Abstract
To generate timely and reliable information for decision making in local health centers, Mexico's National Epidemiological Surveillance System (SINAVE) was evaluated and reformed. The reform was achieved by consensus through national meetings of epidemiologists, using a conceptual model of requirements, leadership, participation, and motivation.
The new SINAVE is run by committees that use data from 16 468 local health centers that generate homogeneous information from all health institutions. Indicators, flowcharts, and standardized instruments were created. The reforms modernized SINAVE and strengthened epidemiologists' leadership, consolidated local decision making, and assessed control actions needed to improve the health of the Mexican population.
THE REFORM BEGAN WITH AN evaluation of SINAVE by means of a qualitative interview, with a guideline to detect potential solutions to several perceived problems at the first national meeting of 150 state epidemiologists (Table 1 ▶).1
TABLE 1.
—SINAVE Problems and Solutions Detected During First National Epidemiological Meeting
| Problem | Solutions |
| Decision making | Institute compulsory notification |
| Facilitate immediate and prompt decision making, based on real needs, analysis, and priorities | |
| Analysis of information | Implement single recording system |
| Standardize programs for recording and processing information | |
| Train personnel in system analysis to integrate multidirectional network information | |
| Excess work | Eliminate useless formats and simplify notification network |
| Integrate information in local health systems | |
| Standardize formats | |
| Communication within institutions | Implement single, constant, bidirectional, and prompt morbidity and mortality feedback system |
| and with other institutions | Integrate interinstitutional surveillance group |
| Feedback | Generate reports and bulletins |
| Frequently update interinstitutional agreements at every operational level | |
| Unify normative and technical documents and periodical revisions according to epidemiological behavior and program impact | |
| SINAVE organization manual | Prepare manual for SINAVE, including case definition |
| Technology | Provide equipment to every operational level |
| Standardize computer programs for recording, processing, and analyzing information | |
| Promptness of information | Redefine channels to allow better information flow |
| Disseminate information to allow updates and advice at other levels | |
| Quality of information | Improve veracity, promptness, integrity, and agreement through technical support and |
| interinstitutional collaboration | |
| System flexibility | Maintain flexibility to allow integration and elimination of diseases, based on experience in a |
| particular state and according to technological and scientific advances | |
| Staff mobilization | Promote agreements by academic institutions to include epidemiological surveys in their curricula |
| Encourage long-term appointment of physicians | |
| Promote better salaries | |
| Training | Implement continuous personnel training |
| Provide epidemiological educational programs | |
| Information, decision, action | Define range and characteristics of decisions and actions at each level |
| Provide prompt and reliable information to focus actions toward specific problems | |
| Have qualified technical personnel | |
| Implement communication network with “state-of-the-art” technology (fax, modem, etc.) | |
| Supervision | Unify supervision criteria |
| Periodical and permanent supervision | |
| Private sector | Incorporate participation by law |
| Parallel information systems | Create single information system |
| Human resources | Define expenditure structure for SINAVE |
| Dissemination of information | Elaborate periodical bulletin |
| Promulgate official procedures at all operational levels | |
| Carry out events with interinstitutional participation |
A second national meeting defined diseases of epidemiological interest, the frequency of epidemiological reports, and technical levels where analysis should be conducted to verify the data for decision making.2 Work teams were given a list of 389 diseases, which they rated for impact, relevance, and vulnerability; they then selected the diseases to be included for national and regional epidemiological surveillance. A cutoff point was defined (μ ± 2SD) so that each professional continued the exercises only with events selected above the cutoff. Participants also considered which diseases should be reported immediately or weekly and whether a case study should be conducted. Listings were subjected to a frequency analysis, and three standardized formats were defined: a Weekly Report of New Cases of Disease (EPI-1-95), a Case Study (EPI-2-95), and an Outbreak Study (EPI-3-95). A pilot test was conducted for a 2-month period. Problems were discussed, and errors were detected and corrected.
At a third national meeting, the simple conceptual model of SINAVE reform, formats, manuals, and training program was presented. A Single Information System for Epidemiological Surveillance (SUIVE) was created to generate efficient homogeneous data to improve the quality and timeliness of epidemiological information.3 An Automated Epidemiological Surveillance System (SUAVE) also was designed, using up-to-date technology.4 SUAVE was created to install, input, process, and analyze data about the diseases included in EPI-1-95 generated in 16 468 local health centers, 2428 municipalities, and 234 health jurisdictions in Mexico.5 SINAVE leaders held weekly meetings to develop case definitions, morbidity manuals, an epidemiology bulletin, and a training plan.
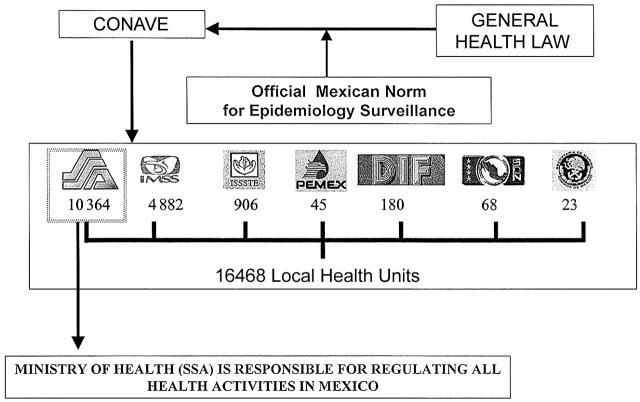
A National Committee for Epidemiological Surveillance (CONAVE) was created through ministerial agreement to make surveillance statutory and compulsory in the National Health System.6 CONAVE was conceived and designed according to the model of academic committees. With Mexico's complex health system, CONAVE has a unique value, because, for the first time, all organizations had been actively involved at SINAVE, and the Official Mexican Norm for Epidemiology Surveillance mandates that involvement (Figure 1 ▶).7
FIGURE 1.
—National Epidemiological Surveillance System (SINAVE).
To assess a SUIVE's performance, 4 indicators were designed: compliance in delivering information, distribution of total versus expected diagnoses reported, coverage of local health centers reporting on time and with delays, and consistency (a measure of the homogeneity of diagnoses reported). These indicators could be analyzed on a weekly or an institution basis, or both, from the national level to the reporting center.
A 2-year training plan was established. Five courses—on leadership, teamwork, total quality, data for decision making, and verbal and written communication—were offered to SINAVE reform leaders.8 Together these courses constituted a special curriculum on leadership in epidemiology for all epidemiologists. To keep the epidemiology leadership in local health centers, annual national meetings were held; since 1995, every epidemiologist in the country has been assured of receiving comprehensive training at least once a year.
To establish a feedback system, the lead team met to determine the contents, periodicity, users, and design of weekly feedback instruments to improve communication. The official newsletter, Boletín Epidemiología, is distributed to 3500 users and through an Internet web page.9 The states also established their own bulletins, which are distributed to all LHCs (dedicated to primary health assistance and members of the local public health system).
DISCUSSION AND EVALUATION
Mexico has been undergoing a decentralization process that SINAVE anticipated, based on timely and reliable information generated by SUIVE, consolidated state decision making, strengthened epidemiologists' leadership, and a national epidemiological outlook of new health policies.8,10–14 Under the reform, local health centers are aware of the diseases to be tracked and the frequency with which they are to be reported; who is responsible for surveillance and reporting; what information is required for each case; what format is necessary; and who should be informed; procedures to be followed at each operating level. As a result, surveillance improved along all 4 indicators.3,7 By 1999, the national average compliance rate was 96%, with 24 of the country's 32 states reaching 100%. National reporting consistency was 85%, and a total of 38.6 million diagnoses were reported. Mexico has 16 900 local health centers;15 of these, 16 468 (95.8%) are included in the SUIVE catalog, and more than 84% report epidemiologic information weekly and send it by e-mail to the Sanitary Jurisdiction. Among the 16% that did not report, the reasons included physicians on leave, vacations, or sickness and lack of transmission means. With regard to mortality reporting, the local health centers now report deaths with a 1-month delay; previously the delays consisted of 5 years or more.
Based on the continuous training program, an epidemiologic reinforcement process was set up. Prior to SINAVE reform, an epidemiologist acting as the head of a department was supported by 2 to 4 people without training. Today, 28 of the 32 state epidemiologists have improved positions, with better salaries and work teams of more than 6 trained people.
The reform undoubtedly had limitations—such as a lack of full integration into the process of change in laboratory areas, specifically modernization and reinforcement of the national public health laboratory network—because there was no active participation by staff responsible for and regulating laboratory areas. Furthermore, the existing infrastructure in the network was insufficient, and rectifying this problem would have involved an infeasible financial investment. Moreover, there is a significant annual staff turnover among people working in the jurisdictional epidemiological area (25%), so it was necessary to maintain a continuous training program. This issue remains a challenge.
NEXT STEPS
The reformed epidemiologic surveillance system is a dynamic, permanent, systematic, planned, and organized process to assess the nature, characteristics, frequency, and distribution of disease.8,11 The new millennium presents the need for renewal in all human actions. Epidemiologic surveillance is improving the quality of information to face the challenges of the coming years.8,10–13 We are therefore working on a new SINAVE-2000.
HIGHLIGHTS
• The reform process established guidelines to evaluate and reform Mexico's epidemiologic surveillance system.
• Epidemiologists have learned how to face the challenges of morbidity information in a country undergoing an epidemiologic transition.
• All epidemiologists have been active participants in the reform of the national epidemiologic surveillance system.
Acknowledgments
We thank the institutions in the Health Sector and our colleagues and friends Oscar Velazquez, Javier Cabral, Celia Escandón, Cuauhtémoc Ruiz, Fernando Meneses, Vicente Cruz, Rocío Cuevas, Gabriela Fernández, César Sandoval, Arturo Revuelta, Manuel Camargo, Arturo González, and Carmen Sánchez for their support and participation.
Peer Reviewed
References
- 1.Thacker SB, Parrish RG, Trowbridge FL. A method for evaluating systems of epidemiological surveillance. World Health Stat Q. 1988;41:11–18. [PubMed] [Google Scholar]
- 2.Risi JB Jr. Using surveillance data for decision making in public health. MMWR Morb Mortal Wkly Rep. 1992; 41(suppl):57–59. [PubMed] [Google Scholar]
- 3.Manual del Sistema de Información de Morbilidad del Sistema Nacional de Vigilancia Epidemiológica [Manual for the Morbidity Information System of the National Epidemiological Surveillance System]. General Directorate of Epidemiology, Mexico, Secretariat of Health, 1994. (Working Paper).
- 4.EPI INFO Version 5.0a. Atlanta, Georgia: Centers for Disease Control and Prevention; 1995.
- 5.Manual del Sistema Unico Automatizado para la Vigilancia Epidemiológica [Manual for the Single Automated Epidemiological Surveillance System]. General Directorate of Epidemiology, Mexico, Secretariat of Health, 1998. (Working Paper.)
- 6.Resolution Number 130. Official Gazette of the Federation. 1995;4:1–30. [Google Scholar]
- 7.Norma Oficial Mexicana para la Vigilancia Epidemiológica [Official Mexican Norm for Epidemiological Surveillance] (NOM 017-SSA2-1994). Official Gazette of the Federation. 1999;553: 53–80. [Google Scholar]
- 8.Wetterhall SF, Pappaioanou M, Thacker SB, Eacker E, Churchill RE. The role of public health surveillance: information for effective action in public health. MMWR Morb Mortal Wkly Rep. 1992;41:207–218. [PubMed] [Google Scholar]
- 9.Boletín Epidemiología. In: National Epidemiological Surveillance System. Single Information System. ISSN 1405-2636. Mexico DF Secretariat of Health, 1995–1999.
- 10.Organización y Funcionamiento. La Reforma en Salud. Mejorar la Salud de los Mexicanos [Organization and Performance. Health Reform. Improving the Health of Mexicans]. Cuadernos de Salud, Mexico D.F. Secretariat of Health, 1994;5:11–70. [Google Scholar]
- 11.Sepúlveda J, López-Cervantes M, Frenk J, Gómez de León J, Lezana-Fernández MA, Santos-Burgoa C. Keynote address: key issues in public health surveillance for the 1990s. MMWR Morb Mortal Wkly Rep. 1992;41:61–76. [PubMed] [Google Scholar]
- 12.Thacker SB, Stroup DF. Future directions for comprehensive public health surveillance and health information systems in the United States. Am J Epidemiol. 1994;140:383–397. [DOI] [PubMed] [Google Scholar]
- 13.Choi BC. Perspectives on epidemiological surveillance in the 21st century. Chronic Dis Can. 1998,19:145–151. [PubMed] [Google Scholar]
- 14.Thacker SB, Berkelman RL. Public health surveillance in the United States. Epidemiol Rev. 1988;10:164–190. [DOI] [PubMed] [Google Scholar]
- 15.Anuario Estadístico [Statistical Yearbook]. General Directorate for Statistics and Informatics. Mexico, D.F. Secretariat of Health. 1997;283–495.