Abstract
Objectives To analyse trends in preterm delivery and the factors contributing to preterm delivery in Denmark. To construct a standard population at low risk (white European, 20-40 years of age, with a singleton spontaneous pregnancy) and describe the changes in this population so that time trends can be compared internationally.
Design Population based study.
Participants 99.8% of all deliveries in Denmark, 1995-2004.
Main outcome measures Proportion of babies born at less than 37 weeks' completed gestation for each year in the overall population and in a standard population at low risk.
Results Overall, the proportion of preterm deliveries increased by 22% from 1995 to 2004. During the same period, known risk factors for preterm delivery such as in vitro fertilisation, multiple pregnancies, and elective deliveries also increased, and logistic regression analyses showed that these factors were associated with an increased risk of preterm delivery. Spontaneous preterm deliveries in primiparous women at low risk rose 51% (from 3.8% to 5.7%) during this time compared with 20% (2.7% to 3.2%) in multiparous women at low risk.
Conclusions The overall proportion of preterm deliveries increased significantly from 1995 to 2004 and primiparity and multiple birth were the most important contributing factors. The rise in spontaneous preterm deliveries in the standard population of primiparous women at low risk was greater than in the total population.
Introduction
Recent data show an increase in the proportion of pre-term births (live infants born before 37 weeks' completed gestation out of all live born infants) in the United States (11.0% in 1995 v 12.1% in 2002) and Norway (7.5% in 1995 v 8.5% in 2002).1,2 The prevalence of several risk factors for preterm delivery, such as in vitro fertilisation (IVF) high maternal age, primiparity, and elective delivery before term, have changed in recent years and this may explain the increase in the proportion of preterm deliveries.
We used data from the Danish national registers to calculate the proportion of preterm deliveries in low risk pregnancies from 1995 to 2004.
Methods
Data comprised case based information from four national registries on 99.8% of live births in Denmark from 1995 to 2004 (646 144 deliveries and 659 154 infants). To study changes in the proportion of spontaneous preterm births over time in women at low risk, we selected a standard population consisting of white European primiparous women aged 20-40 with a singleton spontaneous pregnancy. We calculated the proportion of spontaneous preterm deliveries by dividing the number of spontaneous preterm deliveries (excluding elective caesarean section and induction of labour) by the total number of deliveries in this population. We also studied the proportion of spontaneous preterm deliveries in multiparous women at low risk (20-40 year old white European multiparous women with a singleton spontaneous pregnancy) using the same methods as for primiparous women.
Results
The overall proportion of preterm deliveries (preterm births as a proportion of all live births) increased by 22% between 1995 and 2004 (from 5.2% to 6.3%). When we stratified preterm deliveries in the total population into extremely preterm (22-28 completed weeks of gestation), very preterm (28-32), and moderately preterm (32-36), we found increases of 41%, 22%, and 22% between 1995 and 2005 (table 1).
Table 1.
Deliveries in Denmark. Values are percentages of the total number of deliveries unless otherwise stated
|
Year
|
% Change 1995-2004
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | ||
| No of deliveries | 67 840 | 65 635 | 65 783 | 64 578 | 64 578 | 65 541 | 63 814 | 62 515 | 63 038 | 62 814 | −7.41 |
| Stage of delivery* | |||||||||||
| Extremely preterm | 0.22 | 0.27 | 0.21 | 0.20 | 0.22 | 0.21 | 0.26 | 0.24 | 0.31 | 0.31 | 40.91 |
| Very preterm | 0.55 | 0.61 | 0.58 | 0.61 | 0.61 | 0.61 | 0.59 | 0.63 | 0.66 | 0.67 | 21.82 |
| Moderately preterm | 4.40 | 4.85 | 4.39 | 4.57 | 4.54 | 4.76 | 5.09 | 5.18 | 5.26 | 5.36 | 21.82 |
| Term | 94.83 | 94.27 | 94.82 | 94.63 | 94.63 | 94.42 | 94.06 | 93.94 | 93.77 | 93.67 | −1.22 |
| Characteristics of mother: | |||||||||||
| White European | 95.23 | 94.81 | 94.33 | 94.01 | 93.75 | 93.61 | 93.59 | 93.63 | 94.02 | 94.43 | −0.84 |
| In vitro fertilisation | 1.17 | 1.55 | 1.89 | 2.03 | 2.43 | 2.82 | 2.99 | 2.95 | 3.37 | 2.47 | 111.11 |
| Multiple births | 1.70 | 1.89 | 1.88 | 1.98 | 1.97 | 1.99 | 2.23 | 2.22 | 2.24 | 2.26 | 32.9 |
| Primiparity† | 44.85 | 45.69 | 46.52 | 43.49 | 43.62 | 44.33 | 44.16 | 43.70 | 43.79 | 44.02 | −1.85 |
| Spontaneous delivery‡ | 87.63 | 87.17 | 93.28 | 92.82 | 88.67 | 85.70 | 84.68 | 82.11 | 80.52 | 79.18 | −9.64 |
| Smoker | 26.8 | 25.5 | 22.0 | 21.2 | 20.0 | 19.7 | 18.6 | 17.7 | 16.3 | 15.5 | −42.2 |
| Standard population§ | 34.88 | 35.33 | 37.97 | 35.41 | 33.54 | 32.80 | 32.47 | 31.49 | 31.01 | 31.31 | −10.24 |
Extremely preterm: 22-27 completed weeks of gestation; very preterm: 28-31; moderately preterm: 32-36; term: ≥37.
Women giving birth for the first time.
All deliveries except induced delivery and elective caesarian section.
20-40 year old white European primiparous women with a singleton spontaneous pregnancy.
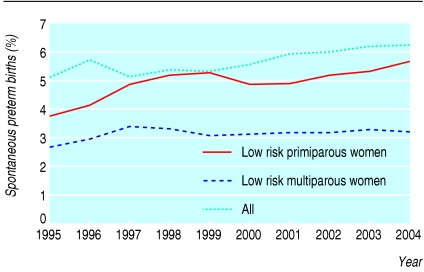
The proportion of spontaneous preterm deliveries in primiparous women at low risk increased by 51% (95% confidence interval 40% to 64%) between 1995 and 2004 (from 3.8% to 5.7%; figure). This rise was significantly higher than the 20% rise (2.7% to 3.2%) seen in the corresponding population of multiparous women at low risk.
Figure 1.
Time trends in spontaneous preterm birth in Denmark
Table 2 shows the multivariate logistic regression analysis comparing extremely preterm, very preterm, and moderately preterm births with term and post-term (≥ 37 weeks) births in the general population. Maternal age and smoking habits, parity, IVF, multiple pregnancy, elective delivery, ethnic origin, and the year of delivery had a significant effect on preterm delivery in all groups. Elective delivery was associated with a decrease in extremely preterm and very preterm delivery and with an increase in moderately preterm delivery, whereas a white European origin was associated with a reduced risk of moderately preterm delivery.
Table 2.
Multivariate logistic analysis of risk factors for preterm delivery in Denmark, 1995-2004
|
All preterm
|
Extremely preterm*
|
Very preterm*
|
Moderately preterm*
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| No | Odds ratio (95% CI) | No | Odds ratio (95% CI) | No | Odds ratio (95% CI) | No | Odds ratio (95% CI) | ||
| Mode of conception: | |||||||||
| Spontaneous | 63 0928 | 34 039 | 1.00 | 1379 | 1.00 | 3607 | 1.00 | 29 053 | 1.00 |
| In vitro fertilisation | 15 216 | 2 711 | 1.25 (1.19 to 1.32) | 197 | 1.76 (1.47 to 2.12) | 345 | 1.15 (1.01 to 1.31) | 2 169 | 1.17 (1.10 to 1.24) |
| Initiation of delivery: | |||||||||
| Spontaneous | 55 7267 | 29 870 | 1.00 | 1433 | 1.00 | 3344 | 1.00 | 25 093 | 1.00 |
| Elective | 88 877 | 6 880 | 1.09 (1.06 to 1.12) | 143 | 0.39 (0.33 to 0.46) | 608 | 0.77 (0.71 to 0.85) | 6 129 | 1.19 (1.15 to 1.23) |
| Parity: | |||||||||
| Primiparous | 28 7080 | 19 938 | 1.53 (1.49 to 1.57) | 931 | 1.79 (1.60 to 1.99) | 2240 | 1.63 (1.52 to 1.74) | 16 767 | 1.48 (1.44 to 1.51) |
| Multiparous | 35 9064 | 16 812 | 1.00 | 645 | 1.00 | 1712 | 1.00 | 14 455 | 1.00 |
| Type of pregnancy: | |||||||||
| Singleton | 633 012 | 30 859 | 1.00 | 1250 | 1.00 | 3171 | 1.00 | 26 438 | 1.00 |
| Multiple | 13 132 | 5 891 | 14.03 (13.75 to 14.90) | 326 | 11.12 (9.6 to 12.87) | 781 | 11.88 (10.83 to 13.02) | 4 784 | 11.70 (11.22 to 12.20) |
| Maternal age† | 646 144 | 36 750 | 1.01 (1.01 to 1.01) | 1576 | 1.03 (1.02 to 1.04) | 3952 | 1.02 (1.01 to 1.02) | 31 222 | 1.01 (1.01 to 1.01) |
| Year‡ | 646 144 | 36 750 | 1.03 (1.02 to 1.03) | 1576 | 1.06 (1.04 to 1.07) | 3952 | 1.03 (1.01 to 1.04) | 31 222 | 1.02 (1.02 to 1.03) |
| Smoking: | |||||||||
| Non-smoker | 489 129 | 24 820 | 1.00 | 916 | 1.00 | 2479 | 1.00 | 21 425 | 1.00 |
| Smoker | 131 914 | 9 190 | 1.52 (1.49 to 1.55) | 379 | 2.26 (2.11 to 2.42) | 1041 | 1.76 (1.68 to 1.85) | 7 770 | 1.41 (1.38 to 1.44) |
| Ethnic origin: | |||||||||
| White European | 608 339 | 34 778 | 0.93 (0.88 to 0.97) | 1493 | 0.86 (0.69 to 1.07) | 3751 | 0.94 (0.81 to 1.09) | 29 534 | 0.94 (0.89 to 0.98) |
| Other | 37 797 | 1 972 | 1.00 | 83 | 1.00 | 201 | 1.00 | 1 688 | 1.00 |
CI, confidence interval.
All odds ratios were mutually adjusted for other variables in the table.
Extremely preterm: 22-27 completed weeks of gestation; very preterm: 28-31; moderately preterm: 32-36; term: ≥37.
Odds ratio for a one year change in age.
Odds ratio for a one year change in calendar time.
A comparison of extremely preterm, very preterm, and moderately preterm delivery showed that IVF increased the risk of extremely preterm delivery significantly more than it increased the risk of very preterm and moderately preterm delivery (P < 0.001).
We calculated the population attributable risks using the prevalence of the various risk factors in the population. They were 17.7% for primiparity, 14.3% for multiple births, 7.2% for smoking, 5.7% for elective delivery, and 5.1% for IVF (based on the unadjusted risk ratios).
Discussion
In Denmark, the proportion of spontaneous preterm births increased by 51%—from 3.8% to 5.7%—over 10 years in primiparous women with singleton spontaneous pregnancies. The increase in this low risk group was higher than the increase in the total population (22%).
Limitations
Increases could theoretically be due to changes in registration policies or dating pregnancies by ultrasound, but this form of dating was used throughout the period and national clinical guidelines have not been changed recently.3,4 Estimated gestational ages may vary owing to inconsistencies in “rounding” and “truncating” the weeks of gestation at delivery, so all analyses were repeated using gestational age truncated to completed weeks only.3 This did not affect the conclusions, indicating that the increase in preterm delivery among low risk primiparous women with a singleton pregnancy is real. Furthermore, changes in methods of calculating and registering gestational age do not explain why the increase in preterm delivery is greater in primiparous women at low risk than in multiparous women at low risk.
Only primiparity and multiple births contributed substantially as explanatory factors of preterm delivery (17.7% and 14.3%). Of the risk factors, only multiple births after IVF could be prevented by transferring just one embryo. Although IVF is a strong risk factor for preterm delivery and contributes to the increase in multiple births, IVF in itself contributed little to the overall risk of preterm delivery (5.1%). Thus the increase is mainly due to other factors.
What is already known on this topic
The proportion of preterm births has increased in many countries over the past few decades. These increases have been attributed to increases in multiple births, greater use of in vitro fertilisation, and more obstetric intervention
Variations in dating pregnancies and calculating gestational age may result in misclassification of preterm delivery
What this study adds
In Denmark, the overall proportion of preterm delivery increased by 22% from 1995 to 2004
The proportion of spontaneous preterm births increased by 51% from 1995 to 2004 in primiparous women with singleton spontaneous pregnancies
The reasons for the higher increase in primiparous women at low risk are unknown
Implications
Do the increases in preterm delivery reflect increased levels of stress in women who try to cope with the demands of both a job and a family? Many obstetricians report that an increasing number of primiparous women are reluctant to take time off work when they are not well. Although stress during pregnancy correlates with preterm delivery, the contribution of stress to the increase in preterm deliveries is unknown.5 Both psychosocial stress and neuroendocrine factors such as corticotrophin releasing hormone are associated with preterm delivery.6
Analysing the differences in proportions of preterm deliveries between countries might increase our understanding of preterm delivery. Populations from different countries cannot be compared owing to different proportions of high risk pregnancies and parity, but using standard populations of primiparous women at low risk identified by the criteria described here could enable valid international comparisons of spontaneous preterm delivery rates to be made.
Editorial by Shennan and Bewley
This article was posted on bmj.com on 23 February 2006: http://bmj.com/cgi/doi/10.1136/bmj.38751.524132.2F
Contributors: JL-R conceived the study in collaboration with UK. SR retrieved register data and performed the initial analyses. UK performed additional statistical analyses. All authors contributed to the data interpretation. JL-R wrote the first draft of the manuscript and all authors contributed to the revision.
Funding: FIGO foundation of the Danish Society of Obstetrics and Gynaecology.
Competing interests: None declared.
Ethical approval: Danish Data Protection Agency.
References
- 1.National Center for Health Statistics fund. Preterm birth: US, 1992-2002. www.marchofdimes.com/peristats/ (accessed 1 Aug 2005).
- 2.Medical Birth Registry of Norway. Preterm births: Norway 1995-2002. www.mfr.no/ (accessed 1 Aug 2005).
- 3.Balchin I, Whittaker JC, Steer PJ, Lamont RF. Are reported preterm birth rates reliable? An analysis of interhospital differences in the calculation of the weeks of gestation at delivery and preterm birth rate. Br J Obstet Gynaecol 2004;111: 160-3. [DOI] [PubMed] [Google Scholar]
- 4.Yang H, Kramer MS, Platt RW, Blondel B, Breart G, Morin I, et al. How does early ultrasound scan estimation of gestational age lead to higher rates of preterm birth? Am J Obstet Gynecol 2002;186: 433-7. [DOI] [PubMed] [Google Scholar]
- 5.Hedegaard M, Henriksen TB, Sabroe S, Secher NJ. The relationship between psychological distress during pregnancy and birth weight for gestational age. Acta Obstet Gynecol Scand 1996;75: 32-9. [DOI] [PubMed] [Google Scholar]
- 6.Mancuso RA, Schetter CD, Rini CM, Roesch SC, Hobel CJ. Maternal prenatal anxiety and corticotropin-releasing hormone associated with timing of delivery. Psychosom Med 2004;66: 762-9. [DOI] [PubMed] [Google Scholar]