Abstract
Objectives. Health care reforms associated with managed care may adversely affect the health care safety net for disadvantaged populations. This study compared changes in health care use among poor and nonpoor individuals enrolled in managed care.
Methods. Data from 3 waves of a random community sample were collected on approximately 3000 adults. Changes in use of mental health services were assessed in a pretest–posttest, quasi-experimental design.
Results. Managed care increased use of specialty services among the nonpoor while maintaining the same level of use for the poor in the public sector.
Conclusions. Reallocation of mental health services may be a result of expanding Medicaid eligibility.
Concerns have been raised about the differential impact of managed mental health care on poor Medicaid populations.1,2 The poor tend to have more need of care3–5 but appear less successful in obtaining services from managed care organizations.6 Several investigators contend that low-income enrollees suffer access problems in managed care relative to those with conventional insurance,7,8 while others report a neutral9,10 or positive11 effect on access for the poor. As states' Medicaid programs enter managed care,12,13 there is a growing need to assess the effects on poor populations.
Recently, some states (such as Oregon and Tennessee) have broadened the reach of Medicaid programs beyond the very poor to the near poor and working populations in an attempt to provide insurance coverage for the uninsured population.14,15 Similarly, Puerto Rico initiated a health reform that enabled the medically indigent and those with incomes up to 200% of the federal definition of poverty to be included in a comprehensive managed health care plan (with pharmacy benefits, no co-pays, and no costs for private specialty care). Thus, nonpoor individuals without insurance who qualified under this exemption could also participate in the reform. In this report, we evaluate the impact of the reform on use of mental health services among the poor and nonpoor in Puerto Rico.
In 1994, Puerto Rico initiated a health care reform policy that dramatically altered the health care system that had operated since the 1960s, serving about half of the island's 3.6 million inhabitants. Dividing the island into 10 health regions, the government privatized public health facilities and instituted managed competition in a fixed health and mental health service package for public sector service recipients. The government solicited proposals from private insurers to provide managed health and mental health care for a fixed capitation rate but at no charge to eligible residents. Eligibility was based on residence in a reform area and the expanded income limits just noted. Members of the police force, veterans, and their families (who in the past had had limited health coverage) were also eligible.
Managed care services were initiated in 1 region in 1994 and in 2 regions each year thereafter. Less densely populated areas were selected for reform early, so reformed and unreformed regions remained in close proximity. The prequalification process for enrollees required proof of residency; thus, individuals in unreformed regions were unable to receive services in reformed regions.
Enrollees in the reformed regions were issued private health insurance cards that enabled them to access private health care services from providers contracting with the insurance company responsible for their region. As of 1997, 7 of 10 regions were reformed. Because of the phased introduction of reform, a third of the island's population remained within the traditional public health sector at the time of our study, yielding a comparison group of poor and nonpoor individuals residing in regions not yet subject to reform. People living in nonreformed regions continued to have free access to providers affiliated with the government-owned public health system, or, if they were privately insured, they were subject to the co-payments (typically $15–$18 per visit) of private health insurance.
In the case of public outpatient mental health services, individuals residing in unreformed regions continued to receive free services, typically provided by counselors, psychiatric nurses, or bachelor's-level therapists, in community mental health centers and drug detoxification centers. With the exception of a group of approximately 40 000 enrollees in 1 region, coverage for private mental health care in the population under reform was provided by behavioral health care companies (mostly those operating in the United States). Specialty providers contracted by the behavioral health care company supplied outpatient mental health, alcohol, and drug services to clients in reform. Only 1 insurer contracted with the community health centers to provide care for chronically ill patients. In 1997, these companies received between $3.00 and $3.50 per member per month in a capitation payment to cover mental health services.
METHODS
Data
Three waves of data from the Puerto Rico Mental Health Utilization Study were collected on a random islandwide probability sample of adults (aged 18–69 years in 1992) living in low-income census tracts in the reformed and unreformed regions of Puerto Rico. The sample has been described in more detail elsewhere.16–18 Total annual family income was used to designate people as poor or nonpoor. For each wave, the US Bureau of the Census definition of poverty for a family of 4 (2 adults and 2 children) was used to classify respondents as poor or nonpoor (1992: $14 654; 1993: $15 029; 1997: $16 276). Annual household incomes (without government assistance) in the sample ranged from $0 to $156 000, with a mean of $13 892.
Hot-deck-based imputation19 was used to assign annual household incomes to respondents with missing income values. Approximately 67% of respondents had household incomes below the federal poverty line. The remaining respondents were classified as nonpoor according to this criterion.
Eligible adults were identified in 4027 housing units, and enumeration was completed for 96.1% of these units (n = 3869 individuals). Standard Kish20 selection methods were then used in selecting 1 adult from each unit. The interview completion rate for this islandwide probability sample of the general population living in low-income areas was 90.6%, yielding 3504 completed face-to-face interviews at baseline (1992–1993).16 In wave 2 (1993–1994), 3263 respondents (93.1%) were reinterviewed, and in wave 3 (1996–1998), 2928 interviews were conducted (83.6%). The overall response rate (excluding deaths) for the 3 waves was 81.5%.
Measures
Formal mental health care use during the previous year was defined as use of the general health sector or the specialty sector for mental health problems. Specialty sector use was defined as treatment by a psychiatrist, psychologist, social worker, or counselor or treatment by a professional in a mental health setting (e.g., hospital psychiatric clinic).
Several covariates drawn from the literature21 on mental health care use were used as controls: age, sex, migration status, marital status, years of education, employment status, availability of private health insurance coverage, self-perception of mental health, self-perception of physical health, number of chronic physical illnesses, presence of physical incapacity, and level of need. Four potential responses (ranging from poor to excellent) were used in evaluating respondents' general perceptions of their physical health and mental health. Mental health need was based on 4 dimensions: level of psychologic distress, diagnosis of psychiatric disorders, functional impairment in role performance or severity of underlying illness, and current illicit drug use. Level of need was represented by 2 dummy variables, one indicating whether the respondent fulfilled criteria for definite need and the other indicating whether the respondent fulfilled criteria for probable need. Those unlikely to need mental health services constituted the reference group.
Statistical Analyses
The analyses compared changes in use of mental health services among the poor and nonpoor as a result of the introduction of managed care in Puerto Rico. First, for each of the 3 waves of data, we calculated unadjusted rates of formal mental health service use among poor and nonpoor individuals in the regions that were and were not reformed. Second, we conducted a logistic regression analysis that included covariates to control for other factors affecting mental health service use in addition to managed care. We used all valid responses in the 3 waves of data, for a total of 9626 observations.
In the logistic regression analysis, time trends were accounted for by dummy variables in the case of waves 2 and 3, with wave 1 as the reference category. Regional differences were accounted for by a dummy variable indicating whether respondents lived in a reform or nonreform region. Impact of managed care on use of mental health care was captured by a variable representing the interaction between wave 3 (post–managed care) and residence in a reform region. This interaction term assumed a value of 1 only in the reformed regions after the introduction of managed care.
We evaluated whether there were differential effects of managed care according to poverty level by including additional interaction terms. Our measure of managed care impact was itself an interaction term; thus, allowing for a differential effect by poverty status required that we include the full set of 2-way interactions as well as the 3-way interaction of time, region, and poverty status. All regression coefficients were estimated with standard errors via a Taylor series approximation.22
RESULTS
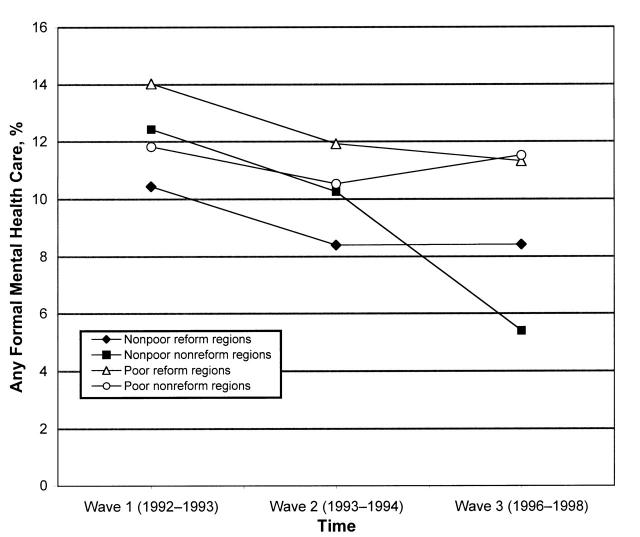
Figure 1 ▶ presents, for all 3 waves, percentages of mental health service use among poor and nonpoor individuals in reform and nonreform regions. Among the nonpoor, there was a drop in use between waves 1 and 2 in both reform and nonreform regions. This decreased rate was sustained in the nonreform regions but did not continue in the reform regions in wave 3 (after introduction of managed care). The rate of use of formal care among the nonpoor in nonreformed regions fell to 5.4% in wave 3, as compared with 12.4% in wave 1 and 10.3% in wave 2.
FIGURE 1—
Formal mental health care use, by poverty status: reformed and nonreformed regions, Puerto Rico, 1992–1998.
This decline in mental health service use appeared to be due to a decrease in specialty care (data not shown). Rates of use among the poor were roughly constant in the nonreform areas over the 3 waves. In the reform regions, rates of use fell steadily (from 14% to below 12%) across the 3 waves, but these differences were not statistically significant. We subsequently tested the statistical significance of the effect of reform in a regression context.
Results of logistic regression analyses of the probability of any formal use and of specialty use are presented in Table 1 ▶. Variables measuring waves 2 and 3 indicate that there were large and significant negative time trends in use. The effect of managed care on the nonpoor was positive and nearly significant in the case of any formal care, and the effect was positive and significant for specialty care. The 3.87 odds ratio in Table 1 ▶ for the nonpoor ¥ managed care interaction implies that managed care (vs non–managed care) was associated with a 300% higher rate of use of any specialty care among the nonpoor. The poor variable alone had no significant effect on the likelihood of use of either any mental health service or specialty services. However, the interaction of the managed care and poor variables was negative (but nonsignificant) in both regressions. This can be interpreted as a downward but nonsignificant trend in the probability of any mental health care or specialty care use among the poor under managed care.
TABLE 1—
Adjusted Odds Ratios for Any Mental Health Service Use and Specialty Use by Adults Living in Poor Areas: Puerto Rico, 1992–1998
| Any Mental Health Use | Specialty Use | |||
| Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | |
| Poor | 0.78 | 0.53, 1.15 | 0.86 | 0.52, 1.42 |
| Reform region | 0.91 | 0.61, 1.36 | 0.69 | 0.41, 1.14 |
| Wave 2 | 0.71 | 0.58, 0.87* | 0.74 | 0.61, 0.90* |
| Wave 3 | 0.36 | 0.18, 0.72* | 0.32 | 0.16, 0.62* |
| Nonpoor × managed care | 1.91 | 0.84, 4.32 | 3.87 | 1.72, 8.73* |
| Poor × managed care | 0.75 | 0.46, 1.24 | 0.86 | 0.51, 1.45 |
| Reform region × poor | 1.38 | 0.88, 2.15 | 1.58 | 0.89, 2.80 |
| Wave 3 × poor | 2.15 | 1.00, 4.58* | 2.59 | 1.29, 5.20* |
| Age, y | 0.99 | 0.98, 0.99* | 0.98 | 0.97, 0.99* |
| Female | 0.87 | 0.71, 1.07 | 0.67 | 0.53, 0.84* |
| Nonmigranta | 0.88 | 0.72, 1.07 | 0.87 | 0.68, 1.11 |
| Disrupted marriageb | 1.34 | 1.05, 1.70* | 1.25 | 0.93, 1.68 |
| Never married | 0.92 | 0.71, 1.20 | 1.03 | 0.76, 1.40 |
| Unemployed | 1.15 | 0.84, 1.58 | 1.31 | 0.90, 1.92 |
| Out of labor force | 1.84 | 1.45, 2.35* | 2.14 | 1.63, 2.80* |
| Years of education | 1.05 | 1.02, 1.08* | 1.05 | 1.02, 1.09* |
| Private insurance | 1.09 | 0.88, 1.34 | 1.10 | 0.87, 1.41 |
| Private insurance × managed care | 0.96 | 0.62, 1.47 | 1.00 | 0.63, 1.58 |
| Self-rated physical health fair or poorc | 1.12 | 0.88, 1.43 | 0.96 | 0.73, 1.26 |
| Self-rated mental health fair or poorc | 1.67 | 1.31, 2.14* | 2.22 | 1.70, 2.89* |
| Physical incapacityd | 1.70 | 1.37, 2.12* | 1.92 | 1.51, 2.44* |
| No. of chronic illnessese | 1.13 | 1.05, 1.21* | 1.08 | 1.01, 1.15* |
| Definite mental health problem | 4.26 | 3.40, 5.35* | 3.38 | 2.64, 4.32* |
| Probable mental health problem | 1.95 | 1.51, 2.52* | 1.72 | 1.28, 2.32* |
| Previous mental health service user | 8.48 | 6.99, 10.28* | 8.62 | 6.88, 10.79* |
aNonmigrant refers to someone living continuously on the island.
bDisrupted marriage means divorced, separated, or widowed, with married as the reference category.
cPhysical and mental health were self-rated with a 4-level response (excellent, good, fair, or poor).
dPhysical incapacity was evaluated by a single question asking whether the respondent had a physical incapacity or disability.
eNumber of chronic illnesses was a self-reported count of the following conditions: asthma, diabetes, heart trouble, high blood pressure, arthritis or rheumatism, emphysema or bronchitis, stroke, cancer, neurologic condition, ulcers, or other serious health condition.
*P < .05.
Within a health care system characterized by a general decline in rates of use, managed care had a positive effect on rates of use among the nonpoor. Among the poor, the effect of managed care was neutral or mildly negative. These results imply a relative reallocation of specialty resources to the nonpoor.
DISCUSSION
Most previous reports of the impact of managed care on mental health access have been subject to several important methodological limitations, including lack of systematic data on the participating enrollees before managed care, no information on nonusers, no comparison group, and only a few important covariates available for control. Our study involved a quasi-experimental design with 2 measurement periods before the introduction of managed care and 1 measurement period 2 years after. Epidemiologic and sociodemographic data beyond those contained in claims records allowed us to compare the impact of managed care among the poor and nonpoor while adjusting for important covariates.
Our study, however, was limited in some ways. Our sample did not include nonpoor residents of higher income areas. The community sample included few individuals with chronic mental illness, so we cannot generalize our findings to this group. Privatization occurred simultaneously with capitation-based managed care in each region, and there was essentially insufficient variation in capitation rates to allow testing of any effect of level of capitation on service use. The nature of the reform dictated that we focus our research on the impact of the reform as a package. The applicability of this study to Medicaid programs in the United States is limited to those in which privatization is combined with managed care.
It must also be recognized that rates of use in our comparison groups (poor and nonpoor residents of nonreform regions) might have been affected by reform in the adjacent regions. Some of the changes occurring in reformed regions may have affected use rates in control regions, perhaps owing to media attention to the reform, to which the poor might have been more responsive. We are aware of the potential issue of contamination of the control regions by factors affecting the reformed regions and note this as a limitation.
With these caveats, it appears that managed care has different effects on poor and nonpoor groups. Among the poor, maintenance of the same levels of use previously observed in the public mental health sector suggests a simple substitution of private practitioners for public sector providers. Managed care brought specialty providers to reform regions, and the nonpoor made more use of these new providers. A possible reason is that before managed care, the nonpoor held more negative attitudes toward public sector mental health services but faced economic constraints on access to private mental health care. The nonpoor may have valued the increased access to private specialty providers (with no co-payments) more than the poor, who had always had relatively open access to specialty care in the public sector.
Furthermore, the nonpoor may be different from the poor in ways that affect how they respond to the reforms. The nonpoor might have more experience with private practitioners than the poor. If so, the nonpoor might have had more success navigating the private health care system when managed care was instituted. More research is necessary on the effects of managed care on the use of various types of services to shed light on the mechanisms by which the reallocation took place.
Our results raise the further question of why, in the nonreform regions, rates of use among the nonpoor were falling dramatically. The decline may have been due to the increase in the restrictiveness of private mental health benefits, escalating out-of-pocket costs, and the perception among the nonpoor of declining quality in the public mental health care sector. Studies of managed mental health care conducted in the 1990s revealed downward trends in rates of mental health care use.23
Our findings highlight the importance of the distributional consequences of comprehensive reforms of mental health systems that include both the poor and the near poor. Such reforms are under way or being contemplated in several states. The challenge is to expand coverage for the uninsured while maintaining an effective safety net for the most vulnerable groups. As eligibility for public health financing programs is expanded upward in terms of income groups, we recommend monitoring the extent to which public funds are directed to economically disadvantaged populations.
Acknowledgments
This study was supported by research grants R01-MH42655 and K05-MH01263 from the National Institute of Mental Health.
Peer Reviewed
M. Alegría was responsible for planning the study and writing the paper. T. McGuire contributed significantly to the writing of the paper. M. Vera and G. Canino helped plan the study and assisted in the writing process. As project director for the study, L. Matías was in charge of data collection and assisted with the study design. J. Calderón was in charge of data analysis and data programming, as well as drafting the table and figure.
References
- 1.Ware JE, Bayliss MS, Rogers WH, Kosinski M, Tarlov AF. Differences in 4-year health outcomes for elderly and poor, chronically ill patients treated in HMO and fee-for-service systems. JAMA. 1996;276:1039–1047. [PubMed] [Google Scholar]
- 2.Mechanic D. Health care for the poor: some policy alternatives. J Fam Pract. 1986;22:283–289. [PubMed] [Google Scholar]
- 3.Holzer CE, Shea BM, Swanson JW, et al. The increased risk for specific psychiatric disorders among persons of low socioeconomic status. Am J Soc Psychiatry. 1986;6:259–271. [Google Scholar]
- 4.Dohrenwend BP, Itzhak L, Shrout P, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255:946–952. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Study. Arch Gen Psychiatry. 1994;51:8–19. [DOI] [PubMed] [Google Scholar]
- 6.Schur CL, Dorosh E. Attitudes toward costcontainment features of managed care: differences among patient subgroups. Am J Managed Care. 1998;4:1385–1391. [PubMed] [Google Scholar]
- 7.Davis K, Collins KS, Schoen C, Morris C. Choice matters: enrollees' views of their health plans. Health Aff. 1995;14:99–112. [DOI] [PubMed] [Google Scholar]
- 8.Mark T, Muller C. Access to care in HMOs and traditional insurance plans. Health Aff. 1996;15:81–87. [DOI] [PubMed] [Google Scholar]
- 9.Leigh WA, Lillie-Blanton M, Martínez RM, Collins KS. Managed care in three states: experiences of low-income African-Americans and Hispanics. Inquiry. 1999;36:318–331. [PubMed] [Google Scholar]
- 10.Lillie-Blanton M, Lyons B. Managed care and low-income populations: recent state experiences. Health Aff. 1998;17:238–247. [DOI] [PubMed] [Google Scholar]
- 11.Sisk JE, Gorman SA, Reisinger AL, Glied SA, DuMouchel WH, Hynes MM. Evaluation of Medicaid managed care. JAMA. 1996;276:50–55. [PubMed] [Google Scholar]
- 12.Gold M. Medicaid managed care: interpreting survey data within and across states. Inquiry. 1999;36:332–342. [PubMed] [Google Scholar]
- 13.Busch S. Carving-out mental health benefits to Medicaid beneficiaries: a shift toward managed care. Adm Policy Ment Health. 1997;21:301–321. [DOI] [PubMed] [Google Scholar]
- 14.Chang CF, Kiser LJ, Bailey JE, et al. Tennessee's failed managed care program for mental health and substance abuse services. JAMA. 1998;279:864–869. [DOI] [PubMed] [Google Scholar]
- 15.Gold M. Markets and public programs: insights from Oregon and Tennessee. J Health Polit Policy Law. 1997;22:633–666. [DOI] [PubMed] [Google Scholar]
- 16.Alegría M, Pescosolido B, Santos D, Vera M. Can we conceptualize and measure continuity of care in individual episodes? The case of mental health services in Puerto Rico. Sociol Focus. 1997;30:113–129. [Google Scholar]
- 17.Vera M, Alegría M, Freeman D, Robles R, Pescosolido B, Peña M. Help seeking for mental health care among poor Puerto Ricans: problem recognition, service use, and type of provider. Med Care. 1998;36:1047–1056. [DOI] [PubMed] [Google Scholar]
- 18.Pescosolido B, Wright E, Alegría M, Vera M. Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Med Care. 1998;36:1057–1072. [DOI] [PubMed] [Google Scholar]
- 19.Fuller WA, Kennedy W, Schnell D, Sullivan G, Park HJ. PC Carp. Ames: Statistical Laboratory, Iowa State University; 1986:104–117.
- 20.Kish L. Survey Sampling. New York, NY: John Wiley & Sons Inc; 1965.
- 21.Frank RG, McGuire TG. Economics and mental health. In: Culyer A, Newhouse JP, eds. Handbook of Health Economics. Amsterdam, the Netherlands: North-Holland; 2000:10.1–10.29.
- 22.Software for Survey Data Analysis (SUDAAN) User's Manual, Version 7.5. Research Triangle Park, NC: Research Triangle Institute; 1997.
- 23.Ma C, McGuire T. Costs and incentives in a behavioral health carve out. Health Aff. 1998;17:53–69. [DOI] [PubMed] [Google Scholar]