Abstract
Objectives. This study analyzed growth and identified related medical conditions among refugee children in Massachusetts.
Methods. Between July 1995 and June 1998, 1825 refugee children were screened. Variables included positive tuberculin (purified protein derivative; PPD) test; dental abnormalities; pathogenic parasites; weight-for-age, height-for-age, and weight-for-height z scores; and body mass index greater than the 84th percentile.
Results. Of all the children, 21% had parasites, 62% had caries, and 25% had a positive PPD reaction. Twelve percent overall and 28% younger than 2 years had anemia. Eight percent had height-for-age z scores less than –2, and 6% had weight-for-age z scores greater than +2. Of those aged 1 to 9 years, 7% had weight-for-height z scores greater than +2. Weight-for-height z scores less than –2 were concentrated among Africans and East Asians (both 8%). Height-for-age z scores less than –2 were seen among African (13%), Near Eastern (19%), and East Asian (30%) children. Weight-for-height z scores greater than +2 and body mass index greater than the 84th percentile were concentrated among children from the former Yugoslavia (8% and 15%) and the former Soviet Union (8% and 14%).
Conclusions. Recently arrived refugee children have significant growth abnormalities. European refugees were overweight; those from developing countries had growth retardation.
Until recently, children granted official refugee visas have originated predominantly from the former Soviet Union and Southeast Asia. Current trends indicate increasing numbers emigrating from other parts of the world, such as the former Yugoslavia, Iraq, Cuba, Haiti, Somalia, and other parts of Africa. In the past year, Bosnians received the largest allocation of refugee visas for the first time. In coming years, refugee visa slots for Africans also will be prioritized.1
In the 1990s, both wars2–4 and environmental disasters5,6 heightened the nutritional and health risks of children living in countries that subsequently sent refugees to the United States. Although previous cohorts of refugee children in the United States have had growth and nutritional disorders,7 more recent studies of smaller clinic populations of refugee children in the United States and abroad did not find high prevalence rates of growth deficiency but detected high prevalence rates of other problems, such as intestinal parasites, anemia, dental abnormalities,8–10 and chronic conditions, including obesity.11 Given the increasing diversity of refugees in recent years, these reports may not provide an accurate description of their health and nutritional status.
In this article, the term refugee applies to children who were eligible for refugee medical screening as defined by US federal law (the Immigration and Nationality Act, as amended by the Refugee Act of 1980): those individuals who, having fled persecution of themselves or their families, hold refugee visas or political asylum designations from the US government or are specially designated entrants from Haiti or Cuba. In mid-1995, refugee medical screening in Massachusetts was consolidated as the Refugee Health Assessment Program (RHAP) under the auspices of the Massachusetts Department of Public Health and contracted to a limited network of clinical sites. By 1999, RHAP was screening 90% of the newly arrived refugees (unpublished state FY2000 program data from the Refugee and Immigrant Health Program, Massachusetts Department of Public Health, November 14, 2000). Consequently, more comprehensive data related to refugee health status are now available for review.
We sought to describe the growth indices and health status of all refugee children screened through the RHAP during a recent 3-year period. In this article, we present findings from the analysis of anthropometric and selected medical screening data collected as part of the RHAP and describe associations between medical conditions and growth abnormalities in a large cohort of refugee children with diverse countries of origin. Findings from this study should be applicable to refugees outside Massachusetts because refugee demographics in Massachusetts roughly match those of other states, except for a slightly higher representation of children from the former Soviet Union. In addition, because many immigrants come from backgrounds similarly traumatic to those of refugees, findings may provide insights relevant to the health status of other immigrant groups.
METHODS
Refugee children younger than 18 years were screened at 16 contracted sites around Massachusetts; nearly half of the children were screened at only 2 sites. All the data were collected within 90 days of arrival in the United States. Data forms were forwarded to the RHAP. Medical screening, data collection, and analysis were conducted pursuant to US law 45 CFR §400.107. Although not mandatory, the health assessment is considered an integral part of refugee resettlement in Massachusetts.
Anthropometric measurements included height, weight, and, in children younger than 5 years, head circumference. This analysis focused on the height and weight measurements. Height was generally measured as recommended by the Centers for Disease Control and Prevention: supine for infants and toddlers younger than 2 years and erect for older children.12 Indices were calculated with Epi Info, Version 6.04b (Centers for Disease Control and Prevention, Atlanta, Ga), based on National Center for Health Statistics data and accepted as international standards.13 Because this was a retrospective analysis, measurements could not be confirmed; however, Epi Info excludes outlying data.
Height-for-age, weight-for-height, and weight-for-age z scores (SDs from the reference median) were assessed. Acute undernutrition, or wasting, was defined as weight-for-height z score less than –2 and was assessed for children who met Epi Info's anthropometric criteria for the calculation. Chronic undernutrition, or stunting, was defined as height-for-age z score less than –2. For overweight, weight-for-age z score greater than +2 was assessed in all children; weight-for-height z score greater than +2 was assessed in children who met Epi Info's criteria. These criteria for males are age 12 to 138 months and height from 49 to less than 145 cm. For females, the criteria are age 12 to 120 months and height from 49 to less than 137 cm. Body mass index (BMI) was calculated for all children aged 10 to 17 years. BMI cutoff values were used to classify children as either at risk for overweight (85th–94th percentiles) or overweight (≥95th percentile).13,14
Screening data relevant to growth and nutritional status were analyzed with bivariate and multivariate analyses, with growth indices as dependent variables. These data included results of microscopy of a single stool specimen for ova and parasites, visual inspection of dentition for abnormalities, complete blood counts, and purified protein derivative (PPD) for tuberculosis skin testing. PPD results were defined as positive with 10 mm or more of induration, in the absence of other high-risk criteria.15 Anemia was assessed in only a subset of the children because hemoglobin values were added to the database only starting in June 1996. Subsequent to June 1, 1996, hematologic data were available for 91% of the children who were screened. Anemia was defined as having a hemoglobin value less than the age- and sex-specific fifth percentile cutoff values from the Third National Health and Nutrition Examination Survey.16 Although evidence exists to support lower cutoff values for African Americans,16 no such baseline data are available for native Africans, mainly Somalians in the case of refugees.
Analyses included t and χ2 tests and multivariate logistic regression analyses. Because of small numbers from some countries, countries were grouped into regions for comparative analyses: Africa, Americas, Near East, East Asia, former Yugoslavia, and former Soviet Union. Bivariate analyses were conducted to assess associations between growth indices and the following variables: sex, age, anemia, pathogenic intestinal parasites, dental abnormalities, PPD, and region of origin. In multivariate analyses, region of origin was dichotomized as either “former socialist economy” (former Yugoslavia and former Soviet Union) or “developing economy” (all others) to reflect the differing growth trends observed in bivariate analyses. We examined the relations between the dependent variables and the independent variables, including age in years, sex, anemia, dental abnormalities, pathogenic parasites, and region. Age in years was treated as a continuous variable; all others were dichotomous.
RESULTS
Demographics
Between July 1, 1995, and June 30, 1998, 1825 refugee children (48% female) were screened through the RHAP. These children originated in 19 countries in addition to 15 newly independent states formerly part of the Soviet Union. Sex distribution did not vary significantly by country or region of origin except for the Near East. Iraqi, Kurdish, and Iranian children were 2.0 times more likely (95% confidence interval [CI] = 1.1, 3.7) to be male compared with all other refugee children, and only 32% were female. On average, refugee children had been in the United States for 30 days at the time of screening (Table 1 ▶).
TABLE 1—
Demographic Data of Refugee Children Screened in Massachusetts, 1995–1998
| Regiona | n (%)b | % Female | Mean Days in US | Mean Age, mo | ≤1 yc | 1–5 yc | 6–9 yc | 10–17 yc |
| Africa | 276 (15) | 50 | 29 | 118 | 7 (3%) | 65 (24%) | 70 (25%) | 134 (49%) |
| Americas | 38 (2) | 47 | 30 | 118 | 1 (3%) | 7 (18%) | 13 (34%) | 17 (45%) |
| East Asia | 261 (14) | 50 | 30 | 132* | 3 (1%) | 36 (14%) | 54 (21%) | 168 (64%) |
| Near East | 53 (3) | 32 | 22 | 90* | 4 (8%) | 19 (36%) | 11 (21%) | 19 (36%) |
| Former Soviet Union | 852 (47) | 48 | 33 | 108* | 30 (4%) | 240 (28%) | 208 (24%) | 374 (44%) |
| Former Yugoslavia | 345 (19) | 47 | 23 | 110 | 17 (5%) | 89 (26%) | 82 (24%) | 157 (46%) |
| Overall | 1825 (100) | 48 | 30 | 113 | 62 (3%) | 456 (25%) | 438 (24%) | 869 (48%) |
aEach region had 1 or 2 predominant countries as follows: Africa (89% Somalian), Americas (50% Haitian and 40% Cuban), East Asia (90% Vietnamese), Near East (98% Iraqi and Kurds), former Soviet Union (41% Ukrainian and 27% Russian), and former Yugoslavia (96% Bosnian).
bPercentages given are those of column total.
cPercentages given are those of row total. May not sum to 100% because percentages were rounded to whole numbers.
*Comparing mean age in months of refugees from the region with that of refugees from all other regions, P < .01.
Approximately 19% of the newly arrived refugee children during the study period were not assessed through the RHAP. (The percentage of children who were screened during the entire study period is lower than the previously noted 90%, which reflects more recent success of the RHAP. The lower number of children screened over the study period reflects the program's transition in late 1995 and early 1996 when the newly organized RHAP system was being consolidated.) Nearly two thirds of the children not screened were from the former Soviet Union and Vietnam, similar to the percentages of children from the former Soviet Union and Vietnam among all who completed the RHAP. However, children from the Americas were overrepresented among those who did not complete the assessment (n = 50, or 11% of those not assessed, compared with 2% of those assessed). Southeast Asians also were more likely than other refugees not to have been screened (odds ratio [OR] = 1.5; 95% CI = 1.2, 2.0).
Health Screening
Pathogenic parasites were detected in 21% of the 1642 children who submitted a stool sample. An additional 16% had only nonpathogenic parasites detected. Refugees from Africa, the Americas, and East Asia harbored a range of different parasitic species; often, multiple parasites were present in an individual. Refugees from the former Soviet Union and former Yugoslavia tended to have Giardia lamblia or nonpathogens, such as Blastocystis hominis. A positive PPD reaction was reported in 25% of the 1737 children tested. Dental abnormalities, mainly caries, were found in 62% of 1702 children (Table 2 ▶).
TABLE 2—
Results of Refugee Children Screened for Medical Conditions in Massachusetts, 1995–1998
| O & Pa | PPD | Dental Abnormality | ||||
| n | + (%)b | n | + (%)b | n | + (%)b | |
| Region | ||||||
| Africa | 232 | 116 (50) | 262 | 65 (25) | 256 | 185 (72) |
| Americas | 26 | 13 (50) | 31 | 8 (26) | 31 | 21 (68) |
| East Asia | 234 | 72 (31) | 243 | 51 (21) | 235 | 163 (69) |
| Near East | 48 | 14 (29) | 53 | 5 (9) | 48 | 28 (58) |
| Former Soviet Union | 782 | 78 (10) | 809 | 214 (26) | 803 | 489 (61) |
| Former Yugoslavia | 320 | 51 (16) | 338 | 97 (29) | 328 | 177 (54) |
| Age group, y | ||||||
| <1 | 53 | 1 (2) | 54 | 7 (13) | 51 | 1 (2) |
| 1–5 | 407 | 84 (21) | 431 | 62 (14) | 426 | 150 (35) |
| 6–9 | 394 | 95 (24) | 427 | 98 (23) | 412 | 202 (49) |
| >9 | 788 | 164 (21) | 825 | 273 (33) | 813 | 536 (66) |
| Overall | 1642 | 344 (21) | 1737 | 440 (25) | 1702 | 1063 (62) |
Note. O & P = ova and parasites; PPD = purified protein derivative tuberculin skin test.
aMicroscopy for ova and parasites: pathogenic parasites only.
bAbsolute number testing positive, with percentage of those tested who had positive results in each row.
Anemia was found in 153 (12%) of 1247 children. Anemia had a high prevalence in most regions; however, anemia prevalence varied greatly by region, age, and sex. Of note, 28% of all children younger than 2 years and 21% of all males between ages 12 and 15 years were anemic. Children from the Americas and Near East had overall prevalence rates of 12% and 17%, respectively, but were of insufficient numbers to permit further analyses. Among Africans, 31% were anemic, with 50% of the children younger than 2 years and 45% of the children between 12 and 15 years of age. No age group of Africans had a prevalence of anemia less than 25%. Among children from the former Soviet Union, 10% were anemic, with 27% of the children younger than 2 years, 12% of the children between 12 and 15 years, and 11% of the children 15 years or older. Among children from both the former Yugoslavia and East Asia, the prevalence of anemia was 14% among children younger than 2 years and 9% and 7%, respectively for each region, among children aged 2 to 5 years before declining in older age groups to levels close to those of the United States.
Anthropometrics
Of the 1767 children with height measurements reported, 143 (8%) had height-for-age z scores less than –2. Of the 964 children for whom weight-for-height z scores were calculated, 23 (2%) had scores less than –2. Of the 1786 with weight measurements reported, 112 (6%) had weight-for-age z scores greater than +2, and of the 964 for whom weight-for-height z scores were calculated, 66 (7%) had scores greater than +2. BMI was calculated for 855 children aged 10 to 17 years. Thirty-two children (4%) had a BMI greater than or equal to the 95th percentile, and 89 (10%) had a BMI at the 85th to 94th percentile.
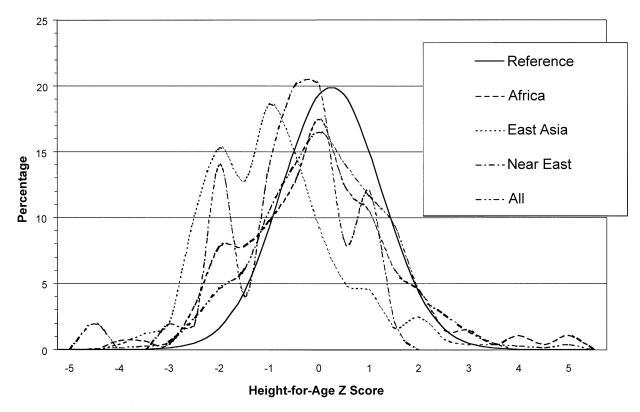
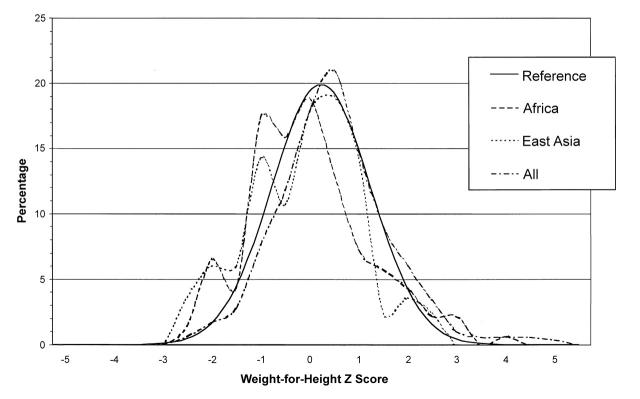
Overall, poor growth was evenly distributed across age and sex groupings. No sex-specific differences were found in prevalence rates of height-for-age z scores or weight-for-height z scores less than –2 in either overall or regional analyses. Height-for-age z scores less than –2 were found predominantly among African (13%), Near Eastern (19%), and East Asian (30%) children. Weight-for-height z scores less than –2 were found mainly among Africans and East Asians (both 8%) (Figures 1 and 2 ▶ ▶).
FIGURE 1—
Height-for-age z score distribution for selected refugee children screened in Massachusetts, 1995–1998.
FIGURE 2—
Weight-for-height z score distribution for selected refugee children screened in Massachusetts, 1995–1998.
Overweight was assessed by analyzing weight-for-height z scores greater than +2, weight-for-age z scores greater than +2, and BMI greater than the 84th percentile. Overall, 6% of the children had high weight-for-age z scores. Of those with weight-for-height z scores calculated, 7% had high scores. Overweight was concentrated in young children, with weight-for-age z scores greater than +2 in 7% of the children aged 1 to 9 years. Prevalence rates of weight-for-age z scores and weight-for-height z scores greater than +2 were particularly high among those children from the former Yugoslavia and former Soviet Union (8% in each region had weight-for-height z scores > +2) and the Americas (11%) (both P < .01 in comparison to US reference). Overall rates of BMI greater than 84% were not elevated. Ten percent of children were at risk for overweight, and 4% were overweight. However, these findings mask substantial regional variation. Of the children from the former Yugoslavia and the former Soviet Union, 15% and 14%, respectively, were at risk for overweight (P = .03 in comparison to US reference). Conversely, excluding children from the Americas (of whom 5 of 12 had BMI > 84th percentile), only 8% of the children from the developing regions were overweight or at risk for overweight (P < .01 in comparison to US reference).
Associations Between Anthropometric Status and Medical Conditions
In bivariate analyses, anemia (OR = 6.1; 95% CI = 2.1, 17.4) and presence of pathogenic parasites (OR = 2.6; 95% CI = 1.1, 6.0) were associated with weight-for-height z scores less than –2. Nineteen of the 23 children (83%) with low weight-for-height z scores came from Africa or East Asia. Children from developing regions were 12 times more likely than other refugee children to have weight-for-height z scores less than –2 (95% CI = 3.8, 47.4). A positive PPD result was associated with lowered likelihood of having height-for-age z scores less than –2 (OR = 0.6; 95% CI = 0.3, 0.9), whereas infection with pathogenic parasites was associated with increased risk of low height-for-age z scores (OR = 2.4; 95% CI = 1.6, 3.4).
In multiple logistic regression analyses, age, anemia, and region had significant associations with low weight-for-height z scores. Each yearly increment in age increased the likelihood of having low weight-for-height z scores by 1.3 (95% CI = 1.2, 1.5). Anemic children were 15 times more likely than nonanemic children to have low weight-for-height z scores (95% CI = 4.1, 49.1). Compared with children from former socialist regions, children from developing regions had 6.3 times the risk of low weight-for-height z scores (95% CI = 3.0, 14.1).
Height-for-age z scores less than –2 were assessed in a similar multivariate analysis. In a regression model with the same independent variables, children from developing regions were 10 times more likely than other children to have height-for-age z scores less than –2 (95% CI = 7.1, 25.5). In subanalyses of each region, however, neither anemia nor infection with parasites was associated with low height-for-age z scores.
Indices suggesting overweight also were assessed in similar multivariate analyses. No independent variable had a significant association with high weight-for-height z scores. Dichotomized BMI values were used as dependent variables in multiple logistic regression as well. Increasing age increments of 1 year (OR = 0.8; 95% CI = 0.7, 0.9), anemia (OR = 0.3; 95% CI = 0.0, 0.9), infection with intestinal parasites (OR = 0.5; 95% CI = 0.2, 0.8), and origin in a developing region (OR = 0.3; 95% CI = 0.1, 0.6) were all inversely associated with BMI greater than the 84th percentile. Reduced risk of BMI at the 85th to 94th percentiles also was observed for the same 4 independent variables. Dental abnormalities, in contrast, were positively associated with being overweight or at risk for overweight (OR = 2.6; 95% CI = 1.2, 4.4).
DISCUSSION
Anemia, positive PPD reaction, infection with pathogenic intestinal parasites, and dental abnormalities were highly prevalent among refugee children resettled in Massachusetts from 1995 through 1998. These problems were found among children of all ages and from most countries of origin. Together with the dramatic rates of undernutrition, as evidenced by the poor growth documented in this study, our findings support the need for universal, comprehensive health screening and treatment of refugee children shortly after arrival in the United States.
Poor growth, particularly low height-for-age z scores, indicating stunting or chronic malnutrition, was found almost exclusively among refugee children from developing regions. The prevalence of low weight-for-height z scores, or wasting, reflecting acute undernutrition, was increased among children from Africa and East Asia. In contrast, overweight is a real concern for children arriving from the former socialist countries of Eastern Europe and the Americas and was associated with the presence of dental abnormalities. Overall, country of origin appeared to be the most important determinant of nutritional and growth status.
The prevalence of anemia, 12% overall, was strikingly elevated in some groups, including 28% of all children younger than 2 years and 21% of the boys aged 12 to 15 years. Given the potential long-term effect of nutritional disorders such as iron deficiency17,18 and stunting early in life,19 treatment and prevention are of special importance.
The relatively low prevalence of anemia (6%) among East Asians differs substantially from the prevalence reported in earlier cohorts of Vietnamese refugees.7 This may be because of the changing demographics of Vietnamese refugees. During the years covered in this study, Vietnamese refugee visas were allocated to individuals and families from a mix of backgrounds within Vietnam through the Orderly Departure Program.1 These demographics contrast with those of earlier cohorts of Vietnamese, who came from refugee camps in other countries throughout East Asia. In recent years, Vietnamese children have tended to be older than other refugee children as well as previous refugee children from Vietnam. Although current Vietnamese refugee children may have been stunted earlier in life, their dietary intake before resettlement in the United States may have been iron-rich enough to prevent or correct anemia but may not have provided sufficient calories for catch-up linear growth.
Associations between medical conditions and growth indices were not consistent. Low weight-for-height z scores were associated with anemia, as might be expected in the acutely undernourished child. The association of dental caries with overweight may be related to dietary patterns and bottle use among the children from the former Yugoslavia and former Soviet Union. It has been our experience that, as has been reported elsewhere,2 many young children who lived in Bosnia during the war were weaned to cow's milk well before age 1 year and then relied on milk (frequently from a baby bottle) and very limited food supplies for nutrition during the critical period of growth in the first 6 years of life. We have found “baby bottle caries” to be common among children from the former Yugoslavia. Therefore, appropriate dietary practices should be introduced during health screening and reinforced during medical encounters.
The findings of this study must be interpreted with caution. We could not verify accuracy of birth dates. Refugees who cannot provide a precise birth date during immigration processing are assigned dates of birth to meet US requirements that all birth dates be in “MM/DD/YY” format. January 1 is a typical assigned date and can create problems in anthropometric analysis. In this sample, 151 (61%) of the Somalians had a birthdate of January 1. Even with a correct year, assigned dates can add months to a child's age. For example, the January 1 date could make a child appear older than he or she is and thus smaller for age. Conversely, it is our experience that some refugee parents understate their children's ages, making them appear younger, but also bigger, than they actually are. These discrepancies would not affect weight-for-height z score data because this measure is age independent.
Growth patterns may vary between racial/ethnic and national groups and also among demographic subgroups within national populations. In this cohort, significant demographic variation within nationalities occurred. For example, among children from the former Soviet Union, those arriving during the earlier part of the study were generally from the region's major urban centers, whereas those arriving later included large numbers of evangelical Christians from smaller industrial cities. Similarly, although origin in a developing country is associated with high risk of poor growth, specific medical conditions identified within this group may vary greatly, as shown by the varying rates of anemia.
Our findings, however, were consistent with those of previous studies of large refugee cohorts that documented poor growth and nutrition in the United States and abroad.7,20–23 Also, multiple sites were used to collect the data, but individuals performing these assessments and measurements were relatively consistent over time, particularly at the RHAP's 2 largest sites, which screened nearly half of the children.
Clinicians who care for refugees must be aware that children from developing countries are at very high risk for growth and nutritional problems with related medical conditions. Prompt screening, adequate medical follow-up, and assurance of appropriate food support are essential. Clinicians should be aware of regional variations in health and nutritional status because they may be the best predictors of health risks in refugees. Knowledge of socioeconomic and demographic conditions associated with refugee migration is essential in identifying higher-risk individuals and populations. For example, refugee children from the former socialist countries of Eastern Europe have higher rates of overweight and risk of overweight but also may have less obvious nutritional abnormalities, such as micronutrient deficiencies, as suggested by high rates of anemia.
Continuity of medical follow-up is essential for preventing ongoing problems in growth and development, physical health, and nutrition. Clinicians providing primary care for refugees must ensure that ongoing nutritional and growth screening is performed and that refugee families receive necessary food supplementation, such as Special Supplemental Nutrition Program for Women, Infants, and Children and food stamps. Ultimately, until refugees become self-sufficient, our society must ensure that refugees have the resources necessary for maintaining a food supply sufficient for repletion, catch-up growth, and maintenance growth.
P. L. Geltman, M. Radin, and J. Cochran conceived of and designed the study, assisted in statistical analyses, interpreted results, and wrote and edited the paper. Z. Zhang designed statistical models, performed most statistical analyses, interpreted results, and helped write and edit the paper, particularly those sections related to the methods, results, and interpretation of statistical analyses. A. F. Meyers interpreted results, and helped write and edit the paper.
Peer Reviewed
References
- 1.Proposed Refugee Admissions for Fiscal Year 1999: Report to the Congress. Washington, DC: US Depts of State, Justice, and Health and Human Services; 1998:9–12.
- 2.Smaijkic A, Zec S, Telebak B, Filipovic-Hadziomeragic A. Changes in nutrition among residents and refugees in Sarajevo during war. Eur J Clin Nutr. 1995;49(suppl):S17–S22. [PubMed] [Google Scholar]
- 3.Dowell SF, Toko A, Sita C, Piarroux R, Duerr A, Woodruff BA. Letter from Goma: health and nutrition in centers for unaccompanied refugee children: experience from the 1994 Rwandan refugee crisis. JAMA. 1995;273:1802–1806. [PubMed] [Google Scholar]
- 4.Nabeth P, Michelet MJ, Le Gallais G, Claus W. Demographic and nutritional consequences of civil war in Liberia. Lancet. 1997;349:59–60. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Update: health and nutritional profile of refugees—Ethiopia, 1989–1990. MMWR Morb Mortal Wkly Rep. 1990;39:707–718. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Nutritional assessment of children in drought-affected areas—Haiti, 1990. MMWR Morb Mortal Wkly Rep. 1991;40:222–225. [PubMed] [Google Scholar]
- 7.Peck RE, Chuang M, Robbins GE, Nichaman MZ. Nutritional status of Southeast Asian refugee children. Am J Public Health. 1981;71:1144–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hayes EB, Talbot SB, Matheson ES, Pressler HM, Hanna AB, McCarthy CA. Health status of pediatric refugees in Portland, ME. Arch Pediatr Adolesc Med. 1998;152:564–568. [DOI] [PubMed] [Google Scholar]
- 9.Meropol SB. Health status of pediatric refugees in Buffalo, NY. Arch Pediatr Adolesc Med. 1995;149:887–892. [DOI] [PubMed] [Google Scholar]
- 10.Tittle BS, Harris JS, Chase PA, Morrell RE, Jackson RJ, Epinoza SY. Health screening of Indochinese refugee children. Am J Dis Child. 1982;136:697–700. [DOI] [PubMed] [Google Scholar]
- 11.Hjern A, Kocturk-Runefors O, Jeppson O, Tegelman R, Hojer B, Adlercreutz H. Health and nutrition in newly resettled refugee children from Chile and the Middle East. Acta Paediatr Scand. 1991;80:859–867. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Pediatric nutrition surveillance system—United States, 1980–1991. MMWR CDC Surveill Summ. 1992;41(SS-7):1–24. [PubMed] [Google Scholar]
- 13.WHO Expert Committee on Physical Status. The Use and Interpretation of Anthropometry. Geneva, Switzerland: World Health Organization; 1995:4–33. [PubMed]
- 14.Himes JH, Dietz WH. Guidelines for overweight in adolescent preventive services: recommendations from an expert committee. Am J Clin Nutr. 1994;59:307–316. [DOI] [PubMed] [Google Scholar]
- 15.American Academy of Pediatrics. Tuberculosis. In: Peter G, ed. 1997 Red Book: Report of the Committee on Infectious Diseases. 24th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 1997:545–562.
- 16.Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. MMWR Morb Mortal Wkly Rep. 1998;47(RR-3):1–29. [PubMed] [Google Scholar]
- 17.Pollit E. Iron deficiency and cognitive function. Annu Rev Nutr. 1993;13:521–537. [DOI] [PubMed] [Google Scholar]
- 18.Lozoff B, Jimenez E, Wolf AW. Long-term developmental outcome of infants with iron deficiency. N Engl J Med. 1991;325:687–694. [DOI] [PubMed] [Google Scholar]
- 19.Mendez MA, Adair LS. Severity and timing of stunting in the first two years of life affect performance on cognitive tests in late childhood. J Nutr. 1999;129:1555–1562. [DOI] [PubMed] [Google Scholar]
- 20.Yip R, Scanlon K, Trowbridge F. Trends and patterns in height and weight status of low-income US children. Clin Rev Food Sci Nutr. 1993;33:409–421. [DOI] [PubMed] [Google Scholar]
- 21.Yip R, Scanlon K, Trowbridge F. Improving growth status of Asian refugee children in the United States. JAMA. 1992;267:975–976. [PubMed] [Google Scholar]
- 22.Olness K, Yip R, Indritz A, Torjesen E. Height and weight status of Indochinese refugee children: an anthropometric study of 1,650 children. Am J Dis Child. 1984;138:544–547. [DOI] [PubMed] [Google Scholar]
- 23.Hop LT, Gross R, Giay T, Scholtink W, Thuan BT, Sastroamidjojo S. Longitudinal observation of growth of Vietnamese children in Hanoi, Vietnam from birth to 10 years. Eur J Clin Nutr. 1997;51:164–171. [DOI] [PubMed] [Google Scholar]