Abstract
Objectives. This study examined sociodemographic and psychosocial factors that predict survival among parents living with HIV.
Methods. Parents with HIV (n = 307) were recruited from 1993 to 1995 in New York City and repeatedly assessed. Survival was monitored among the sample (81% mothers; 45% Latino, 34% African American).
Results. Over a median period of 28 months (range = 0–53 months), 44% (n = 135) of the parents died. Having an AIDS diagnosis and being African American were associated with earlier death. Sex, age, and financial status were not related to survival. Parents who survived had initially higher levels of anxiety that decreased over time; in contrast, parents who died reported initially lower, but constant, levels of anxiety over time. After HIV diagnostic status was controlled for, it was found that parents who reported having more children, using a coping style of seeking social support, and being sexually active at baseline survived longer.
Conclusions. The counterintuitive findings raise hypotheses regarding the role of change and responsibilities in the survival of parents with HIV.
Increasing numbers of women are being infected with HIV,1 resulting in substantially higher numbers of infected parents.2–4 Some factors found to predict survival in men5 also predict survival in women; for example, physical health status predicts survival in both men and women.6,7 In particular, a high CD4 count appears to be the best correlate of increased survival, and older age at diagnosis is linked to an earlier death.8–11 Existing studies have not found sociodemographic factors such as sex9 and ethnicity10 to be associated with survival. Unlike the findings for sociodemographic predictors of survival, the psychosocial factors associated with disease progression have been less clear and have been examined primarily among gay men. The goal of this study was to examine survival and its predictors over time among a cohort of parents living with HIV (predominantly African American and Latino), including factors previously found to be related to survival among HIV-seropositive gay men.
Clinicians12 and patients13 expect psychosocial factors to influence the time to death from AIDS. Only one factor, having a realistic acceptance of one's disease state, has been directly linked to an earlier death.14 Psychoneuroimmunologists have predicted that depression impairs immune function,15 possibly leading to an earlier death; however, the findings have been mixed. In one study of survival among gay, HIV-infected men, depression was unrelated to survival,16 yet with a similar sample and the same assessment measure (i.e., the Center for Epidemiologic Studies Depression Scale), depression was related to survival.17 Depression has also been associated with functional health status18 and disease progression.19 Long-term survivors of HIV perceive that their positive attitudes and active styles of coping with stressful events influence their survival.20 However, observational reports of survivors note that these patients have closely monitored their medical conditions and that their medical care has been exceptionally well managed.21,22 Thus, it may be high levels of medical management of disease status, not the patients' positive psychosocial perceptions, that prolong survival.
Previous research has demonstrated that lifestyles and social support are related to survival with other life-threatening conditions (e.g., cancer23). With HIV, perceptions of social support19 and stressful life events24 have been related to disease progression, particularly end-stage disease,19 but not survival. As the proportion of women infected with HIV continues to grow,1 the impact of parents' lifestyle (substance use and sexual behavior) and social networks (e.g., their families, including children and partners) must be examined. Mothers are much more likely than fathers to be infected through heterosexual transmission,1 typically through partners who are injecting drug users. Fathers living with HIV were often infected through injection drug use (67%) or are bisexual (14%).25 Substance use may influence the survival of parents with HIV in several ways: those who are using drugs may be less adherent to medical regimens and medications,26 leading to an early death, or they may overdose and die early. Substances may also directly influence physical health. Thus, substance use is expected to be associated with decreased survival among parents.
Psychosocial and sociodemographic characteristics of the family may also influence survival. For example, among women with breast cancer, the psychosocial functioning of the family has been directly associated with survival.27 Children and sexual partners may provide an increased incentive for survival, as parents fulfill their responsibility to care for their families. Among gay men with AIDS,8,18 economic hardship has been associated with higher emotional distress, which in turn influences their health. Families affected by AIDS are often of low socioeconomic status,28 and providing for one's family is a substantial responsibility for parents. Characteristics of a family's living situation may be associated with survival.
This report examines survival among parents living with HIV and expands the range of predictors associated with survival. Factors previously linked to survival (physical health status, depression, emotional distress, and coping) were included in the study. However, parents' lifestyle (substance use and choices of sexual partners), children, and family support were also included.
METHODS
Participants
The present sample was recruited primarily to conduct an intervention study for parents living with HIV who had adolescent children. From August 1993 to March 1995, the Division of AIDS Services (DAS) in New York City received notification of all persons diagnosed with AIDS or advanced HIV who had financial need. A list of 429 eligible parents living with HIV was constructed; eligible parents were those who were alive during the recruitment period (155 died), who had at least 1 adolescent child (aged 11 to 18 years), and whose clinical social worker agreed to the parent's participation (32 denials). Among the 429 parents, 65 (15%) were untraceable and 46 (11%) refused to participate. Extreme illness and institutionalization (e.g., jail) resulted in an additional 11 (3%) not being recruited. Thus, 84% (307 of 364) of the traceable parents, or 72% of the total eligible parents (307 of 429), were successfully recruited. Families who spoke only Spanish (3%) were recruited and assessed in Spanish. As of June 30, 1998, this sample was followed up for a median of 28 months (range = 0–53 months) after their entry into the study.
Procedures
Institutional review board approval was obtained from Columbia University, the University of California at Los Angeles, and the Human Resource Administration of New York City. Case managers of the DAS secured consent for contact by university-based field interviewers, and voluntary informed consent was then secured. Parents were assured that nonparticipation would not affect service delivery or eligibility within the DAS.
The parents were interviewed in their homes for 1.5 to 3 hours by interviewers using laptop computers; the interviewers were typically African American or Latino (66%) graduate students, social workers, or health educators. All interviewers received 40 hours of training from experienced supervisors with PhD degrees; the training covered interviewing, ethics, confidentiality, child abuse, emergency crisis protocols, and HIV/AIDS. All interviews were audiotaped, and a randomly selected portion of the tapes was monitored for quality assurance on an ongoing basis.
Parents were assessed at the time of recruitment, at 3-month intervals over the next 2 years, and at 6-month intervals from 2 years to 5 years after recruitment. At least 95% were reassessed at least once annually; the follow-up rate at 2 years was 90%.
Assessments
The interviews covered each of the following domains.
Sociodemographic characteristics.
For each participant, we assessed age, sex, ethnicity, educational level, receipt of government entitlements, financial condition (very poor, poor, having the necessities, comfortable), number of children in the household, and relationship status (married, living with partner, dating).
HIV diagnostic status and physical health.
Participants self-reported their HIV diagnostic status as AIDS, HIV with symptoms (symptomatic), or HIV without symptoms (asymptomatic). In addition, their CD4 counts were reported on a measure previously demonstrated to have high reliability (r = 0.85) between self-reports of CD4 and medical chart review.29 The correlation coefficient between self-reported HIV diagnostic category and CD4 counts was 0.37 (P < .001).
HIV-related risk acts.
We assessed lifetime and current (previous 3 months) sexual risk by using reports of (1) the number of sexual partners with whom the parent engaged in vaginal, oral, or anal intercourse; (2) the number of unprotected encounters of vaginal, oral, or anal intercourse; and (3) the proportion of protected sex acts (acts were categorized as “never using a condom,” “sometimes using a condom,” or “always and consistently using a condom”) for the individual's lifetime and over the previous 3 months.
We assessed substance use for the lifetime and the previous 3 months, using street names for cigarettes, alcohol, marijuana, crack, cocaine, injection drug use, heroin, barbiturates, inhalants, hallucinogens, and methamphetamine. Lifetime and current use of hard drugs was defined as having used any drug other than marijuana. Injection drug use also was reported.
Emotional distress.
The Brief Symptom Inventory30 was administered to assess overall emotional distress. The 53-item scale provides 1 overall summary score of symptoms of emotional distress (Cronbach a = .84) and 2 primary symptom subscales for depression (a = .94) and anxiety (a = .92). Participants reported the degree of distress for each symptom during the previous week on a scale of 0 (“not at all”) to 4 (“extremely”).
Coping with illness.
The Coping With Illness Questionnaire31 (revised by D. A. Murphy, M. J. Rotheram-Borus, and W. Marelich; unpublished data, 1999) consists of 40 items rated on a scale of 1 (never) to 5 (always). Seven reliable (a ranging from .76 to .89) styles for dealing with illness are generated from these ratings, each with an eigenvalue greater than 1, indicating that it is a distinct factor (range = 2.12–7.94): taking positive actions (e.g., seeking information about a conflict), self-destructive escape (e.g., using substances when depressed), passive problem-solving (e.g., avoiding others when in conflict), depressive (e.g., feeling blue but not acting), spiritual hope (e.g., praying when stressed), seeking social support, and denial (e.g., acting as if no problem exists).
Time to Death
Family members reported the date of death of the parent, which was confirmed by the New York State Department of Records. When discrepancies occurred, the date in the New York State Records was used as the date of death.
Statistics
Descriptive statistics were conducted on data obtained at the baseline interview. Parents who were still alive at analysis were censored on June 30, 1998, but those who were lost to follow-up were censored at the last interview date before June 1998. The Kaplan–Meier method was used for estimating the cumulative survival probabilities. The log-rank test was used for comparison among survival curves. Cox proportional hazards models were used to describe the unadjusted effects for each of the variables listed in Table 1 ▶ (e.g., sex, age, and education) on survival. The relative risks of death were computed with 95% confidence intervals, and the Wald test was used to examine the significance of each predictor variable over time from baseline to death. If the confidence interval includes “1,” the univariate predictor is nonsignificant at the P > .05 level. After the univariate analyses were conducted, the sustainability of the effects in a multivariate analysis was examined with stepwise Cox proportional hazards regression. This regression examined the potential predictors of survival simultaneously, using a P < .05 level in the univariate analyses as the level for inclusion in the multivariate analysis. In the multivariate analysis, HIV status was classified into 2 categories: “with AIDS” and “without AIDS” (i.e., symptomatic and asymptomatic combined).
TABLE 1—
Results of the Univariate Analyses Showing the Estimated Relative Risk of Death and the 95% Confidence Interval Levels for Each Predictor Variable Over Time From Baseline to Death
| Predictor | Estimated Relative Risk | 95% Confidence Interval |
| Intervention condition (reference: control) | 1.154 | 0.823, 1.617 |
| HIV status (reference: asymptomatic) | ||
| Symptomatic | 1.270 | 0.744, 2.169 |
| AIDS | 1.949*** | 1.155, 3.291 |
| Race/ethnicity (reference: African American) | ||
| Latino | 0.604*** | 0.415, 0.880 |
| White | 0.846 | 0.485, 1.474 |
| Other | 0.522* | 0.266, 1.024 |
| No. of children | 0.887*** | 0.788, 0.999 |
| Education: at least high school diploma (reference: less than high school) | 1.433** | 1.014, 2.026 |
| Female | 1.199 | 0.795, 1.809 |
| Age, per-year increase | 1.005 | 0.977, 1.034 |
| Financial status (reference: very poor) | ||
| Poor | 0.932 | 0.569, 1.527 |
| Has the necessities | 1.280 | 0.781, 2.096 |
| Comfortable | 1.509 | 0.897, 2.538 |
| Substance use, lifetime | ||
| Alcohol (reference: no use) | 0.877 | 0.570, 1.348 |
| Marijuana (reference: no use) | 1.237 | 0.844, 1.815 |
| Hard drugs (reference: no use) | 0.674** | 0.475, 0.955 |
| Injected drugs (reference: no use) | 0.933 | 0.653, 1.333 |
| Substance use, previous 3 months | ||
| Alcohol (reference: no use) | 0.888 | 0.610, 1.292 |
| Marijuana (reference: no use) | 0.881 | 0.536, 1.447 |
| Hard drugs (reference: no use) | 0.942 | 0.591, 1.500 |
| Injected drugs (reference: no use) | 0.570 | 0.233, 1.394 |
| Sexual behavior, previous 3 months | ||
| Abstinent (reference: yes) | 0.622*** | 0.435, 0.889 |
| No. of sexual partners | 1.002 | 0.828, 1.213 |
| Coping | ||
| Spiritual hope | 1.066 | 0.908, 1.251 |
| Positive action | 0.937 | 0.789, 1.112 |
| Passive problem solving | 0.872 | 0.733, 1.039 |
| Nondisclosure | 0.986 | 0.818, 1.189 |
| Social support | 0.773*** | 0.641, 0.932 |
| Depression withdrawal | 0.832 | 0.646, 1.073 |
| Self-destructive escape | 0.886 | 0.632, 1.244 |
| Brief Symptom Inventory | ||
| Total score | 0.818* | 0.647, 1.034 |
| Depression score | 0.834* | 0.691, 1.006 |
| Anxiety score | 0.792** | 0.647, 0.969 |
*P < .10; **P < .05; ***P < .01.
To further explicate the finding on emotional distress, the trends in Brief Symptom Inventory scores over time were compared between the parents who survived and the parents who did not. Repeated-measures random-effects models were used to examine differences in the Brief Symptom Inventory scores over time.
RESULTS
Description of the Sample
The parents' mean age was 38 years (SD = 5.6), with a range of 25 to 70 years. Most (81%) were mothers; 45% were Latino, 34% African American, 11% White, and 10% of other ethnicities. Almost all parents (94%) were living with their children; the remainder were only temporarily separated from their children. Parents had a mean of 3.0 children (SD = 1.6), ranging in age from a few months to more than 18 years (mean = 13.2 years). While most were living with their children, only 27% (n = 81/303) were living with an adult partner at the time of recruitment (30% of these were spouses). More than half the cohort (53%) had completed high school, fewer than 10% had a regular job, and almost all participants (94%) were receiving 1 or more government entitlements when they entered the study. Government entitlements included Medicaid, public assistance, supplemental security income, Social Security disability, food stamps, Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), DAS housing, Social Security survivor benefits, and Department of Veterans Affairs benefits.
Parents eligible for recruitment were already enrolled in the DAS, which supposedly required a diagnosis of advanced HIV disease or AIDS as an entry criterion. Yet, only 40% (n = 120/301) of the parents reported that they had an AIDS diagnosis; 42% (n = 126/301) had AIDS-related symptoms (symptomatic), and 18% (n = 55/301) had no AIDS-related symptoms (asymptomatic). Not all participants reported their CD4 counts. For the total sample, 81% (n = 250) reported the most current CD4 counts at entry (mean = 185.5 μL, SD = 175.1 μL); data were collected before the DAS began requiring, on the basis of the Center for Disease Control and Prevention's definition of AIDS, that participants with a CD4 count of 200μL be classified as having AIDS. Among 45 asymptomatic parents who reported their CD4 counts, 24 (53%) had CD4 counts of between 200μL and 500μL, and 19 (42%) had CD4 counts below 200μL.
Most parents had engaged in multiple high-risk behaviors over their lifetime, including the use of alcohol (81%), marijuana (69%), hard drugs (67%), and injection drugs (37%). At the time they were recruited into the study, parents' reports of their recent substance use (i.e., over the previous 3 months) were substantially lower: only 16% used at least 1 illegal drug other than marijuana, and only 6% injected drugs. Alcohol was used by only 30%, and only 14% reported marijuana use.
More than half of the parents (57%) had had 6 or more sex partners in their lifetime (median = 7, mean = 67.23, SD = 297.73). Only 1% had had only 1 sexual partner over their lifetime. Within the 3 months before recruitment, 57% of the parents were abstinent. Among the sexually active parents, 92% had only 1 partner (mean = 1.3, SD = 1.5). For about half (52%) of this sexual activity, condoms were used. At the time of recruitment, parents' reports of recent behaviors indicated 6 subgroups: (1) 39% abstained from both substance use and sex; (2) 13% abstained from substance use and used condoms for 100% of sexual acts; (3) 10% abstained from substance use but had sexual intercourse without using condoms; (4) 18% abstained from sex but used alcohol, drugs, or both; (5) 9% used condoms for 100% of sexual acts but used alcohol, drugs, or both; (6) 11% used substances and were having sexual intercourse without using condoms.
Parents' style of coping with problems is described by 7 factors. When the number of items for each style of coping was adjusted for, spiritual hope and positive action were the most common styles; self-destructive escape was used least often. Assessment of emotional distress by the Brief Symptom Inventory (overall mean score = 1.0, SD = 0.7) indicates that the parents were comparable to a sample of psychiatric outpatients in their levels of distress.30 Similarly, subscale scores for depression (mean = 1.1, SD = 0.9) and anxiety (mean = 0.9, SD = 0.9) were similar to those in reports of outpatients.
Factors Associated With Survival
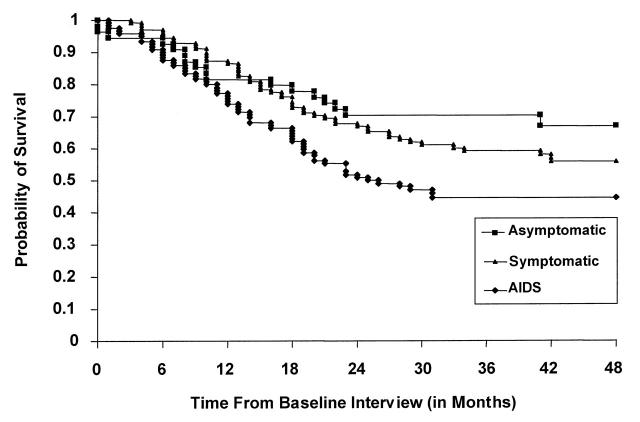
As of June 1998, 135 (44%) of the parents had died. Half of the parents had been randomized to receive an intervention and half received standard care; the intervention was not associated with survival. Figure 1 ▶ shows the Kaplan–Meier survival curves stratified by diagnostic status. At each point in time, the Kaplan–Meier curve reflects the probability of survival until that point in time. For example, at 2 years, those parents with an AIDS diagnosis at the baseline interview had a 51% probability of survival; in contrast, those who were asymptomatic at the baseline interview had a 70% probability of survival.
FIGURE 1—
Kaplan–Meier survival curves for parents of each HIV diagnostic status (asymptomatic, symptomatic, AIDS) at recruitment.
Table 1 ▶ summarizes the univariate analyses of the sociodemographic, psychosocial, and lifestyle variables associated with survival. Factors that were related to longer survival were being asymptomatic for HIV, Latino ethnicity, having had more children, being more educated, having used hard drugs in one's lifetime, having a current sexual partner, and more frequently coping with the illness by seeking social support. Current substance use was not related to survival.
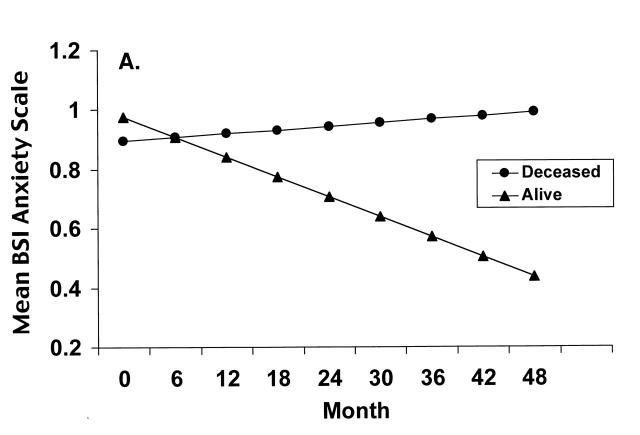
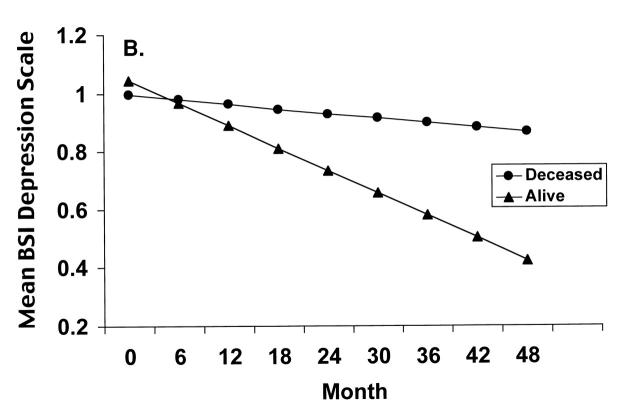
We also examined the relation between emotional distress and time to death with univariate Cox proportional hazards models. The 3 baseline measures of emotional distress on the Brief Symptom Inventory (total scale, depression subscale, and anxiety subscale) were examined; the anxiety subscale at the baseline interview was significantly related to the time to death (P = .043), and the depression subscale tended to be significant (P = .057). Higher anxiety subscale scores at baseline were associated with significantly later death, a counterintuitive finding. Similarly, higher depression subscale scores tended to be associated with later death, a second unexpected finding.
These findings required closer examination of the relation between death and emotional distress. Therefore, we conducted repeated-measures regressions examining changes in anxiety over time for those who survived and those who did not. We used the SAS PROC MIXED procedure (SAS Institute, Inc, Cary, NC), which is a general mixed-model regression program. In the mixed models, the anxiety scores after death were considered as missing data. Similar analysis was conducted for depression, and these regression lines are plotted in Figure 2 ▶. The slopes of the anxiety scores monitored over time were significantly different for those who survived and those who did not survive (P = .01); similarly, the slopes of the depression scores monitored over time differed significantly between the 2 groups (P = .046). As can be seen, the level of anxiety among those who survived decreased over time, in contrast to a relatively stable level of anxiety over time among those who did not survive. A similar pattern was found for reports of depression over time among those who survived and those who did not.
FIGURE 2—
Levels of anxiety (A) and depression (B), monitored over time since recruitment, among parents with HIV who lived and among those who died during the study.
Table 2 ▶ presents a summary of the stepwise Cox multivariate modeling process that included all factors significantly associated with survival in the univariate analyses (P < .05). In the final multivariate proportional hazards model, parents who were diagnosed with AIDS before entering the study were 1.6 times more likely to die than those who were not. Parents who were not African American or who had more children, a recent sexual partner, or a coping style of seeking support were more likely to survive.
TABLE 2—
Results of Multivariate Cox Proportional Model Showing the Significant Predictor Variables (P < .05) for the Estimated Relative Risk of Death and the 95% Confidence Interval Levels Over Time From Baseline to Death
| Predictor | Estimated Relative Risk | 95% Confidence Interval | P |
| Non–African American (reference: African American) | 0.568 | 0.400, 0.806 | .002 |
| Social support coping | 0.750 | 0.622, 0.905 | .003 |
| Has AIDS (reference: no AIDS) | 1.572 | 1.110, 2.227 | .011 |
| Currently sexually active (reference: abstinent ) | 0.646 | 0.450, 0.929 | .019 |
| No. of children | 0.874 | 0.773, 0.989 | .033 |
DISCUSSION
Most studies of survival have focused on gay men. In examining the survival of parents, some factors were found that were also found for gay men: physical health status was a significant predictor, and age was not related to survival. Subject's sex was also not related to survival.
In contrast to findings with male injection drug users recruited from 1988 to 1991 in New York City,10 being African American was associated with decreased survival among parents in the same city 5 years later. A nationally representative sample of persons living with HIV has demonstrated that African Americans and women receive a lower quality of care than other HIV-infected persons.32 In our sample, African Americans were better educated than Latinos. African Americans also reported significantly lower subscale scores on anxiety and depression than did parents of other ethnicities. The relationships between survival and education and between survival and emotional distress observed in the univariate analyses did not emerge in the multivariate analysis because of the relationship between ethnicity and these predictor variables. Further research must investigate whether factors such as access to or quality of care are related to decreased survival among African American parents.
Family factors, however, typically have not been examined in predictions of survival. In this study, parents with more children survived longer. Similarly, current sexual activity was also associated with increased survival. The relation between survival and social support is similar to findings for survival with cancer: high levels of social support are associated with survival.23 The finding of increased survival among parents with more children and a partner supports the importance of social support in mediating survival, similar to findings for persons with other terminal or chronic diseases.
There is, however, an alternative hypothesis regarding the increased survival of parents who had more children or who had a sexual partner. The more children parents have, the greater are their family responsibilities, and sexual partners often are associated with interpersonal responsibilities. Responsibility may be a factor associated with survival. Because our data are limited to indices of the number of persons living in a household, the responsibility hypothesis must be investigated in future research.
The relation between depression, anxiety, and survival, which was the most important finding in this study, was complex. Unexpectedly, the initial levels of anxiety were higher among those parents who survived, in contrast to levels of anxiety at the baseline interview among those who later died. Over time, however, the anxiety of those who survived decreased, while the initially lower levels of anxiety of those who died remained constant. A similar pattern was found for depression. This finding highlights the potential role of parents' mental health status in their survival and may explain the mechanism of increased survival previously reported among cancer patients.23
Longitudinal studies provide important information about predictors of survival. In this study, survival was predicted by the change in levels of emotional distress, not the level at the point of recruitment.17 Parents' lifetime hard drug use, not current use, was associated with longer survival. About 28% had stopped injecting drugs and more than 51% had stopped using marijuana. These are large changes. Additionally, parents are constantly challenged to adapt to their children's shifting needs and developmental capacities. Perhaps children actually help keep parents alive, not just young.
Acknowledgments
This paper was completed with the support of National Institute of Mental Health grant 1ROI MH49958-04.
We wish to thank the staff of the Family Center/MHRA and Housing Works, and the parents, caregivers, and adolescents who participated in the study. We also thank Coleen Cantwell, Tri Cisek, Barbara Draimin, Ernesto De Guzman, Jennifer Elliott, Earl Foss, Carlos Garcia, Marya Gwadz, Nionne James, Kris Langabeer, Julie Lehane, Patrice Lewis, Javelle McElhaney, Sheldon McLeod, Sutherland Miller, Tanko Mohammed, Sanna Moore, Fred Muench, Wilfredo Rosado-Ordonez, Laura Rosen, Marion Riedel, Martha Saab, Karen Schlichting, Phyllis Sena, and Karen Wyche.
This study was approved by the University of California–Los Angeles General Campus Human Subjects Protection Committee, and participants gave their informed consent.
M. Lee designed the analytic plan for the paper, conducted and supervised the data analysis, analyzed the data, and wrote the Results section and the data analysis portion of the Methods section. M. J. Rotheram-Borus designed the study, wrote the first draft of the paper, and supervised analysis. Both authors revised and edited all drafts of the paper.
Peer Reviewed
References
- 1.Centers for Disease Control and Prevention. US HIV and AIDS cases reported through June 1999. HIV AIDS Surveill Rep. 1999;11:1–42. [Google Scholar]
- 2.Mok J, Cooper S. The needs of children whose mothers have HIV infection. Arch Dis Child. 1997;77:483–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black MM, Nair P, Kight C, Wachtel R, Roby P, Schuler M. Parenting and early development among children of drug-abusing women: effects of home intervention. Pediatrics. 1994;94:440–448. [PubMed] [Google Scholar]
- 4.Schable B, Diaz T, Chu SY, et al. Who are the primary caretakers of children born to HIV-infected mothers? Results from a multistate surveillance project. Pediatrics. 1995;95:511–515. [PubMed] [Google Scholar]
- 5.Ohno-Machado L, Musen MA. A comparison of two computer-based prognostic systems for AIDS. Proc Annu Symp Comp Appl Med Care. 1995:737–741. [PMC free article] [PubMed]
- 6.Laine C, Markson LE, McKee LJ, Hauck WW, Fanning TR, Turner BJ. The relationship of clinic experience with advanced HIV and survival of women with AIDS. AIDS. 1998;12:417–424. [DOI] [PubMed] [Google Scholar]
- 7.Fleishman JA, Crystal S. Functional status transitions and survival in HIV disease: evidence from the AIDS Costs and Service Utilization Survey. Med Care. 1998;36:533–543. [DOI] [PubMed] [Google Scholar]
- 8.Mocroft A, Johnson M, Phillips A. Factors affecting survival in patients with acquired immunodeficiency syndrome. AIDS. 1996;10:1057–1065. [PubMed] [Google Scholar]
- 9.Vella S, Giuliano M, Floridia M, et al. Effect of sex, age and transmission category on the progression to AIDS and survival of zidovudine-treated symptomatic patients. AIDS. 1995;9:51–56. [DOI] [PubMed] [Google Scholar]
- 10.Brown LS, Siddiqui NS, Chu AF. Natural history of HIV-1 infection and predictors of survival in a cohort of HIV-1 seropositive injecting drug users. J Natl Med Assoc. 1996;88:37–42. [PMC free article] [PubMed] [Google Scholar]
- 11.Spino C, Kahn JO, Dolin R, Phair JP. Predictors of survival in HIV-infected persons with 50 or fewer CD4 cells/mm3. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;15:346–355. [DOI] [PubMed] [Google Scholar]
- 12.Lea A. Women with HIV and their burden of caring. Health Care Women Int. 1994;15:489–501. [DOI] [PubMed] [Google Scholar]
- 13.Troop M, Easterbrook P, Thornton S, Flynn R, Gazzard B, Catalan J. Reasons given by patients for “non-progression” in HIV infection. AIDS Care. 1997;9:133–142. [DOI] [PubMed] [Google Scholar]
- 14.Reed GM, Kemeny ME, Taylor SE, Wang H-YJ, Visscher BR. Realistic acceptance as a predictor of decreased survival time in gay men with AIDS. Health Psychol. 1994;13:299–307. [DOI] [PubMed] [Google Scholar]
- 15.Schneiderman N, McCabe P, Baum A, eds. Stress and Disease Processes. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992.
- 16.Lyketsos CG, Hoover DR, Guccione M. Depression and survival among HIV-infected persons [letter]. JAMA. 1996;275:35–36. [DOI] [PubMed] [Google Scholar]
- 17.Mayne TJ, Vittinghoff E, Chesney MA, Barrett DC, Coates TJ. Depressive affect and survival among gay and bisexual men infected with HIV. Arch Intern Med. 1996;156:2233–2238. [PubMed] [Google Scholar]
- 18.Palombi L, Mancinelli S, Liotta G, Narciso P, Marazzi MC. The impact of socio-economic factors, mental health and functional status on survival in a sample of AIDS patients. AIDS Care. 1997;9:671–680. [DOI] [PubMed] [Google Scholar]
- 19.Patterson TL, Shaw WS, Semple SJ, et al. Relationship of psychosocial factors to HIV disease progression. Ann Behav Med. 1996;18:30–39. [DOI] [PubMed] [Google Scholar]
- 20.Remien RH, Rabkin JG, Williams JB, Katoff L. Coping strategies and health beliefs of AIDS long-term survivors. Psychol Health. 1992;6:335–345. [Google Scholar]
- 21.Rabkin JG, Ferrando S. A “second-life” agenda: psychiatric research issues raised by protease inhibitor treatments for people with the human immunodeficiency virus or the acquired immunodeficiency syndrome. Arch Gen Psychiatry. 1997;54:1049–1053. [DOI] [PubMed] [Google Scholar]
- 22.Jue S. Psychosocial issues of AIDS long-term survivors. Fam Soc. 1994;75:324–332. [Google Scholar]
- 23.Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2:888–891. [DOI] [PubMed] [Google Scholar]
- 24.Evans DL, Leserman J, Perkins DO, et al. Severe life stress as a predictor of early disease progression in HIV infection. Am J Psychiatry. 1997;154:630–634. [DOI] [PubMed] [Google Scholar]
- 25.Lightfoot M, Robin L, Rotheram-Borus MJ, et al. Lifestyle choices of parents living with AIDS: differences in health behaviors and mental health. AIDS Behav. 2000;4:253–260. [Google Scholar]
- 26.Gwadz M, De Vogli R, Rotheram-Borus MJ, et al. Behavioral practices regarding combination therapies for HIV/AIDS. J Sex Educ Ther. 1999;24:81–88. [Google Scholar]
- 27.Weihs K, Reiss D. Family reorganization in response to cancer: a developmental perspective. In: Baider L, Cooper C, De-Nour A, eds. Cancer and the Family. Chichester, England: John Wiley & Sons; 1996:3–29.
- 28.Institute of Medicine. Reducing the Odds: Preventing Perinatal Transmission of HIV in the United States. Washington, DC: National Academy Press; 1999. [PubMed]
- 29.Murphy DA, Rotheram-Borus MJ, Joshi V. HIVinfected adolescent and adult perceptions of tuberculosis testing, knowledge and medication adherence in the USA. AIDS Care. 2000;12:59–63. [DOI] [PubMed] [Google Scholar]
- 30.Derogatis LR. Brief Symptom Inventory: Administration, Scoring, and Procedures Manual. 3rd ed. Minneapolis, Minn: National Computer Systems; 1993.
- 31.Namir S, Wolcott D, Fawzy F, Alumbaugh MJ. Coping with AIDS: psychological and health implications. J Appl Soc Psychol. 1987;17:309–328. [Google Scholar]
- 32.Shapiro MF, Morton SC, McCaffrey DF, et al. Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. JAMA. 1999;281:2305–2315. [DOI] [PubMed] [Google Scholar]