Abstract
Objectives. This study examined voluntary HIV testing rates in sexually transmitted disease (STD) clinics.
Methods. Anonymous, unlinked surveys of HIV seroprevalence and medical chart abstractions were conducted in 28 STD clinics in 14 US cities in 1997.
Results. Among the 52 260 patients included in the anonymous HIV serosurveys, voluntary HIV testing rates by clinic ranged from 30% to 99% (median = 58%). Patients not tested were more likely to be HIV infected than were patients who were tested, even after those with documented HIV infection were excluded, regardless of demographic characteristics, risk group, or STD diagnosis.
Conclusions. HIV infection is unrecognized in substantial numbers of patients with HIV infection visiting STD clinics. Efforts are needed to increase HIV testing and counseling of all patients visiting these clinics.
Patients attending sexually transmitted disease (STD) clinics are at increased risk for infection with HIV.1,2 For this reason, the US Public Health Service has recommended that counseling and HIV antibody testing services be available at all public STD clinics and that all patients attending these clinics be offered these services.3
Anonymous HIV serosurveys, conducted by the Centers for Disease Control and Prevention in collaboration with state and local health departments,4–6 provide an opportunity to evaluate the extent to which counseling and testing services are reaching these at-risk populations. With the availability of effective antiretroviral drug therapies, persons who are HIV infected can clearly benefit from knowledge of their serostatus and referral into care.7 Patients with HIV infection who acquire other STDs are at risk for transmitting HIV to their sexual partners; thus, providing them with counseling services8,9 also may have important public health benefits.
METHODS
The methods and study design for anonymous, unlinked HIV seroprevalence surveys in STD clinics have been described previously.6,10 Unlinked HIV testing is performed on blood samples collected for routine clinical purposes (usually for serologic syphilis testing) after personal identifiers have been permanently removed. In this study, serum samples from all patients who had blood drawn for syphilis serologic screening and who had not previously visited the clinic during the year's survey period were included in the serosurvey.
The survey period ranged from 3 months to 1 year during 1997 depending on clinic patient volume. Data routinely obtained and recorded during the STD clinic visit were abstracted from the medical records of patients eligible for inclusion in the survey. The only STD diagnoses considered in this analysis were new diagnoses of the following STDs and STD syndromes: syphilis, gonorrhea, chlamydia, genital ulcer disease, cervicitis, nongonococcal urethritis, pelvic inflammatory disease, and trichomoniasis. The survey protocol allowed for abstracting information related to HIV testing at the STD clinic visit and self-reported results of previous HIV tests from the medical chart. This information was routinely collected at 28 clinics from 14 cities (Atlanta, Ga; Baltimore, Md; Boston, Mass; Chicago, Ill; Denver, Colo; Houston, Tex; Los Angeles, Calif; Miami, Fla; New Orleans, La; New York, NY; Newark, NJ; San Francisco, Calif; Seattle, Wash; Washington, DC).
RESULTS
Of the 52 260 patients tested in unlinked HIV serosurveys (clinic range = 419–3839 patients), 30 809 (59%) came to the clinic with symptoms of an STD, 28% came for an examination but were asymptomatic, and 4% came solely for HIV testing. Most patients were male, between ages 15 and 34, African American, and heterosexual (Table 1 ▶). Overall, unlinked survey results showed that 4% were HIV infected.
TABLE 1.
—Percentage of Patients Tested for HIV, by Demographic and Risk Group Characteristics, at 28 Sexually Transmitted Disease Clinics in 14 US Cities, 1997
| Voluntarily Tested | Not Tested | |||||
| No. | % | % HIV+ | % | % HIV+ | % HIV+ (Excluding Patients Reported as +) | |
| Total | 52 260 | 61 | 2.0 | 39 | 7.4 | 4.8 |
| Male | 33 221 | 59 | 2.4 | 41 | 9.0 | 6.0 |
| Female | 19 039 | 66 | 1.2 | 34 | 3.8 | 2.3 |
| Age, y | ||||||
| <15 | 814 | 41 | 3.3 | 59 | 6.0 | 5.0 |
| 15–24 | 17 939 | 65 | 0.9 | 35 | 1.6 | 1.2 |
| 25–34 | 18 353 | 62 | 2.4 | 38 | 8.0 | 5.3 |
| 35–44 | 10 166 | 60 | 2.7 | 40 | 13.9 | 8.8 |
| >44 | 4988 | 56 | 2.7 | 44 | 10.1 | 6.5 |
| Race/ethnicitya | ||||||
| African American | 31 649 | 58 | 2.3 | 42 | 7.0 | 4.9 |
| Asian or Pacific Islander | 888 | 59 | 0.2 | 41 | 3.1 | 2.0 |
| Hispanic | 10 236 | 72 | 1.5 | 28 | 6.0 | 3.7 |
| White | 8153 | 62 | 1.4 | 38 | 10.6 | 5.8 |
| Other | 790 | 61 | 1.5 | 39 | 6.0 | 2.7 |
| Risk groupb | ||||||
| Men who have sex with men | 4228 | 49 | 9.1 | 51 | 30.6 | 19.7 |
| Injection drug users | 1260 | 61 | 5.1 | 39 | 22.2 | 7.3 |
| Heterosexual persons | 46 772 | 62 | 1.4 | 38 | 4.2 | 3.1 |
| HIV infectedc (total) | 2112 | 30 | . . . | 70 | . . . | . . . |
| HIV infectedc (excluding patients reported as +) | 1435 | 35 | . . . | 65 | . . . | . . . |
aRace/ethnicity was not determined in 544 patients (1%).
bInjection drug user subgroup does not include men who have sex with men. Heterosexual subgroup does not include men who have sex with men or injection drug users.
cBased on unlinked HIV serosurveys.
Among the 28 clinics, voluntary HIV testing rates at the current visit ranged from 30% to 99% (median = 58%). HIV seroprevalence by clinic ranged from 0.6% to 11.5% (median = 4.7%). Among patients who were voluntarily tested, HIV seroprevalence was lower (range = 0.3%–5.8%, median = 2.4%) than among patients who were not voluntarily tested (range = 1.7%–28.6%, median = 7.3%). In all but 1 clinic, where HIV seroprevalence in the 2 groups was similar, HIV seroprevalence was 1.4 to 18 times higher among patients not voluntarily tested than among those voluntarily tested.
Patients not tested were more likely to be HIV infected than were patients who were tested, regardless of demographic characteristics, risk group, or STD diagnosis. Even after patients known to be HIV infected were excluded, seroprevalence was markedly higher among patients who were not tested (Tables 1 and 2 ▶ ▶).
TABLE 2.
—Percentage of Patients Tested for HIV, by Sexually Transmitted Disease Diagnosis During the Visit, at 28 Sexually Transmitted Disease (STD) Clinics in 14 US Cities, 1997
| Voluntarily Tested | Not Tested | |||||
| Diagnosis | No. | % | % HIV+ | % | % HIV+ | % HIV+ (Excluding Patients Reported as +) |
| Primary or secondary syphilis | 206 | 56 | 4.4 | 44 | 16.5 | 11.6 |
| Genital ulcera | 405 | 61 | 2.4 | 39 | 16.5 | 12.1 |
| Gonorrhea | 5646 | 55 | 3.0 | 45 | 12.3 | 8.4 |
| Any STDb | 18 613 | 58 | 2.0 | 42 | 7.8 | 5.5 |
| No STD | 33 647 | 62 | 1.9 | 38 | 6.8 | 4.3 |
aIncludes primary syphilis.
bIncludes syphilis at any stage, gonorrhea, chlamydia, genital ulcer, cervicitis, nongonococcal urethritis, pelvic inflammatory disease, trichomoniasis.
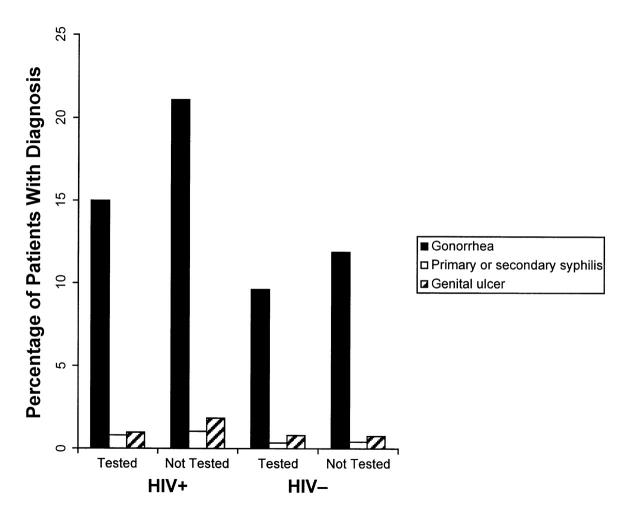
Patients who were HIV infected were equally or more likely to receive new diagnoses of gonorrhea, primary or secondary syphilis, or genital ulcer disease than were patients who were HIV negative, regardless of testing status (Figure 1 ▶). Overall, 43% of the patients who were HIV infected received an STD diagnosis, compared with 35% of the patients who were HIV negative. Among patients who were HIV infected, a diagnosis of an STD at the clinic visit was more common for patients not tested (46%) than for patients who were tested (34%). When this analysis was limited to patients attending the clinic with reported symptoms of an STD (59% of the population studied), a similar pattern was observed, although STD rates were higher for all groups.
FIGURE 1.
—Percentage of patients with a diagnosis of gonorrhea, syphilis, or genital ulcer disease, grouped by testing and HIV status.
Of the 52 260 patients included in the serosurveys, 27 738 (53%) reported having a previous HIV test and 14 750 (28%) reported not having a previous test. For 9772 (19%), no information about prior testing was available. Among those reporting a previous positive test result (n = 740), 91% had positive test results in the serosurveys; among those reporting a previous negative test result (n = 24 240), 1.9% now had positive test results; and among those reporting a previous indeterminate result (n = 52), 21% had positive test results. Of the 2706 patients for whom previous reported test results were unavailable, 3.4% had positive test results. Among those reporting a previous HIVnegative result, 63% were tested at the STD clinic visit, whereas 21% of those reporting a previous HIV-positive result were tested.
DISCUSSION
We found that many patients visiting STD clinics are not being tested for HIV. Although the proportion of patients receiving voluntary HIV testing services varied by clinic, the overall testing rates observed (61%; median clinic rate = 58%) were no higher than those reported much earlier in the epidemic at individual clinics11–13 before the availability of combination antiretroviral therapy.
All STD clinics participating in these serosurveys routinely offer voluntary HIV counseling and testing services. However, many HIV counseling and testing services are available near STD clinics but are not necessarily integrated with other STD services.14 A patient visiting an STD clinic who wants to undergo HIV testing may need to wait longer, pay more, and receive an additional needlestick. Patients should always be able to decline specific diagnostic tests; however, if HIV and STD services were better integrated, more patients who were offered HIV testing would likely accept it, and more patients who are HIV positive could be identified, counseled, and referred for treatment.
Clearly, some persons attending STD clinics already know from prior testing that they are HIV positive. Of the 2112 persons found to be HIV positive in these unlinked serosurveys, 32% reported a previous HIV-positive test result, and another 24% were voluntarily tested at the STD clinic visit. Others may have denied knowledge of their serostatus, or it may not have been recorded in the medical chart. However, for more than 40% of the HIV-infected population, no evidence indicated that patients knew or were about to learn their HIV status.
Compared with patients without HIV infection, a higher proportion of persons with HIV infection visiting these clinics, regardless of testing status, were given new STD diagnoses, indicating that they are continuing to engage in risk behaviors that may transmit HIV to their sexual partners. These data suggest that although all STD clinic patients should be counseled about reducing their risks for transmitting or acquiring HIV and other STDs, prevention efforts should be directed specifically toward those individuals who are HIV infected. Because these persons represent a relatively small proportion of the overall clinic population (<4%), it could be time- and cost-efficient to concentrate extra counseling and follow-up efforts on this group.8
To the extent that counseling is linked to testing or knowledge of serostatus, many patients infected with HIV are currently not being counseled. By separating counseling from HIV testing, patients with HIV infection who do not need retesting because their HIV infection status is already documented can benefit from patient-centered risk reduction counseling, which has been shown to prevent new STDs.9 When patients with HIV infection and their clinicians do not know their status, HIV testing is a necessary first step for providing such counseling and referral for treatment, which has been shown to reduce morbidity and mortality.15,16
Our findings show that HIV testing programs currently in place in STD clinics are not reaching substantial numbers of patients, including many who are unaware that they are infected with HIV. Many patients with HIV infection visiting these clinics have new STDs and may be transmitting HIV to sexual partners. Prevention efforts directed toward these persons who are HIV infected could have a significant effect on both the individuals' and the public's health. First steps should be removing barriers to HIV testing in STD clinics and providing patient-centered risk reduction counseling.
Acknowledgments
The results of this analysis were presented in part at the 1998 National STD Prevention Conference, December 6–9, 1998, Dallas, Tex.
The study was approved by the Institutional Review Board of the Centers for Disease Control and Prevention.
We are indebted to the staffs at the local and state health departments who conducted these surveys. We also thank Drs Thomas Peterman and Mary Kamb for their review of the manuscript and helpful suggestions.
H. Weinstock, L. Linley, and M. Gwinn planned the study. H. Weinstock analyzed the data and wrote the paper. M. Dale supervised the conduct of the study and assisted with data analysis. M. Gwinn contributed to the writing of the paper. All authors assisted with drafting the paper and approved the final version.
Peer Reviewed
References
- 1.Weinstock HS, Sidhu J, Gwinn M, et al. Trends in HIV seroprevalence among persons attending sexually transmitted disease clinics in the United States, 1988–1992. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;9:514–522. [PubMed] [Google Scholar]
- 2.Weinstock HS, Sweeney S, Satten GA, et al. HIV seroincidence and risk factors among patients repeatedly tested for HIV attending sexually transmitted disease clinics in the United States, 1991–1996. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;19:506–512. [DOI] [PubMed] [Google Scholar]
- 3.HIV Counseling, Testing, and Referral: Standards and Guidelines. Atlanta, Ga: Centers for Disease Control and Prevention; 1994.
- 4.Dondero TJ, Gill ON. Large-scale HIV serologic surveys: what has been learned? AIDS. 1991;5(suppl 2):S63–S69. [DOI] [PubMed] [Google Scholar]
- 5.Pappaioanou M, Dondero TJ, Petersen LR, et al. The family of HIV seroprevalence surveys: objectives, methods, and uses of sentinel surveillance for HIV in the United States. Public Health Rep. 1990;105:113–119. [PMC free article] [PubMed] [Google Scholar]
- 6.Onorato IM, McCray E, Pappaioanou M, et al. HIV seroprevalence surveys in sexually transmitted disease clinics. Public Health Rep. 1990;105:119–124. [PMC free article] [PubMed] [Google Scholar]
- 7.Carpenter CC, Fischl MA, Hammer SM, et al. Antiretroviral therapy for HIV infection in 1998: updated recommendations of the International AIDS Society–USA Panel. JAMA. 1998;280:78–86. [DOI] [PubMed] [Google Scholar]
- 8.HIV Prevention Case Management. Atlanta, Ga: Centers for Disease Control and Prevention; 1997.
- 9.Kamb ML, Fishbein M, Douglas JMJ, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. Project RESPECT Study Group. JAMA. 1998;280:1161–1167. [DOI] [PubMed] [Google Scholar]
- 10.National HIV Prevalence Surveys, 1997 Summary. Atlanta, Ga: Centers for Disease Control and Prevention; 1998.
- 11.Hull HF, Bettinger CJ, Gallaher MM, et al. Comparison of HIV-antibody prevalence in patients consenting to and declining HIV-antibody testing in an STD clinic. JAMA. 1988;260:935–938. [PubMed] [Google Scholar]
- 12.Schwarcz SK, Bolan GA, Kellogg TA, et al. Comparison of voluntary and blinded human immunodeficiency virus type 1 (HIV-1) seroprevalence surveys in a high prevalence sexually transmitted disease clinic population. Am J Epidemiol. 1993;137:600–608. [DOI] [PubMed] [Google Scholar]
- 13.Ford W, Kerndt PR, Rose TP, Nahlen BL. Comparison of acceptors and refusers of confidential HIV testing among patients in sexually transmitted disease clinics in Los Angeles County. In: Program and abstracts of the VI International Conference on AIDS; June 20–24, 1990; San Francisco, Calif. Abstract S.C.673.
- 14.Landry DJ, Forrest JD. Public health departments providing sexually transmitted disease services. Fam Plann Perspect. 1996;28:261–266. [PubMed] [Google Scholar]
- 15.Hogg RS, Heath KV, Yip B, et al. Improved survival among HIV-infected individuals following initiation of antiretroviral therapy. JAMA. 1998;279:450–454. [DOI] [PubMed] [Google Scholar]
- 16.Palella FJJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–860. [DOI] [PubMed] [Google Scholar]