Abstract
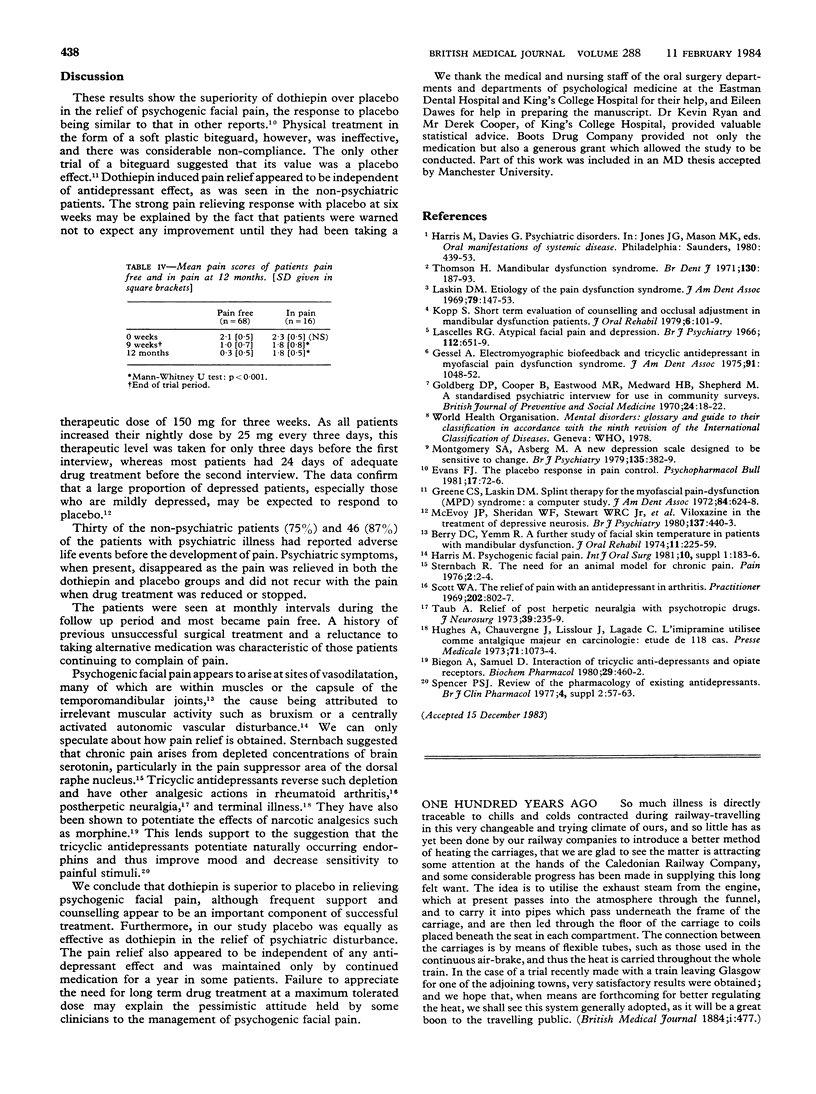
Ninety three patients took part in a two centre double blind controlled clinical trial designed to assess the efficacy of dothiepin (Prothiaden) as compared with placebo and a soft biteguard in the treatment of psychogenic facial pain. The results showed the superiority of dothiepin over placebo in achieving pain relief; 71% of patients were pain free in the dothiepin group at nine weeks compared with 47% in the placebo group. The biteguard conferred no benefit and compliance in its use was poor. Out of 84 patients followed up for 12 months, 68 (81%) became pain free. An adverse life event before development of pain, minimal previous surgical treatment, and freedom from pain at nine weeks were strong prognostic indicators for successful treatment. These results are clear evidence of the efficacy of dothiepin in psychogenic facial pain, though the drug may be needed for up to a year.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Biegon A., Samuel D. Interaction of tricyclic antidepressants with opiate receptors. Biochem Pharmacol. 1980 Feb;29(3):460–462. doi: 10.1016/0006-2952(80)90531-6. [DOI] [PubMed] [Google Scholar]
- Evans F. J. The placebo response in pain control. Psychopharmacol Bull. 1981 Apr;17(2):72–76. [PubMed] [Google Scholar]
- Gessel A. H. Electromygraphic biofeedback and tricyclic antidepressants in myofascial pain-dysfunction syndrome: psychological predictors of outcome. J Am Dent Assoc. 1975 Nov;91(5):1048–1052. doi: 10.14219/jada.archive.1975.0512. [DOI] [PubMed] [Google Scholar]
- Goldberg D. P., Cooper B., Eastwood M. R., Kedward H. B., Shepherd M. A standardized psychiatric interview for use in community surveys. Br J Prev Soc Med. 1970 Feb;24(1):18–23. doi: 10.1136/jech.24.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene C. S., Laskin D. M. Splint therapy for the myofascial pain--dysfunction (MPD) syndrome: a comparative study. J Am Dent Assoc. 1972 Mar;84(3):624–628. doi: 10.14219/jada.archive.1972.0090. [DOI] [PubMed] [Google Scholar]
- Harris M. Psychogenic facial pain. Int J Oral Surg. 1981;10(Suppl 1):183–186. [PubMed] [Google Scholar]
- Kopp S. Short term evaluation of counselling and occlusal adjustment in patients with mandibular dysfunction involving the temporomandibular joint. J Oral Rehabil. 1979 Apr;6(2):101–109. doi: 10.1111/j.1365-2842.1979.tb01270.x. [DOI] [PubMed] [Google Scholar]
- Lascelles R. G. Atypical facial pain and depression. Br J Psychiatry. 1966 Jul;112(488):651–659. doi: 10.1192/bjp.112.488.651. [DOI] [PubMed] [Google Scholar]
- Laskin D. M. Etiology of the pain-dysfunction syndrome. J Am Dent Assoc. 1969 Jul;79(1):147–153. doi: 10.14219/jada.archive.1969.0234. [DOI] [PubMed] [Google Scholar]
- McEvoy J. P., Sheridan W. F., Stewart W. R., Jr, Ban T. A., Wilson W. H., Guy W., Schaffer J. D. Viloxazine in the treatment of depressive neurosis: a controlled clinical study with doxepin and placebo. Br J Psychiatry. 1980 Nov;137:440–443. doi: 10.1192/bjp.137.5.440. [DOI] [PubMed] [Google Scholar]
- Montgomery S. A., Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979 Apr;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Scott W. A. The relief of pain with an antidepressant in arthritis. Practitioner. 1969 Jun;202(212):802–807. [PubMed] [Google Scholar]
- Sternbach R. A. The need for an animal model of chronic pain. Pain. 1976 Mar;2(1):2–4. [PubMed] [Google Scholar]
- Taub A. Relief of postherpetic neuralgia with psychotropic drugs. J Neurosurg. 1973 Aug;39(2):235–239. doi: 10.3171/jns.1973.39.2.0235. [DOI] [PubMed] [Google Scholar]
- Thomson H. Mandibular dysfunction syndrome. Br Dent J. 1971 Mar 2;130(5):187–193. doi: 10.1038/sj.bdj.4802645. [DOI] [PubMed] [Google Scholar]


