Abstract
Factors affecting the postincisional use of analgesics for ovariohysterectomy (OVH) in dogs and cats were assessed by using data collected from 280 Canadian veterinarians, as part of a national, randomized mail survey (response rate 57.8%). Predictors of analgesic usage identified by logistic regression included the presence of at least 1 animal health technician (AHT) per 2 veterinarians (OR = 2.3, P = 0.004), and the veterinarians’ perception of the pain caused by surgery without analgesia (OR = 1.5, P < 0.001). Linear regression identified the following predictors of veterinarians’ perception of pain: the presence of more than 1 AHT per 2 veterinarians (coefficient = 0.42, P = 0.048) and the number of years since graduation (coefficient = −0.073, P < 0.001). Some of these risk factors are similar to those identified in 1994. The results suggest that continuing education may help to increase analgesic usage. Other important contributors may be client education and a valid method of pain assessment.
Résumé
Facteurs influençant l’utilisation post opératoire d’analgésique chez les chiens et les chats par les vétérinaires canadiens en 2001. Les facteurs influençant l’utilisation post opératoire d’analgésiques lors d’ovario-hystérectomies (OVH) chez les chiennes et les chattes ont été évalués à partir de données recueillies chez 280 vétérinaires canadiens lors d’une enquête postale nationale effectuée au hasard (taux de réponse de 57,8 %). Les facteurs de prévision d’utilisation d’analgésiques, identifiés par régression logistique, comprenaient la présence d’au moins 1 technicien en santé animale (TSA) par 2 vétérinaires (OR = 2,3, P = 0,004) et la perception par les vétérinaires de la douleur causée par la chirurgie sans analgésie (OR = 1,5, P < 0,001). La régression linéaire a identifié les facteurs suivants de perception de la douleur par les vétérinaires : la présence de plus de 1 TSA par 2 vétérinaires (coefficient = 0,42, P = 0,048) et le nombre d’années depuis la graduation (coefficient = −0,073, P < 0,001). Certains de ces facteurs de risque sont semblables à ceux identifiés en 1994. Les résultats suggèrent que la formation continue pourrait aider à augmenter l’utilisation d’analgésiques. D’autres facteur importants pourraient être l’éducation des clients et une méthode efficace d’évaluation de la douleur.
(Traduit par Docteur André Blouin)
Introduction
In 1994, a randomized national survey of Canadian veterinarians indicated that the likelihood of postoperative analgesic use was greater in practices where animal health technicians (AHTs) were employed, and that it increased with increases in the veterinarians’ perception of the pain caused by surgery (1). Pain perception was, in turn, affected by the veterinarian’s gender and the employment of AHTs (1). The likelihood of postoperative analgesic usage was reduced by concerns about various negative aspects of opioid drugs (1). Since 1994, approaches to analgesia have been refined and nonsteroidal anti-inflammatory drugs (NSAIDs) have become available. In light of this, a 2nd survey was conducted in 2001 to examine the extent of perioperative analgesic usage among Canadian veterinarians and to identify factors predicting analgesic use. The descriptive data are presented in a preceding paper (2). This paper presents the factors influencing analgesic use.
Materials and methods
The study design and details of data collection are described in detail in the preceding paper (2). Data were collected by means of a mailed questionnaire, a copy of which is available on request. All eligible veterinarians in Atlantic Canada and a random sample of eligible veterinarians from the rest of Canada were surveyed (n = 652). They provided demographic information, information about their attitudes to pain, and information about their preincisional and postincisional use of analgesics in dogs and cats following common surgeries (analgesic drugs given respectively at any time before or after the first incision).
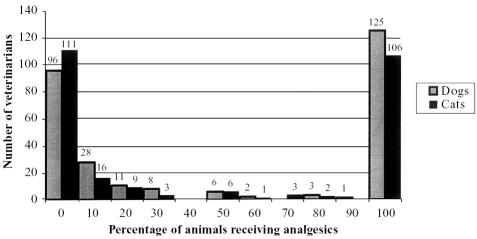
Analysis to identify factors affecting usage of preincisional drugs was not possible, because the vast majority of respondents gave these drugs to all their surgical cases (2), limiting the power of any analysis. The distribution of postincisional analgesic use by respondents was bimodal (Figure 1). Based on the distribution of those data and on best analgesic practice, the outcome was dichotomized as those respondents who gave postincisional analgesics to 100% of cases of a particular surgery, and those respondents who gave postincisional analgesics to less than 100% of their cases. Ovariohysterectomy was chosen as the representative surgery in dogs and cats, because it is common, invasive, and there is little variability in the surgical procedure; also, the outcome was divided between analgesic users and nonusers more evenly than for other surgeries.
Figure 1.
Distribution of Canadian veterinarians according to the percentages of dogs and cats that underwent ovariohysterectomy and received postincisional analgesia.
A causal diagram was drafted with analgesic use as the outcome, including all potential predictor variables, as follows: the veterinarian’s sex, age, and school of graduation; the number of years since graduation; the practice type (small animal or mixed), and the province where the practice was located; the number of veterinarians in the practice, and the ratio of animal health technicians to veterinarians (either more than 1 AHT per 2 veterinarians, or 1 or fewer AHTs per 2 veterinarians); the average number of surgeries that the veterinarian performed each month; the veterinarian’s perception of the pain felt in the first 24 h after surgery, if no analgesics (neither pre- nor postincisional) were given; the date of the veterinarian’s last attendance at continuing education about perioperative analgesia; the veterinarian’s reported adequacy of knowledge about perioperative analgesia; and the veterinarian’s maximum level of concern about using each of butorphanol, morphine, and NSAIDs. Maximum level of concern was derived from the ratings (on a scale of 1 to 10) that the veterinarian assigned to a list of several potential concerns, appropriate to each drug type; each list included specific side effects and cost.
The linearity of the relationship of continuous variables with the outcome was assessed by examination of smoothed scatterplots. Univariable analyses (chi square or logistic regression, as appropriate) were used to identify predictors having some association with the outcome (P ≤ 0.2). The variables that best predicted analgesic use were identified by using a combination of forward and backward stepwise logistic regression, and manual comparisons of possible models. Significant variables (P ≤ 0.1) were assessed for confounding and interaction. The model’s fit and adequacy were assessed by using the Hosmer-Lemeshow χ2 statistic, and assessing standardized residuals and the delta-beta values of covariate patterns (3).
A similar procedure, involving the same potential risk factors, was used to develop a linear regression model that identified factors affecting veterinarians’ perception of the pain caused during the first 24 h after surgery, if no analgesia were used, on a scale of 1 to 10. In the case of continuous predictor variables, the Pearson correlation coefficient was used to first identify if they had potential to contribute to the model. Homoscedasticity and normality were assessed. The model’s fit and adequacy were also assessed by use of the multiple correlation coefficient (R2) and by examination of standardized residuals, leverage points, and the deltabeta and dfits statistics (3). All statistical analyses were performed by using specialized software (Stata, version 7; Stata Corporation, College Station, Texas, USA).
Results
The response rate of the survey was 57.8%. The demographic characteristics of the respondents, and the data describing analgesic usage, pain perception scores, concerns about drugs, and respondents’ preferences in continuing education have all been presented previously (2). Analgesic use in dogs was highly correlated with that in cats (r = 0.865), as was pain perception (r = 0.944); therefore, the analysis was restricted to dogs (n = 280). Of these respondents, not all provided data on all variables; this is reflected in the denominators of the following results.
Descriptive data are given in Table 1. Approximately 45% (44.6%, 125/280) of respondents were analgesic users. Age was not examined as a potential predictor for either model, because it was highly correlated with “years since graduation,” which was examined (Table 1). Concern about adverse reactions to morphine, and attendance at continuing education about perioperative analgesia within the past 12 mo were also omitted, because 43 (15.4%) and 62 (22.1%) of their respective data points were missing. The other potential predictor variables for analgesic use and the results of analysis of unconditional associations are listed in Table 1. The final model is shown in Table 2; model checking indicated no strongly influential observations. The odds of a dog receiving postincisional analgesics increased with the veterinarian’s perception of pain. Thus, if a dog were spayed by a veterinarian whose perception of pain was 2 units higher than that of a colleague, the dog would be (1.5)2 = 2.25 times more likely to receive postincisional analgesia. The odds of analgesic usage were more than doubled if there were more than 1 AHT per 2 veterinarians. Graduates of the Atlantic Veterinary College (AVC) or the Ontario Veterinary College (OVC) were more likely to be analgesic users than were graduates of other colleges: analgesic usage was approximately one third as likely if veterinarians had graduated from the Faculté de médecine vétérinaire, Université de Montréal (FMV) or the Western College of Veterinary Medicine (WCVM). The veterinarians’ concerns about negative aspects of using butorphanol reduced the odds of veterinarians giving analgesia to all their patients: if a dog were spayed by a veterinarian whose maximum level of concern was 2 units higher than that of a colleague, the odds of the dog receiving analgesia would be approximately (0.88)2 = 0.78 times that of a dog spayed by the colleague.
Table 1.
Factors with the potential to affect postincisional analgesic use for canine ovariohysterectomy among 280 Canadian veterinarians: descriptive statistics and unconditional associations
| Analgesic nonusers (N = 155)
|
Analgesic users (N = 125)
|
||||||
|---|---|---|---|---|---|---|---|
| Variable name | na | % | Mean (sb) | na | % | Mean (sb) | P |
| Veterinarian’s sex | — | — | 0.5 | ||||
| Male | 64 | 41.6 | 47 | 37.6 | |||
| Female | 90 | 58.4 | 78 | 62.4 | |||
| Number of years since graduation | 155 | — | 13.1 (8.8) | 124 | — | 11.7 (9.4) | 0.2 |
| School of graduation | — | — | 0.09 | ||||
| Atlantic Veterinary College | 38 | 24.5 | 38 | 30.7 | |||
| Ontario Veterinary College | 53 | 34.1 | 54 | 43.6 | |||
| Western College of Veterinary Medicine | 29 | 18.7 | 17 | 13.7 | |||
| Université de Montréal | 25 | 16.1 | 10 | 8.0 | |||
| Other | 10 | 6.6 | 5 | 4.0 | |||
| Practice type (small animal or mixed practice) | — | — | 0.11 | ||||
| Mixed | 52 | 33.6 | 31 | 24.8 | |||
| Companion animal | 103 | 66.4 | 94 | 75.2 | |||
| Region of Canada in which practice located | — | — | 0.01 | ||||
| Atlantic Canada | 74 | 47.7 | 60 | 48.0 | |||
| Quebec | 18 | 11.6 | 5 | 4.0 | |||
| Ontario | 28 | 8.1 | 41 | 32.8 | |||
| Manitoba, Saskatchewan, Alberta | 20 | 12.9 | 10 | 8.0 | |||
| British Columbia | 15 | 9.7 | 9 | 7.2 | |||
| Number of veterinarians in the practice | 155 | — | 3.3 (1.9) | 125 | — | 3.5 (2.8) | 0.35 |
| Ratio of animal health technicians (AHTs) to veterinarians | — | — | 0.01 | ||||
| Exceeds 1 AHT per 2 veterinarians | 93 | 61.2 | 57 | 46.0 | |||
| Equal to or less than 1 AHT per 2 veterinarians | 59 | 38.8 | 67 | 54.0 | |||
| Average monthly number of surgeries, per veterinarian | 155 | — | 14.9 (10.8) | 125 | — | 13.0 (10.4) | 0.142 |
| Perception of the pain in the first 24 h after surgery if no analgesic were used at any time (on a scale of 1 to 10) | 155 | — | 5.1 (1.9) | 123 | — | 6.5 (1.6) | <0.001 |
| Most highly rated concern from among various negative aspects (side effects; cost) of each of (on a scale of 1 to 10) | |||||||
| Butorphanol | 151 | — | 4.8 (2.4) | 123 | — | 4.1 (2.1) | 0.01 |
| Nonsteroidal antiinflammatory drugs | 154 | — | 4.5 (2.1) | 122 | — | 4.1 (2.3) | 0.18 |
| Knowledge of analgesia reported to be | 0.03 | ||||||
| Adequate | 67 | 43.8 | — | 70 | 56.9 | — | |
| Inadequate | 86 | 56.2 | — | 53 | 43.1 | — | |
For some variables missing data meant that the total of n < N
Standard deviation
Table 2.
Final logistic regression model of factors affecting veterinarians’ use of postincisional analgesics in dogs undergoing ovariohysterectomy
| Predictor | Odds ratio (coefficient) | 95% confidence interval | P |
|---|---|---|---|
| Veterinarian’s perception of the pain caused by surgery | 1.5 (0.41) | 1.3, 1.7 | < 0.001 |
| School of graduationa | |||
| Ontario Veterinary College | 0.98 (−0.019) | 0.51, 1.9 | 0.96 |
| Western College of Veterinary Medicine | 0.35 (−1.0) | 0.15, 0.83 | 0.018 |
| Faculté de médecine vétérinaire, Université de Montréal | 0.34 (−1.1) 0.12, 0.94 | 0.037 | |
| Other | 0.53 (−0.63) | 0.15, 1.9 | 0.33 |
| Maximum level of concern about butorphanol | 0.88 (−0.12) | 0.78, 0.99 | 0.047 |
| Ratio of animal health technicians to veterinarians exceeds | 0.5 2.3 (0.82) | 1.3, 4.0 | 0.004 |
Compared with the Atlantic Veterinary College
Hosmer Lemeshow χ2 = 3.0, P = 0.94
No interactions were detected, but there was evidence that the AHT variable was confounded by school of graduation. Unlike graduates from the AVC or OVC, graduates from the WCVM or FMV were more likely to work in practices with a ratio of more than 1 AHT per 2 veterinarians (WCVM: OR = 3.1, 95% confidence interval = 1.4, 6.8; FMV: OR = 3.3, 95% confidence interval = 1.4, 7.7). Year of graduation was not a significant predictor of analgesic use, once pain perception and the AHT variable had been controlled.
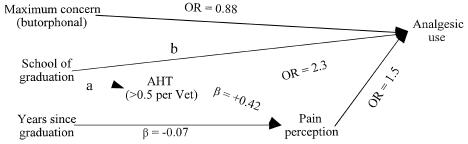
The results of analyses of unconditional associations between potential predictors and pain perception are shown in Table 3. The final model is shown in Table 4 and suggests that, on a scale of 1 to 10, a veterinarian’s rating of the pain caused by surgery without any analgesia was approximately 0.07 units lower for each year of graduation before 2001. The presence of more than 1 AHT per 2 veterinarians was associated with a pain rating that was higher than if there were 1 or fewer AHTs per 2 veterinarians. No interactions or confounding was detected, and the assumptions of homoscedasticity and normality were upheld (Cook Weisberg P = 0.813; Shapiro Wilk P = 0.329; no visual abnormalities on histogram of Studentized residuals, or Q-Q plot of residuals). Consistent with the low predictive ability of the model (Table 4), a substantial number of observations had large residuals (35 observations < −2, and 36 observations > 2): the negative group was comprised of veterinarians who gave pain a low rating, but who had graduated recently and worked in practices with more than 1 AHT per 2 veterinarians. The positive group was comprised of veterinarians with the opposite characteristics to the negative group. No influential observations were detected by the dfits or leverage statistics. A path model derived from all these results is shown in Figure 2.
Table 3.
Factors with the potential to affect veterinarians’ perception of the pain caused by canine ovariohysterectomy in the first 24 h after surgery, if no analgesics were given: descriptive statistics and unconditional associations
| Variable name | n | Mean pain ranking (s)a | Correlation coefficient | P |
|---|---|---|---|---|
| Veterinarian’s sex | 0.006 | |||
| Male | 110 | 5.4 (1.9) | — | |
| Female | 167 | 6.0 (1.8) | — | |
| Number of years since graduation | 280 | — | −0.32 | < 0.001 |
| School of graduation | 0.149 | |||
| Atlantic Veterinary College | 76 | 5.9 (1.8) | — | |
| Ontario Veterinary College | 106 | 5.7 (1.9) | — | |
| Western College of Veterinary Medicine | 46 | 6.0 (1.9) | — | |
| University of Montreal | 34 | 5.3 (1.9) | — | |
| Other | 15 | 5.2 (2.0) | — | |
| Practice type (small animal or mixed practice) | 0.803 | |||
| Mixed | 82 | 5.7 (2.2) | — | |
| Companion animal | 196 | 5.7 (1.8) | — | |
| Region of Canada in which practice located | 0.377 | |||
| Atlantic Canada | 134 | 5.6 (1.8) | — | |
| Quebec | 22 | 5.6 (2.0) | — | |
| Ontario | 68 | 6.1 (1.7) | — | |
| Manitoba, Saskatchewan, Alberta | 30 | 6.0 (2.2) | — | |
| British Columbia | 23 | 5.5 (2.1) | — | |
| Number of veterinarians in the practice | 280 | — | 0.02 | 0.746 |
| Ratio of animal health technicians (AHTs) to veterinarians | 0.083 | |||
| Exceeds 1 AHT per 2 veterinarians | 124 | 6.0 (1.9) | — | |
| Equal to or less than 1 AHT per 2 veterinarians | 150 | 5.6 (1.8) | — | |
| Average monthly number of surgeries, per veterinarian | 280 | — | −0.074 | 0.222 |
| Most highly rated concern (on a scale of 1 to 10) from among various negative aspects (side effects; cost) of each of | ||||
| Butorphanol | 274 | — | −0.054 | 0.38 |
| Nonsteroidal antiinflammatory drugs | 276 | — | −0.044 | 0.46 |
| Knowledge of analgesia reported to be | 0.02 | |||
| Adequate | 136 | 6.0 (1.9) | — | |
| Inadequate | 138 | 5.5 (1.8) |
Mean (standard deviation; 95% confidence interval)
Table 4.
Final linear regression model of factors affecting Canadian veterinarians’ perception of the pain experienced by dogs in the first 24 h after ovariohysterectomy, if no analgesics were given
| Predictor | Coefficient | 95% confidence interval | P |
|---|---|---|---|
| Number of years since graduation | −0.073 | −0.096–0.05 | < 0.001 |
| Ratio of animal health technicians to veterinarians exceeds 0.5 | 0.42 | 0.004–0.84 | 0.048 |
Adjusted R2 = 0.13
Figure 2.
Path diagram showing relationship among factors affecting postincisional analgesic use by Canadian veterinarians. Coefficients on arrows leading to pain perception are linear regression coefficients; all others are odds ratios (OR).
aWestern College of Veterinary Medicine: OR = 3.1 Faculté de médecine vétérinaire, Université de Montréal: OR = 3.3
bWestern College of Veterinary Medicine: OR = 0.35 Faculté de médecine vétérinaire, Université de Montréal: OR = 0.34
Discussion
The results reflect postincisional analgesic usage following feline and canine OVH, among participating veterinarians, in 2001. A discussion of the generalizability of the survey’s findings is given in the preceding paper (2). Although the 1994 study (1) examined analgesic use for abdominal surgeries other than OVH, some predictors of analgesic usage were common to both studies: the veterinarian’s maximum level of concern about negative aspects of opioid use (butorphanol, in 2001), and the veterinarian’s perception of pain. The new explanatory variable in 2001 was school of graduation (Table 2). Predictors of pain perception common to both studies were year of graduation, and employment of AHTs (1); however, these explained little of the variability in the pain data (as reflected by the low R2), probably because of the subjectivity of pain assessment. Pain scores assigned by using clinical judgement are likely to be more variable and less accurate than those assigned by using a validated pain assessment tool, if one were available. The roles of all the risk factors identified in this study are now discussed.
Maximum level of concern about the negative aspects of butorphanol use may be said not to be important in future efforts to encourage veterinarians to provide postincisional analgesia for OVH, for 2 reasons. First, butorphanol is a weak analgesic with a very short duration of action (2 h) (4); the drug has been shown to be less effective than meloxicam for postoperative use in dogs undergoing OVH (5). Second, the most commonly cited issue of maximum concern was, “The high frequency of dosing outweighs the benefits (of using butorphanol).” Owing to this limitation of butorphanol, NSAIDs are preferable for postincisional pain management of OVH (5). However, few nonusers gave NSAIDs, even though concerns about negative effects of NSAIDs were not significant risk factors for nonusage.
Pain perception was a strong predictor of analgesic use, and year of graduation was a predictor for pain perception, although school of graduation was not (Table 4, Figure 2). This suggests that more recent graduates tended to rate pain more highly than did graduates of longer standing, regardless of the school attended. This may, in turn, reflect increasing societal concern for animal suffering, and greater current emphasis on pain management at all the veterinary schools. However, the lack of a detectable association between school attended and pain perception is similar to the findings among final-year veterinary students in the United Kingdom (6).
The employment of AHTs was also a predictor for pain perception; this suggests an effective working relationship between veterinarians and their AHTs. While graduates from FMV and WCVM were less likely to be analgesic users, they were more likely to work in practices with at least 1 AHT per 2 veterinarians; this offset the negative effect of school of graduation. If there were fewer AHTs per veterinarian in those practices, the graduates might have been even less likely to be analgesic users. It is not clear why those graduates tended to work in practices with a high ratio of AHTs to veterinarians.
Unlike in 1994, there was no significant difference between male and female veterinarians in their perception of the pain caused by surgery. This is a positive finding, particularly because the mean pain rating for OVH in 2001 was approximately 30% higher than that in 1994 (2,7), and because approximately twice as many animals received postincisional analgesics for OVH in 2001 as received them for other abdominal surgery in 1994 (2,7). These data suggest that, in comparison with 1994, increasing numbers of Canadian veterinarians are doing more to prevent pain following abdominal surgeries in dogs and cats.
The direct effect of school of graduation on analgesic use is difficult to interpret, but might reflect differences in teaching programs or, perhaps less likely, a direct effect of school or regional culture. A direct effect of school might come about if veterinary students tend to follow the example of faculty more than other clinical staff: in that case, the attitudes and analgesic practices of faculty at the different schools might be expected to affect the analgesic use of graduating veterinarians. A retrospective study at North Carolina State University veterinary teaching hospital regarding management of very painful surgeries found that faculty tended to treat postoperative pain less aggressively than did interns and residents (8). A survey of the attitudes of students and clinical faculty at Colorado State University’s veterinary teaching hospital in 1996 suggested that 4th-year veterinary students and faculty were less likely than students of earlier years to give postoperative analgesics following certain surgeries, but OVH was not examined (9). The implications of both studies were limited by multiplicity (multiple statistical comparisons) (10). An effect of region might also be expected to contribute to the association between school of graduation and analgesic use: veterinary students generally attend the school in their region; therefore, school may be a marker for the regional culture, which, in turn, may affect analgesic usage.
The role in analgesic use of the veterinarian’s perception of the pain caused by surgery bears further examination. In our study, 1 respondent commented that pain is over-rated and another that it is underrated, indicating different beliefs within the profession about the significance of perioperative pain, as was also reported in a survey of veterinarians in Colorado (response rate, 31%) (11). In pediatric medicine, a persuasive case has been made against allowing personal beliefs about pain management to prevent “optimal recognition and treatment of pain for all children” (12).
Our survey did not examine risk factors such as attitudes of colleagues, particularly employers; practice policy; and respondents’ perception of pet owners’ willingness to pay for analgesic medication. However, respondents’ comments indicated that these factors may have influenced their use of the drugs. For example, 2 respondents indicated the need for guidance on how to market optimal perioperative analgesia to pet owners. Two other respondents indicated that price was an obstacle to analgesic usage, in 1 case because neighboring clinics charged much less. A further 3 respondents indicated that owners were always willing to pay for perioperative analgesia. The marketing of analgesia to pet owners has been reviewed (13). However, the above comments about price point to different experiences within the profession, notwithstanding 2 surveys of pet owners that indicated price to be less important to owners than factors such as the veterinarian’s medical knowledge and interest in their animals’ wellbeing (14). Those data (14) may have been biased by social desirability or “faking good” biases (15), but, if valid, suggest that many or most pet owners might not oppose use of perioperative analgesics on the grounds of price.
A possible role of emotional self-defence in veterinary underuse of analgesics cannot be discounted: human health professionals are reported to underestimate children’s pain, as a way of coping with daily encounters with distressed children (16). In the case of dogs, behavioral and physiological data indicate that OVH causes pain (17,18), but more than half the respondents in our survey did not give analgesics following this surgery and 40% of these nonusers considered their knowledge of analgesia to be adequate. A further explanation for this apparent contradiction is that OVH can be performed very quickly, which helps to minimize postoperative pain (but does not eliminate it). The routine nature of OVH and the perception that the surgery is less painful than others (2) might influence decisions about analgesic use.
All analgesic nonusers indicated that OVH would cause pain if no analgesics were given in the first 24 h after surgery, but some nonusers may have perceived postincisional analgesia to be unnecessary if owners did not report that their animals were in pain on returning home. One respondent, who worked in an emergency clinic, reported seeing 6 to 8 animals per month that had undergone elective surgeries, including OVH, and were experiencing postoperative pain, but whose owners reported not to have been given take-home analgesic medications by their regular veterinarian. The incidents illustrate that failure to provide adequate analgesia can result in avoidable distress for animals and cost for their owners.
While the difficulty in assessing pain is an understandable reason for any tendency to underuse analgesic drugs, the difficulty should not necessitate nonuse in any animal. If veterinarians have difficulty in assessing pain and do not give perioperative analgesics because they perceive that an animal does not need them, some or many owners are likely to have similar difficulties. However, in a nonrandomized survey of 911 veterinarians from large and small animal practice in Finland, 57% of respondents disagreed with the statement that “Owners actively insist on analgesics for their animals” (19). In the Colorado survey (all members of the Colorado Veterinary Medical Association), 76% of respondents reported that fewer than 50% of their clients “expressed concern about postoperative pain in their animals” (11). Those findings suggest that some owners may not know to ask about analgesia; or that they may assume that their veterinarian has already done all that can be done to manage any postoperative pain; or that they may not recognize signs of pain in their animals. Whatever the case, analgesic drugs are indicated whenever a procedure may cause pain (20,21).
The most important way to increase perioperative analgesic usage by veterinarians may be a valid and reliable means of assessing pain. Our results indicate that, as in 1994 (1), being a recent graduate and working in a practice that employed a relatively large number of AHTs increased the likelihood of individual veterinarians being analgesic users. However, these elements cannot be modified easily and are therefore of little help in increasing current analgesic usage. Continuing education is more feasible and would help to ensure that veterinarians use the most appropriate perioperative analgesic drugs, and avoid overreliance on weak analgesic opioids such as butorphanol. In our study, lectures or seminars at the provincial level, and review articles in journals were the preferred routes of continuing education (2). Client education is also indicated (22), as is practical guidance on the promotion of analgesic usage to pet owners. Also, veterinary clinical faculty should ensure that pain management is always emphasized, and the topic should be a subject in its own right in the curriculum (21). A similar approach should be taken in AHT training. Future surveys would help the profession to monitor its progress in these regards, and the response rate in our survey indicates that the majority are interested in such evaluation. CVJ
Footnotes
This research was funded by a grant from the Sir James Dunn Animal Welfare Centre, Atlantic Veterinary College, University of Prince Edward Island.
References
- 1.Dohoo SE, Dohoo IR. Factors influencing the postoperative use of analgesics in dogs and cats by Canadian veterinarians. Can Vet J. 1996;37:552–555. [PMC free article] [PubMed] [Google Scholar]
- 2.Hewson CJ, Dohoo IR, Lemke KA. Perioperative use of analgesics in dogs and cats by Canadian veterinarians in 2001. Can Vet J 2006 (in press). [PMC free article] [PubMed]
- 3.Dohoo I, Martin W, Stryhn H. Veterinary Epidemiologic Research. Charlottetown: AVC Inc., 2003:273–366.
- 4.Mathews KA. Pain assessment and general approach to management. Vet Clinics North Am Small Anim Pract. 2000;30:729–755. doi: 10.1016/s0195-5616(08)70004-4. [DOI] [PubMed] [Google Scholar]
- 5.Caulkett N, Read M, Fowler D, Waldner C. A comparison of the analgesic effects of butorphanol with those of meloxicam after elective OVH in dogs. Can Vet J. 2003;44:565–570. [PMC free article] [PubMed] [Google Scholar]
- 6.Paul ES, Podberscek AL. students’ attitudes towards animal welfare. . Vet Rec. 2000;146:269–272. doi: 10.1136/vr.146.10.269. [DOI] [PubMed] [Google Scholar]
- 7.Dohoo SE, Dohoo IR. Postoperative use of analgesics in dogs and cats by Canadian veterinarians. Can Vet J. 1996;37:546–551. [PMC free article] [PubMed] [Google Scholar]
- 8.Hansen B, Hardie E. Prescription and use of analgesics in dogs and cats in a veterinary teaching hospital: 258 cases (1983–1989) J Am Vet Med Assoc. 1993;202:1485–1494. [PubMed] [Google Scholar]
- 9.Hellyer PW, Frederick C, Lacy M, Salman MD, Wagner, AE Attitudes of veterinary medical students, house officers, clinical faculty and staff towards pain management in animals. J Am Vet Med Assoc. 1999;214:238 –244. [PubMed] [Google Scholar]
- 10.Bender R, Lange S. Adjusting for multiple testing — when and how? J Clin Epidemiol. 2001;54:343–349. doi: 10.1016/s0895-4356(00)00314-0. [DOI] [PubMed] [Google Scholar]
- 11.Wagner AE, Hellyer PW. Survey of anesthesia techniques and concerns in private veterinary practice. J Am Vet Med Assoc. 2000;217:1652–1657. doi: 10.2460/javma.2000.217.1652. [DOI] [PubMed] [Google Scholar]
- 12.Hagan JF, Coleman WL, Foy JM, et al. The assessment and management of acute pain in infants, children and adolescents. Pediatrics. 2001;108:793–797. doi: 10.1542/peds.108.3.793. [DOI] [PubMed] [Google Scholar]
- 13.Gaynor JA. Pain management: Ensuring a fair profit from a valuable service. Vet Med. 1999;94:358–361. [Google Scholar]
- 14.Osborne D. Relationships more important than price. Proc 1st Int Conf Commun Vet Med, Niagara-on-the-Lake, Ontario June 13–16, 2004:49–51.
- 15.Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to their Development and Use. New York: Oxford Univ Pr, 1995:72–75.
- 16.Byrne A, Morton J, Salmon P. Defending against patients’ pain. A qualitative analysis of nurses’ responses to children’s postoperative pain. J Psychosom Res. 2001;50:69–76. doi: 10.1016/s0022-3999(00)00207-5. [DOI] [PubMed] [Google Scholar]
- 17.Hardie EM, Hansen BD, Carroll GS. Behaviour after ovariohysterectomy in the dog: what’s normal? Appl Anim Behav Sci. 1997;51:111–128. [Google Scholar]
- 18.Hansen BD, Hardie EM, Carroll GS. Physiological measures after ovariohysterectomy in dogs: what’s normal? Appl Anim Behav Sci. 1995;51:101–109. [Google Scholar]
- 19.Raekallio J, Heinonen KM, Kuussaari J, Vainio O. Pain alleviation in animals: attitudes and practices of Finnish veterinarians. Vet J. 2003;165:131–135. doi: 10.1016/s1090-0233(02)00186-7. [DOI] [PubMed] [Google Scholar]
- 20.ACVA American College of Veterinary Anesthesiologists’ position paper on the treatment of pain in animals. J Am Vet Med Assoc. 1998;213:628–630. [PubMed] [Google Scholar]
- 21.Short CE. Management of Animal Pain: A Course Syllabus on Basic Concepts and Clinical Applications. University of Tennessee, Center for the Management of Animal Pain, July 2001. Available from: College of Veterinary Medicine, University of Tennessee, Knoxville, Tennessee 37996–4550 USA.
- 22.Flecknell PA, Roughan JV. Assessing pain in animals — putting research into practice. Anim Welfare. 2004;13:S71–75. [Google Scholar]