and month sampled. The method was applied in 40 practices, representing 120 doctors who had been recruited to the third morbidity study in general practice. In these practices 488 items per 1000 people had been prescribed compared with 548 items per 1000 people from the matched values of family practitioner committees. There was a parallel reduction in the net ingredient cost of items per 1000 people--1414 pounds for the practices compared with 1600 pounds for the family practitioner committees. These differences were highly significant. The average net ingredient cost was the same for both groups. Study practices were biased towards reduced prescribing costs for drugs used to treat infections, respiratory diseases, disorders of the nervous system, skin disease, rheumatic disorders, and gastrointestinal problems. The comparison and its interpretation provide a model that may be used by individual practices to evaluate their own prescribing reports.
Full text
PDFPage 1425-1428