Abstract
Objectives. This study estimated the prevalence of medication treatment for attention deficit–hyperactivity disorder (ADHD) among elementary school children in a North Carolina county.
Methods. Parents of 7333 children in grades 1 through 5 in 17 public elementary schools were asked whether their child had ever been given a diagnosis of ADHD by a psychologist or physician and whether their child was currently taking medication to treat ADHD. Parents of 6099 children (83%) responded.
Results. By parental report, 607 children (10%) had been given an ADHD diagnosis and 434 (7%) were receiving ADHD medication treatment. Seventy-one % of the diagnosed children were receiving medication. Treatment rates varied by sex, race/ethnicity, and grade.
Conclusions. If treatment patterns observed in this study are representative, the public health impact of ADHD may be underestimated. (Am J Public Health. 2002;92:231–234)
Population-based data on the prevalence of medication treatment for attention deficit–hyperactivity disorder (ADHD) are limited. Data on national prescribing trends are available and have been used to estimate the proportion of office visits in which a stimulant medication is prescribed.1–3 However, these data cannot be used to estimate the proportion of children with ADHD who are being treated with stimulant medication, because in any year, each treated child typically has multiple office visits and receives many prescriptions.4
Some studies have estimated the prevalence of ADHD medication treatment on the basis of school records. In 1987, Safer and Krager5 estimated that 6% of the elementary school children in Baltimore, Md, received medication treatment for ADHD. LeFever et al.6 estimated that between 8% and 10% of second- through fifth-grade students in 2 Virginia school districts were receiving stimulant medication at school in 1995. In the Virginia study, treatment rates were particularly high among White boys: 17% took stimulant medication at school.6 In 2000, a survey conducted among school nurses in Maryland reported that 3.7% of all public elementary school children took ADHD medication at school.7
School-based surveys have an important limitation: they exclude children who take their medication only at home. Many parents choose to give medication at home by administering slow-release forms of stimulant medications. The authors of the Maryland school nurse study acknowledged this problem; they estimated that they missed about 20% of the children who were being treated for ADHD in their study population.7
Few population-based parent surveys of ADHD medication treatment rates among schoolchildren have been done. The Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) study, a large epidemiologic survey of 4 US communities, reported that about 2% of the children in its sample were receiving ADHD medication treatment.8 However, the children in the MECA study were aged 9 to 17 years. It is difficult to compare these data with those from samples of younger children, because medication rates tend to decline sharply among teenagers.9
In this article, we use parent reports to estimate the prevalence of medication treatment for ADHD among public elementary school children in grades 1 through 5 in a North Carolina county and to examine how prevalence varies by grade, sex, and race/ethnicity.
METHODS
Study Population
We defined our sample as all children enrolled in grades 1 through 5 in Johnston County's 17 public elementary schools. We excluded Johnston County children of elementary school age who were attending private schools (n = 75), receiving home schooling (n = 140), or attending middle schools (n = 268) because of concern that their learning environments might be different from those in public elementary schools. We excluded children with severe developmental disabilities placed in self-contained classrooms (n = 146). We also excluded children attending regular classes with special education designations for autism, mental handicap (IQ < 70), or severe health disabilities (such as traumatic head injury or childhood cancer) (n = 114). Children with learning disabilities or behavior problems were included in the sample regardless of classroom placement. A total of 7333 children were eligible.
Assessment
We surveyed parents from 8 schools during 1997 to 1998 and from the remaining 9 schools during 1998 to 1999. Parents with more than 1 child in elementary school received a questionnaire for each child. We asked parents 2 questions: (1) “Has a doctor or psychologist ever told you that your child has attention-deficit disorder (ADD), attention deficit–hyperactivity disorder (ADHD), or hyperactivity?” and (2) “Is your child currently taking any medicine prescribed by a doctor to help with symptoms of ADHD (for example, inattention or hyperactivity) or to help the child's mood or behavior?” If parents reported that their child was taking medication, we also asked them to name the medicine. We categorized children as taking ADHD medication if their parents answered yes to both questions.
Analysis
To calculate confidence intervals (CIs) for prevalence and prevalence ratios and to adjust for covariates, we fitted generalized linear models with a logarithmic link function and a binomial error distribution.10,11 The calculations were done with the GENMOD procedure in SAS software (SAS Institute Inc, Cary, NC). Prevalence ratios were adjusted for sex, race/ethnicity, and grade.
RESULTS
Parents of 6099 children (83%) answered both questions about their child's history of diagnosis and current medication treatment. This report is based on these 6099 children.
According to their parents, 607 children (10% of the sample) had ever been given an ADHD diagnosis. Prevalence estimates for various subgroups and prevalence ratios adjusted for sex, race/ethnicity, and grade appear in Table 1 ▶. Prevalence of ADHD diagnosis was similar for both years of the study. About 15% of the boys and 5% of the girls had been given an ADHD diagnosis (adjusted prevalence ratio = 3.1, 95% CI = 2.6, 3.7, P < .001). African American children were only slightly less likely than White children to have been diagnosed with ADHD (adjusted prevalence ratio = 0.9, 95% CI = 0.7, 1.1, P = .19). Hispanic children were much less likely to have been diagnosed with ADHD (adjusted prevalence ratio = 0.4, 95% CI = 0.2, 0.6, P < .001). The proportion of children with a history of ADHD diagnosis increased with age, from 6.5% in grade 1 to a high of about 13% in grades 4 and 5.
TABLE 1.
—Prevalence of Parent-Reported Attention Deficit–Hyperactivity Disorder (ADHD) Diagnosis and Parent-Reported Current Use of ADHD Medication
| Children Previously Diagnosed With ADHD | Children Currently Taking ADHD Medication | |||||||||||
| Children in Sample | ||||||||||||
| Grouping | N | % of Total | N | Prevalence, % | 95% CI | Adjusted Prevalence Ratioa | 95% CI | N | Prevalence, % | 95% CI | Adjusted Prevalence Ratioa | 95% CI |
| Total sample | 6099 | 100.0 | 607 | 10.0 | (9.2, 10.7) | 434 | 7.1 | (6.5, 7.8) | ||||
| Study year | ||||||||||||
| 1 | 3012 | 49.4 | 307 | 10.1 | (9.2, 11.3) | 205 | 6.8 | (6.0, 7.8) | ||||
| 2 | 3087 | 50.6 | 300 | 9.7 | (8.7, 10.8) | 229 | 7.4 | (6.5, 8.4) | ||||
| Sex | ||||||||||||
| Girls | 2951 | 48.4 | 140 | 4.7 | (4.0, 5.6) | 1.0 | 92 | 3.1 | (2.5, 3.8) | 1.0 | ||
| Boys | 3148 | 51.6 | 467 | 14.8 | (13.6, 16.1) | 3.1 | (2.6, 3.7) | 342 | 10.9 | (9.8, 12.0) | 3.5 | (2.8, 4.3) |
| Race/ethnicity | ||||||||||||
| White | 4437 | 72.7 | 479 | 10.8 | (9.9, 11.7) | 1.0 | 364 | 8.2 | (7.4, 9.1) | 1.0 | ||
| Black | 1208 | 19.8 | 110 | 9.1 | (7.6, 10.9) | 0.9 | (0.7, 1.1) | 62 | 5.1 | (4.0, 6.5) | 0.7 | (0.5, 0.8) |
| Hispanic | 376 | 6.2 | 15 | 4.0 | (2.4, 6.6) | 0.4 | (0.2, 0.6) | 8 | 2.1 | (1.1, 4.2) | 0.3 | (0.1, 0.5) |
| Other | 78 | 1.3 | 3 | 3.9 | (1.3, 11.7) | 0.4 | (0.1, 1.2) | 0 | 0.0 | . . . | 0.0 | . . . |
| Grade | ||||||||||||
| 1 | 1425 | 23.4 | 93 | 6.5 | (5.6, 7.9) | 1.0 | 62 | 4.4 | (3.4, 5.5) | 1.0 | ||
| 2 | 1367 | 22.4 | 112 | 8.2 | (6.9, 9.8) | 1.2 | (1.0, 1.6) | 81 | 5.9 | (4.8, 7.3) | 1.3 | (1.0, 1.8) |
| 3 | 1222 | 20.0 | 131 | 10.7 | (9.1, 12.6) | 1.6 | (1.2, 2.0) | 97 | 7.9 | (6.6, 9.6) | 1.7 | (1.3, 2.4) |
| 4 | 1140 | 18.7 | 149 | 13.1 | (11.3, 15.2) | 2.0 | (1.6, 2.5) | 107 | 9.4 | (7.8, 11.2) | 2.1 | (1.6, 2.8) |
| 5 | 945 | 15.5 | 122 | 12.9 | (10.9, 15.2) | 1.9 | (1.5, 2.5) | 87 | 9.2 | (7.5, 11.2) | 2.0 | (1.5, 2.8) |
Note. CI = confidence interval.
aPrevalence ratios were adjusted for sex, grade, and race/ethnicity.
By parental report, 434 children (7.1%, 95% CI = 6.5, 7.8) were currently receiving medication to treat ADHD (Table 1 ▶). Medication treatment rates were similar during both years of the study. About 11% of the boys in the sample were taking ADHD medication, compared with about 3% of the girls. ADHD medication treatment also varied by race/ethnicity. About 8% of the White children were currently receiving medication treatment, compared with 5% of the African American children and 2% of the Hispanic children. In comparison with White children, the prevalence ratio of ADHD medication treatment was 0.7 (95% CI = 0.5, 0.8, P = .001) among African American children and 0.3 (95% CI = 0.1, 0.5, P < .001) among Hispanic children after adjustment for grade and sex. Medication treatment rates tended to increase with grade: more than 9% of the children in both the fourth and the fifth grades were taking medication to treat ADHD.
Of the children who had ever been given an ADHD diagnosis, 71% were currently receiving medication treatment. Even though 3 times as many boys as girls were taking ADHD medication, the proportions of diagnosed children of each sex receiving treatment barely differed: 73% of the boys and 66% of the girls (adjusted prevalence ratio = 1.1, 95% CI = 1.0, 1.3, P = .05). Racial/ethnic differences in the proportion treated were more pronounced: 76% of the ADHDdiagnosed White children were taking medication, compared with 56% of the African American and 53% of the Hispanic children. The adjusted prevalence ratios relative to Whites were 0.7 (95% CI = 0.6, 0.9, P < .001) and 0.7 (95% CI = 0.4, 1.1, P = .12), respectively.
Of the 434 children receiving treatment, 402 (93%) were taking a stimulant; 9.7% of those taking a stimulant were taking at least 1 other medication. Medication type was missing for 2 children. Of the 30 children taking other medications, 16 were taking a centrally acting adrenergic receptor agent (clonidine or guanfacine) and 14 were taking either an antidepressant or a mood stabilizer.
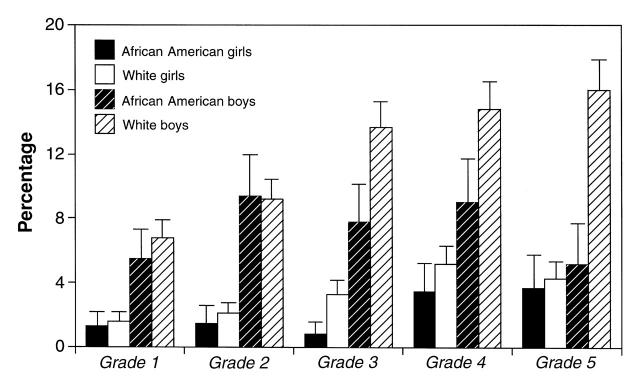
Treatment rates with stimulant medication were particularly high for White boys (Figure 1 ▶). More than 15% of the White boys in the fourth and fifth grades (123 of 800) were currently taking stimulant medication. In fourth-grade students, the proportion of African American boys taking stimulant medication (10 of 111, 9%) was about 60% that of White boys (63 of 426, 15%). The rate of stimulant treatment for African American boys was lower in the fifth grade. This sharp decrease was probably a methodologic artifact; the 2 schools with the highest rates of stimulant treatment for African American boys lacked a fifth grade. Children from these schools attended middle school in fifth grade and therefore were not included in the sample. Stimulant medication treatment rates were higher among White girls than among African American girls in each grade, but the racial/ethnic disparity was less pronounced among girls than among boys.
FIGURE 1.
—Prevalence of attention deficit–hyperactivity disorder stimulant medication treatment, by grade, race/ethnicity, and sex.
DISCUSSION
The prevalence of parent-reported ADHD medication treatment reported here (7%) is similar to that reported in 2 school-based studies.5,6 Heretofore, treatment rates were viewed as abnormally high if they exceeded the 3% to 5% prevalence estimate for ADHD cited in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).12 ADHD prevalence estimates vary widely, however, depending on the methodology used.13
Our study was conducted in only 1 county, so the generalizability of our results is not clear. It is difficult to gauge to what extent treatment patterns in Johnston County pertain to other parts of North Carolina or the United States. Johnston County has a racial/ethnic and educational profile similar to that of North Carolina as a whole. In addition, the authors of the Great Smoky Mountain study, a study of children's mental health in 11 western North Carolina counties, reported that 7.3% of the children in their sample were being treated with stimulant medication.14 However, that study oversampled children with psychiatric disorders and Native American children, so those data are not directly comparable with ours. Additional population-based studies of the prevalence of ADHD medication treatment are needed.
Our data are consistent with other observations that suggest that the prevalence of medication treatment for ADHD is higher among boys than among girls15,16 and higher among Whites than among African Americans.6,15–17 Our data showed only a small difference in history of diagnosis between Whites and African Americans but a substantial difference in medication treatment rates between the 2 groups. Hispanic children were the least likely to have been given an ADHD diagnosis or to be receiving medication treatment for ADHD. Our data on Hispanics should be interpreted cautiously because of small numbers. Nevertheless, the Maryland school nurse study also reported low treatment rates among Hispanic children.7
Demographic variation in the prevalence of medication treatment may be important. Differences in treatment rates between boys and girls may reflect sex differences in the prevalence of ADHD, but it also may reflect referral bias.18,19 Despite the sex difference in treatment rates, it was reassuring to see that once diagnosed with ADHD, boys and girls received medication in similar proportions. In contrast, significantly smaller proportions of African American and Hispanic children than of White children with ADHD were receiving medication treatment. We are not sure why. Compared with White children, Hispanic and African American children face many barriers to care, including less access to medical providers, less health insurance coverage, and less ability to pay for medication.15 Cultural differences also may influence parents' or children's acceptance of using medication to treat ADHD. In addition, difficulties in speaking English may mask inattention symptoms among Hispanic children.
Both history of diagnosis of ADHD and current medication treatment were based on parent report and not confirmed with medical or pharmacy records. The nomenclature and diagnostic criteria for ADHD have been revised several times over the past 10 years,20 and many primary care physicians do not use DSM-IV when diagnosing attentional disorders.21 Thus, parent-reported history of a diagnosis of ADHD is likely to be a poor surrogate for the true DSM-IV prevalence of ADHD in a study population. The data presented here can estimate the prevalence of medication treatment but do not address whether ADHD is under- or overdiagnosed or under- or overtreated in our population.
Obtaining information on children's medication use from parents instead of from school records avoids missing children who take medication only at home. However, response bias is a potentially important problem for parent-based surveys. Our study had a relatively high response rate (83%), but we had little information from which to assess selection bias. Several scenarios are plausible. Some parents of children with ADHD may have chosen not to participate because of concerns about confidentiality, whereas others may have been motivated to participate out of a desire to increase public understanding of the disorder.
We may have misclassified some children as taking ADHD medication if they were taking a medication prescribed for a comorbid condition such as anxiety or depression. We believe, however, that any resulting bias was probably small, because only 7% of the children we classified as taking ADHD medication were not taking a stimulant.
Few community-based studies of the prevalence of ADHD and the prevalence of ADHD medication treatment exist. Since 1997, the National Health Interview Survey has asked about history of diagnosis of “attention deficit disorder.” This phrasing is potentially problematic because of the changing terminology: parents of children with a diagnosis of the hyperactive subtype or combined subtype of ADHD may not have answered yes. Questions about history of diagnosis and current medication treatment similar to the questions that we used could be added to large national surveys such as the National Health Interview Survey, the National Health and Nutrition Examination Survey, or other community-based surveys. If the prevalence of ADHD diagnosis or ADHD medication treatment among elementary school children in the United States is similar to the estimates reported here, educators and public health officials may have substantially underestimated the public health impact of ADHD.
Acknowledgments
This study was conducted with funds provided by the National Institute of Environmental Health Sciences.
The authors would like to thank Gretchen LeFever, PhD, Lewis P. Rowland, MD, Frank Stallone, PhD, David Rabiner, PhD, Cindy Reuben, MA, Patricia Pastor, PhD, Julie Daniels, PhD, and Matthew Longnecker, MD, ScD, for their careful reading of the paper and thoughtful critical comments. We also would like to thank Vann Langston, James Causby, PhD, Keith Beamon, and Susan Deitz for their unflagging encouragement and help in making the study possible within the Johnston County schools.
Note. The study was approved by the National Institute of Environmental Health Sciences Institutional Review Board. All study participants provided informed consent.
A. S. Rowland, D. M. Umbach, and D. P. Sandler designed the study, and A. S. Rowland and L. Stallone conducted it. A. S. Rowland, D. M. Umbach, A. J. Naftel, and E. M. Bohlig analyzed the data. All of the authors wrote the report.
Peer Reviewed
References
- 1.Jensen PS, Bhatara VS, Vitiello B, Hoagwood K, Feil M, Burke LB. Psychoactive medication prescribing practices for US children: gaps between research and clinical practice. J Am Acad Child Adolesc Psychiatry. 1999;38:557–565. [DOI] [PubMed] [Google Scholar]
- 2.Pincus HA, Tanielian TL, Marcus SC, et al. Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialties. JAMA. 1998;279:526–531. [DOI] [PubMed] [Google Scholar]
- 3.Hoagwood K, Kelleher KJ, Feil M, Comer DM. Treatment services for children with ADHD: a national perspective. J Am Acad Child Adolesc Psychiatry. 2000;39:198–206. [DOI] [PubMed] [Google Scholar]
- 4.Zito JM, Safer DJ, Riddle MA, Johnson RE, Speedie SM, Fox M. Prevalence variations in psychotropic treatment of children. J Child Adolesc Psychopharmacol. 1998;8:99–105. [DOI] [PubMed] [Google Scholar]
- 5.Safer DJ, Krager JM. A survey of medication treatment for hyperactive/inattentive students. JAMA. 1988;260:2256–2258. [PubMed] [Google Scholar]
- 6.LeFever GB, Dawson KV, Morrow AL. The extent of drug therapy for attention deficit–hyperactivity disorder among children in public schools. Am J Public Health. 1999;89:1359–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Safer DJ, Malever M. Stimulant treatment in Maryland public schools. Pediatrics. 2000;106:533–539. [DOI] [PubMed] [Google Scholar]
- 8.Jensen PS, Kettle L, Roper MT, et al. Are stimulants overprescribed? Treatment of ADHD in four US communities. J Am Acad Child Adolesc Psychiatry. 1999;38:797–804. [DOI] [PubMed] [Google Scholar]
- 9.Rappley MD, Gardiner JC, Jetton JR, Houang RT. The use of methylphenidate in Michigan. Arch Pediatr Adolesc Med. 1995;149:675–679. [DOI] [PubMed] [Google Scholar]
- 10.McCullagh P, Nelder JA. Generalized Linear Models. New York, NY: Chapman and Hall; 1989.
- 11.Zocchetti C, Consonni D, Bertazzi PA. Estimation of prevalence rate ratios from cross-sectional data [letter]. Int J Epidemiol. 1995;24:1064–1065. [DOI] [PubMed] [Google Scholar]
- 12.Attention-deficit and disruptive behavior disorders. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994:78–85.
- 13.Cantwell DP. Attention deficit disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1996;35:978–987. [DOI] [PubMed] [Google Scholar]
- 14.Angold A, Erkanli A, Egger HL, Costello EJ. Stimulant treatment for children: a community perspective. J Am Acad Child Adolesc Psychiatry. 2000;39:975–984. [DOI] [PubMed] [Google Scholar]
- 15.Bussing R, Zima BT, Perwien AR, Belin TR, Widawski M. Children in special education programs: attention deficit hyperactivity disorder, use of services, and unmet needs. Am J Public Health. 1998;88:880–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Safer DJ, Zito JM. Psychotropic medication for ADHD. Ment Retard Dev Disabil Res Rev. 1999;5:237–242. [Google Scholar]
- 17.Zito JM, Safer DJ, dosReis S, Riddle MA. Racial disparity in psychotropic medications prescribed for youths with Medicaid insurance in Maryland. J Am Acad Child Adolesc Psychiatry. 1998;37:179–184. [DOI] [PubMed] [Google Scholar]
- 18.Arcia E, Conners CK. Gender differences in ADHD? J Dev Behav Pediatr. 1998;19:77–83. [DOI] [PubMed] [Google Scholar]
- 19.Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36:1036–1045. [DOI] [PubMed] [Google Scholar]
- 20.Barkley RA. Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. New York, NY: Guilford; 1998.
- 21.Wasserman RC, Kelleher KJ, Bocian A, et al. Identification of attentional and hyperactivity problems in primary care: a report from pediatric research in office settings and the ambulatory sentinel practice network. Pediatrics. 1999;103:E38. [DOI] [PubMed] [Google Scholar]