Abstract
Since 1990, the number of people without access to safe water sources has remained constant at approximately 1.1 billion, of whom approximately 2.2 million die of waterborne disease each year. In developing countries, population growth and migrations strain existing water and sanitary infrastructure and complicate planning and construction of new infrastructure.
Providing safe water for all is a long-term goal; however, relying only on time- and resource-intensive centralized solutions such as piped, treated water will leave hundreds of millions of people without safe water far into the future. Self-sustaining, decentralized approaches to making drinking water safe, including point-of-use chemical and solar disinfection, safe water storage, and behavioral change, have been widely field-tested. These options target the most affected, enhance health, contribute to development and productivity, and merit far greater priority for rapid implementation.
We continue to allocate more money to conflict than to services, prestige projects take precedence over more mundane services, and populations without water and sanitation have neither the contacts nor the power to exert any influence. . . . [That] we have been unable or unwilling to ensure the access of one-quarter of the world's population to a safe supply of water and one-half of the world's population to adequate excreta disposal is among the most glaring examples of a failure to apply basic scientific principles to protect human health.
Paul Taylor1
WATER IS ESSENTIAL TO LIFE. We drink it, raise crops and livestock with it, clean our bodies and environment with it, and play in it. When it is contaminated with human or animal wastes, however, water carries illness and death. Approximately 1.1 billion persons, or one sixth of the world's population, lack access to safe water sources, and many more lack access to safe water.2
Important diseases that can be transmitted by the waterborne route include cholera, typhoid fever, amoebic and bacillary dysentery, and other diarrheal diseases; these diseases, which cause an estimated 2 187 000 deaths worldwide each year (A. Pruess, MPH; World Health Organization; written communication; May 10, 2001), account for most water-associated morbidity and mortality. Other contributors include (1) the water-washed diseases (e.g., scabies, trachoma), caused by poor personal hygiene and preventable through improved access to safe water; (2) the water-based diseases, caused by parasites found in intermediate organisms living in water (e.g., dracunculiasis, schistosomiasis); and (3) the water-related diseases, caused by insect vectors that breed in water (e.g., dengue, malaria).3 The direct health burden is supplemented by the annual expenditure of over 10 million person-years of time and effort by persons carrying water from distant and often polluted sources.4 In addition, indigent populations often pay exorbitant prices for limited quantities of poor-quality water, at costs that can represent 20% of a family budget,5 while services to wealthier urban dwellers are heavily subsidized and of relatively high quality.6 The claim has been made that no single type of intervention has greater overall impact on national development and public health than does the provision of safe drinking water and the proper disposal of human excreta.4
In 1980, the United Nations General Assembly proclaimed the period 1981 to 1990 as the International Drinking Water Supply and Sanitation Decade, with the primary goal of full access to water supplies and sanitation for all.6 During the course of that decade, access to safe water was provided to an additional 1347 million people and access to sanitation facilities was provided to an estimated 748 million, at an estimated cost of US $133.9 billion.6 Despite these major accomplishments, by the decade's end more than 1.1 billion people still lacked access to safe water and 2.4 billion were without adequate sanitation.2 Reasons cited for the decade's failure to achieve more include population growth (estimated at 750 million), funding limitations, inadequate operation and maintenance, inadequate cost recovery, insufficient trained personnel,7 and continuation of a “business as usual approach,” drawing on traditional policies, resources, and technologies.6 In particular, little progress was made in providing services to rapidly expanding, low-income, marginalized urban populations and to rural areas.6,7 The most recent assessment of water supply and sanitation coverage shows that although more people than ever have access to water supply and sanitation services, the absolute numbers of unserved people remained constant throughout the period 1990 to 2000, when 1.1 billion were without access to improved water sources and 2.4 billion lacked access to basic sanitation.2
Water treatment plants and other large-scale projects remain an important and necessary objective of many development agencies; they were major advances in the sanitary revolution in industrialized countries at the end of the 19th century.8 A century later, providing safe piped water to dispersed populations in rural areas of developing countries can be prohibitively expensive for governments, donors, and private utilities, calling into question the sustainability of this approach and whether anticipated health gains will be achieved, even from large investments. Meanwhile, in urban areas, rapid population growth and migrations motivated by cultural, economic, political, and environmental factors strain existing water and sanitary infrastructures and create enormous problems in planning and constructing new infrastructure. Residents of many of the world's largest cities enjoy only intermittent access to piped water, often of dubious quality and only from public taps at substantial distances from their homes. Others depend on water vendors for small volumes of costly water of unsure quality. Where providers cannot guarantee water quality at the point of supply, or where it cannot be guaranteed at the point of use, because of contamination during collection, transport, and storage, consumers face significant health risks.
Given the failure to reduce the numbers of people without access to basic water supply and sanitation during the 1990s, and the financial implications of even the apparently modest international development target of halving the proportion of people not served with improved drinking water by 2015 (A. Pruess, MPH, written communication, May 10, 2001), it is evident that “business as usual” cannot provide a satisfactory response. Approaches that rely solely on time- and resource-intensive centralized solutions will leave hundreds of millions of people without access to safe water far into the foreseeable future; a radical reorientation toward interventions to support these populations is urgently required. This commentary reviews 2 low-cost decentralized technologies used to improve drinking water quality in developing countries and considers the role these technologies may play in future efforts to provide safe drinking water for all.
POINT-OF-USE CHEMICAL DISINFECTION
Where water sources are contaminated, drinking water must be treated to prevent waterborne disease. In the absence of functioning centralized water treatment systems, this responsibility falls to consumers by default. Treatment by boiling inactivates viral, parasitic, and bacterial pathogens, but it is economically and environmentally unsustainable.9, 10 Boiling provides no residual protection; after cooling, water can easily be recontaminated,11 and it is associated with the risk of scalding, especially among infants. Safe and inexpensive chemical disinfectants that are suitable for household use in developing countries offer a practical alternative to boiling. Various point-of-use chemical agents for water treatment have been reviewed.12 Overall, sodium hypochlorite, the active ingredient in commercial laundry bleach solutions, appears to be the safest, most effective, and least expensive chemical disinfectant for point-of-use treatment. As described in this issue, a dilute solution of sodium hypochlorite can be produced on-site through electrolysis of salt water13 or can be commercially manufactured by a private company.14
In the past 5 years, several published field trials of hypochlorite for point-of-use water treatment have established that it is acceptable for and effective at improving water quality in a number of settings, and that its use can reduce diarrheal illness by up to 85%.15–19 It has been used to improve the safety of oral rehydration solutions and street-vended beverages,20,21 and, as described in this issue, as an emergency response measure for persons displaced by natural disasters and threatened by epidemic cholera.13, 22, 23 Among the limitations of hypochlorite-based disinfectants are their relative ineffectiveness against parasites and viruses and the reduced efficiency and disagreeable taste or odor that may result when they are used to treat water with excessive amounts of organic material.12, 14 In their favor are the protective residual effect against bacterial contamination and the fact that they can be easily and reliably quantified in treated water by simple and inexpensive colorimetric assays.
POINT-OF-USE SOLAR DISINFECTION
The earth is bathed in electromagnetic radiation emitted from the sun, and solar radiation can be harnessed for point-of-use water disinfection.24 Inactivation of pathogens in water may be achieved through the effects of ultraviolet radiation with or without the synergistic effects of increased temperature, or through increased temperature alone (“solar pasteurization” or “solar distillation”). The bactericidal effects of solar radiation obtained in different types of containers, at different exposure times and under different meteorologic conditions, have been documented.25–27 Much of what has been learned has been incorporated into SODIS, a solar water disinfection project initiated by the Department of Water and Sanitation in Developing Countries (SANDEC). Clear plastic soda bottles or bags made of polyethylene terephthalate (PET) are used because they transmit ultraviolet A and are widely available, inexpensive, and chemically stable.28 Thermal inactivation is significant only at water temperatures above 45°C.28,29 Because heat increases the bactericidal effects of ultraviolet radiation, the bottom half of the bottle may be painted black or the clear bottles may be laid on a black surface to increase thermal effects. A paraffin-filled tube can be used to indicate temperatures at which sufficient disinfection is achieved. Turbidity markedly decreases the penetration of ultraviolet radiation; hence, it is advisable to treat water with turbidity greater than 30 nephelometric turbidity units by filtration, flocculation, or sedimentation before solar disinfection. Water can be aerated by vigorous shaking before exposure to solar radiation to take advantage of the increased bactericidal effects that occur in the presence of oxygen.30
“Approaches that rely solely on time- and resource-intensive centralized solutions will leave hundreds of millions of people without access to safe water far into the foreseeable future.”
Field trials of solar disinfection in Kenya demonstrated that it was an acceptable and effective means of improving water quality and significantly reduced the incidence of diarrhea and severe diarrhea in children.31,32 Other health impact studies are under way. The limitations of solar disinfection are the need for sufficient solar radiation and relatively clear water and the difficulty in treating large volumes. Its advantages are simplicity, extremely low cost, and the fact that it leaves the taste of water unchanged.
SAFE WATER STORAGE
Water from potable sources, as well as water that has been made potable by boiling, chemical treatment, or solar disinfection, remains susceptible to the introduction of contaminants during collection, transport, and storage. The risk of diarrhea due to the contamination of drinking water during household storage, first noted in the 1960s,33 has since been repeatedly observed.34–38 It has been argued that people are less likely to suffer illness from organisms in their stored drinking water when the person introducing the organisms is a member of their household rather than a stranger.39 While this may be true, infants and young children, who suffer the highest rates of diarrheal mortality, are vulnerable to infection from even small doses of waterborne pathogens that may be familiar to, and unlikely to cause illness in, other household members. Furthermore, studies have identified drinking water contaminated during collection, transport, and storage as a significant route of transmission during epidemics of cholera and dysentery.40–42 Simply replacing unsafe water storage vessels with safer ones led to lower rates of cholera transmission in households in Calcutta43 and less diarrhea in children in a refugee camp in Malawi.38
The principles of safe water storage, the characteristics of safe water storage vessels, and early intervention studies evaluating these vessels have been reviewed.12 Safe water storage vessels with tight-fitting lids and narrow mouths, which allow users to remove water by pouring or through spigots but not by dipping, have been incorporated into both chemical and solar water treatment programs.28, 44 The articles in this issue by Makutsa et al.14 and Ogutu et al.45 highlight the challenges of creating water storage vessels that meet traditional cultural standards and still fulfill the role of adequately protecting treated water from recontamination.
BEHAVIORAL CHANGE
To achieve significant reductions in the incidence or severity of diarrheal diseases, public health programs must change behavior.46 Point-of-use water treatment adds to the time and expense required of consumers. Adopting a new vessel for water storage also adds expense and may have other disadvantages, such as the inability to maintain stored water at cooler temperatures.19,45 The process by which new water treatment and storage behaviors are promoted is as critical as the disinfection and storage “hardware.” Several innovative approaches have been applied to change behavior in the context of programs to promote point-of-use disinfection and safe water storage. These include social marketing, motivational interviewing,47 and, as described in this issue by Dunston et al.13 and Makutsa et al.,14 community mobilization.44
Improvements in the quality of drinking water provide far more benefit when coupled with improvements in hygiene and sanitation.48, 49 Introducing treated drinking water into households in storage vessels with spigots or spouts enables families to reduce their exposure to waterborne pathogens and, in conjunction with hand washing and soap promotion, provides a platform for reducing the risk of water-washed diseases.50 Safe storage of water in covered or closed containers may significantly reduce contamination by host organisms for the parasitic causes of water-based diseases and by mosquito vectors of water-related diseases such as dengue. Finally, safe water and, if available, hypochlorite disinfectant can be used for washing fruits, vegetables, and other foods consumed raw, thereby potentially reducing the incidence of food-borne infections.
THE ROLE OF LOW-COST, APPROPRIATE TECHNOLOGIES
In the past decade, low-cost decentralized approaches to making drinking water safer have been field-tested and have begun to be implemented in self-sustaining “real world” programs.17, 44 A systems approach, incorporating elements of water treatment, safe water storage, and health education into a single program, will probably have greater, longer-lasting positive impacts on public health. Even greater impact may be attainable by increasing water availability and improving sanitation, according to the needs and resources of the communities served. Novel methods for safe disposal of human wastes, such as dehydrating toilets with urine separation, are already being evaluated in some areas.51 The limiting factor for sustaining these interventions may be the economic capacity of the target population.
Safe water storage vessels with tightfitting lids and narrow mouths have been incorporated into both chemical and solar water treatment programs.
The problems of unsafe water and poor sanitation demand a multitude of varied and complementary solutions. In most areas, available options for point-of-use water treatment are limited and ineffective at preventing disease (filtration, sedimentation) or inconvenient and prohibitively expensive (boiling). Point-of-use programs in several countries have demonstrated that the market for safe water will readily absorb more effective treatment options if these are reasonably priced and properly promoted.44
We are witnessing unprecedented experimentation with new forms of privatization worldwide and increased attention to accountability and performance. People are increasingly perceived as consumers, rather than recipients, of development. Recognition of this trend favors an emphasis on consumer choice and a more pluralistic approach toward water safety, with an increasing number of options of varying costs, convenience, and effectiveness more widely available.1 Field trials, such as the ones reported in this issue from Kenya14,45 and Madagascar,13,22,23 can help define the optimal use of each of these options.
Cellular phones and satellite dishes revolutionized the telecommunications industry in developing countries, bypassing the expenditures and delays associated with traditional wire-based systems and allowing consumers rapid access to phone and television service. Similarly new scientific research and the current global economic and political climate offer dramatic opportunities to introduce new decentralized approaches for improving water quality. Capitalizing on these opportunities requires unique partnerships between the private and public sectors that can be brokered by the donor community. Multinational consumer products firms that produce, market, and distribute soap, bleach, and vessels suitable for safe water storage are well positioned to participate in this new sanitary revolution. But many barriers still need to be overcome and much work remains to be done before safe water is made as widely available as tobacco, alcohol, or carbonated soft drinks.
CONCLUSIONS
Far too many people live without access to safe drinking water, and this is a primary determinant of continuing poverty. Progressive expansion of improved water supplies is important but often fails to address the immediate needs of the most disadvantaged. Options such as point-of-use water treatment target the most affected directly, enhance health benefit, and thereby contribute to development and productivity. Existing sector institutions are structured for traditional approaches and have a poor track record for promoting alternative technologies. Point-of-use water treatment merits far greater priority for achieving a meaningful rate of implementation.
Figure 3.
Figure 1.
Promotional materials for branded, locally produced sodium hypochlorite solution manufactured and marketed in Bolivia (CLARO), Madagascar (Sûr'Eau), Zambia (Clorin), and Ecuador (Agua Pura). Social marketing of such safe water products is used to promote behavior change.
Figure 2.
Above. A Chinese woman in Ningxia Province appreciating the good taste of SODIS-treated water.
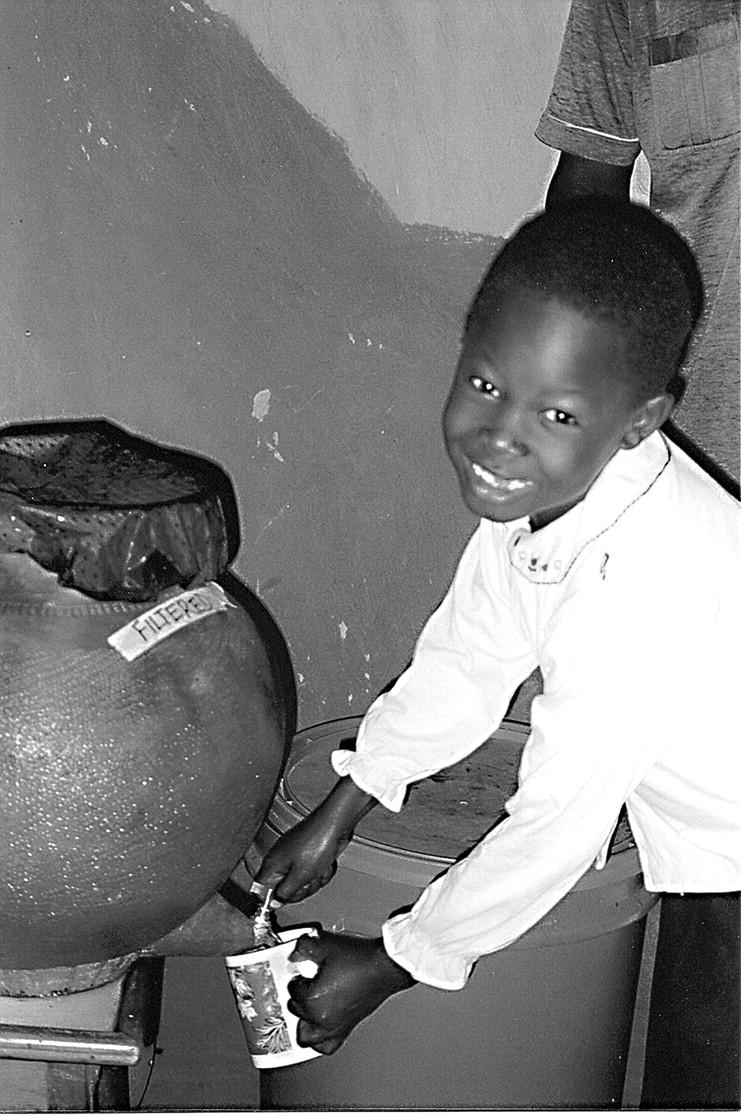
Right. A child from the Rachuonyo District, Nyanza Province, western Kenya, drawing water from the spigot of a clay pot that has been locally modified for safe water storage. (Photo: Valerie Garrett.)
Acknowledgments
All authors contributed to the conception, writing, and editing of the paper.
Peer Reviewed
Note. The views expressed in this commentary do not necessarily represent the decisions or the stated policy of the World Health Organization.
References
- 1.Taylor P. Regional perspectives on water safety: Africa. In: Craun GF, Robinson DE, Hauchman FS, eds. Microbial Pathogens and Disinfection By-Products in Drinking Water: Health Effects and Management of Risks. Washington, DC: International Life Sciences Institute Press; 2001.
- 2.World Health Organization, United Nations Children's Fund (UNICEF), Water Supply and Sanitation Council. Global Water Supply and Sanitation Assessment 2000 Report. New York, NY: UNICEF; 2000.
- 3.Bradley DJ, Emurwon P. Predicting the epidemiological effect of changing water sources. East Afr Med J. 1968;45: 284–291. [PubMed] [Google Scholar]
- 4.Water and Sanitation. Fact Sheet Number 112. Geneva, Switzerland: World Health Organization; November 1996. Available at http://www.who.inl/inf-fs/en/factiiz.html.
- 5.Urban Example—Prospective for the Future. Water Supply and Sanitation to Urban Marginal Areas of Tegucigalpa, Honduras. New York, NY: UNICEF; 1989.
- 6.World Health Organization, UNICEF. Water Supply and Sanitation Sector Monitoring Report 1990. New York, NY: UNICEF; 1992.
- 7.The International Drinking Water Supply and Sanitation Decade. End of Decade Review (as at [sic] December 1990). Geneva, Switzerland: World Health Organization; 1992.
- 8.Melosi M. The Sanitary City: Urban Infrastructure in America From Colonial Times to the Present. Baltimore, Md: Johns Hopkins University Press; 2000.
- 9.Gilman RH, Skillicorn P. Boiling of drinking water: can a fuel-scarce community afford it? Bull World Health Organ. 1985;63:157–163. [PMC free article] [PubMed] [Google Scholar]
- 10.deKonig HW, Smith KR, Last JM. Biomass fuel consumption and health. Bull World Health Organ. 1985;63: 11–26. [PMC free article] [PubMed] [Google Scholar]
- 11.Luby S, Syed A, Atiullah N, Faizan K, Fisher-Hoch S. The limited effectiveness of home drinking water purification efforts in Karachi, Pakistan. Int J Infect Dis. 2000;4:3–7. [DOI] [PubMed] [Google Scholar]
- 12.Mintz ED, Reiff FM, Tauxe RV. Safe water treatment and storage in the home: a practical new strategy to prevent waterborne disease. JAMA. 1995; 273:948–953. [PubMed] [Google Scholar]
- 13.Dunston C, McAfee D, Kaiser R, et al. Collaboration, cholera, and cyclones: a project to improve point-of-use water quality in Madagascar. Am J Public Health. 2001;91:1574–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Makutsa P, Nzaku K, Ogutu P, et al. Challenges in implementing a point-of-use water quality intervention in rural Kenya. Am J Public Health. 2001; 91:1571–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quick RE, Venczel LV, Gonzales O, et al. Narrow-mouthed water storage vessels and in situ chlorination in a Bolivian community: a simple method to improve drinking water quality. Am J Trop Med Hyg. 1996;54:511–516. [DOI] [PubMed] [Google Scholar]
- 16.Semenza J, Roberts L, Henderson A, Bogan J, Rubin CH. Water distribution system and diarrheal disease transmission: a case study in Uzbekistan. Am J Trop Med Hyg. 1998;59:941–946. [DOI] [PubMed] [Google Scholar]
- 17.Quick RE, Mintz ED, Sobel J, Mead P, Reiff F, Tauxe RV. A new strategy for waterborne disease prevention. In: Pickford J, et al., eds. Proceedings of the 23rd WEDC Conference, Durban, South Africa, 1997. Loughborough, England: Loughborough University: 1998.
- 18.Quick RE, Venczel LV, Mintz ED, et al. Diarrhea prevention in Bolivia through point-of-use disinfection and safe storage: a promising new strategy. Epidemiol Infect. 1999;122:83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luby S, Agboatwalla M, Raza A, et al. A low-cost intervention for cleaner drinking water in Karachi, Pakistan. Int J Infect Dis. In press. [DOI] [PubMed]
- 20.Daniels N, Simons S, Rodrigues A, et al. First do no harm: making oral rehydration solution safer in a cholera epidemic. Am J Trop Med Hyg. 1999; 60:1051–1055. [DOI] [PubMed] [Google Scholar]
- 21.Sobel J, Mahon B, Mendoza C, et al. A simple system for water purification and storage, handwashing, and beverage storage reduces fecal contamination of street-vended beverages in Guatemala. Am J Trop Med Hyg. 1998; 59:380–387. [DOI] [PubMed] [Google Scholar]
- 22.Mong Y, Kaiser R, Ibrahim D, Rasoatiana, Razafimbolololona L, Quick RE. Impact of the safe water system on water quality in cyclone-affected communities in Madagascar. Am J Public Health. 2001;91:1577–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reller M, Mong JM, Rabenjoelina, Hoekstra RM, Quick RE. Cholera prevention with traditional and novel water treatment methods: a report of an outbreak investigation in Fort-Dauphin, Madagascar. Am J Public Health. 2001; 91:1608–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rolla TC. Sun and water: an overview of solar water treatment devices. J Environ Health. 1998; 60:30–32. [Google Scholar]
- 25.Acra A, Raffoul Z, Karahagopian L. Solar Disinfection of Drinking Water and Oral Rehydration Solution. Beirut, Leb-anon: Illustrated Publications SAL (for UNICEF); 1984.
- 26.Joyce TM, McGuigan KG, Elmore-Meegan M, Conroy RM. Inactivation of fecal bacteria in drinking water by solar heating. Appl Environ Microbiol. 1996; 62:399–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wegelin M, Canonica S, Meschner K, Fleischmann T, Pesaro F, Metzler A. Solar water disinfection: scope of the process and analysis of radiation experiments. J Water Supply Res Technol AQUA. 1994;43:154–169. [Google Scholar]
- 28.Wegelin M. Solar water disinfection (SODIS): a simple water treatment process. J Water Supply Res Technol AQUA. 2001;50:125–134. [Google Scholar]
- 29.McGuigan KG, Joyce TM, Conroy RM, Gillespie JB, Elmore-Meegan M. Solar disinfection of drinking water contained in transparent plastic bottles: characterizing the bacterial inactivation process. J Appl Microbiol. 1998; 84: 1138–1148. [DOI] [PubMed] [Google Scholar]
- 30.Reed R. Solar inactivation of faecal bacteria in water: the critical role of oxygen. Lett Appl Microbiol. 1997; 24: 276–280. [DOI] [PubMed] [Google Scholar]
- 31.Conroy RM, Elmore-Meegan M, Joyce T, McGuigan K, Branes J. Solar disinfection of drinking water and diarrhoea in Maasai children: a controlled field trial. Lancet. 1996;348:1695–1697. [DOI] [PubMed] [Google Scholar]
- 32.Conroy RM, Meegan ME, Joyce T, McGuigan K, Barnes J. Solar disinfection of water reduces diarrhoeal disease: an update. Arch Dis Child. 1999;81:337–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Zilj WJ. Studies on diarrhoeal diseases in seven countries by the WHO Diarrhoeal Diseases Study Team. Bull World Health Organ. 1966; 35: 249–261. [PMC free article] [PubMed] [Google Scholar]
- 34.Deb BC, Sircar BK, Sengupta PG, et al. Intra-familial transmission of Vibrio cholerae biotype El Tor in Calcutta slums. Indian J Med Res. 1982;76:814–819. [PubMed] [Google Scholar]
- 35.Gunn RA, Kimball AM, Mathew PP, Dutta SR, Rifatt AHM. Cholera in Bahrain: epidemiological characteristics of an outbreak. Bull World Health Organ. 1981;59:61–66. [PMC free article] [PubMed] [Google Scholar]
- 36.Echeverria P, Taylor DN, Seriwatnana J, et al. Potential sources of enterotoxigenic Escherichia coli in homes of children with diarrhoea in Thailand. Bull World Health Organ. 1987; 65: 207–215. [PMC free article] [PubMed] [Google Scholar]
- 37.Khairy AEM, Sebaie OE, Gawad AA, El Attar L. The sanitary condition of rural drinking water in a Nile Delta village, I: parasitological assessment of “zir” stored and direct tap water. J Hyg Camb. 1982;88:57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts L, Chartier Y, Chartier O, Malenga G, Toole M, Rodka H. Keeping clean water clean in a Malawi refugee camp: a randomized intervention trial. Bull World Health Organ. 2001;79: 280–287. [PMC free article] [PubMed] [Google Scholar]
- 39.VanDerslice J, Briscoe J. All coliforms are not created equal: a comparison of the effects of water source and in-house water contamination on infantile diarrheal disease. Water Resources Res. 1993;29:1983–1995. [Google Scholar]
- 40.Swerdlow DL, Mintz ED, Rodriguez M, et al. Waterborne transmission of epidemic cholera in Trujillo, Peru: lessons for a continent at risk. Lancet. 1992;340:28–32. [DOI] [PubMed] [Google Scholar]
- 41.Swerdlow DL, Malenga G, Begokyian G, et al. Epidemic cholera among refugees in Malawi, Africa: treatment and transmission. Epidemiol Infect. 1997;118:207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tuttle J, Ries AA, Chimba R, Perera C, Griffin PM. Epidemic antimicrobial-resistant Shigella dysenteriae type 1 in Zambia: the hazards of stored water and street vended foods. J Infect Dis. 1995;171:371–375. [DOI] [PubMed] [Google Scholar]
- 43.Deb BC, Sircar BK, Sengupta PG, et al. Studies on interventions to prevent eltor cholera transmission in urban slums. Bull World Health Organ. 1986; 64:127–131. [PMC free article] [PubMed] [Google Scholar]
- 44.Safe Water Systems for the Developing World: A Handbook for Implementing Household-Based Water Treatment and Safe Storage Projects. Atlanta, Ga: Centers for Disease Control and Prevention; 2001. Available at: http:// www.cdc.gov/safewater. Accessed July 14, 2001.
- 45.Ogutu P, Garrett V, Barasa P, Om-beki S, Mwaki A, Quick RE. Seeking safe storage: a comparison of drinking water quality in clay and plastic vessels. Am J Public Health. 2001;91: 1610–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stanton B, Black R, Engle P, Pelto G. Theory-driven behavioral intervention research for the control of diarrheal diseases. Soc Sci Med. 1992;35:1405–1420. [DOI] [PubMed] [Google Scholar]
- 47.Thevos AK, Quick RE, Yanduli V. Application of motivational interviewing to the adoption of water disinfection practices in Zambia. Health Promot Int. 2000;15:207–214. [Google Scholar]
- 48.Esrey S, Feachem RG, Hughes JM. Interventions for the control of diarrhoeal diseases among young children: improving water supplies and excreta disposal facilities. Bull World Health Organ. 1985;63:757–772. [PMC free article] [PubMed] [Google Scholar]
- 49.VanDerslice J, Briscoe J. Environmental interventions in developing countries: interactions and their implications. Am J Epidemiol. 1995;141:135–144. [DOI] [PubMed] [Google Scholar]
- 50.Pinfold JV. Faecal contamination of water and fingertip-rinses as a method for evaluating the effect of low-cost water supply and sanitation activities on faeco-oral disease transmission, II: a hygiene intervention study in rural north-east Thailand. Epidemiol Infect. 1990; 105:377–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Esrey S, Gough J, Rapaport D, et al. Ecological Sanitation. Stockholm, Sweden: Swedish International Development Cooperation Agency (SIDA); 1998.