Abstract
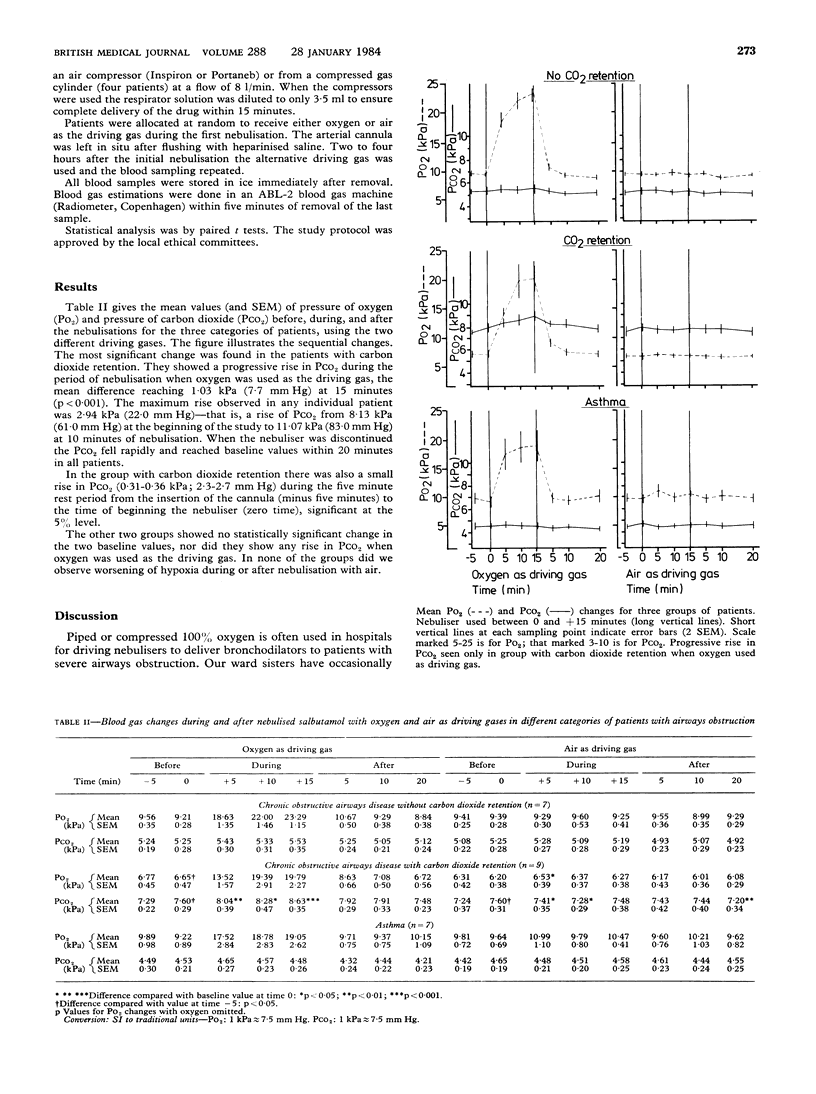
Changes in blood gas tensions occurring when 100% oxygen or air was used as the driving gas for nebulised salbutamol were studied in 23 patients with severe airways obstruction. The patients fell into three groups: nine had chronic bronchitis and emphysema with carbon dioxide retention, seven had emphysema and chronic bronchitis without carbon dioxide retention, and seven had severe asthma (no carbon dioxide retention). When oxygen was used as the driving gas patients who retained carbon dioxide showed a mean rise of 1.03 kPa (7.7 mm Hg) in their pressure of carbon dioxide (Pco2) after 15 minutes (p less than 0.001) but the Pco2 returned to baseline values within 20 minutes of stopping the nebuliser. The other two groups showed no rise in Pco2 with oxygen. When air was used as the driving gas none of the groups became significantly more hypoxic. Although it is safe to use oxygen as the driving gas for nebulisers in patients with obstructive airways disease with normal Pco2, caution should be exercised in those who already have carbon dioxide retention.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- COMROE J. H., Jr, BAHNSON E. R., COATES E. O., Jr Mental changes occurring in chronically anoxemic patients during oxygen therapy. J Am Med Assoc. 1950 Jul 22;143(12):1044–1048. doi: 10.1001/jama.1950.02910470004002. [DOI] [PubMed] [Google Scholar]
- DaCosta J., Hedstrand U. The effect of a new sympathomimetic beta-receptor stimulating drug (terbutaline) on arterial blood gases in bronchial sthma. Scand J Respir Dis. 1970;51(3):212–217. [PubMed] [Google Scholar]
- Flenley D. C. Blood gas tensions in severe asthma. Proc R Soc Med. 1971 Nov;64(11):1149–1151. [PMC free article] [PubMed] [Google Scholar]
- Rees H. A., Borthwick R. C., Millar J. S., Donald K. W. Aminophylline in bronchial asthma. Lancet. 1967 Dec 2;2(7527):1167–1169. doi: 10.1016/s0140-6736(67)91890-9. [DOI] [PubMed] [Google Scholar]
- Rees H. A., Millar J. S., Donald K. W. A study of the clinical course and arterial blood gas tensions of patients in status asthmaticus. Q J Med. 1968 Oct;37(148):541–561. [PubMed] [Google Scholar]
- SIEKER H. O., HICKAM J. B. Carbon dioxide intoxication: the clinical syndrome, its etiology and management with particular reference to the use of mechanical respirators. Medicine (Baltimore) 1956 Dec;35(4):389–423. [PubMed] [Google Scholar]
- Tai E., Read J. Response of blood gas tensions to aminophylline and isoprenaline in patients with asthma. Thorax. 1967 Nov;22(6):543–549. doi: 10.1136/thx.22.6.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WESTLAKE E. K., SIMPSON T., KAYE M. Carbon dioxide narcosis in emphysema. Q J Med. 1955 Apr;24(94):155–173. [PubMed] [Google Scholar]


