In 1997, the Robert W. Woodruff Foundation provided $5 million, through the CDC Foundation, for the Cooperative for Assistance and Relief Everywhere (CARE) International and the Centers for Disease Control and Prevention (CDC) to create a sustainable partnership in global health. The investment provided discretionary resources and an incentive for CARE and CDC to maximize each other's strengths. This grant enabled the CARE–CDC Health Initiative (CCHI) to fund 9 collaborative projects in Africa and Central and South America and 1 Atlanta-based project involving CARE and CDC headquarters staff. Now, 4 years later, CCHI is concluding its initial phase of activity.
Reports from these projects, which reflect community-based participatory research, are featured in this special global health issue of the Journal. Significantly, nearly all of the articles have been authored or coauthored by CARE national field staff and demonstrate the unique ways in which CCHI has fostered community-based participatory research. In this editorial we discuss the current research process, community-based participatory research as a philosophical premise, the CCHI model, and recommendations for the future.
LIMITATIONS OF CURRENT PARTICIPATORY RESEARCH PRACTICES
Even though the value of community involvement in setting research goals or questions is recognized,1 resources are frequently awarded without soliciting community input. Rarely are community partners, such as local nongovernmental or community organizations, asked to comment on proposed initiatives or requests for research proposals. Consequently, researchers often must bridge an approach that validates communitydefined research issues with another that provides resources according to predetermined, categorical solutions. The Asian Forum for Health Research Regional Meeting in February 2000 echoed the need to involve community stakeholders in research planning. Challenging how research priorities are set and by whom, participants proposed a paradigm shift that emphasizes research vision, equity, consumer orientation, and incentives for promoting locally generated information and ownership of knowledge.2
A second limitation attributed to current research practices is the failure to routinely engage local investigators as authors or coauthors of scientific manuscripts emanating from research conducted in developing countries. In 1995, an article in Scientific American documented the overwhelming authorship gap between developed and less developed countries. The author observed that the developing world's share of mainstream journal articles in the international scientific literature was less than 1%.3 With the notable exception of Brazil and a few other developing countries, little has changed since this article was published. This issue is all the more significant given the downward trend in the numbers of journals published in less developed countries over the past decade.4
This omission has created a dichotomy whereby health issues from the developing world are almost exclusively reported and described by researchers from the developed world. A common perception among local investigators is that publications by first-world authors are the end line for research, and that capacity building and technology transfer are not given high enough priority.2 This point was underscored in a recent site visit to Ghana. CCHI sent a team of health professionals to present this initiative to the World Health Organization country representative and senior staff. In the course of the discussion, the World Health Organization participants began to volunteer their individual frustrations over their inability to publish their work. The issue resonated among these professionals, who unanimously endorsed CCHI's approach of integrating professional development throughout the partnership.
Finally, community-based research is limited by the timeintensive nature of developing and maintaining community trust within the context of short funding cycles. Although a recent US Department of Health and Human Services task force recommended funding time frames compatible with building and sustaining such partnerships,5 the inevitable lag between proposing and enacting recommendations continues to inhibit participatory research.
COMMUNITY-BASED PARTICIPATORY RESEARCH
Community-based participatory research capitalizes on the strengths and resources inherent in host communities. Although terminology—“participatory research,” “community-involved research,” “community-centered research”—varies by author, each study involves and is influenced by nonacademic community partners.
In contrast to the positivist paradigm, which demands static, “objective” knowledge independent of a researcher's interest, community-based research asserts that the way in which questions are framed is inherently purposive, value-laden, and ideological.6, 7(p175) In community-based participatory research, the definition of scientific rigor is broadened to encompass community participation in decision making at every phase of the research process: defining the problem, setting goals, selecting methods, interpreting data, and recommending policy. Essential to this philosophical construct is the assurance of quality decision making throughout the research process. In the document Building Community Partnerships in Research, participatory research is described as the gold standard toward which all federally funded research should aspire.5(p7)
CARE–CDC HEALTH INITIATIVE
To achieve the desired community-based partnership, CCHI developed a model that enabled CARE and CDC to incorporate each other's strengths within a community participatory framework.8 Specifically, CCHI asked CARE offices in 67 countries to solicit health issues or needs from local constituencies. CCHI then matched these responses with the appropriate scientific expertise within CDC and subsequently requested jointly developed proposals that included input from CDC scientists, CARE field staff, and their communities.
Soliciting, reviewing, and awarding these proposals took less than 3 months—considerably faster than the 6 to 9 months typically required for federal awards. Despite this reduced processing time, each proposal received thorough scientific and ethical review in accordance with established CDC policy. Each CARE–CDC awardee was required to produce a written manuscript, protocol, or handbook at the end of the project period. CDC technical advisors were required to participate in CCHI meetings, to provide ongoing dialogue among stakeholders, and to engage their national partners in implementing the research process.
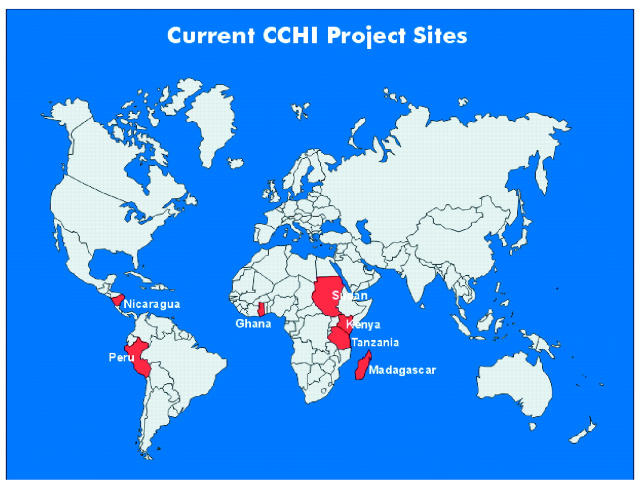
The CCHI collaborations described below showcase diverse public health projects on 3 continents:
• In a sleeping sickness intervention in South Sudan, CCHI joined the International Medical Corps to improve vector control, active case detection, and treatment.9
• Water projects in Madagascar10, 11 and Kenya12 provided clean and affordable drinking water to urban and rural communities, using an internationally proven intervention that combines local water purification, safe water storage, and educational awareness campaigns.
• In Lima, Peru, a CCHI team responded to requests from urban municipalidades (local jurisdictions) for an environmental health plan addressing unsafe drinking water, lack of sanitation, poor air quality, and other environmental problems.13
• In a campaign to prevent HIV/AIDS in Ghana, CCHI worked with local media to produce a radio soap opera incorporating messages about sexual responsibility and safe sexual practices.14
• In Tanzania, CCHI teams sought to improve access to emergency obstetric care, which is a significant problem in rural areas lacking public transportation and paved roads.15
• In western Kenya, where the country's mortality rate for children less than 5 years is highest, CCHI trained lay volunteers to determine appropriate treatment and referral on the basis of a child's presenting signs and symptoms.16, 17
• In Nicaragua, CCHI improved local capacity by training national teams in total quality management, team building, and supervision.18
Finally, CCHI funded publication of 2 manuals: Safe Water Systems for the Developing World,19 a compilation of lessons learned from years of experience implementing the system, and The Healthy Newborn: A Reference Manual for CARE Program Managers, which is reviewed in this issue of the Journal.20
To meet its objective of enhancing program staff's capacity in scientific writing, CCHI convened a 1-week scientific writers workshop in the spring of 2000.
This workshop brought together CARE national project managers, CDC technical advisors, and editors from the American Journal of Public Health, the Canadian Medical Association Journal, and CDC. The CARE national staff consulted with seasoned editors and technical writers and received expert guidance regarding their manuscripts. In one example of the success of the workshop, a CARE Malagasy collaborator is first author of a report featured in this issue.11 This is the first publication of a Malagasy author in an internationally recognized journal.
CARE national staff were also oriented to the process of publishing in peer-reviewed scientific journals, a process in which many health professionals from the developing world have had no opportunity to engage. Enthusiastic praise along with requests from participants for more opportunities of this kind clearly indicated that the workshop tapped an unmet need. This effort exemplifies the global health approach, recently advocated in The Lancet,21 of emphasizing small-scale projects and individual collaborations. Because the CCHI model fosters full involvement of national staff in every phase of research, including publication in a peer-reviewed journal, it offers a comprehensive, full-circle approach to collaboration while ensuring accountability from CDC and CARE.
A FINAL WORD: RECOMMENDATIONS FOR FUTURE ACTIVITY
The goals of global and domestic public health research are the same: to integrate knowledge into strategies for community and social change.7 Success will come only when local ownership and decentralized decision making are integral to public health interventions. Accordingly, the following issues deserve further consideration:
-
Emphasize the “how.” The way in which public health agencies select, fund, implement, and make research accountable can be as important as the selection of an intervention. Valuing “how” means keeping field practitioners abreast of new practices, providing flexibility to budget processes, focusing on appropriate outcomes, and allowing communities a much greater hand in developing the program, rather than passively receiving outside researchers' solutions.
Public health researchers often chastise clinicians for being so invested in a medical procedure that they will not give it up, even when evidence consistently reveals its ineffectiveness.22 The same may be true of public health researchers when we attempt to implement what may be a tremendously effective intervention by means of dated and ineffective processes. The CCHI model demonstrates the value of innovative approaches with collaboration between scientists and the community. Preliminary results suggest that this model has facilitated the timely translation of research findings into improved public health practices.
What's past is prologue. Historians appreciate the importance of analyzing present circumstances in light of past events. When developing initiatives to award resources for new public health priorities, agencies should review lessons from past investments with regard to research in community settings. For example, with the emergence of the community-based participatory research model, reviewing literature describing previous experiences, such as the community intervention projects conducted in Tanzania or the empowerment work carried out in Brazil and Chile more than 30 years ago, would provide valuable insight.23–25 Looking to the future, publishing the results of contemporary community-based participatory research is vital so that lessons learned can continue to be shared.
Alternatives should be encouraged. With developed countries controlling the majority of resources, the tendency is to develop assistance programs without soliciting local community input or acknowledging their strengths. The community-based participatory model offers a fresh approach to local capacity building in applied research. Accordingly, improved methodologies and assessments are needed to better understand the dynamics of community change and to identify what works.
CCHI has attempted to address limitations of current research practices. Factors that contributed to CCHI's success included an adherence to the community-based participatory model in project design, development, and implementation; ongoing communication and collaboration between CARE field staff and CDC scientists throughout the project period; and a comprehensive approach to building capacity in the CARE country staff that encompassed community proficiency in project implementation, provided opportunities for scientific authorship, and presented findings to local public health practitioners.
CCHI, which tapped into the interests and strengths of both CARE and CDC, offers a successful model for public–private collaborations that is relevant to both domestic and global settings.
Figure .
Acknowledgments
The authors would like to thank Stanley O. Foster, visiting professor, Rollins School of Public Health, Emory University, for serving as senior evaluator for the CARE–CDC Health Initiative. The authors also wish to acknowledge the invaluable reference and editorial assistance provided by Stephen Blount, Onnalee Henneberry, Jay McAuliffe, Bobby Milstein, Marguerite Pappaioanou, Joy Lawn, and Gwen Ingraham of CDC and John Steward of the Agency for Toxic Substances and Disease Registry. Special appreciation is accorded to Wayt Gibbs, Scientific American, for writing an article that inspired CCHI to integrate scientific writing as an essential feature of this initiative.
References
- 1.Institute of Medicine. Linking Research and Public Health Practice: A Review of CDC's Program of Centers for Research and Demonstration of Health Promotion and Disease Prevention. Washington, DC: National Academy Press; 1997:3. [PubMed]
- 2.Asian consultative process. Available at: http://www.conference2000.ch/asianconsult.html. Accessed July 23, 2001.
- 3.Gibbs WW. Lost science in the Third World. Scientific American. August 1995:92.
- 4.Tenth International Conference of Science Editors; August 27–30, 2000; Rio de Janeiro, Brazil. Proceedings available at: http://www.bireme.br/ifse-rio/I/proceedings.htm. Accessed July 23, 2001.
- 5.Building Community Partnerships in Research: Recommendations and Strategies. Executive Summary. Washington, DC: US Dept of Health and Human Services; April 7, 1998.
- 6.Ratcliffe JW. Rigor in health-related research: toward an expanded conceptualization. Int J Health Serv. 1988;18:361–363. [DOI] [PubMed] [Google Scholar]
- 7.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. [DOI] [PubMed] [Google Scholar]
- 8.Bell PD, Stokes CC. Melding disparate cultures and capacities to create global health partnerships. Am J Public Health. 2001;91:1552–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joja LL, Okoli U. Trapping the vector: community action to curb sleeping sickness in southern Sudan. Am J Public Health. 2001;91:1583–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunston C, McAfee D, Kaiser R, et al. Collaboration, cholera, and cyclones: a project to improve point-of-use water quality in Madagascar. Am J Public Health. 2001;91:1574–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mong Y, Kaiser R, Ibrahim D, Rasoatiana, Razafimbololona L, Quick RE. Impact of the Safe Water System on water quality in cyclone-affected communities in Madagascar. Am J Public Health. 2001;91:1577–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Makutsa P, Nzaku K, Ogutu P, et al. Challenges in implementing a point-of-use water quality intervention in rural Kenya. Am J Public Health. 2001;91:1571–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baffigo V, Albinagorta J, Nauca L, et al. Community environmental health assessment in Peru's desert hills and rainforest. Am J Public Health. 2001;91:1580–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panford S. Using folk media in HIV/AIDS prevention in rural Ghana. Am J Public Health. 2001;91:1559–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmid T, Kanenda O, Ahluwalia I, Kouletio M. Transportation for maternal emergencies in Tanzania: empowering communities through participatory problem solving. Am J Public Health. 2001;91:1589–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly JM, Osamba B, Garg R, et al. Community health worker performance in the management of multiple childhood illnesses: Siaya District, Kenya, 1997–2001. Am J Public Health. 2001;91:1617–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garg R, Omwomo W, Witte J, Lee LA, Deming MS. Care seeking during fatal childhoood illnesses: Siaya District, Kenya, 1998. Am J Public Health. 2001;91:1611–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McEwan E, Conway MJ, Bull DL, Malison MD. Developing Public Health Management Training Capacity in Nicaragua. Am J Public Health. 2001;91:1586–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Safe Water Systems for the Developing World: A Handbook for Implementing Household-Based Water Treatment and Safe Storage Projects. Atlanta, Ga: Centers for Disease Control and Prevention; 2000. Also available at: http://www.cdc.gov/safewater. Accessed July 3, 2001.
- 20.Foege W. The Healthy Newborn: A Reference Manual for the Program Manager [commentary]. Am J Public Health. 2001;91:1563–1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Enabling research in developing countries [editorial]. Lancet. 2000;356:1043. [PubMed] [Google Scholar]
- 22.McKinlay JB. The promotion of health through planned sociopolitical changes: challenges for research and policy. Soc Sci Med. 1993;36:112. [DOI] [PubMed] [Google Scholar]
- 23.Park P, Brydon-Miller M, Hall B, Jackson T, eds. Voices of Change: Participatory Research in the United States and Canada. Westport, Conn: Bergin & Garvey; 1993.
- 24.Green LW, George A, Daniel M, et al. Study of Participatory Research in Health Promotion: Review and Recommendations for the Development of Participatory Research in Health Promotion in Canada. Ottawa, Ontario: Royal Society of Canada; 1995.
- 25.Freire P. Pedagogy of the Oppressed. New York, NY: Continuum; 1993.