Abstract
To prevent diarrheal diseases in western Kenya, CARE Kenya initiated the Water, Sanitation, and Education for Health (WASEH) Project in 1998. The project targets 72 farming and fishing communities with a total population of 43 000.
Although the WASEH Project facilitated construction of shallow wells and pit latrines, the water quality still needed improvement. Consequently, in 2001, CARE implemented the Safe Water System (which consists of point-of-use water treatment with sodium hypochlorite, safe storage, and behavior change techniques) within the already established WASEH infrastructure, using existing community organizations in combination with a social marketing approach that introduced affordable products. The project has resulted in adoption rates of 33.5% for chemical water treatment and 18.5% for clay pots modified for safe water storage.
IN WESTERN KENYA, diarrheal diseases are a major cause of morbidity and mortality among children younger than 5 years, largely because of inadequate water treatment and human waste disposal infrastructure. A 1999 health survey revealed that 66% of the population in rural Nyanza Province lacked access to safe drinking water, and 47% of children younger than 5 years had experienced diarrhea in the preceding 2 weeks (CARE Kenya, unpublished data, 1999). To further the goals of the WASEH Project, which was already under way, in 2001 CARE implemented the Safe Water System.1
The Nyanza Healthy Water Project adopted the existing WASEH community mobilization and management structure and ensured support by first introducing the project to Kenyan government officials, community management committees, and leaders of women's groups.
In March 2000, we conducted a baseline survey in randomly selected households in 24 villages, asking heads of household about demographic and socioeconomic status, knowledge of causes and prevention of diarrhea, and water handling and sanitation practices. Next, focus groups were convened to discuss community health problems and water-related issues and to help develop an appealing brand name (Klorin) and logo for promoting the solution.
The Products
More than 90% of survey respondents reported boiling as their primary water treatment method. In the focus groups, however, most participants acknowledged that they rarely treated water, despite believing that contaminated drinking water was the main cause of diarrhea in their villages. Most expressed interest in using an inexpensive chemical disinfectant.
CARE signed a memorandum of understanding with a private company to produce a 1% sodium hypochlorite solution, packaged in a 500-mL bottle with an 8-mL cap suitable for dosing. When the first lot of solution proved to have twice the agreed-upon concentration, CARE established quality control to verify the concentration of each lot.
Survey and focus group data revealed that 91% of households stored drinking water in open-mouthed clay pots and that they preferred these pots over plastic jerry cans. Testing determined that, if treated with a high enough dose, water stored in clay pots could retain an adequate level of free chlorine for 24 hours.2 For safer storage, we developed improved clay pots with fitted lids and spigots and evaluated them in the laboratory and the field. Daily power blackouts of up to 18 hours hindered product procurement and delayed implementation by 3 months.
Because of poor road conditions and large distances between communities, product distribution was a major challenge. We chose a noncommercial distribution source, using existing structures organized by WASEH to ensure that products went directly to targeted communities.
This project was designed to recover at least part of its costs. Prices were calculated by adding fixed and variable costs and factoring in the cost of similar, commonly purchased items. Thus, a 500-mL bottle of solution was priced at about US $0.33 and a 20-L modified clay pot at US $2.53. Margins were used as incentives for wholesalers, and small sales commissions were offered to stimulate sales.
Behavior Change
An important challenge was changing the behavior of a population with well-established water-handling habits, limited income, and a history of receiving free goods from nongovernmental organizations. We used promotion venues preferred by focus groups: community meetings, schools, and village health training workshops. Village health promoters used participatory hygiene and sanitation transformation (PHAST) methodology3 to teach their communities about the Safe Water System and to resolve problems. For example, when rumors arose that Klorin would make people infertile, community meetings were called to dispel these fears with accurate product information and support from respected community leaders.
To encourage behavior change, we employed social marketing tools such as Klorin-themed posters, brochures, banners, and T-shirts. Promotional activities included puppet shows, skits, dancers dressed in Klorin bottle costumes, a truck with a loudspeaker system, soccer tournaments, public product demonstrations, and Klorin quizzes with prizes. Village health promoters received T-shirts, water vessels, or Klorin bottles as incentives for meeting sales targets. To encourage improved water storage, we subsidized the modified clay pots and packaged them with a free bottle of Klorin during the promotional period.
Monitoring
Six months after introducing the Safe Water System, we monitored product adoption in a random sample of 20% of households in 12 project villages. A short questionnaire about water sources, storage, and treatment was administered, and free and total chlorine residuals were determined.
DISCUSSION AND EVALUATION
Water stored in 58 (33.5%) of 173 households had detectable free chlorine residuals, indicating use of Klorin, and 32 (18.5%) of 173 households were using modified clay pots (Table 1 ▶). The adoption rate for chlorination was substantially higher than rates measured in urban projects in other countries, where 5% to 15% is typical (R.E.Q., unpublished data, 1999). This finding was particularly remarkable because of the impoverishment of the communities in this project. Contributing factors include a perceived need for water treatment to prevent diarrhea, interest in chemical disinfection and willingness to pay for it, ease in accessing and using the product, and affordability of the product. The community mobilization and the attendant trust developed by WASEH, and the product awareness created through marketing activities, were also influential.
TABLE 1—
Households With Detectable Free Chlorine Residuals in Stored Water and Households Purchasing a Modified Clay Pot for Water Storage, by Village: Nyanza Province, Kenya, March 2001
| Village | No. of Households Interviewed | No. (%) With Detectable Free Chlorine in Stored Water | No. (%) Purchasing Modified Clay Pot |
| Minyere C | 14 | 0 (0) | 0 (0) |
| Ariri | 5 | 2 (40) | 0 (0) |
| Nyasanja | 8 | 0 (0) | 1 (12.5) |
| Nyobongo | 30 | 2 (6.7) | 11 (36.7) |
| Magoria | 17 | 5 (29.4) | 3 (17.6) |
| Gamba | 8 | 2 (25) | 2 (25) |
| Kaditonje | 9 | 2 (22.2) | 5 (55.6) |
| Kaluoch | 10 | 3 (30) | 1 (10) |
| Ogando Central | 13 | 7 (53.8) | 0 (0) |
| Disii | 17 | 6 (35.3) | 7 (41.2) |
| Olasi | 17 | 13 (76.5) | 1 (5.9) |
| Ongero A | 25 | 16 (64) | 1 (4) |
| Total | 173 | 58 (33.5) | 32 (18.5) |
Adoption rates for the modified clay pots, though lower than for the disinfectant solution, were no less remarkable, because the pots were substantially more expensive than the solution. The purchase price of nearly US $2.53 represents as much as 3 or 4 days' earnings for this population. A strong local preference for clay pots, improved design, ease of use, local access, effective promotion, affordability, and community mobilization influenced the outcome.
In spite of the overall success of the project, adoption rates were 0 in 2 villages for the disinfectant and in 3 villages for the modified clay pots. Because cultural factors that are sometimes difficult to ascertain can hinder diffusion of innovations,4 additional study is needed to determine how to promote this intervention more effectively.
NEXT STEPS
Despite the good early outcome, 2 major areas of concern remain. First, these safe water handling and storage practices must be maintained and made routine. Achieving this objective will require continuous monitoring, active promotion and community mobilization, and ongoing access to the products.5 Second, project costs must be at least partially recovered. Monitoring trends in product use will help direct marketing activities. Similarly, monitoring adoption of Klorin and modified pots and following up with focus group discussions will help identify factors that motivate or hinder adoption. Evaluating health impacts will also determine the project's effectiveness.
The project must continue to look for opportunities to expand. In particular, the commercial sector should be exploited, and partnerships with other community development agencies should be established.5 Models for combining social marketing with community mobilization should be more fully developed to encourage wide dissemination and improve penetration in target communities.6
HIGHLIGHTS
• The Nyanza Healthy Water Project promoted water treatment and safe storage through an approach that combined community mobilization and social marketing.
• Because the local population preferred using clay pots for water storage, rather than plastic jerry cans, the pots were modified for safe storage and field-tested.
• During the first 4 months of the project, one third of the population purchased and used water disinfectant, and one fifth purchased modified clay pots.
Figure 4.
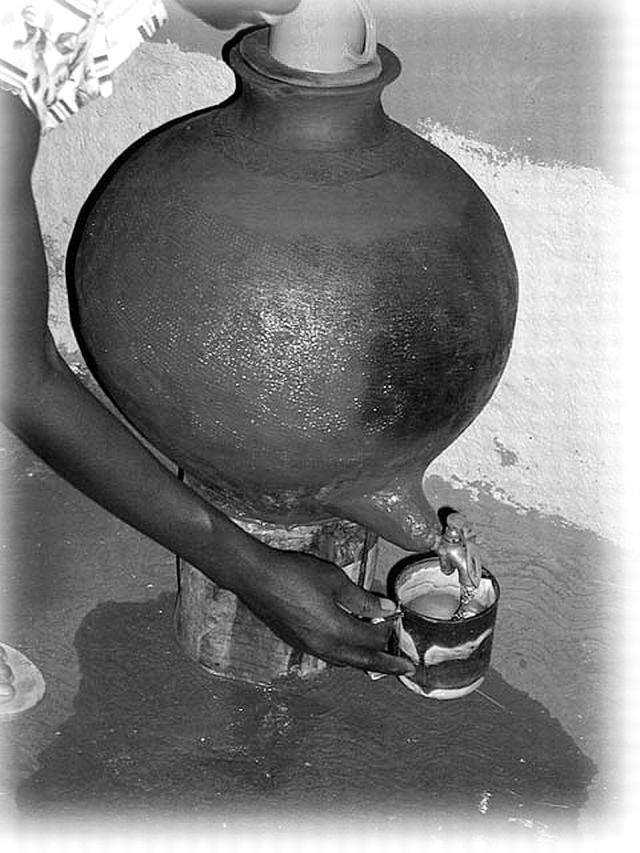
Figure 1.

Women from the Oriang Women Pottery Group in Rachonyu District, Nyanza Province, Kenya, demonstrate clay pots with narrow mouths, fitted lids, and spigots that they made for CARE's Nyanza Healthy Water Project. (Photo: Robert E. Quick.)
Figure 2.
Five-hundred–mL and 1-L Klorin bottles: Nyanza Healthy Water Project, Kenya, March 2001. (Photo: Robert E. Quick.)
Figure 3.
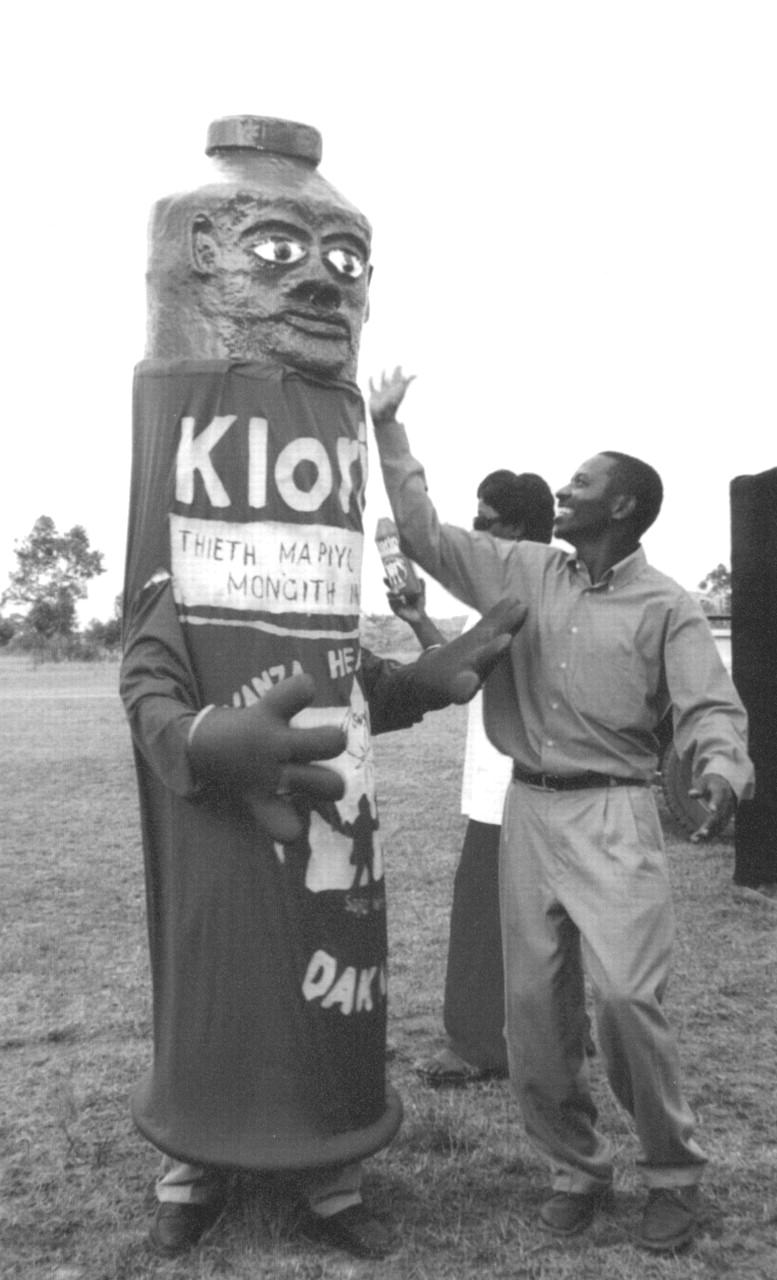
Chlorine bottle costume worn by CARE Kenya personnel to promote use of water disinfectant in social marketing project. (Photo: Robert E. Quick.)
Acknowledgments
All authors contributed to the project's design, implementation, and evaluation and to writing the report.
Resources for this research were provided by the R. W. Woodruff Foundation to CARE and the CDC Foundation, as part of the CARE–CDC Health Initiative. Additional assistance was provided by the US Agency for International Development through its funding of the Dak Achana program.
We thank Patricia Riley, Dr Luke Nkinsi, Reema Jossy, and Lori Buhi of the CARE–CDC Health Initiative and Dr Adam Koons and George Kidenda of CARE Kenya for their support. We are grateful for the editorial support provided by Gwen Ingraham. We appreciate the hard work and dedication of CARE's Dak Achana staff. We are especially grateful for the cooperation and enthusiasm of the community members of project villages in Suba, Homa Bay, and Rachuonyo districts.
Peer Reviewed
References
- 1.Safe Water Systems for the Developing World: A Handbook for Implementing Household-Based Water Treatment and Safe Storage Projects. Atlanta, Ga: Centers for Disease Control and Prevention; 2000. Also available at: http://www.cdc.gov/safewater. Accessed July 3, 2001.
- 2.Ogutu PO, Garrett VB, Barasa PM, Ombeki GS, Mwaki KA, Quick RE. Seeking safe storage: a comparison of drinking water quality in clay and plastic vessels. Am J Public Health. 2001;91:1610–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wood S, Sawyer R, Simpson-Hebert M. PHAST Step-by-Step Guide: A Participatory Approach for the Control of Diarrhoeal Disease. Geneva, Switzerland: World Health Organization; 1998.
- 4.Rogers EM. Diffusion of Innovations. 4th ed. New York, NY: Free Press; 1995.
- 5.Rudd R, Goldberg J, Dietz W. A five-stage model for sustaining a community campaign. J Health Commun. 1999;4:37–48. [DOI] [PubMed] [Google Scholar]
- 6.Bryant CA, Forthofer MS, Brown KR, Landis DC, McDermott RJ. Community-based prevention marketing: the next steps in disseminating behavior change. Am J Health Behav. 2000;24: 61–68. [Google Scholar]



