Abstract
Objectives. This study assessed the contribution of age and other risk factors to racial disparities in rates of moderately low birthweight (MLBW; 1500–2499 g) and very low birthweight (VLBW; <1500 g).
Methods. Logistic regression models were developed to determine the effects on MLBW and VLBW of maternal age, race, and poverty, adjusting for birth order, smoking, substance abuse, marital status, and educational level. The sample consisted of 158 174 singleton births to US-born African American and White women in New York City between 1987 and 1993.
Results. The effects of maternal age on MLBW varied by race and poverty, with the most extreme effects among poor African American women. The effects of maternal age on VLBW also varied by race, but these effects were not moderated by poverty. Community poverty had a significant effect on MLBW among African American women, but no effect on VLBW. The adverse effect of older maternal age on MLBW and VLBW did not vary with community poverty.
Conclusions. Older maternal age is associated with reduced birthweight among infants born to African American women, and the age effect is exacerbated by individual poverty.
The persistence of a Black–White gap in low birthweight (LBW) and very low birthweight (VLBW) rates in the United States continues to be a serious public health problem. African American infants are more than twice as likely as White infants to be born weighing less than 2500 g (14.2% vs 6.3%), and almost 3 times as likely to be born weighing less than 1500 g (3.1% vs 1.2%).1 The vast majority of births under 1500 g are associated with preterm delivery—the leading cause of death among African American infants in the United States.2,3
For the most part, the risks for LBW and VLBW births have been “individualized,” emphasizing those characteristics of individuals that increase the likelihood of a low-weight delivery rather than environmental and social factors affecting population rates.4 Although African American women carry a disproportionate burden of individual risk factors, such as unmarried status and late entry into prenatal care,5 racial differences in the distribution of such risks do not explain the disparity in birth outcomes,6 nor are interventions based on these factors likely to reduce the racial gap.7–9 Furthermore, some individual risk factors operate differently across racial/ethnic groups,10–15 making it difficult to adjust meaningfully for confounders in studies involving multiple racial groups and potentially biasing estimates of effect.16
Recent reports suggest that older maternal age is also associated with increased risk of low birthweight among singletons, but this effect has been described among African American women only.17–19 Geronimus has termed the deterioration in reproductive health status over the childbearing years among African American women “weathering.”11 Although these findings suggest that maternal age operates differently for African American and White women, studies of birth outcomes generally treat this factor as a covariate or confounder, rather than exploring the joint impact of maternal age, race, and other risk factors.
Recently, there has been renewed public health interest in the role of community and other social-structural factors as determinants of birth outcomes,20–23 providing additional insight into racial disparities. For example, rates of LBW and VLBW are higher in US cities than the suburbs or the nation as a whole,24 with the highest rates found in the largest cities.25 Ecological influences on birth outcomes have also been demonstrated within racial/ethnic groups, further supporting the idea that residential context (or factors associated with residential context) may have important health consequences.
Polednak found that infant mortality rates among African Americans differed by degree of racial segregation, possibly because highly segregated areas are characterized by extremely concentrated poverty, inadequate health care, substandard housing, crime, and other stressors.26 Consistent with this finding is a report that rates of LBW (specifically, intrauterine growth retardation) among lowincome African Americans are higher for women who reside in more violent, as compared with less violent, communities. 27 Finally, a number of studies have shown that African American women born in the United States have higher rates of LBW than African American women born outside the United States, suggesting the importance of nativity in addition to community of current residence.28,29
The question arises as to whether maternal age operates as a risk factor for pregnant women entirely at the individual level (possibly in concert with other individual-level risk factors) or whether the aging effect also expresses the cumulative impact of some higher-level conditions or exposures on birth outcomes.8 At first look, maternal age would seem to offer little explanation for the Black–White gap in LBW or VLBW rates. To begin with, a racial gap is clearly evident at all maternal ages.5–7 In addition, the distribution of births by maternal age peaks much earlier for African Americans than for Whites, so that a larger proportion of African American births occur to women who are actually at lowest risk for LBW delivery.1
Nevertheless, the few studies that have looked at the impact of maternal age in community context suggest that geographic variations in magnitude of the maternal age effect may provide clues to the presence of exposures in certain populations that erode reproductive health outcomes over the childbearing years, possibly shedding light on the causes of racial disparities at all ages. For example, Geronimus reported that the effect of maternal aging on birthweight (weathering) is magnified among African American women who reside in low-income, as compared with high-income, urban areas,19 suggesting that the impact of maternal age on birth outcomes may depend on some underlying processes associated with social or residential context.
Findings such as these have prompted researchers to employ contextualized, multilevel analytic strategies to take into consideration social-structural influences on health.30–33 In one of the few perinatal studies that used multilevel modeling techniques, O'Campo et al.34 demonstrated that associations between individual risk factors and LBW were moderated by neighborhood characteristics. Specifically, the adverse impact of older maternal age on infant birthweight was more pronounced under community conditions of high unemployment.
The present study was undertaken to explore the impact of maternal age on infant birthweight under varying community conditions while taking into consideration the role of individual risk factors. Specifically, we aimed to clarify the contribution of maternal age to the likelihood of moderately low birthweight (MLBW) and VLBW among African American and White women living in a major urban area and to determine whether the association between older maternal age and low birthweight depends on community conditions.
METHODS
Study Population
The study included all first and second singleton births to US-born non-Hispanic African American and White women aged 20 to 39 years who delivered in New York City from 1987 to 1993 (n = 158 174). Third and higher-order births were excluded to eliminate the potentially confounding effects of high birth order and repeated short interpregnancy intervals. Multiple births were excluded to eliminate confounding due to the effects of fertility drugs on the maternal age–birthweight relationship. Because of the focus on the rise in reproductive risk with increasing maternal age following a period of minimum or baseline risk for MLBW and VLBW, the study included women from 20 through 39 years of age. Women born outside the United States and women of Hispanic origin were excluded to eliminate nativity-related influences on birth outcomes.
Data Collection
All individual-level data were obtained from New York City birth certificates (Bureau of Vital Statistics, New York City Department of Health) for the years 1987 through 1993. The data consisted of birthweight, race/ethnicity, maternal health, area of residence, maternal age, birth order, marital status, educational level, mother's place of birth, Medicaid status, and whether or not the mother smoked cigarettes or used drugs during pregnancy. Receipt of Medicaid during the perinatal period was used as a proxy for very low income. (In 1990, the annual income ceiling for Medicaid eligibility, regardless of marital status, ranged from $8200 for a family of 2 to $10 300 for a family of 4, with total resources not exceeding $5100 or $7100, respectively.) The outcomes of interest were MLBW (1500–2499 g) and VLBW (<1500 g), mutually exclusive categories, each assessed by a single binary item. The VLBW category largely comprises preterm deliveries, a classification that is etiologically distinct from MLBW (which includes some preterm but mostly full-term low-weight infants). The referent group for MLBW births excluded VLBW births.
Individual-level data were linked to aggregate-level data obtained from the 1990 US census for 328 health areas in New York City (1990 US decennial census, summary tape file 3a). The health area is a geographic unit established by the New York City Department of Health for statistical reporting of community health status indicators. It consists of 4 to 6 census tracts (approximately 20 000 people) and was adopted as the unit of analysis because sample sizes were large enough to yield stable estimates of relationships between risk factors and birth outcomes for both African American and White women in each health area.
Data Analysis
Age-specific analyses of MLBW and VLBW rates provided a cross-sectional view of birth outcomes across the childbearing years, stratified by race and birth order. Logistic regression was used to estimate the odds of MLBW and VLBW by maternal age, after controlling for the effects of the other individual-level risk factors. The odds ratio was used as an approximation of the relative risk of VLBW and MLBW, to show the increase in risk for each year of maternal age. The value of a was set at .01, and we report 99% confidence intervals (CIs) for all analyses. Comparisons of slopes across models employed the test statistic for parallelism, distributed as a Student t.35
All covariates derived from New York City birth certificate data for use in these models were well-established risk factors for MLBW or VLBW: smoking (yes/no), unmarried status (yes/no), substance use (yes/no), Medicaid status (yes/no), and educational level (measured continuously in years). All risk factors were coded so that a high numeric value represents high risk (the education scale was inverted).
The racial and economic distribution of births within New York City communities provided sufficient variability to permit multilevel analysis. We hypothesized (1) that MLBW and VLBW rates would increase with community poverty and (2) that the association of older maternal age with MLBW and VLBW would be stronger in low-income than in higherincome communities. Community-level poverty was defined by US census data, using the proportion of residents falling below the federal poverty line for each of the 328 New York City health areas. This continuous measure was then divided into tertiles (empirical thirds of the total distribution) representing low (0%–13%), medium (14%–20%), and high (>20%) poverty.
To detect main and cross-level effects of community poverty on individual risk, we employed the nonlinear version of hierarchical linear modeling (hierarchical generalized nonlinear modeling, or HGLM), a recently developed approach that is suited to binary outcomes.36 HGLM involves a 2-stage regression or “slopes as outcomes” approach, which we used to quantify and test (1) the main effect of community poverty on MLBW or VLBW and (2) the extent to which community poverty moderates the impact of individual risk factors.
RESULTS
Individual-Level Factors
Table 1 ▶ shows the distribution of sociodemographic and behavioral risk factors by race and birth order for the study population. Inspection of the table reveals substantial differences by race; African American women were more likely than White women to be Medicaid recipients and unmarried at the time of birth, to report substance use in pregnancy, to smoke during pregnancy, and to have completed fewer years of education. In addition, the distribution of first and second births to African American (as compared with White) women for the entire 7-year study period was more highly concentrated in the 20- to 24-year-old age category, with the proportion of births declining steadily through the childbearing years.
TABLE 1.
—Demographic Characteristics of the Population: Singleton Births to US-Born African American and White Women (n = 158 174): New York City, 1987–1993
| First Births, % | Second Births, % | |||
| White (n = 59 370) | African American (n = 31 260) | White (n = 41 601) | African American (n = 25 943) | |
| Maternal age, y | ||||
| 20–24 | 23.3 | 52.0 | 18.3 | 47.7 |
| 25–29 | 36.3 | 28.9 | 32.2 | 31.5 |
| 30–34 | 29.1 | 14.0 | 34.2 | 15.2 |
| 35–39 | 11.4 | 5.1 | 15.5 | 5.3 |
| Smokinga | 4.7 | 6.8 | 6.2 | 9.3 |
| Medicaid receipt | 7.6 | 45.3 | 8.8 | 44.1 |
| Substance usea | 2.2 | 5.2 | 2.5 | 5.7 |
| Unmarried status | 12.6 | 73.3 | 11.5 | 69.3 |
| Education, y | ||||
| 0–8 | 0.5 | 0.9 | 0.5 | 0.6 |
| 9–11 | 3.6 | 20.0 | 4.9 | 19.3 |
| 12 | 39.4 | 45.1 | 38.9 | 44.0 |
| 12+ | 56.5 | 33.7 | 55.7 | 36.1 |
aDuring current pregnancy.
Table 2 ▶ shows the unadjusted rates of MLBW and VLBW by maternal age category, race, and birth order. Overall, African American women were approximately 4 times as likely as White women to deliver a VLBW infant, and they were increasingly likely to deliver a VLBW infant with advancing maternal age (beyond 20 years). This age-related trend was highly significant for first births (χ2 = 44.05, P < .001) but not for second births (χ2 = 4.69, P = .20). Among Whites, there was no significant increase in VLBW with maternal age for first (χ2 = 4.99, P = .17) or second (χ2 = 2.33, P = .53) births. The significant increase in crude VLBW rates with advancing maternal age for African American, but not White, first births contributes to a racial gap for first births that widens significantly with increasing maternal age.
TABLE 2.
—Rates of Very Low and Moderately Low Birthweight, by Maternal Age, Race, and Birth Order: Singleton Births to US-Born Women (n = 158 174), New York City, 1987–1993
| Maternal Age, y | ||||||||||
| 20–24 | 25–29 | 30–34 | 35–39 | All | ||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| Very low birthweight | ||||||||||
| African American | ||||||||||
| First births | 16 258 | 2.3 | 9034 | 3.0 | 4377 | 3.6 | 1591 | 4.7 | 31 260 | 2.8 |
| Second births | 12 386 | 2.1 | 8161 | 2.4 | 4030 | 2.6 | 1366 | 2.6 | 25 943 | 2.3 |
| White | ||||||||||
| First births | 13 804 | 0.7 | 21 523 | 0.6 | 17 269 | 0.6 | 6774 | 0.9 | 59 370 | 0.7 |
| Second births | 7631 | 0.6 | 13 411 | 0.6 | 14 242 | 0.5 | 6317 | 0.7 | 41 601 | 0.6 |
| Moderately low birthweight | ||||||||||
| African American | ||||||||||
| First births | 15 879 | 10.1 | 8764 | 12.7 | 4220 | 14.1 | 1517 | 16.1 | 30 380 | 11.7 |
| Second births | 12 129 | 9.5 | 7969 | 10.8 | 3927 | 11.9 | 1330 | 12.9 | 25 355 | 10.5 |
| White | ||||||||||
| First births | 13 704 | 4.6 | 21 387 | 4.0 | 17 157 | 4.4 | 6715 | 5.2 | 58 963 | 4.4 |
| Second births | 7583 | 4.0 | 13 333 | 3.2 | 14 169 | 3.4 | 6275 | 3.9 | 41 360 | 3.5 |
African American women were more than twice as likely as White women to deliver a MLBW infant (lower portion of Table 2 ▶), and the rate of MLBW increased dramatically with maternal age for both first (χ2 = 96.8, P < .001) and second (χ2 = 29.11, P < .001) births to African American women. Age effects were also significant for both firstborn (χ2 = 19.88, P < .001) and second-born White infants (χ2 = 13.03, P < .01), although the age-related trend does not appear before the maternal age of 30. The greater increase in MLBW rates with increasing age among African American women contributes to a larger racial disparity at older maternal ages.
To determine whether or not these patterns of MLBW and VLBW over the childbearing years were explained by the distribution of other individual risk factors, we conducted logistic regression analyses, adjusting for demographic and behavioral characteristics: age, race, parity, unmarried status, smoking, Medicaid, substance use, and years of education. Table 3 ▶ shows the results of separate regression models for MLBW and VLBW. The first model for each outcome tested the main effect of each risk factor, adjusted for effects of all other individual risk factors. In the second model for each outcome, we tested the effects of all possible age × risk factor interactions. Only significant age × risk factor cross-product terms are shown in Table 3 ▶.
TABLE 3.
—Odds Ratios (ORs)and 99% Confidence Intervals (CIs) for Moderately Low Birthweight (MLBW) and Very Low Birthweight Associated With Demographic and Behavioral Risk Factors: Singleton Births to US-Born Women (n = 158 174), New York City, 1987–1993
| Moderately Low Birthweight | Very Low Birthweight | |||
| Model 1 | Model 2a | Model 1 | Model 2a | |
| Adjusted OR (99% CI) | Adjusted OR (99% CI) | Adjusted OR (99% CI) | Adjusted OR (99% CI) | |
| Maternal ageb | 1.03 (1.03, 1.04) | 1.01 (1.01, 1.02) | 1.03 (1.02, 1.05) | 1.01 (0.99, 1.03) |
| African American race | 2.10 (1.95, 2.25) | 1.19 (0.85, 1.68) | 3.08 (2.64, 3.60) | 1.43 (0.67, 3.06) |
| First birth | 1.21 (1.14, 1.28) | 1.20 (1.13, 1.27) | 1.24 (1.10, 1.39) | 1.23 (1.09, 1.38) |
| Medicaid receipt | 1.10 (1.03, 1.18) | 0.57 (0.41, 0.80) | 0.88 (0.77, 1.01) | 0.57 (0.29, 1.15) |
| Smokingc | 1.43 (1.30, 1.57) | 1.41 (1.28, 1.55) | 1.18 (0.96, 1.44) | 1.16 (0.95, 1.42) |
| Substance usec | 2.42 (2.18, 2.68) | 2.39 (2.15, 2.65) | 2.15 (1.74, 2.65) | 2.12 (1.72, 2.62) |
| Unmarried status | 1.70 (1.58, 1.83) | 1.70 (1.58, 1.83) | 1.72 (1.48, 2.01) | 1.73 (1.48, 2.02) |
| Educationb | 1.15 (1.12, 1.18) | 1.14 (1.11, 1.17) | 1.15 (1.09, 1.20) | 1.14 (1.09, 1.20) |
| Age × African American race | . . . | 1.02 (1.01, 1.03) | . . . | 1.03 (1.00, 1.06) |
| Age × Medicaid receipt | . . . | 1.03 (1.01, 1.04) | . . . | 1.02 (0.99, 1.04) |
aModel 2 includes all significant cross-product terms, including maternal age, that were significant at the .01 level.
bMeasured continuously in years. For age, the adjusted odds ratio is interpreted as the percentage increase in the odds of MLBW or VLBW for each 1-year increase in age; for education, the adjusted odds ratio is interpreted as the percentage increase in the odds of MLBW or VLBW for each 1-year decrease in education.
cDuring current pregnancy.
After adjustment for the effects of other risk factors, both age and race remained significant predictors: older women and African American women were at increased risk for both MLBW and VLBW. With respect to MLBW, in addition to the main effects of age and race, there were 2 significant age × risk factor interactions, indicating that the adverse impact of older maternal age was significantly heightened among African American women and among those receiving Medicaid. With respect to VLBW, the age × race term was only marginally significant (P < .05), indicating that the adverse impact of maternal aging on VLBW was only slightly greater among African American women. There was no heightened risk for women receiving Medicaid. While crude rates indicated a larger maternal age effect among firstborns (Table 2 ▶), regression analyses revealed no significant effect modification by birth order in any model after adjustment for other individual risk factors.
The presence of effect modification by race and poverty prompted further stratum-specific analyses. We constructed 4 regression models for MLBW and 4 models for VLBW to estimate the size of the maternal age effect associated with each combination of race and poverty, after adjusting for smoking, substance abuse, parity, marital status and education. The test statistic for parallelism was used to compare the magnitude of the odds ratios for maternal age effects across models.35 The results, summarized in Table 4 ▶, show that there is a significant effect of maternal age on MLBW in all 4 race-and-poverty groups, such that the likelihood of MLBW increases with advancing maternal age.
TABLE 4.
—Summary of Effects of Maternal Age on Moderately Low and Very Low Birthweight From Logistic Regression Analyses for 4 Strata Defined by Race and Poverty Level,a Adjusted for Other Individual Risk Factorsb: Singleton Births to US-Born Women (n = 158 174), New York City, 1987–1993
| Very Low Birthweight, | Moderately Low Birthweight, | |
| Race and Poverty Stratum | Adjusted OR (99% CI) | Adjusted OR (99% CI) |
| African-American | ||
| Medicaid | 1.05 (1.03, 1.08) | 1.06 (1.05, 1.08) |
| Non-Medicaid | 1.04 (1.02, 1.06) | 1.03 (1.02, 1.04) |
| White | ||
| Medicaid | 1.04 (0.97, 1.09) | 1.03 (1.00, 1.05)c |
| Non-Medicaid | 1.02 (0.99, 1.04) | 1.02 (1.01, 1.03) |
Note. OR = odds ratio; CI = confidence interval.
aPoverty was defined by receipt of Medicaid during the perinatal period.
bSmoking, unmarried status, substance use, parity, and education.
cThe 99% confidence interval does not include 1; the lower confidence limit was rounded from 1.002 to 1.00.
The age effect for births to African American women receiving Medicaid was significantly greater than the age effect for births to African American women who were not receiving Medicaid (t = 5.13, P < .001). Furthermore, the age effect was significantly greater for African American Medicaid recipients than for White Medicaid recipients (t = 3.66, P < .001). Perhaps most important, there were no significant racial differences in the strength of the maternal age effect among women who were not receiving Medicaid (t = 1.94, NS), suggesting that the bulk of the racial disparity is driven by poverty. There were significant maternal age effects on VLBW among African American but not White women, regardless of Medicaid status.
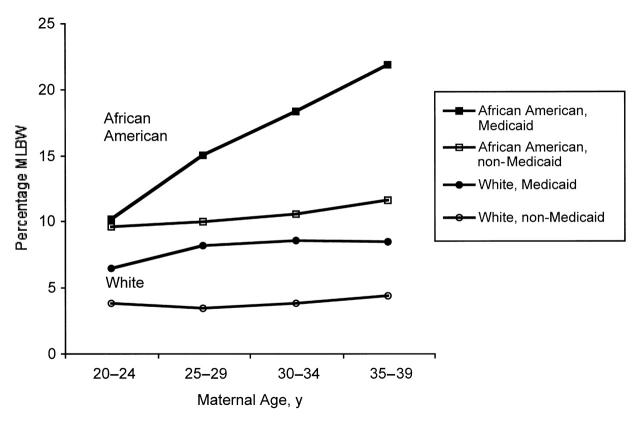
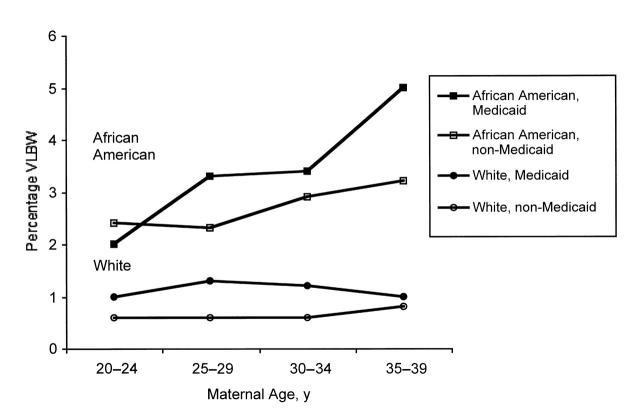
Figure 1 ▶ shows the dramatic nature of the stratum-specific MLBW rates in New York City, using unadjusted rates to illustrate the interactions demonstrated by the regression models. Although a racial disparity is present across the childbearing years, it is clear that the age-related increase is largely concentrated among very poor African American women. Figure 2 ▶ shows that the highest rates of VLBW are also concentrated among poor African American women, but the poverty effect is less dramatic. Among White women, there is no significant age or poverty effect on VLBW.
FIGURE 1.
—Rates of moderately low birthweight (MLBW) among first and second births to US-born women in New York City, by maternal age, race, and poverty, 1987–1993.
FIGURE 2.
—Rates of very low birthweight (VLBW) among first and second births to US-born women in New York City, by maternal age, race, and poverty, 1987–1993.
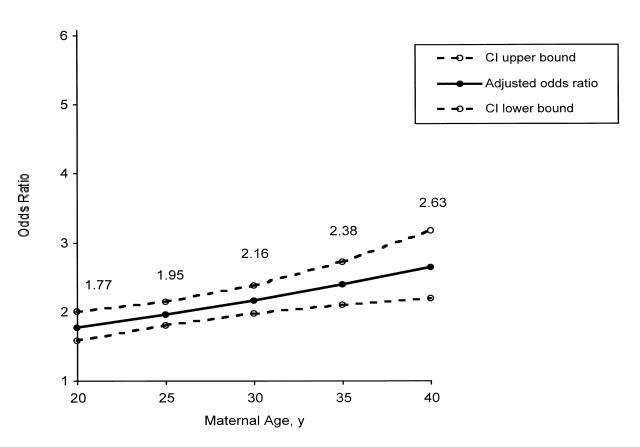
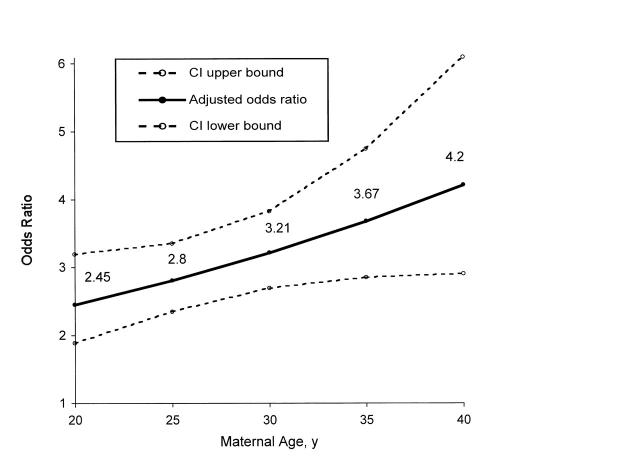
To highlight the contribution of maternal age to racial disparities in birthweight outcomes across the childbearing years, we used the regression weights from the omnibus logistic regression models shown in Table 3 ▶ to calculate the odds of MLBW and VLBW, respectively, for African American women in 5 age categories, with all other risks (including age-related interactions) held constant.37 The odds ratios are interpreted as the likelihood that an African American woman, as compared with a White woman, will experience MLBW (or VLBW) at a particular age, all other risks being equal. As shown in Figures 3 and 4 ▶ ▶, the odds ratios increase steadily from age 20 through age 40 for both MLBW and VLBW, illustrating the contribution of the maternal age effect (“weathering”) to increasing racial disparities over the childbearing years.
FIGURE 3.
—Adjusted odds ratios and 99% confidence intervals (CIs) for moderately low birthweight among first and second births to US-born African American women in New York City, 1987–1993.
FIGURE 4.
—Adjusted odds ratios and 99% confidence intervals (CIs) for very low birthweight among first and second births to US-born African American women in New York City, 1987–1993.
Community-Level Effects
To explore the impact of community-level poverty on race-specific rates of VLBW and MLBW and the magnitude of maternal age effects, we assigned individual births to high-, medium-, and low-poverty communities on the basis of maternal address at the time of delivery. Table 5 ▶ shows crude MLBW and VLBW rates by maternal age, race, and community poverty level. There is an unadjusted effect of community poverty for African American and White women at all ages—the poorer the community, the higher the rates of MLBW. In addition, among African American women, the age effect is most extreme in the poorest communities. With respect to VLBW, there is no indication of either a main community effect or an age × community poverty interaction.
TABLE 5.
—Rates of MLBW and VLBW Among US-born African American and White Women (n = 158 174), by Age and Community Poverty Level: New York City, 1987–1993
| Maternal Age, y | |||||||||||||||
| 20–24 | 25–29 | 30–34 | 35–39 | Overall | |||||||||||
| Community Poverty Level | MLBW | VLBW | n | MLBW | VLBW | n | MLBW | VLBW | n | MLBW | VLBW | n | MLBW | VLBW | n |
| African American | |||||||||||||||
| High poverty | 10.6 | 2.3 | 15 083 | 13.2 | 3.0 | 8374 | 15.7 | 3.3 | 3735 | 16.2 | 4.0 | 1306 | 12.3 | 2.7 | 28 498 |
| Medium poverty | 9.4 | 2.0 | 9339 | 10.9 | 2.4 | 5939 | 11.5 | 2.8 | 3119 | 14.5 | 3.8 | 1088 | 10.5 | 2.4 | 19 485 |
| Low poverty | 8.2 | 2.3 | 4222 | 9.6 | 2.3 | 2816 | 9.7 | 3.1 | 1553 | 11.0 | 3.0 | 563 | 9.1 | 2.5 | 9 220 |
| White | |||||||||||||||
| High poverty | 5.2 | 0.8 | 4106 | 5.4 | 1.1 | 2009 | 4.8 | 0.7 | 1367 | 5.3 | 1.2 | 644 | 5.2 | 0.9 | 8126 |
| Medium poverty | 4.4 | 0.7 | 8357 | 3.8 | 0.7 | 10 489 | 4.3 | 0.7 | 9012 | 4.2 | 0.8 | 4071 | 4.2 | 0.7 | 31 929 |
| Low poverty | 4.0 | 0.6 | 8972 | 3.5 | 0.5 | 22 436 | 3.7 | 0.6 | 21 132 | 4.7 | 0.7 | 8376 | 3.8 | 0.6 | 60 916 |
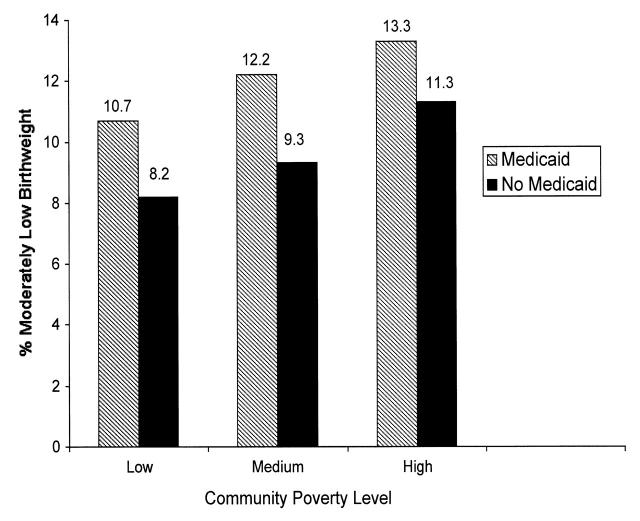
To determine whether the apparent main effect of community poverty on MLBW is simply a proxy for the individual poverty effect, we stratified the MLBW rate for African American women into Medicaid and non-Medicaid groups at each level of community poverty. Figure 5 ▶ shows that the community poverty effect is relatively constant across Medicaid and non-Medicaid groups and that the effect of individual poverty is similar at each level of community poverty. There is no suggestion of an interaction between individual and community poverty.
FIGURE 5.
—Effect of individual and community poverty on moderately low birthweight among first and second births to US-born African American women in New York City, 1987–1993.
Multilevel Modeling
The main effect of community poverty on MLBW rates (suggested by both Table 5 ▶ and Figure 5 ▶) could be a function of the association between community poverty and other individual-level risk factors. That is, women living in the poorest communities are more likely to be unmarried at the time of birth, to abuse drugs, and so forth, than women living in more affluent communities, introducing a form of aggregation bias to estimates of effect. A more rigorous test of the community effect on MLBW requires simultaneous adjustment for the effects of differences in the distribution of all individual risks between communities. The question is whether 2 women who have similar individual risk profiles (Medicaid coverage, smoking during pregnancy, etc.) but live in different kinds of communities have the same probability of delivering a MLBW baby, or whether the probability of MLBW varies as a function of the poverty level in the community of residence.
The second question concerns the impact of maternal aging in different types of communities; that is, does the association between older maternal age and MLBW become stronger as a function of community poverty? To answer these questions, we used HGLM. Nonlinear modeling was used because the birthweight outcomes are dichotomous. In the level 1 models, MLBW and VLBW were regressed on individual risk factors and interaction terms within each of the 328 health areas (level 1 model: log[P/(1 – P)] = β0 + β1 [unmarried] + β2 [Medicaid], etc.), making this the HGLM equivalent of a logistic regression model. In the level 2 models, the regression coefficients (slopes and intercepts) from the level 1 models become the outcomes, and the unit of analysis shifts to the health area level. The level 2 model tests, within health areas, (1) whether community poverty predicts the absolute MLBW or VLBW rate (within health area intercepts as outcomes) and (2) whether community poverty predicts the strength of association between maternal age and birthweight (within health area slopes as outcomes).
In HGLM, the effects of community poverty are adjusted for all covariates, both individual-level and community-level. The level 2 model is given by
 |
where γq0 and γq1 are the level-2 intercept and slope for community poverty with respect to the outcome Bqj; Wj is the value of community poverty for the jth health area; and uqj is a level-2 random effect.
For the analysis of community-level effects on birth outcomes, 158 174 births were nested within 328 health areas.
The final estimates of effects in racespecific HGLM models for VLBW and MLBW revealed a significant main effect of community poverty on MLBW among African American women only (γ01 = 0.0723, 99% CI = 0.0176, 0.1270), after controlling for the individual-level effects of maternal age, birth order, Medicaid, marital status, smoking, substance abuse, education, and the 2 interaction terms involving age that were significant in the original logistic regression models. Among White women, there was no main effect of community poverty on MLBW (γ01 = 0.0326, 99% CI = –0.0500, 0.1152).
Furthermore, there is no evidence for cross-level effects in either racial group, meaning that the effect of maternal aging on MLBW is not exacerbated by community poverty when individual risk is controlled. The age × community poverty effect for African Americans was γ91 = 0.0103 (99% CI = –0.0241, 0.0447); for Whites, it was γ91 = 0.0149 (99% CI = –0.0263, 0.0561). With respect to VLBW, there were no significant main (African Americans, γ01 = 0.0143, 99% CI = –0.0933, 0.1219; Whites, g01 = 0.0204, 99% CI = –0.1780, 0.2188) or cross-level (African Americans, γ91 = –0.0106, 99% CI = –0.0761, 0.0148; Whites, γ91 = –0.0632, 99% CI = –0.1573, 0.0308) community effects.
DISCUSSION
In New York City between 1987 and 1993, African American women were almost 4 times as likely as White women to deliver a VLBW infant and 2 to 3 times as likely to deliver a MLBW infant, for both first and second births. Crude rates revealed a steady increase in the proportion of VLBW and MLBW with advancing maternal age for African American women, and this trend was most marked for first births. After adjusting for demographic and health behavioral risk factors, multivariate analyses showed that African American women still experienced increased risk of VLBW and MLBW with advancing age.
Among White women, adjusted analyses revealed a small but significant age-related increase for MLBW, but no maternal age effect for VLBW. The extreme age-related effects observed for African American women in relation to MLBW were largely concentrated among poor women. In fact, among women not receiving Medicaid, the increased risk of MLBW with advancing maternal age was not significantly greater for African Americans than for Whites, after adjustment for other individual risk factors. This finding supports the idea that racial differences in the effect of maternal aging on MLBW are exacerbated by, or depend on, individual poverty.
The joint impact of maternal age and poverty on MLBW, a category of births reflecting fetal growth problems, may reflect length of exposure to poverty-related factors such as nutritional status, prepregnancy weight, and weight gain during pregnancy. As suggested by Geronimus, individual poverty and the stresses that accompany poverty may work to erode overall health among African American women, with serious consequences for MLBW, regardless of birth order.19 Our results support this idea by showing that the age effect is most extreme among poor African American women.
With respect to VLBW, an outcome associated with preterm delivery, exposure to individual poverty does not exacerbate the maternal age effect. In this study, VLBW was only a crude proxy for preterm birth, an outcome that likely comprises a number of etiologically distinct categories. In the absence of more accurate birth certificate data for gestational age and a more refined classification system for preterm births,38 possible differential effects of maternal age and poverty on different categories of preterm deliveries cannot be evaluated.
In addition to the contribution of individual poverty (as defined by Medicaid eligibility), we explored the impact of community socioeconomic conditions on the age-related patterns. Holding individual-level risk factors constant, we found a significant main effect of community poverty on MLBW rates for African American but not White women, such that MLBW rates among African American women were higher in the poorer communities. That is, if 2 African American women have similar individual risk profiles, but woman A lives in one of the poorest communities in New York City and woman B lives in a more affluent community, then woman A is at higher risk for MLBW than woman B. Multilevel modeling also enabled us to test cross-level effects—the potential moderating effects of community poverty on the predictive power of individual risk factors. There was no indication that community poverty exacerbated the effects of individual poverty or maternal aging over the childbearing years.
Several other studies have reported cross-level effects on weathering, finding that the risk associated with older maternal age was greater in the presence of community poverty. For example, Geronimus found a weathering pattern among African American women with respect to MLBW only in the presence of community poverty, with no weathering in the more affluent communities.19 Although the crude rates in the present study intimated such an interactive effect, multilevel analyses, adjusted for individual social and health behavioral factors, did not confirm this finding. Rather, after adjustment for individual poverty, the age-related pattern was observed for African American women at all community income levels.
The significance of this age-related effect among African American women residing in higher-income communities (and hence, a constant effect across the whole range of communities) may have been detectable in the present study because of the large sample size; there were 11 364 births to African American women who were at least 30 years of age, and of these, 2116 women were residing in higher-income communities.
The interpretation of community-level effects in this and other studies is, at best, a perilous enterprise, even when one attempts to take individual-level risk into account. At the individual level, we used maternal Medicaid status (yes/no) at the time of delivery as a proxy for poverty. Poverty, of course, is not a dichotomous phenomenon. It may well be that African American women receiving Medicaid and living in the very poorest communities are more impoverished than African American Medicaid recipients living in more affluent communities, and that we have failed to capture this variability despite the attempt to measure poverty at both the individual and the community level. For this reason, the community effect may simply reflect incomplete measurement of individual-level risk.
Furthermore, there are many unanswered questions about the scale or radius of influence on birth outcomes. The health area is a large “community” and may not conform to the boundaries that define an individual woman's sense of space. Although community income has been shown to be the dominant factor differentiating communities in New York City,39 it is only a crude indicator for a web of social and environmental exposures.40,41 These exposures include norms regarding health practices, political power structures, low social capital,42 discrimination, and many other social stressors that disproportionately visit African American women as well as the communities in which they live.27,43,44 Furthermore, it may be the burden of deprivation relative to the advantages of other groups or individuals living nearby that is actually responsible for the adverse effects of low income on general health status.45,46
But while the interpretation of a community poverty effect for African American women is debatable, the finding is nevertheless important. First, the presence of significant community effects, over and above the contribution of individual risk factors, underscores the importance of poverty-related risk (regardless of its scale) for MLBW among African American women and further suggests that this risk may be associated with the quality of the communities in which women reside in large urban areas (a nonrandom and race-related phenomenon).
Second, although individual income as an indicator of poverty or wealth is unreliable and subject to fluctuations over short time periods, community conditions change more slowly, providing a more constant set of influences on individual health. To the extent that women are exposed to similar kinds of community environments in the period leading up to and during their childbearing years, community-level effects, however crudely measured, capture a more chronic view of poverty- and racerelated experience. At the community level, it is very likely that inequalities in health result from group differences in exposure to an accumulation of health-damaging or health-promoting environments over time.47–52
Just as Starfield et al.18 have shown (at the individual level) that it is chronic poverty rather than a brief period of welfare receipt that is most predictive of birth outcomes, studies are needed to explore residential history or patterns of exposure to various community conditions and how these cumulative exposures relate to reproductive health outcomes throughout the childbearing years. Such studies will almost certainly require new analytic strategies to take into consideration a more dynamic interaction of individuals with each other as well as multiple exposures over time.33
In summary, the age-related patterns of MLBW and VLBW seen in this New York City population provide a picture of differential reproductive risk over the childbearing years as a function of individual poverty and race. The actual size of the racial disparity in MLBW and VLBW at any time will depend on several conditions: (1) the increasing odds of MLBW and VLBW with increasing maternal age, as demonstrated in Figures 3 and 4 ▶ ▶; (2) the distribution of births by maternal age in each racial group; and (3) the distribution of births by community type.
During the 1987–1993 study period, the age distribution of births to African American women changed. In 1987, 9.3% of all African American singleton births in New York City were to women aged 35 years or older. In each successive year, the percentage increased by approximately 0.5%, so that by 1993, 12.8% of all African American singleton births were to women aged 35 years and older. To the extent that this trend continues,5 there will be increasing numbers of African American women exposed to “weathering” (the processes underlying maternal age–related risk) and the racial disparity will persist.
Although a discussion of the race–poverty link (and how individuals “choose” or are selected into urban communities) is beyond the scope of this article, disproportionately higher rates of individual and community poverty among African American, as compared with White, women will also contribute to the disparity. It is clear that being African American and poor at 20 years of age carries meaningful reproductive risks, but the incidence of low-birthweight outcomes to poor African American women after the age of 30 is truly alarming. For poor women, and especially for poor African American women, maternal age undoubtedly reflects length of exposure to a lifetime of health-eroding experiences, a factor captured, but not fully explained, by Geronimus' elegant and unsettling construct of weathering. The public health challenge is now to assess and redress these exposures.30
Acknowledgments
This work was supported in part by funding from the National Institute of Environmental Health Sciences (project 1-P50-ES09600), the US Environmental Protection Agency (project R827027), and the March of Dimes Perinatal Data Center.
We thank Ming X. Tang and Bruce Levin for guidance with respect to statistical analysis and Sharon Schwartz for helpful comments. Birth certificate data were provided by the New York City Department of Health. Community-level data were derived from the INFOSHARE system, Community Studies, Inc.
V. A. Rauh and H. F. Andrews designed the study and wrote the article. R. S. Garfinkel and H. F. Andrews conducted the data analysis.
Peer Reviewed
References
- 1.Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Report of final natality statistics, 1996. MonthVital Stat Rep. 1998;46(11, suppl). [PubMed]
- 2.Centers for Disease Control and Prevention. Preterm singleton births—United States, 1989–1996. MMWR Morb Mortal Wkly Rep. 1999;48:185–189. [PubMed] [Google Scholar]
- 3.England L, Ferre C, Martin JA, Hogan V. Trends in Preterm Birth Among Singletons, US 1989–1996. Atlanta, Ga: National Center for Chronic Disease Prevention and Health Promotion; September 1999.
- 4.Goldenberg RL, Iams JD, Merces BM, et al. The preterm prediction study: the value of new vs standard risk factors in predicting early and all spontaneous preterm births. Am J Public Health. 1998;88:233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Summary of Vital Statistics, 1997. New York, NY: City of New York, Office of Vital Statistics and Epidemiology, New York Dept of Health; 1997.
- 6.Institute of Medicine. Preventing Low Birthweight. Washington, DC: National Academy Press; 1985. [PubMed]
- 7.Guyer B, Strobino DM, Ventura SJ, Singh GK. Annual summary of vital statistics. Pediatrics. 96:1029–1039. [PubMed]
- 8.Schwartz S, Carpenter KM. The right answer for the wrong question: consequences of type III error for public health research. Am J Public Health. 1999;89:1175–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wise P. Confronting racial disparities in infant mortality: reconciling science and politics. Am J Prev Med. 1993;9(suppl):7–16. [PubMed] [Google Scholar]
- 10.Collins JW Jr, David RJ. Differences in neonatal mortality by race, income, and prenatal care. Ethn Dis. 1992;2:18–26. [PubMed] [Google Scholar]
- 11.Geronimus AT. The weathering hypothesis and the health of African American women and infants: evidence and speculations. Ethn Dis. 1992;2:207–221. [PubMed] [Google Scholar]
- 12.Kleinman J, Kessel S. Racial differences in low birthweight. N Engl J Med. 1987;317:749–753. [DOI] [PubMed] [Google Scholar]
- 13.Hogue CJ, Hargraves MA. Class, race, and infant mortality in the United States. Am J Public Health. 1993;83:9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.James SA. Racial and ethnic differences in infant mortality and low birth weight: a psychosocial critique. Ann Epidemiol. 1993;3:130–136. [DOI] [PubMed] [Google Scholar]
- 15.Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10:87–121. [DOI] [PubMed] [Google Scholar]
- 16.Kaufman J, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–628. [PubMed] [Google Scholar]
- 17.Collins JW Jr, David RJ. The differential effects of traditional risk factors in infant birthweights among blacks and whites in Chicago. Am J Public Health. 1990;80:679–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Starfield B, Shapiro S, Weiss J, et al. Race, family income, and low birth weight. Am J Epidemiol. 1991;134:1167–1174. [DOI] [PubMed] [Google Scholar]
- 19.Geronimus AT. African American/White differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42:589–597. [DOI] [PubMed] [Google Scholar]
- 20.Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv. 1999;29:295–352. [DOI] [PubMed] [Google Scholar]
- 21.Rowley DL, Hogue CJ, Blackmore CA, et al. Preterm delivery among African-American women: a research strategy. Am J Prev Med. 1993;9(suppl):1–6. [PubMed] [Google Scholar]
- 22.Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med. 1993;9(6 suppl):82–122. [PubMed] [Google Scholar]
- 23.Rowley DL. Beyond the medical model: research on social factors and preterm delivery. Prenat Neonat Med. 1998;3:170–172. [Google Scholar]
- 24.Ahmed F. Urban–suburban differences in the incidence of low birthweight in a metropolitan black population. J Natl Med Assoc. 1989;81:849–855. [PMC free article] [PubMed] [Google Scholar]
- 25.Low birthweight for selected US cities: 1993–1995. CityLights.1997;6(summer/fall).
- 26.Polednak AP. Segregation, Poverty, and Mortality in Urban African Americans. New York, NY: Oxford University Press; 1997.
- 27.Collins JW Jr, David RJ. Urban violence and African-American pregnancy outcome: an ecologic study. Ethn Dis. 1997;7:184–190. [PubMed] [Google Scholar]
- 28.David RJ, Collins JW Jr. Differing birthweight among infants of US-born blacks, African-born blacks, and US-born whites. N Engl J Med. 1997;337:1209–1214. [DOI] [PubMed] [Google Scholar]
- 29.Cabral H, Fried LE, Levenson S, Amaro H, Zuckerman B. Foreign-born and US-born black women: differences in health behaviors and birth outcomes. Am J Public Health. 1990;80:70–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geronimus AT. To mitigate, resist, or undo: addressing structural influences on the health of urban populations. Am J Public Health. 2000;90:867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Susser M. The logic in ecological, I: the logic of analysis. Am J Public Health. 1994;84:825–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diez-Roux AV. Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am J Public Health. 1998;88:216–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koopman JS, Lynch JW. Individual causal models and population system models in epidemiology. Am J Public Health. 1999;89:1170–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Campo P, Xue X, Wang MC, Caughy M. Neighborhood risk factors for low birthweight in Baltimore: a multilevel analysis. Am J Public Health. 1997;87:1113–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kleinbaum DG, Kupper LL, Muller KE. Applied Regression Analysis and Other Multivariate Methods. 2nd ed. Boston, Mass: PWS-Kent Publishing Co; 1988.
- 36.Raudenbush S, Bryk A, Cheong YF, Congdon R. HLM5: Hierarchical Linear and Nonlinear Modeling. Lincolnwood, Ill: Scientific Software International; 2000.
- 37.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York, NY: John Wiley & Sons Inc; 1989.
- 38.Klebanoff MA. Conceptualizing categories of preterm birth. Prenat Neonat Med. 1998;3:13–15. [Google Scholar]
- 39.Pittman J, Andrews H, Struening E. The use of zip-coded populations in social area studies of service utilization. Eval Program Plann. 1986;9:309–317. [DOI] [PubMed] [Google Scholar]
- 40.Mayer SE, Jencks C. Growing up in poor neighborhoods: how much does it matter? Science. 1989;243:1441–1445. [DOI] [PubMed] [Google Scholar]
- 41.Wallace R, Wallace D, Andrews H. AIDS, tuberculosis, violent crime and low birthweight in six US metropolitan areas: public policy, stochastic resonance and the regional diffusion of inner-city markers. Environ Plann. 1997;29:525–555. [Google Scholar]
- 42.Coleman JS. Social capital in the creation of human capital. Am J Sociol. 1988;94(suppl):S95–S120. [Google Scholar]
- 43.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–924. [DOI] [PubMed] [Google Scholar]
- 44.Kawachi I. Social capital and community effects on population and community health. Ann N Y Acad Sci. 1999;896:120–130. [DOI] [PubMed] [Google Scholar]
- 45.Wilkinson RG. Unhealthy Societies: The Afflictions of Inequality. London, England: Routledge; 1996.
- 46.Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self-rated health in the United States: multilevel analysis. BMJ. 1998;317:917–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young African American and white adults. Am J Public Health. 1996;86:1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–351. [DOI] [PubMed] [Google Scholar]
- 49.Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol. 1997;8:322–333. [DOI] [PubMed] [Google Scholar]
- 50.Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv. 1999;29:295–352. [DOI] [PubMed] [Google Scholar]
- 51.Lynch JW, Kaplan GA, Shema SJ. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med. 1997;337:1889–1895. [DOI] [PubMed] [Google Scholar]
- 52.Collins JW Jr, Schulte NF, Drolet A. Differential effect of ecologic risk factors on the low birthweight components of African American, Mexican-American and non-Latino white infants in Chicago. J Natl Med Assoc. 1998,90:223–229. [PMC free article] [PubMed] [Google Scholar]