Abstract
South Sudan experienced a resurgence of trypanosomiasis (sleeping sickness) in the 1990s. In 1997 in Tambura County, public health officials combined standard mass screening and treatment techniques for infected persons with an additional component—trapping the vectors of the disease. The intent of this integrated approach was to lower the number and concentration of the tsetse flies that spread the disease while reducing the level of infection in the human population to make the likelihood of transmission extremely low.
Because the trapping project depends on village participation (making, setting, and maintaining the traps), village volunteers and their neighbors learned more about the causes and prevention of sleeping sickness and became much more willing to participate in serosurveys and to seek treatment.
HUMANS, LIVESTOCK, AND game animals are all hosts for the causative organism of sleeping sickness (Trypanosoma brucei gambiense), which is transmitted through the bite of an infected tsetse fly (Glossina species). For this reason, the most effective known measure for controlling sleeping sickness in humans is not vector control but treating infected persons with drugs until the infection disappears. This practice has been used since epidemics of sleeping sickness were first documented in the region, in the early years of the 20th century.
Study Area
Tambura County is in the southwestern part of the Western Equatoria region of South Sudan, in a zone of endemic human trypanosomiasis. The humid climate—there is a warm, rainy season from April to October and a dry season from November to March—tends to create favorable breeding sites for the tsetse fly. Tambura County borders the Democratic Republic of Congo and the Central African Republic. These borders are crossed regularly and easily by residents of the region, and sleeping sickness is present in all 3 countries.
In 1997, following reports of unusual numbers of cases of human trypanosomiasis (sleeping sickness) in South Sudan, the Cooperative for Assistance and Relief Everywhere (CARE), the International Medical Corps, and the US Centers for Disease Control and Prevention (CDC) began to conduct cluster surveys to determine the prevalence of this serious and potentially deadly infection. In some areas, up to 20% of the local population tested positive for the disease organism.1 These results led to a concerted public health response based on screening, treatment, and prevention.
The 1997 seroprevalence survey results were used to identify the foci of infection and villages with elevated levels of seroprevalence for inclusion into the vector control project. Medical Emergency Relief International, with support from the CARE–CDC Health Initiative, conducted an entomologic assessment to identify the particular tsetse fly vector, sites of intense human–vector contact, and most appropriate trap design for Tambura County before establishing the vector control program (Medical Emergency Relief International, unpublished reports, January–August 1998).
National health officials were trained in tsetse fly biology and control methodology, and a training-the-trainers program was established. Intense community mobilization was carried out prior to community selection of volunteers. County health officials trained these volunteers to be trap monitors and worked with volunteers to prepare maps of villages with key sites for trap placement. Supervisory trap monitors received bicycles to enable them to collect and submit caught flies to county health officials. These officials, in collaboration with CARE, monitored (and continue to monitor) fly density. Together with the communities, they have taken responsibility for the tsetse fly control project.
The traps are simple pyramid-shaped structures made from black and blue cloth by local tailors and women's groups. They can be suspended from trees or bushes. Flies are attracted to the trap colors; they alight, are trapped, and eventually die. The traps are placed near village farm plots, water sources, and areas in which people gather firewood, all places of increased human–vector contact. The cost to maintain a trap for 1 full year is about 2000 Sudanese pounds (US $4.00).
Between 1997 and 2001, 3250 traps were crafted and set up in areas of highest known concentration of tsetse flies. The number of flies trapped dropped from 25 per trap per week at the beginning of the project to fewer than 3 flies per trap per week at the time this report was written (see graph on p 1585).
An aggressive program to identify and treat persons with sleeping sickness was also conducted. In 1997, the prevalence of sleeping sickness in Tambura County was almost 9%. By the end of 1999, the prevalence of sleeping sickness in the county had been reduced to less than 2%. Although it is not possible to document a cause-and-effect relationship between the trapping activities and the reduced prevalence of infection, it is reasonable to postulate that the trapping project has increased local interest in monitoring the disease and participating in prevention and treatment efforts.
DISCUSSION AND EVALUATION
Important components of this vector control program include the simplicity of the trap design; the ease with which traps can be made, set up, and maintained; and the key role of village volunteers in conducting the trapping activities. More than 350 volunteers (mostly recruited among traditional birth attendants) have been trained in making, setting up, and monitoring the traps. Their participation has brought this group of volunteers the additional benefit of increased status in the villages. Where once there was difficulty in recruiting trainees, owing to ignorance, war, and a lack of volunteerism, there is no longer any such difficulty.
The project to control sleeping sickness in Tambura County demonstrates the importance of actively engaging local participation rather than imposing solutions on the population affected by a health problem. When people understand how a health problem occurs and have some economical and practical means to combat the problem, they are likely to raise their level of participation in efforts to increase their own well-being and the well-being of villagers yet to be born.
The combination of treatment, prevention, and locally sustained effort can reduce the serious public health problem that sleeping sickness represents in South Sudan. In the past, entire villages have disappeared because of repeated epidemics of sleeping sickness, all beyond the outside world's awareness. We hope that this situation can be prevented in the future and that sleeping sickness will become a part of Africa's melancholy past but not part of its optimistic future.
NEXT STEPS
Sleeping sickness will continue to be a serious public health problem in this region unless the Democratic Republic of Congo and the Central African Republic provide similar interventions to address the problem. Cross-border movement into South Sudan by infected persons seeking treatment adds to the already overloaded health delivery system in Tambura County.
This model of collaboration should be intensified among all nongovernmental organizations involved in sleeping sickness interventions. An integrated approach to control that includes community-based vector control (when appropriate) should be emphasized. Involvement of women's groups at the village level is crucial to the success of this type of prevention effort.
KEY FINDINGS
• To trap the vectors of trypanosomiasis (sleeping sickness) in Tambura County, South Sudan, more than 3000 pyramidal traps made locally and maintained by volunteers were placed at sites where people were likely to come into contact with tsetse flies.
• Between 1997 and 1999, the seroprevalence of sleeping sickness in Tambura County villages in which screening, drug treatment, and vector control activities were being conducted dropped from almost 9% to less than 2%.
• The vector control intervention received enthusiastic community support. It increased local awareness of the importance of participating in screening and of compliance with treatment recommendations.
Figure 5.
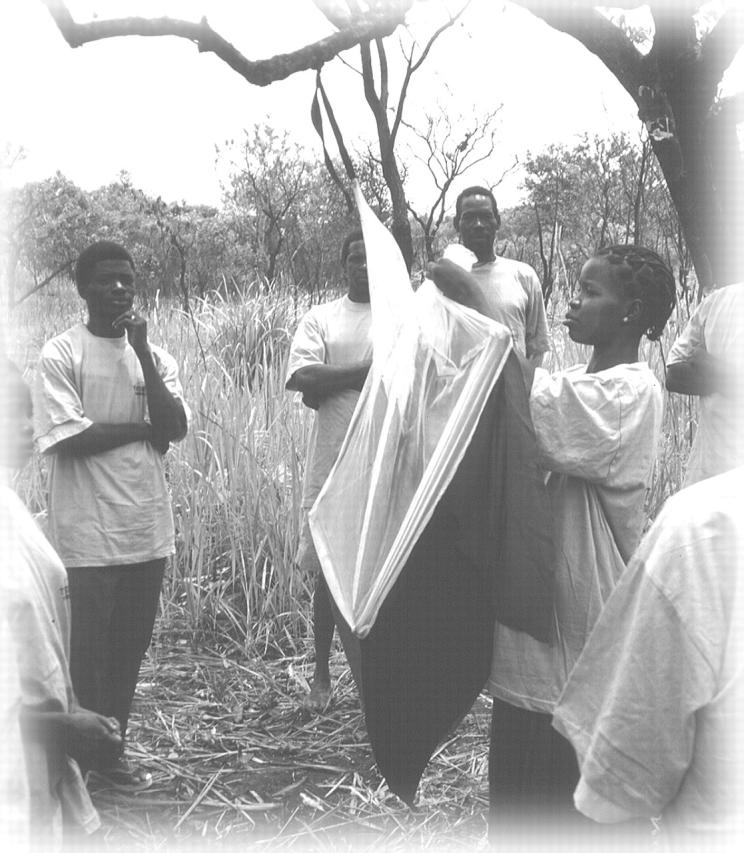
Figure 1.
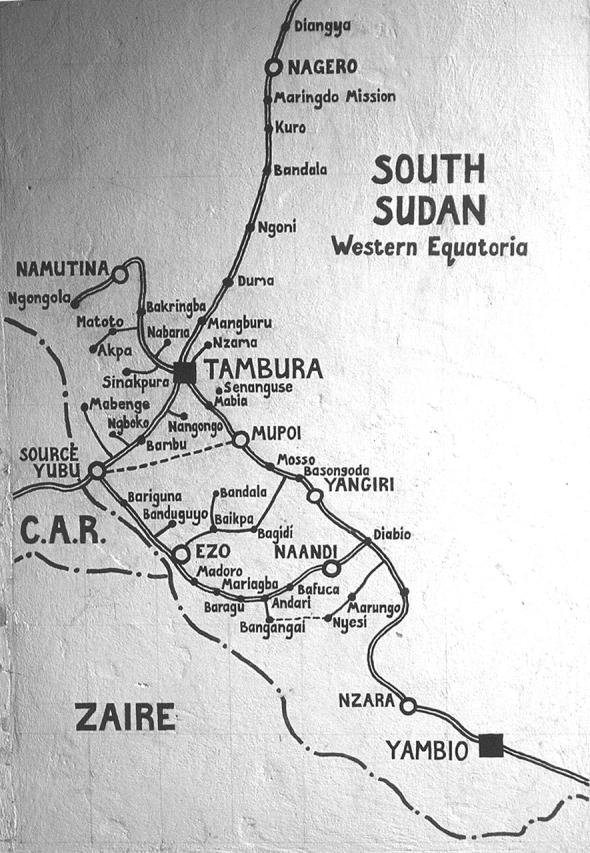
Location of community-based vector-trapping project: Tambura County, South Sudan, 1997– 2001.
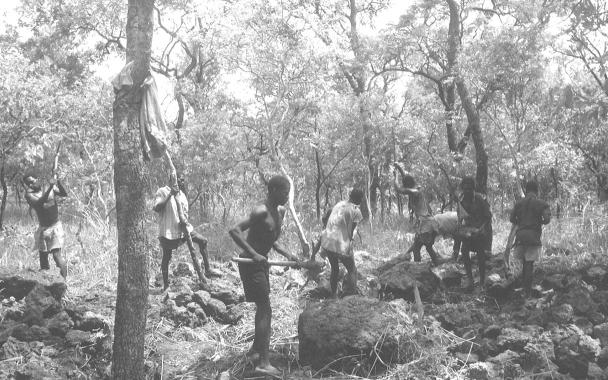
Figure 2.
Below. Field workers from Naandi village, south of Tambura County. The regional economy is based upon subsistence agriculture. (Photo: Lasu Lauya Joja.)
Figure 3.
Above. Thatched housing is common in Tambura County, South Sudan. Community members are sometimes exposed to tsetse fly bites within these house, especially when vegetation is not cleared around the compound. (Photo: Lasu Lauya Joja.)
Figure 4.
Number of traps deployed and number of tsetse flies trapped: community-based vector-trapping project, Tambura County, South Sudan, February 1997–June 2001.
Acknowledgments
This work is supported by the CARE– CDC Health Initiative and CARE Africa Fund (grant US 138-001), the Office of Foreign Disaster Assistance (grant AOT-G-00-97-00382-00), and Australian Aid for International Development (grant AUSAID/05983/14). Resources for this research were also provided by the R. W. Woodruff Foundation to CARE and the CDC Foundation, as part of the CARE–CDC Health Initiative.
The authors wish to acknowledge the invaluable technical and editorial assistance provided by Dr Anne Moore and Elliott Churchill. We would like to express our sincere appreciation to CARE Somalia and South Sudan, the Tambura suboffice and primary health care staff; the Tambura County Primary Health Care Department; and the Sudan Relief and Rehabilitation Association in Tambura County for their continued support of this project.
L. L. Joja trained and monitored the local health personnel on vector control measures. U. A. Okolo initiated the vector control program and trained the local health personnel.
Peer Reviewed
Reference
- 1.Moore A, Richer M, Enrile M, Losio E, Roberts J, Levy D. Resurgence of sleeping sickness in Tambura County, Sudan. Am J Trop Med Hyg. 1999;61: 315–318. [DOI] [PubMed] [Google Scholar]