Abstract
The accomplishments of Latin American social medicine remain little known in the English-speaking world. In Latin America, social medicine differs from public health in its definitions of populations and social institutions, its dialectic vision of “health–illness,” and its stance on causal inference.
A “golden age” occurred during the 1930s, when Salvador Allende, a pathologist and future president of Chile, played a key role. Later influences included the Cuban revolution, the failed peaceful transition to socialism in Chile, the Nicaraguan revolution, liberation theology, and empowerment strategies in education. Most of the leaders of Latin American social medicine have experienced political repression, partly because they have tried to combine theory and political practice—a combination known as “praxis.”
Theoretic debates in social medicine take their bearings from historical materialism and recent trends in European philosophy. Methodologically, differing historical, quantitative, and qualitative approaches aim to avoid perceived problems of positivism and reductionism in traditional public health and clinical methods. Key themes emphasize the effects of broad social policies on health and health care; the social determinants of illness and death; the relationships between work, reproduction, and the environment; and the impact of violence and trauma.
ALTHOUGH SOCIAL MEDICINE has become a widely respected field of research, teaching, and clinical practice in Latin America, the accomplishments of this field remain little known in the English-speaking world. This gap in knowledge derives partly from the fact that important publications remain untranslated from Spanish or Portuguese into English. In addition, the lack of impact reflects a frequently erroneous assumption that the intellectual and scientific productivity of the Third World manifests a less rigorous and relevant approach to the important questions of our age.
In this article, we describe the history of the field, depict the challenges of leadership and daily work activities, and analyze the debates, theoretic approaches, methodological techniques, and major themes emerging from Latin American social medicine. We also present Latin American perspectives on the definition of social medicine and on the perceived differences between social medicine and traditional public health. A separate article presents a critical review of work conducted at the major centers of social medicine in Argentina, Brazil, Chile, Colombia, Cuba, Ecuador, and Mexico.1 Our methods included a review of publications and unpublished literature in Spanish and Portuguese, a study of archives, and focused, in-depth interviews with leaders, health care practitioners, and lay participants in social medicine programs. (A summary of the methods can be obtained from the corresponding author or at the Web site http://hsc.unm.edu/lasm.)
HISTORICAL DEVELOPMENT
Most Latin American accounts of social medicine's history emphasize its origins in Europe.2,3 Such historical accounts usually cite the work of Rudolf Virchow in Germany.4 Especially through his political activism in the reform movements that culminated in the revolutions of 1848, Virchow initiated a series of influential investigations concerning the effects of social conditions on illness and mortality. Presenting pathologic observations and statistical data, he argued that the solution of these problems required fundamental social change. Virchow defined the new field of social medicine as a “social science” that focused on illness-generating social conditions.5–7
Adherents of Virchow's vision immigrated to Latin America near the turn of the 20th century. Virchow's followers helped establish departments of pathology in medical schools and initiated courses in social medicine. For instance, a prominent German pathologist, Max Westenhofer, who directed for many years the department of pathology at the medical school of the University of Chile, influenced a generation of students, including Salvador Allende, a medical student activist, pathologist, and future president of Chile.8
Salvador Allende and the “Golden Age” of Social Medicine in Chile
Although the roots of Chilean social medicine date back to the mid-19th century, the most sustained activities began after the nationwide strikes of 1918. During that year, saltpeter workers in the northern desert encouraged work stoppages in other industries, with the goal of improving wages, benefits, and working conditions. Luis Emilio Recabarren, a charismatic organizer among the saltpeter workers, emphasized the destructive effects of malnutrition, infectious diseases, and premature mortality. During the next 3 decades, Recabarren and his political allies agitated for economic reforms as the only viable route to improvements in patterns of illness and mortality that affected the poor. During the 1920s and 1930s, social medicine flourished in Chile, partly as a response to the demands of the labor movement.
Allende's experiences as a physician and pathologist shaped much of his later career in politics. Acknowledging debts to Virchow and others who studied the social roots of illness in Europe, Allende set forth an explanatory model of medical problems in the context of underdevelopment. Although parallel activities in social medicine were occurring during the same period in North America and Europe,9,10 these developments do not appear to have directly influenced Allende's work.
Writing in 1939 as minister of health for a newly elected popular front government, Allende presented his analysis of the relationships between social structure, disease, and suffering in his classic book, La Realidad Médico-Social Chilena (The Chilean Medico-Social Reality).11 This book conceptualized illness as a disturbance of the individual fostered by deprived social conditions. Breaking new ground in Latin America at the time, Allende described the “living conditions of the working classes” that generated illness. He emphasized the social conditions of underdevelopment and international dependency, as well as the effects of foreign debt and the work process. In this book, Allende focused on several specific health problems, including maternal and infant mortality, tuberculosis, sexually transmitted and other communicable diseases, emotional disturbances, and occupational illnesses. Describing issues that had not been studied previously, he analyzed illegal abortion, the responsiveness of tuberculosis to economic advances rather than innovations in treatment, housing density in the causation of infectious diseases, and differences between generic and brand-name pricing in the pharmaceutical industry.
The Ministry of Health's proposals that concluded La Realidad Médico-Social Chilena took a unique direction by advocating social rather than medical solutions to health problems. Allende proposed income redistribution, state regulation of food and clothing supplies, a national housing program, and industrial reforms to address occupational health problems. Rather than seeing improved health care services as a means toward a more productive labor force, Allende valued the population's health as an end in itself and advocated social changes that went far beyond the medical realm.
Allende's analytic position in social medicine lay behind much of his political work until his death in 1973 during the military coup d'état. In addition to the work of Virchow and Westenhofer in pathology, the Civil War in Spain influenced Allende, as it did many later practitioners of social medicine in Latin America. The struggle against fascism and for a more egalitarian society in Spain during the late 1930s led to a movement for improved public health among activists in the exiled Spanish Republican community. Allende and his supporters incorporated principles from the Spanish public health movement into their efforts for change in Chile.
As an elected senator in the early 1950s, Allende introduced the legislation that created the Chilean national health service, the first national program in the Americas that guaranteed universal access to services. He linked this reform to other efforts that aimed to achieve more equitable income distribution, job security, improved housing and nutrition, and a less dominant role for multinational corporations within Chile. Similarly, as a senator during the 1960s and elected president between 1970 and 1973, Allende sought reforms in the national health service and other institutions that would have achieved structural changes throughout society. Because of his advocacy of a unified health service in the public sector, the Chilean national medical association (Colegio Médico) feared the effects of Allende's policies on private practice and therefore frequently opposed him, especially before the coup of 1973.
Social Medicine vs Public Health Elsewhere in Latin America
Other Latin American countries did not advance as far in adopting the perspectives and activism that characterized Chile during the 1930s. Public health efforts throughout Latin America, as clarified recently by several major investigations,12–18 provided a background to which contemporary practitioners of social medicine responded. For instance, leaders of social medicine in many Latin American countries reacted critically to the Rockefeller Foundation's public health initiatives, which emphasized the productivity of labor in enhancing the ventures of US-based multinational corporations.19–21 However, from our literature review and interviews, we conclude that the early history of social medicine in some countries proved much more influential than in others. Although substantial early public health efforts occurred in Brazil, Colombia, Cuba, and Mexico, current leaders in social medicine view the influence of these attempts as less important for social medicine than those in Chile, Argentina, and Ecuador.
Both historically and currently, leaders in Latin America have distinguished social medicine from traditional public health.
Both historically and currently, leaders in Latin America have distinguished social medicine from traditional public health. From this perspective, public health tends to define a population as a sum of individuals. Specific characteristics, such as sex, age, education, income, and race/ethnicity, permit the classification of these individuals into groups. In traditional epidemiology, rates for a population are calculated arithmetically from the characteristics of individuals who compose the population. By contrast, much work in social medicine envisions populations, as well as social institutions, as totalities whose characteristics transcend those of individuals.4 Social medicine therefore defines problems and seeks solutions with social rather than individual units of analysis. In this way, the population can be analyzed through such categories as social class, economic production, reproduction, and culture, not simply through the characteristics of individuals.22–24
Another distinction between social medicine and traditional public health concerns the static vs dynamic nature of health vs illness, as well as the effect of social context. Social medicine conceptualizes “health–illness” as a dialectic process rather than a dichotomous category. As in Eng-els's earlier and Levins and Lewontin's more recent interpretations of dialectic processes in biology,25,26 critical epidemiologists have studied disease pro-cesses in a contextualized model, considering the changing effects of social conditions over time. The epidemiologic profile of a society or group within a society requires a multilevel analysis of how social conditions such as economic production, reproduction, culture, marginalization, and political participation affect the dynamic process of health– illness. In this theoretic vision, multivariate models in public health (such as recent logistic regression models with disease as a dependent variable, dichotomized as either present or absent) obscure health–illness as a dialectic process.27
By contrast, in Argentina during the 1920s, a group led by Juan B. Justo tried to go beyond the public health initiatives of the time, known as “hygienic” interventions (higienismo), which emphasized infection control, improved sanitation, nutrition, and similar efforts to improve population health.28 Higienismo usually aimed to improve labor force productivity, in the interest of national development and international investment. Justo, a surgeon, became a founding leader of the Socialist Party and provided an early Spanish translation of Marx's Capital. Like Allende, Justo called attention to the pervasive effects of social class on health services and outcomes.29 This work led to regional and national organizing efforts that sought broad social change as the basis of improved health. However, as higienismo gained dominance, Justo's was a minority position.
Another line of work in social medicine that grew from Argentine roots was that of Ernesto (“Che”) Guevara. Guevara's childhood asthma, as well as role models in his family, led him to enter medical school and eventually to specialize in allergic diseases. After medical school, he toured South America, Central America, and Mexico by motorcycle. Through experiences of poverty and suffering during this trip, he developed his views about the need for revolution as a prerequisite for improving health conditions.30
In his speeches and writings on “revolutionary medicine,” Guevara called for a corps of physicians and other health workers who understood the social origins of illness and the need for social change to improve health conditions.31,32 Guevara's work profoundly influenced Latin American social medicine. One might expect that Guevara's views developed partly from knowledge about Allende, Justo, and others who preceded him, but apparently this was not the case. Sources close to Guevara, including an uncle who served as a role model in medicine, claimed that throughout his medical training and career Guevara remained unexposed to earlier works in Latin American social medicine and that he developed his analysis linking health outcomes with social conditions largely through experiences during his motorcycle trip (Francisco Lynch Guevara, oral communication, Buenos Aires, Argentina, 1995).
In Ecuador, leaders in social medicine trace their local roots back more than 150 years. During the early 19th century, the physician Eugenio Espejo linked his work as a physician to the revolutionary struggles against Spain.33 In his efforts to control epidemics, Espejo became convinced, as Virchow later would in Germany, that poverty, inadequate housing and sanitation, and insufficient nutrition fostered such outbreaks. Later, in the early 20th-century movement toward social security, Pablo Arturo Suárez's book on “the situation of the working class” provided epidemiologic data on adverse health outcomes.34 During the 1930s, the physician Ricardo Paredes studied occupational lung diseases and accidents among Ecuadoran miners working at a US-owned mining company.35 In addition to legislation that improved working conditions, Paredes's efforts led to a broad consciousness in Ecuador of the effects on health of “economic imperialism” by multinational corporations.
The 1960s and Later
Among the changes that occurred worldwide during the 1960s, the Cuban revolution, which began in 1959, emerged as one of the most important for social medicine. Cuba's improved public health system emerged as part of a social revolution in which accomplishments in health occurred as an integral part of broad structural changes in the society as a whole.36,37 The social changes underlying Cuba's achievements in primary care, public health, medical education, planning and administration, and epidemiologic surveillance inspired activists and scholars in other countries.
If Cuba provided a positive model for Latin American social medicine, Chile created ambivalence. Social medicine groups took a keen interest when Allende and the Unidad Popular government achieved victory in 1970. Many people in social medicine came to Chile to work with the new government. Allende had proposed a peaceful transition to socialism through electoral rather than military means—the first such transition in history. The government moved toward a “unified” national health program, in which the contradictions of coexisting private and public sectors would be reduced. After the violent coup d'état of 1973, repression of the population and especially of health workers reached unprecedented levels of violence.38,39 The failure of the peaceful road to socialism left a mark on those throughout Latin America who pursued social medicine.
Nicaragua's revolution of 1979 also inspired social medicine activists, although many worried about the health-related social policies of the Sandinista government. Leaders of social medicine from several countries contributed to the new Nicaraguan government's health reforms, including extensive programs that dealt with infectious diseases and with maternal and child health.40,41 These leaders' concerns, which were never published, focused on the contradictions of the Nicaraguan revolution, which, for instance, permitted a continuing major role for private practice, even for health professionals who worked full-time for the national health service. Government representatives argued that such policies enhancing the private sector of the economy would prevent an exodus of health professionals similar to the one that had occurred in Cuba. Owing to such contradictions, some social medicine leaders eventually reduced their support activities, especially after the Sandinistas' electoral losses.
Liberation theology became a source of inspiration for many of social medicine's activists.
Liberation theology became a source of inspiration for many of social medicine's activists. Priests such as Frei Betto in Brazil advocated participation in “base communities,” which fused religious piety with struggles for social justice.42 These struggles included efforts to improve health and public health services. Certain leaders of liberation theology grew skeptical about nonviolent processes in base communities. Influenced by Camilo Torres, a priest who joined the revolutionary movement in Colombia, some social medicine activists entered armed struggle in several countries and later returned to the practice of social medicine.43
Another important influence on social medicine stemmed from the educational innovations of Paulo Freire and coworkers in Brazil. Through adult literacy campaigns, Freire encouraged people in poor communities to approach education as a process of empowerment. In the efforts that led to his classic book, Pedagogy of the Oppressed,44 Freire fostered the organization of small educational “circles,” by which local residents could link their studies to the solution of concrete problems in their communities. Activists later began to extend this approach to public health education and organizing to improve health services.45 Freire himself became more interested in applications of empowerment strategies to health.46 While Freire's orientation also has affected public health in the United States,47,48 the impact proved even greater in Latin American social medicine.
During the 1970s, a leader emerged who profoundly affected the course of social medicine from a base in Washington, DC. Trained as a physician in Argentina and as a sociologist in Chile, Juan César García served as research coordinator within the Pan American Health Organization (PAHO) from 1966 until his death in 1984. García himself produced seminal works on medical education, the social sciences in medicine, social class determinants of health outcomes, and the ideologic bases of discrimination against Latinos.49–52 Although his Marxist social philosophy manifested itself in several works published under his own name while he was working for PAHO, he also published more explicitly political articles under pseudonyms (A. Mier, unpublished observations, 1975).
García affected social medicine through the financial and socioemotional support that he provided through PAHO. With his colleague at PAHO, María Isabel Rodríguez, who was living in exile after serving as dean of the school of medicine at the University of El Salvador, García orchestrated grants, contracts, and fellowships that proved critical for social medicine groups throughout Latin America. PAHO funding helped establish the first influential training program in social medicine at the Autonomous Metropolitan University, Xochimilco, in Mexico City, which attract-ed students from throughout Latin America. Current leaders consistently refer to García's initiative and tenacity, despite opposition that he increasingly received within PAHO.
In advocating social medicine, García helped distribute Spanish-language translations of works by Vicente Navarro. These works influenced Latin American social medicine with regard to the effects of capitalism, imperialism, and maldistribution of economic resources on health services and outcomes. The International Journal of Health Services, edited by Navarro, provided an English-language forum for Latin American authors.
POLITICAL REPRESSION AND WORK CHALLENGES
Among the 24 in-depth interviews with leaders of social medicine that we conducted, only 4 respondents denied having suffered some form of political repression. Respondents have experienced repression because of their work in Chile's Unidad Popular government, their activity in human rights, or their role as health care activists. The forms of repression have included torture, imprisonment in concentration camps, exile, exclusion from government jobs, loss of economic security and work stability, loss of professional prestige, and restriction of political activity.
The work process in social medicine varies widely, depending on political and economic conditions. From Chile and Argentina, most leaders of social medicine took refuge in other countries. These refugees from South America's southern cone made major contributions to the dissemination of social medicine while they were living and working abroad. If people remained within their homelands, they usually supported themselves through clinical laboratory work, market research, or retail sales. Since the fall of the dictatorships, people in social medicine have faced great difficulties in attempts to reintegrate themselves into universities or medical schools. Most hold multiple jobs, usually in clinical or administrative work, and pursue social medicine as largely unpaid activities.
In countries without dictatorships, or where dictatorships proved somewhat less brutal, such as in Brazil, fewer people needed to emigrate and more remained at work in universities or teaching hospitals. In Colombia, owing to a tradition of violence, prominent leaders of social medicine have perished or entered exile despite the presence of elected governments. In other countries such as Mexico, Ecua-dor, and Cuba, participants in social medicine have been able to maintain relatively stable academic positions. Currently, the most favorable institutional conditions for social medicine exist in Mexico, Ecuador, Brazil, and Cuba. Although conditions in Argentina, Chile, and Colombia remain more adverse, participants in social medicine struggle to achieve high levels of productivity.
THEORY, METHOD, AND DEBATE
Latin American social medicine has developed into a rich and diverse field rather than a single, homogeneous tradition. Intense debates have focused on theory, method, and strategies for change.53 For instance, theoretic debates have questioned the usefulness of traditional Marxist analysis as opposed to more recent theories. Theoretic differences also have focused on the primacy of economic forces vs other issues such as gender and race/ethnicity. Methodological debates have considered the balance between quantitative and qualitative methodologies in research, as well as individuals vs groups as units of analysis. Strategically, practitioners of social medicine have differed widely in their willingness to collaborate with international health organizations and multilateral lending agencies.
If there is one commonality that distinguishes the field, however, it is an emphasis on theory. Practitioners of social medicine have argued that a lack of explicitly stated theory in North American medicine and public health does not signify an absence of theory. Instead, an atheoretic or antitheoretic stance means that the underlying theory remains implicit. Latin American critics have used this prism to interpret the North American tendency to focus on the biological rather than social components of such problems as cancer, hypertension, and occupational illnesses. The biological focus, from this perspective, reduces the unit of analysis to the individual and thus obscures social causes amenable to societal-level interventions.27,54
Referring to the linkage between theory and practice, practitioners of social medicine frequently use the term “praxis.” Influenced by Gramsci's work in Italy, Latin American leaders have emphasized theory that both informs and takes inspiration from efforts toward social change.45,55 Research and teaching activities often take place in collaboration with labor unions, women's groups, Native American coalitions, and community organizations.56
If there is one commonality that distinguishes the field [of social medicine], it is an emphasis on theory.
Although Marxist theory has stimulated social medicine, conceptual work has focused on the strengths and limitations of traditional Marxism in the Latin American context. Adverse experiences in socialist countries like the Soviet Union also have revealed the limited applicability of traditional Marxist theory.57 Certain components of Marxist theory, however, have continued to ground conceptual work and research.
First, social medicine has emphasized social class, as defined by the relations of economic production. In Marxist theory, the most important characteristic of social class involves ownership and control of the productive process.58 Practitioners of social medicine have argued that the exploitation of labor remains an inherent condition of economic production, especially in less developed countries. As a result, they have maintained a vision of social class rooted in economic production rather than in such demographic characteristics as income, education, and occupational prestige. This theoretic position concerning economic production has led to the choice of research questions that focus on the labor process itself in both industrial and agricultural settings. The social medicine groups in Mexico, Chile, Ecuador, and Brazil have initiated studies of work hierarchies, the production process in factories, and the impact of work conditions on health and mental health outcomes.
A second focus involves the reproduction of economic production. Marxist theory questions how the capitalist system can justify reproducing the inherently exploitative relations of production across generations. Among the supporting institutions that accomplish this reproduction, the family figures most prominently, especially through the patterning of gender roles. Marx and Engels argued, for instance, that the exploitation of workers was inherently linked to the exploitation of women, since economic production required the reproduction of the labor force, mainly through the activities of women within families.59 In contemporary societies, women often bear the “triple burden” of wage labor, housework, and child-rearing. For that reason, social medicine groups in several countries have collaborated in research that focuses on women workers and the effects of their roles in economic production and reproduction.60
Ideology, a third theoretic focus, comprises the distinctive ideas and doctrines of a social group. Some Latin American theorists in social medicine have adopted Althusser's perspective in arguing that ideology represents individuals' imagined relationship to the material conditions of their existence.61 A “hegemonic” ideology tends to justify the interests of the class that dominates a society during a specific historical period. Demystification of this dominant ideology then becomes a task for theoretic and political work.62,63 The social medicine groups in Latin America have accepted this task of demystification as a priority. During earlier years, the work of demystification focused on “developmentalist” policies, fostered by North American and European governments.64 More recently, demystification efforts have emphasized the health policies of the World Bank and other multilateral lending agencies. These agencies have encouraged increasing indebtedness, privatization, and cutbacks in public services, based on macroeconomic, market-based principles.65–67
Contemporary European theory also has influenced Latin American social medicine. For instance, theoretic efforts in Italy on the work process have shaped the conceptual approach taken by the Mexican group in collaboration with industrial unions.68 French psychoanalysis and institutional analysis have influenced the efforts of Argentine and Brazilian investigators in their studies of health services.69,70 Philosophical advances in France, partly developed by Argentinians in exile, have informed the critique of ideologies in health policies and proposals for change.71,72
The theory of health–illness as a dialectic process has generated criticisms of traditional approaches to causal inference in medicine and public health.73,74 At a basic level, social medicine practitioners have criticized monocausal explanations of disease. Taking a perspective similar to Virchow's, they maintain that simplistic explanations by which a specific agent causes a specific disease do not adequately consider the social conditions that increase the likelihood of disease. However, even multicausal models, such as those that consider the interactions among agent, host, and environment, still define disease in a relatively static fashion. Critiques from the standpoint of social medicine have argued that by dichotomizing the presence or absence of a disease, traditional multicausal models do not adequately consider the dynamic linkages by which social conditions affect the dialectic process of health–illness. These analyses have suggested a more complex approach to causality, in which social and historical conditions receive more explicit emphasis.
Anticipating current methodological trends in the United States, leaders in Latin American social medicine since the mid-1970s have called for a multimethod approach that “triangulates” complementary methods at both individual and societal levels of analysis. Even in early research, the Mexican and Ecuadoran researchers combined quantitative, multivariate analyses with qualitative, in-depth interviews that they often conducted in group situations (“collective interviews”).75,76 Recent approaches to multilevel research have included quantitative techniques, such as structural equation modeling, combined with qualitative techniques, such as focus groups and computerized content analysis.77
EMERGING THEMES
Social Policies, Power, Health, and Health Care
Social medicine groups throughout Latin America have emphasized the effects of international policies. Historically, such work has analyzed the impact of economic imperialism, the extraction of raw materials, and the exploitation of inexpensive labor. More recently, social medicine groups have focused on international macroeconomic policies and the political power of multinational corporations and lending agencies. The burden of foreign debt in Third World countries has emerged as an issue of grave concern. Public sector cutbacks, privatization of public services, and the opening of markets in health care to multinational corporations have received critical attention. Several groups have collaborated in evaluating managed care as a privatization initiative by multinational corporations and lending agencies. These studies have emphasized the detrimental effects on access to services as the public sector “safety net” deteriorates and have demystified claims that market-oriented practices improve conditions for the poor.66,67,78–82
The social medicine groups have linked their policy research with organizing efforts aiming to change power relationships. These actions try to expand public debate and to redirect reform initiatives toward meeting the needs of vulnerable populations. Social medicine groups have collaborated with the opposition Party of the Democratic Revolution and the Zapatista Army of National Liberation in Mexico, the coalition of indigenous and labor organizations in Ecuador, the Workers Party in Brazil, and the Central Organization of Argentine Trade Unions.
Social and Cultural Determinants of Illness and Death
Several groups have pioneered research on social and cultural determinants. Researchers in Ecuador have focused on urban ecology, economic changes stemming from petroleum production, and the relationships between gender and the work process in explaining morbidity and mortality patterns.83,84 The Ecuadoran group has pioneered the use of multivariate, quantitative techniques to conduct multilevel research on social determinants, using data at the individual, social, and cultural units of analysis.27,77 Brazilian researchers have used multilevel and multimethod approaches—including anthropologic, nonquantitative methods in epidemiology—to clarify mechanisms at the community, family, and biological levels that mediate the impact of social inequalities.85
Work, Reproduction, Environment, and Health
This focus emerges from a theoretic emphasis on economic production and reproduction, as well as a recognition that such problems represent some of the chief threats to health in Third World countries. Mexican researchers have worked with industrial unions and local communities to clarify health and mental health problems that derive from the work process and environment. In this effort, the investigators have pioneered such methods as the collective interview.76,86 The Ecuadoran group has emphasized the differing health outcomes that women experience in industrial and agricultural work environments.83,84 In Chile, the social medicine group has carried out research that links gender, work, and environmental conditions.88 Micro-level research on the work process in Brazilian health institutions has informed the policy efforts of the national Workers Party.88
Violence, Trauma, and Health
Partly reflecting the violent conditions that practitioners of social medicine themselves have confronted, research on violence and trauma has received priority in several countries. In Colombia, the social tradition of violence—previously linked to poverty and cycles of rebellion but more recently reflecting narcotics traffic and paramilitary operations—has generated research on the effects of violence on health outcomes.89,90 Chilean investigators have studied families whose members experienced torture, exile, or death during the dictatorship.91 Influenced by psychologic studies of violence in El Salvador by Ignacio Martín-Baró, a US-trained psychologist who himself was assassinated by paramilitary forces, researchers in Argentina have focused on the survivors of the more than 30 000 individuals who “disappeared” during the Argentine dictatorship.92–94
CONCLUSION
Social medicine in Latin America has emerged as a sometimes dangerous but very productive field of work. A focus on the social origins of illness and early death inherently challenges the relationships of economic and political power in Latin America. As a result, participation in social medicine has led to suffering and even death for some of the movements most talented and productive adherents. The themes and findings of Latin American social medicine have become pertinent for problems in medicine and public health throughout the world. Owing to language barriers and possibly to skepticism about research emanating from the Third World, ignorance prevails among many health professionals whose work could advance if the production of Latin American social medicine were more accessible.
Practitioners of Latin American social medicine have used theories and methods that distinguish their efforts from those of traditional public health. In particular, a focus on the social and historical contexts of health problems, an emphasis on economic production and social causation, and the linkage of research and education to political practice have provided innovative approaches to some of the most important problems of our age. For the United States and other “First World” countries, during an era of globalization and its dangers, the courageous work of Latin American social medicine may become a highly valued import.
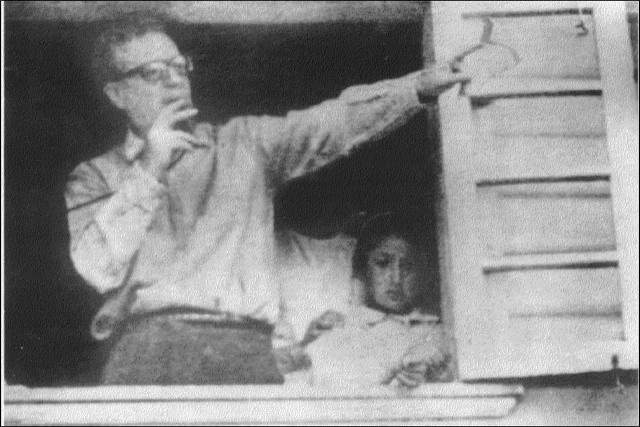
Figure 1.
Salvador Allende, leader of social medicine in Chile, during a political campaign in the late 1940s. (Photograph courtesy of Fundación Salvador Allende.)
Figure 2.
Juan César García (third from left) at social medicine conference in Ecuador, 1983. (Photo courtesy of Edmundo Granda, Ecuador).
Figure 3.
A workshop on research in the social sciences and health: Cuenca, Ecuador, 1983. (Photo courtesy of Edmundo Granda, Ecuador.)
Acknowledgments
H. Waitzkin contributed to the study's design; gathered, analyzed, and interpreted the data; and drafted the article. C. Iriart contributed to the study's design and helped to interpret the data and revise the manuscript. A. Estrada contributed to the study's design, helped to analyze and interpret the data, drafted one section of the article, and helped in revising the manuscript. S. Lamadrid gathered and analyzed data and participated in the revision.
This work was supported in part by grants from the Fulbright Commission (Senior Fellowship for Independent Research, American Republics Program), the Fogarty International Center of the National Institutes of Health (TW 01982), the Pacific Rim Program of the University of California, the American College of Physicians (George C. Griffith Traveling Fellowship), the World Health Organization (Special Programme for Research and Training in Tropical Diseases), the Dedicated Health Research Funds of the University of New Mexico School of Medicine, and the National Library of Medicine (1G08 LM06688).
We are indebted to our many colleagues and friends who offered advice, participated in interviews, and provided examples of courage in pursuing social medicine despite threats to their safety for doing so.
The informed consent procedures for the participation of human subjects in this project were reviewed and approved by the institutional review board at the University of California, Irvine.
Peer Reviewed
References
- 1.Waitzkin H, Iriart C, Estrada A, Lamadrid S. Social medicine in Latin America—productivity and dangers facing the major national groups. Lancet. 2001;358:315–323. [DOI] [PubMed] [Google Scholar]
- 2.Rosen G. De la Política Médica a la Medicina Social. Mexico City, Mexico: Siglo XXI; 1985.
- 3.Foucault M. El nacimiento de la medicina social. Rev Centroam Ciencias Salud. 1977;3(6):89–108. [Google Scholar]
- 4.Franco S, Nunes ED. Presentación. In: Franco S, Nunes E, Breilh J, Laurell C. Debates en Medicina Social. Quito, Ecuador: Organización Panamericana de la Salud; 1991:7–16.
- 5.Virchow R. Gesammelte Abhandlungen aus dem Gebiet der Oeffentlichen Medicin und der Seuchenlehre. Berlin, Germany: Hirschwald; 1879.
- 6.Virchow R. Letters to His Parents, 1839 to 1864. Canton, Mass: Science History Publications; 1990.
- 7.Waitzkin H. The social origins of illness. In: The Second Sickness: Contradictions of Capitalist Health Care. 2nd ed. Lanham, Md: Rowman & Littlefield; 2000:55–73.
- 8.Illanes MA. “En el Nombre del Pueblo, del Estado y de la Ciencia …”: Historia Social de la Salud Pública, Chile 1880–1973. Santiago, Chile: Colectivo de Atención Primaria; 1993.
- 9.Fee E, Brown TM. Making Medical History: The Life and Times of Henry E. Sigerist. Baltimore, Md: Johns Hopkins University Press; 1997.
- 10.Porter D. Health, Civilization, and the State: A History of Public Health From Ancient to Modern Times. London, England: Routledge; 1999. [DOI] [PMC free article] [PubMed]
- 11.Allende S. La Realidad Médico-Social Chilena. Santiago, Chile: Ministerio de Salubridad; 1939.
- 12.Lobato MZ, Álvarez A. Política, Médicos y Enfermedades: Lecturas de la Historia de la Salud en la Argentina. Buenos Aires, Argentina: Editorial Biblos; 1996.
- 13.Cueto M, ed. Salud, Cultura y Sociedad en América Latina. Washington, DC: Organización Panamericana de la Salud—Instituto de Estudios Peruanos; 1996.
- 14.Hochman G. Aprendizado e Difusão na Constituição de Políticas: A Previdência Social e seus Técnicos. Rio de Janeiro, Brazil: Instituto Universitário de Pes-quisas do Rio de Janeiro; 1987.
- 15.Estrella E, Crespo A, Herrera D, Estrella A. Desarrollo Histórico de las Políticas de Salud en el Ecuador, 1967– 1995. Quito, Ecuador: Proyecto Análisis y Promoción de Políticas de Salud; 1997.
- 16.Cueto M. El Regreso de las Epidém-ias: Salud y Sociedad en el Perú del Siglo XX. Lima, Peru: Instituto de Estudios Peruanos; 1997.
- 17.Birn A-E. Skirting the issue: women and international health in historical perspective. Am J Public Health. 1999;89:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Birn A-E, Solórzano A. Public health policy paradoxes: science and politics in the Rockefeller Foundation's hookworm campaign in Mexico in the 1920s. Soc Sci Med. 1999;49:1197– 1213. [DOI] [PubMed] [Google Scholar]
- 19.Brown EF. Rockefeller Medicine Men. Berkeley: University of California Press; 1979.
- 20.Cueto M, ed. Missionaries of Science: The Rockefeller Foundation and Latin America. Bloomington: Indiana University Press; 1994.
- 21.Franco-Agudelo S. The Rockefeller Foundation's antimalarial program in Latin America: donating or dominating? Int J Health Serv. 1983;13:51–67. [DOI] [PubMed] [Google Scholar]
- 22.Dierckxsens W. Capitalismo y Población: La Reproducción de la Fuerza de Trabajo bajo el Capital. San José, Costa Rica: Editorial Universitaria Centroamericana; 1979.
- 23.Rojas Soriano R. Capitalismo y Enfermedad. Mexico City, Mexico: Folios Ediciones; 1982.
- 24.Rojas Soriano R. Sociología Médica. Mexico City, Mexico: Folios Ediciones; 1983.
- 25.Engels F. Dialectics of Nature. New York, NY: International; 1940.
- 26.Levins R, Lewontin R. The Dialectical Biologist. Cambridge, Mass: Harvard University Press; 1985.
- 27.Breilh J. Componente de metodo-logía: la construcción del pensamiento en medicina social. In: Franco S, Nunes E, Breilh J, Laurell C. Debates en Medicina Social. Quito, Ecuador: Organización Panamericana de la Salud; 1991:138–248.
- 28.Buchbinder M. Rol de lo social en la interpretación de los fenómenos de salud y enfermedad en la Argentina. Salud Problema Debate. 1990;2(4):37–50. [Google Scholar]
- 29.Justo JB. Teoría y Práctica de la Historia. Buenos Aires, Argentina: La Vanguardia; 1933.
- 30.Guevara C. The revolutionary war. In: Gerassi J, ed. Venceremos! The Speeches and Writings of Ernesto Che Guevara. New York: Clarion; 1968: 28–30
- 31.Guevara C. On revolutionary medicine. In: Gerassi J, ed. Venceremos! The Speeches and Writings of Ernesto Che Guevara. New York, NY: Clarion: 1968:112–119.
- 32.Harper G. Ernesto Guevara, MD: physician–revolutionary physician–revolutionary. N Engl J Med. 1969;281: 1285–1289. [DOI] [PubMed] [Google Scholar]
- 33.Espejo E. Voto de un Ministro Togado de la Audiencia de Quito. Quito, Ecuador: Comisión Nacional de Conmemoraciones Cívicas; 1994.
- 34.Suárez PA. Contribución al Estudio de las Realidades entre las Clases Obreras y Campesinas. Quito, Ecuador: Imprenta Fernández; 1934.
- 35.Paredes R. Oro y Sangre en Portocavelo. Quito, Ecuador: Editorial Artes Gráficas; 1938.
- 36.Feinsilver JM. Healing the Masses: Cuban Health Politics at Home and Abroad. Berkeley: University of California Press; 1993.
- 37.Waitzkin H, Wald K, Kee R, Danielson R, Robinson L. Primary care in Cuba: low- and high-technology developments pertinent to family medicine. J Fam Pract. 1997;45:250–258. [PubMed] [Google Scholar]
- 38.Waitzkin H, Modell H. Medicine, socialism, and totalitarianism: lessons from Chile. N Engl J Med. 1974;291: 171–177. [DOI] [PubMed] [Google Scholar]
- 39.Cornely PB, Belmar R, Falk LA, et al. Report of the APHA Task Force on Chile. Am J Public Health. 1977;67: 71–73. [PMC free article] [PubMed] [Google Scholar]
- 40.Garfield R. Health Care in Nicaragua: Primary Care Under Changing Regimes. New York, NY: Oxford University Press; 1992.
- 41.Garfield RM, Frieden T, Vermund SH. Health-related outcomes of war in Nicaragua. Am J Public Health. 1987;77: 615–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Betto F, Castro F. Fidel and Religion: Castro Talks on Revolution and Religion With Frei Betto. New York, NY: Simon & Schuster; 1987.
- 43.Torres C. Revolutionary Priest: The Complete Writings and Messages. New York, NY: Random House; 1971.
- 44.Freire P. Pedagogy of the Oppressed. New York, NY: Herder & Herder; 1970.
- 45.Costa NdR. Transición y movimientos sociales: contribuciones al debate de la reforma sanitaria. Cuadernos Med Soc. 1988;44:51–61. [Google Scholar]
- 46.Freire P. Pedagogy of Freedom: Ethics, Democracy, and Civic Courage. Lanham, Md: Rowman & Littlefield; 1998.
- 47.Wallerstein N, Bernstein E. Empowerment education: Freire's ideas adapted to health education. Health Educ Q. 1988;15:379–394. [DOI] [PubMed] [Google Scholar]
- 48.Magaña R, Ferreira-Pinto JB, Blair M, Mata A. Una pedagogia de concientización para la prevención del VIH/SIDA. Rev Latino Am Psicol. 1992;24:97–108. [PubMed] [Google Scholar]
- 49.García JC. La Educación Médica en la América. Washington, DC: Organización Panamericana de la Salud; 1972.
- 50.García JC. La Investigación en el Campo de la Salud en Once Países de la América Latina. Washington, DC: Organización Panamericana de la Salud; 1982.
- 51.García JC. La Mortalidad de la Niñez Temprana Según Clases Sociales. Medellín, Colombia: Universidad Pontífica Bolivariana; 1979.
- 52.García JC. The laziness disease. History Phil Life Sci. 1981;3:31–59. [Google Scholar]
- 53.Franco S, Nunes E, Breilh J, Laurell C, eds. Debates en Medicina Social. Quito, Ecuador: Organización Panamericana de la Salud; 1991.
- 54.Laurell AC. Social analysis of collective health in Latin America. Soc Sci Med. 1989;28:1183–1191. [DOI] [PubMed] [Google Scholar]
- 55.Gramsci A. The Prison Notebooks. New York, NY: International; 1971.
- 56.Franco S. Tendencias de la medicina social en América Latina. Salud Cambio. 1990;2:4–16. [Google Scholar]
- 57.Escudero JC. Salud–ecología–política. Salud Cambio. 1991;2(3):8–20. [Google Scholar]
- 58.Laurell AC. Trabajo y salud: estado del conocimiento. In: Franco S, Nunes E, Breilh J, Laurell C. Debates en Medicina Social. Quito, Ecuador: Organización Panamericana de la Salud; 1991:249–339.
- 59.Breilh J. Epidemiología: Economía, Medicina y Política. Mexico City, Mexico: Fontamara; 1989.
- 60.Breilh J. Género, Poder y Salud. Quito, Ecuador: Centro de Estudios y Asesoría en Salud; 1993.
- 61.Grimberg M. 1992. Programas, actores y prácticas sociales: encuentros y desencuentros entre antropología y políticas de salud. Salud Cambio. 1992; 3(9):6–18. [Google Scholar]
- 62.Breilh J, Granda E. La epidemiología en la forja de una contrahegemonía. Salud Problema. 1986;11:25–40. [Google Scholar]
- 63.Breilh J, Granda E. Epidemiología y contrahegemonía. Soc Sci Med. 1989; 28:1121–1127. [DOI] [PubMed] [Google Scholar]
- 64.Laurell AC. Mortality and working conditions in agriculture in underdeveloped countries. Int J Health Serv. 1981; 11:3–20. [DOI] [PubMed] [Google Scholar]
- 65.Laurell AC, López Arellano O. Market commodities and poor relief: the World Bank proposal for health. Int J Health Serv. 1996;26:1–18. [DOI] [PubMed] [Google Scholar]
- 66.Stocker K, Waitzkin H, Iriart C. The exportation of managed care to Latin America. N Engl J Med. 1999; 340:1131–1136. [DOI] [PubMed] [Google Scholar]
- 67.Iriart C, Merhy E, Waitzkin H. Managed care in Latin America: the new common sense in health policy reform. Soc Sci Med. 2001;52:1243–1253. [DOI] [PubMed] [Google Scholar]
- 68.Laurell AC, Noriega M, López O, Ríos V. La experiencia obrera como fuente de conocimiento: confrontación de resultados de la encuesta colectiva e individual. Cuadernos Med Soc. 1990; 51:5–26. [Google Scholar]
- 69.Testa M. Saber en Salud: La Construcción del Conocimiento. Buenos Aires, Argentina: Lugar Editorial; 1997.
- 70.Merhy E, Onocko R, eds. Agir em Saúde. São Paulo, Brazil: Hucitec; 1997.
- 71.Iriart C, Merhy E, Waitzkin H. La Atención Gerenciada en América Latina: Su Papel en la Reforma de los Sistemas de Salud. Buenos Aires, Argentina: Instituto de Estudios y Formación/Central de Trabajadores Argentinos; 1999.
- 72.Testa M. Pensar en Salud. Buenos Aires, Argentina: Lugar Editorial; 1993.
- 73.Laurell AC. La salud-enfermedad como proceso social. Rev Latinoam Salud. 1982;2:7–25. [Google Scholar]
- 74.Franco S. Anotaciones preliminares para una historia de la causalidad en medicina. In: Nuño J, Bruni B, Franco S, et al., eds. Filosofîa en la Medicina. Cara-bobo, Venezuela: Universidad de Carabobo, Ediciones del Rectorado; 1998: 49-84.
- 75.Laurell AC, Blanco Gil J, Machetto T, et al. Disease and rural development: a sociological analysis of morbidity in two Mexican villages. Int J Health Serv. 1977;7:401–423. [DOI] [PubMed] [Google Scholar]
- 76.Breilh J, Granda E, Campaña A, Betancourt O. Ciudad y Muerte Infantil. Quito, Ecuador: Ediciones CEAS; 1983.
- 77.Breilh J. Nuevos Conceptos y Técnicas de Investigación. Quito, Ecuador: Centro de Estudios y Asesoría en Salud; 1995.
- 78.Iriart C. La reforma del sector salud en Argentina: de la salud como derecho social a bien público a responsabilidad individual y bien de mercado. In: Centro de Estudios y Asesoría en Salud. Reforma en Salud: Lo Privado o lo Solidario. Quito, Ecuador: CEAS; 1997:127–150.
- 79.Breilh J. Reforma: democracia profunda, no retroceso neoliberal. In: Centro de Estudios y Asesoría en Salud. Reforma en Salud: Lo Privado o lo Solidario. Quito, Ecuador: CEAS; 1997:71–115.
- 80.Merhy E, Iriart C, Waitzkin H. Atenção gerenciada: da micro-decisão corporativa à micro-decisão administrativa, um caminho igualmente privatizante? In: Bursmester H, ed. Managed Care: Alternativas de Gestão em Saúde. São Paulo, Brazil: Editora PROAHSA/ Editora Fundação Getulio Vargas; 1998:85–115.
- 81.Laurell AC, Ortega M. The free trade agreement and the Mexican health sector. Int J Health Serv. 1992; 22:331–337. [DOI] [PubMed] [Google Scholar]
- 82.Laurell AC, Wences M. Do poverty programs alleviate poverty? The case of the Mexican National Solidarity Program. Int J Health Serv. 1994;24:381–401. [DOI] [PubMed] [Google Scholar]
- 83.Colectivo CEAS. Mujer, Trabajo y Salud. Quito, Ecuador: Ediciones CEAS; 1994.
- 84.Betancourt O. La Salud y el Trabajo. Quito, Ecuador: Centro de Estudios y Asesoría en Salud y Organización Panamericana de la Salud; 1995.
- 85.de Almeida Filho N. Epidemiología sin Números. Washington, DC: Organización Panamericana de la Salud; 1992.
- 86.Laurell AC. The role of union democracy in the struggle for workers' health in Mexico. Int J Health Serv. 1989;19:279–293. [DOI] [PubMed] [Google Scholar]
- 87.Montecino S. Madres niñas, madresolas, continuidad o cambio cultural? Salud Cambio. 1993;4(11):6–8. [Google Scholar]
- 88.Franco T, Bueno W, Merhy E. O acolhimento e os processos de trabalho em saúde: o caso de Betim, Minas Gerais, Brasil. Cad Saude Publica. 1999;15:345–53. [DOI] [PubMed] [Google Scholar]
- 89.Franco Agudelo S. Violencia y salud en Colombia. Rev Panam Salud Publica. 1997;1:93–103. [PubMed] [Google Scholar]
- 90.Franco S. International dimensions of Colombian violence. Int J Health Serv. 2000;30:163–185. [DOI] [PubMed] [Google Scholar]
- 91.Estrada A, Hering M, Donoso A. Familia, Género y Terapia: Una Experiencia de Terapia Familiar Sistémica. Santiago, Chile: Ediciones CODEPU; 1997.
- 92.Martín-Baró I. Writings for a Liberation Psychology. Cambridge, Mass: Harvard University Press; 1994.
- 93.Martín-Baró I. La violencia en Centroamérica: una visión psicosocial. Salud Problema Debate. 1990;2(4):53–66. [Google Scholar]
- 94.Stolkiner A. Tiempos “posmodernos”: ajuste y salud mental. In: Cohen H, de Santos B, Fiasché A, et al. Políticas en Salud Mental. Buenos Aires, Argentina: Lugar Editorial; 1994:25–53.