Short abstract
The UK, like many other countries, is trying to reduce health inequality. Current targets, however, could end up improving the health of the richest fastest
The UK government's health inequalities policy aims to improve the health of the poorest fastest.1-3 Targets have been set to reduce health gaps between population groups,4 indicators have been identified for monitoring progress,1 and the new planning tool of health equity audit has been made mandatory for all primary care trusts.4 All these require the quantification and comparison of health gaps. Although we have many guidelines and directions on how to reduce socioeconomic inequalities in health, there has been little discussion or clear direction on how to quantify inequalities. This is important because the way health gaps are measured and compared affects the results. Lack of clarity about these distinctions has led to inconsistencies in the targets set and anomalies in how progress is assessed.
How should we measure health gaps?
The measurement issue has been brought into focus by the government's recent status report on delivery of the national health inequalities strategy.3 The report raises, but does not answer, two questions about how to assess progress in reducing health inequalities. Should progress be assessed in terms of:
changes in absolute or relative gaps?
changes in gaps between a target group and the average or changes in gaps within populations?
Below we use simple graphs to explain these distinctions and their importance for health policy.
Distinction between relative and absolute gaps
The national targets for reducing health inequalities are set using different measures of gaps in health. The targets for infant mortality and life expectancy at birth use relative gaps,5 whereas the targets for mortality from cancer and circulatory diseases use absolute gaps.3,5
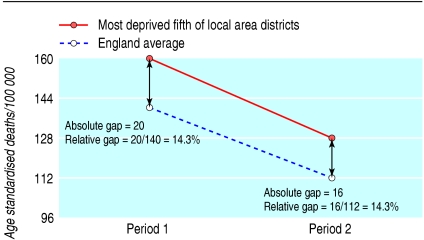
Figure 1 shows the distinction between absolute and relative gaps using data on cancer mortality for the most deprived fifth of local authority districts and England as a whole.3 In period 1 the cancer death rate for the most deprived districts (160) is higher than the England average (140). The gap can be presented either in absolute terms (20 deaths per 100 000) or in relative terms, as 14.3% of the England death rate (20/140).
Fig 1.
Health gaps in mortality from cancer between the most deprived fifth of districts and the national average. Baseline rates are taken from Department of Health data with rounding to facilitate clarity
To consider the implications of measuring absolute and relative gaps when considering changes over time, let us assume that death rates decrease by 20% for both groups between periods 1 and 2, as shown by the two lines in figure 1. The relative gap at period 1 and at period 2 is 14.3%. The rate of reduction of mortality is the same in both groups, and this is faithfully captured by the relative gap. However, the absolute gap has decreased by 20% from 20 to 16/100 000.
The 2004 spending review identified a spearhead group of 88 primary care aligned with the fifth of local authority districts with the worst health and deprivation indicators. The government set a new health improvement target to reduce mortality from cancer by at least 20% with a reduction in the absolute gap of at least 6% between the spearhead group and the whole population by 2010. As figure 1 shows, an across the board reduction in mortality of 20% will in itself result in a 20% reduction in the absolute gap. The target of a 20% reduction in the death rate for England as a whole, in conjunction with a 6% reduction in the absolute gap between the England average and the spearhead group, implies that the health of the spearhead group should improve more slowly than the average. This, of course, is not consistent with the policy objective of improving the health of the poorest fastest.
Health equity audit
The advantage of measuring relative gaps is that they are scale neutral. This is relevant if there is a general decrease (or increase) in the level of a health outcome indicator.6 But relative gaps have another advantage. Because they are scale neutral, inequality can be compared for rates of outcome measured on different scales. This means that relative gaps in need (health outcomes) can be compared directly with relative gaps in service delivery (rates of access to or use of services). This comparison is the essence of health equity audit, which aims to reduce inequalities in health outcomes by identifying how fairly services or other resources are distributed in relation to the health needs of different groups.4
For service distribution to be fair, any socioeconomic inequality in health should be balanced by a similar level of socioeconomic inequality in delivery of health care related to that outcome. For example, if a minority ethnic group has a greater rate of ill health than the rest of the population, the minority group should also have a greater rate of access to relevant health services.
The health equity audit of coronary heart disease by the County Durham and Tees Valley Public Health Network provides a practical example.7 For each primary care trust, the network estimated relative gaps across wards using deprivation score as the socioeconomic dimension. The relative gaps in mortality from coronary heart disease were used as an indicator of need and compared with the relative gaps in the elective admission rate for coronary heart disease. In all trusts, the relative gap in mortality between deprived and affluent wards was greater than the relative gap in elective admissions, indicating an inequity in provision relative to need. However, the magnitude of the inequity differed by a factor of five across the trusts. In general, those trusts with high levels of socioeconomic inequality in mortality from coronary heart disease also had the highest levels of inequity in provision relative to need.
Use of relative gaps enables a direct link to be established between inequity of provision and inequalities in health outcomes. This is essential both to identify areas where changes in provision can be expected to help reduce inequalities in health outcomes and to evaluate the effect of health equity audit on reducing health inequalities.
Gaps between and within groups
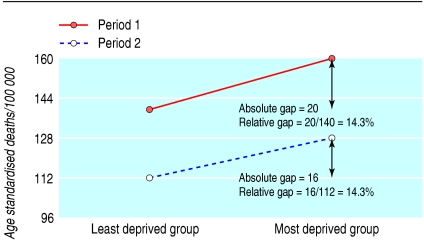
To appreciate the distinction of measuring health inequality between and within groups contrast figure 1 with figure 2, which presents exactly the same information. Instead of comparing how health indicators have changed across time for two different populations, figure 2 compares how health indicators vary across subgroups within a single population for one period and then compares this with another period. The slopes of the lines in figure 2 represent the levels of inequality at each period. The measure of the inequality at each period will be the relative gap. As before, the denominator for calculating the relative gap is the least deprived.
Fig 2.
Health gaps in mortality from cancer measured within a population
In their review of progress in reducing gaps in life expectancy in the UK, Shaw et al pointed out some of the problems with the government's between approach (fig 1) to setting and monitoring national targets and opted to use the within approach (fig 2). However, Shaw et al did not discuss the problem of using the between approach in monitoring progress at the local level.
The Healthcare Commission will use the targets set for reducing the gap in health inequality between the spearhead group and the England average to assess performance of primary care trusts as part of future annual trust ratings.8 But, since the targets only apply to spearhead trusts, only 20% of trusts will have their performance rated on reducing health inequality. This is something of an anomaly, given that all trusts are mandated to adopt strategies, including health equity audits, to reduce health inequalities in their local populations.
Use of the within measurement approach would overcome the anomaly. All primary care trusts could be set a common target to reduce the relative gap between their most deprived and most affluent wards. Another advantage of using the within approach is that a more inclusive measure of socioeconomic inequality can be used.9 One such metric is the slope index of inequality, which has been applied locally across all wards within a primary care trust,10,11 nationally across all districts within a country,12 and globally across continents.13 The use of inclusive measures is important because the government has made it clear that its health inequalities agenda is not just concerned with the extreme ends of the spectrum but with the gradient across the whole population.14,15
Discussion
In support of reporting progress in terms of absolute gaps, the Department of Health status report quotes the former chief medical officer, Donald Acheson, who argued that absolute rather than relative measures should be used to identify major problems that need tackling.16 However, once the problems have been identified, we argue that changes in absolute gaps can be misleading and that relative gaps should be used to measure progress.
For example, the status report claims that the narrowing of absolute gaps in death rates from cancer and circulatory disease shows that progress is being made in reducing health inequalities.3 This interpretation is misleading when set against the objective of increasing the health of the poorest fastest and the observation that relative gaps have not narrowed.
Summary points
The UK has a policy objective to improve the health of the poorest fastest
Measuring absolute gaps in health outcomes gives a misleading impression of progress
Relative gaps should be used to assess progress in reducing health inequality
Relative gaps can also be used to compare inequality of health outcome with inequalities in provision of health services
Measurement of health gaps within populations rather than between populations will provide a more inclusive rating system
The advantage of using the between approach to set targets and monitor progress is that it mirrors the long used and familiar health inequality measure of the standardised mortality ratio. However, we join Shaw et al in questioning whether this conventional approach is fit for purpose.
Most descriptions of the national inequality targets do not specify whether the reductions required are relative or absolute, as if it does not matter. We have shown why it does matter. Moreover, lack of transparency in this regard has led to the inconsistent use of relative and absolute gaps in government targets going unquestioned. It has also resulted in confusion over how to establish local health improvement targets that are consistent with national policy on reducing health inequalities.
Contributors and sources: Anne Low has led work on tackling health inequalities in southern Africa and the north east of England. Allan Low wrote his MSc thesis on the assessment of health inequalities in Sunderland. Both authors have published independently and jointly on health inequality issues relating to developing countries and the UK. The idea for this article came out of discussions at the 13th UK Public Health Association annual conference in April 2005. Allan Low wrote the first draft. Anne Low provided information on policy directives and edited subsequent drafts. Allan Low is guarantor.
Competing interests: None declared.
References
- 1.Department of Health. Tackling health inequalities: a programme for action. London: DoH, 2003.
- 2.Wanless D. Securing good health for the whole population. London: HM Treasury, 2004.
- 3.Department of Health. Tackling health inequalities: status report on the programme for action. London: DoH, 2005.
- 4.Department of Health. National standards, local action: health and social care standards and planning framework 2005/6-2007/8. London: DoH, 2004.
- 5.Department of Health. Technical notes for the spending review 2004. Public service agreement 2005-2006. www.dh.gov.uk/assetRoot/04/08/69/19/04086919.pdf (accessed 10 Feb 2006).
- 6.Low A, Low A. Relative rather than absolute gaps are important over time and place. BMJ 2005;330: 1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fleming M, Eynon C, Reilly M, Green L. Mending hearts: inequality and inequity in coronary heart disease, County Durham and Tees Valley, 1993-2003. Middlesbrough: County Durham and Tees Valley Public Health Network, 2005.
- 8.Healthcare Commission. Assessment of new national targets. http://ratings2006.healthcarecommission.org.uk/Indicators_2006Nat/home.asp (accessed 26 Mar 2006).
- 9.Shaw M, Davey Smith G, Dorling D. Health inequalities under New Labour: reply. BMJ 2005;330: 1507-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Low A, Low A. Measuring the gap: quantifying and comparing local health inequalities. J Public Health 2004;26: 388-95. [DOI] [PubMed] [Google Scholar]
- 11.Low A. Health gaps analysis: a tool for addressing health inequalities [MSc dissertation]. York: University of York, 2002.
- 12.Shaw M, Davey Smith G, Dorling D. Health inequalities and New Labour: how the promises compare with real progress. BMJ 2005;330: 1016-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dorling D, Shaw M, Davey Smith G. Global inequality of life expectancy due to AIDS. BMJ 2006;332: 662-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wanless D. Securing good health for the whole population: population health trends. London: HM Treasury, 2003.
- 15.Johnson M. The challenge of tackling health inequalities—mobilising action at all levels and in all sectors. Ministerial speech at first Health Development Agency annual conference, London, October 2003. http://image.guardian.co.uk/sys-files/Society/documents/2003/10/30/MelanieJohnsonSpeech.pdf (accessed 24 Mar 2006)
- 16.Acheson D. Independent inquiry into inequalities in health report. London: HMSO, 1998.