Abstract
Since 1999, many African governments have launched programs to offer short-course antiretroviral drug regimens to reduce mother-to child transmission of HIV. HIV testing in prenatal care is the gateway to these antiretroviral regimens. Pilot projects in Africa show an uptake of antiretroviral drugs in 8% to 50% of pregnant women presumed to be HIV infected; often, a minority of eligible women in care received these regimens. Use of lay counselors and rapid onsite HIV testing may alleviate health service barriers.
Community education to promote voluntary counseling and testing, which involves men, is the long-term solution. In the short term, possibilities to enhance delivery of an effective intervention include group pretest counseling, universal offer of testing with women having the right to “opt out,” universal treatment (mass treatment for those whose HIV status is not determined by voluntary counseling and testing), universal testing with women having the right to “opt out” of learning their test results, and mass treatment for all without testing.
SEVERAL SHORT-COURSE antiretroviral regimens effectively prevent mother-to-child transmission of HIV, with reductions in the range of 30% to 50% depending on the regimen and breastfeeding practices.1–6 The potential public health impact of such regimens is large, especially in sub-Saharan Africa, where HIV prevalence is high. Even if the aim is only to reach the 40% of women who give birth in health facilities, we have the means today to avert over 100 000 infant infections in Africa.
To achieve this public health goal, African governments, United Nations (UN) agencies, and others acted to translate research findings into lives saved. By mid-2001, programs sponsored by the UN and the Elizabeth Glaser Pediatric AIDS Foundation alone had reached more than 180 000 pregnant women in sub-Saharan Africa,7 a tally that does not take into account the many efforts by nongovernmental organizations and research groups to prevent mother-to-child transmission.
Still, the challenge ahead is enormous. In June 2001, the UN General Assembly, in deliberating its response to AIDS, set new targets. In the Declaration of Commitment on HIV/AIDS (paragraph 54), the member states agreed that by 2005 they would "reduce the proportion of infants infected with HIV by 20 percent."8
The Declaration of Commitment called for exposing 80% of women who use antenatal care to a package of mother-to-child transmission prevention interventions. Achieving this goal means reaching perhaps 10 million women in sub-Saharan Africa, a truly massive task.
BOTTLENECKS IN IMPLEMENTATION
In the last 2 years, we have learned more about what is involved in taking programs on the prevention of mother-to-child transmission to scale. By 1999, it was already clear that providing voluntary counseling and testing (VCT) would be a major bottleneck in delivering these interventions on a wide scale in countries where HIV is prevalent.9 Part of the bottleneck is simply the cost of delivering VCT on the scale required. VCT comprises a large share of the program costs. In a model presented by Elliot Marseille and colleagues, a strategy offering counseling, testing, and—for those found to be HIV positive—antiretroviral drugs was twice as expensive as mass treatment, where all pregnant women would receive antiretroviral drugs without learning their HIV status.10 VCT is also less effective than mass treatment at reaching HIV-infected women. There are inevitable dropouts at each step of the VCT process: not all wo-men agree to be tested, not all those who are tested return for results, and not all those who learn of an HIV-positive status will take antiretroviral drugs or give birth in health facilities.
The benefits of VCT are well established. There is good evidence that when people learn their HIV status—whether they are HIV positive or HIV negative—they are more likely to practice safe sex.11 Knowledge of HIV-positive status also can help assure access to appropriate care, the options for which are expanding in the developing world. And in settings where it is more common to learn one's HIV status, the fear, stigma, and shame that surround AIDS is reduced. Uganda, for example, has been exemplary in its openness about AIDS and has pioneered voluntary HIV testing centers.12
The advantages of known HIV status are especially apparent in pregnancy, where low-cost antiretroviral interventions increasingly are available. Some changes in obstetric practice, such as reducing invasive procedures during childbirth, do not require knowledge of HIV status; however, it is certainly preferred that only women whose infants might benefit—that is, HIV-positive women—be advised to take antiretroviral drugs. Most especially, a decision not to breastfeed and to use replacement feeds must be based on a mother's knowledge of her positive-HIV status.13
EXPERIENCE IN PROGRAM DELIVERY
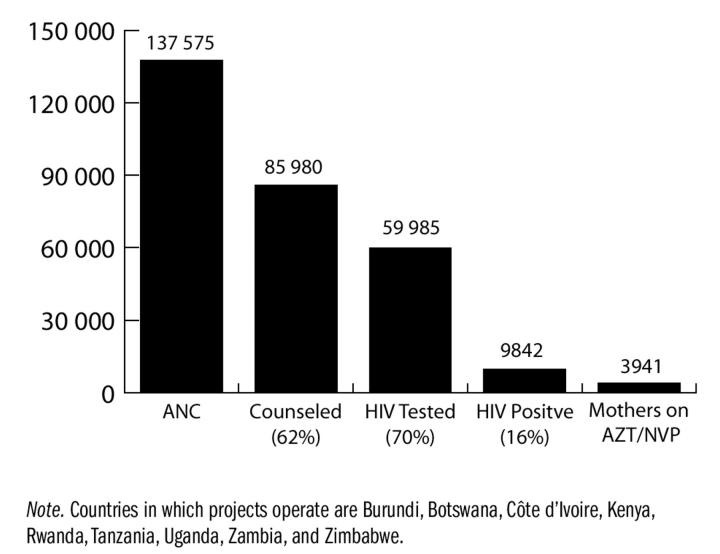
Figure 1 ▶ shows the aggregate experience of the pilot projects supported by the UN-sponsored program to prevent mother-to-child transmission in 9 sub-Saharan African countries. Since 1999, nearly 140 000 women who registered for antenatal care have been offered HIV counseling, testing, and antiretroviral drugs. At each step, there has been a drop in participation. In aggregate, 62% of women took part in counseling; of whom 70% were tested, meaning that fewer than half (43%) of the women in antenatal care had an HIV test.
Figure 1—
Experience of UN-sponsored pilot projects to prevent mother-to-child transmission in sub-Saharan Africa, July 2001.7
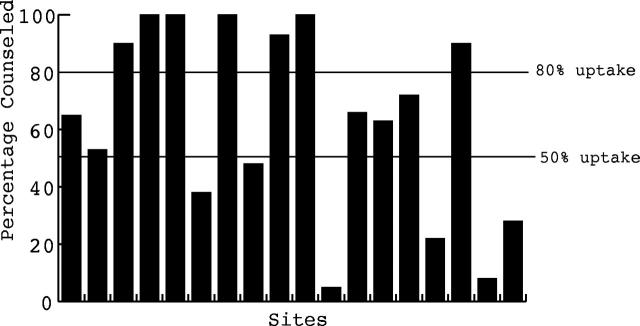
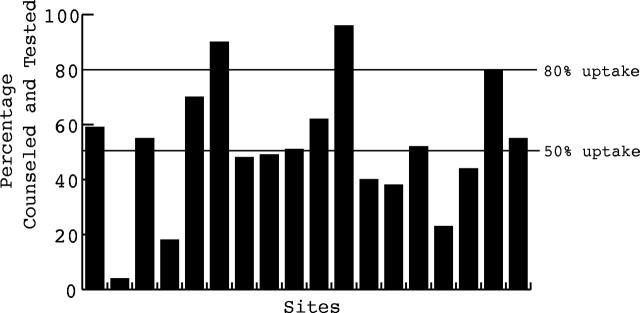
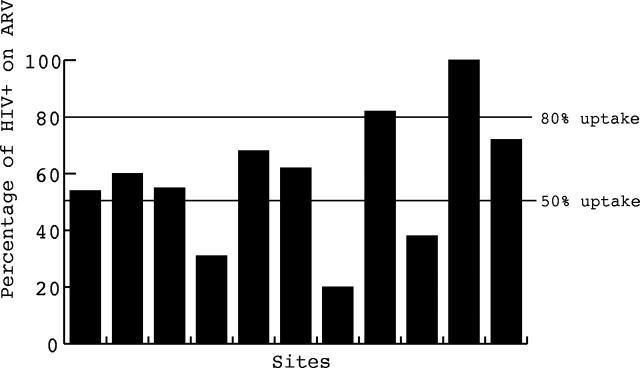
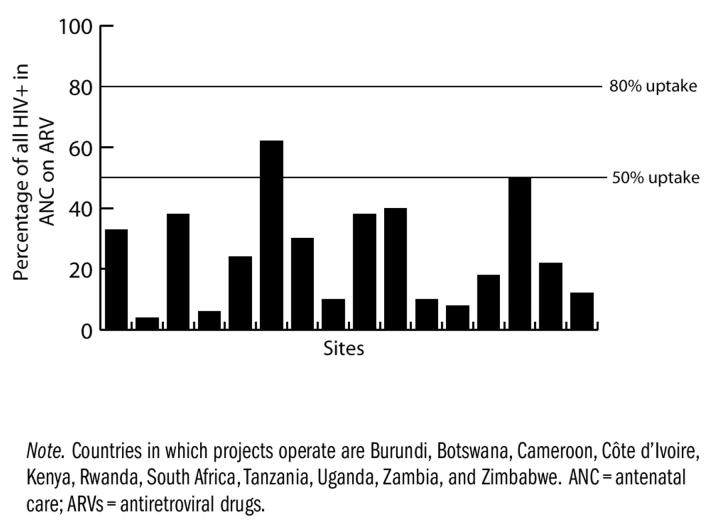
These aggregate data do not capture a rather large variation in uptake at different sites, as shown in Figure 2 ▶, based mainly on data from the UN-sponsored programs and the Elizabeth Glaser Pediatric AIDS Foundation Call to Action program. Some of the bars in the figure represent single sites, others country programs; they vary considerably in the number of women served. Rwanda, Cameroon, and a few other sites successfully counseled 100% of all women who came for antenatal care and achieved at least 80% counseling and testing rates. Rates were lower for other sites, sometimes below 50%. The proportion of women tested also varied: over 80% at a few sites and under 50% at many. Of the women identified as HIV positive through counseling and testing, the proportion who had received antiretroviral drugs at the time of the tally varied (some were not yet due to receive drugs and may well have received them at a later appropriate date).
Figure 2—
Variability in uptake of counseling, testing, and antiretroviral drug therapy in UN-sponsored pilot projects in sub-Saharan Africa, May 2001.14
ROOM FOR MORE PROGRESS
If it is assumed that HIV prevalence is the same for tested and untested women (an assumption that may be wrong), we get a sense of what proportion of the targeted population received antiretroviral drugs. If all HIV-positive women received antiretroviral drugs, this proportion would be 100%; in fact, it is quite low. In many cases, we must conclude that most HIV-positive pregnant women in care where short-course antiretroviral drugs for the prevention of mother-to-child transmission were offered did not benefit from the interventions, mainly because they were never identified.
The proportions shown in the bar graphs of Figure 2 ▶ show at least 2 things. First, whenever we see this much variability, we know that the outcome can be modified. There is something about the environment that can be changed, whether it is the health care delivery system, the health worker, the counselor, the woman, her partner, or the community.
These numbers also show that in general too few women benefit from programs for preventing mother-to-child transmission. We must be prepared to think creatively about how to deliver care differently to save more lives, while striving to help women to fully benefit from HIV testing.
BARRIERS TO VOLUNTARY COUNSELING AND TESTING
Where are the barriers to VCT? They occur at each step and have different origins. There are 2 important health system factors: lack of counselors and delays in offering test results.
Health Services
When counseling is undertaken, there must be staff to perform it. Nurses often are trained in counseling, but they have many competing demands on their time. Use of lay counselors, either paid or volunteer, can augment counseling capacity. This has been tried successfully in several settings.15–17 Training for a few weeks, followed by ongoing supervision, has resulted in reliable counseling services accepted by clinic staff and clients.
A tiered approach, which relies on lay or peer counselorsbacked up by professional counselors for the bulk of needs, can reduce the demand for full-time professional counselors. The World Health Organization is exploring this approach.
The use of group pretest counseling, rather than one-on-one counseling, is another strategy that has been both successful and acceptable.17 The provided counseling is mainly informational and fits in with the widespread practice of morning health education talks. In some settings, where technology is available, videos are a useful adjunct.
Advances in technology have greatly reduced turnaround times for test results. Rapid HIV testing results in higher uptake of results, because the gap between testing and getting the result is a matter of hours. Many programs are shifting from conventional enzyme-linked immunosorbent assays (ELISAs) to these rapid tests.12
Social Barriers
Adequate staff and test kits are often a direct problem of resources, but acceptability barriers are more complex in origin. These barriers arise among health workers, women, their partners, and communities at large. Primary care health workers often work under difficult circumstances with low pay and poorly supplied and equipped clinics. They may have low morale, and the clinical onslaught of AIDS is grim. They have no treatment options to offer. Talking about the risk of AIDS raises the specter of personal risk. Few health workers have had VCT themselves, and they may be skeptical about the wisdom of HIV testing for their clients, especially where high HIV prevalence makes the odds high that a positive test result will result.18,19
What follows are typical words of counselors and their clients:
From a counselor: “Once HIV is diagnosed, death comes more quickly.”
During a discussion with a client, a counselor speaks in a normal voice about the advantages and disadvantages of HIV testing. Then, in whispered voice, the counselor asks, “So, do you want to have a test?”
Client: “I would like to have an HIV test.” Counselor: “Are you sure?”
We need to address the reluctance of health workers to promote VCT.
Next, there are barriers for women themselves.20,21 Dominating their decisions are issues related to stigma. Women may correctly assess that the cost of an HIV-positive test is high. An infant does not only need to be born HIV negative; it needs food and shelter, something that the mother may depend on her spouse to provide. To have learned of her status without consulting her partner is risky. To talk with him is difficult. To tell her partner that she is HIV positive is risky. In many countries, fewer than half of women disclose their status. Further, to know she is HIV positive and not tell is risky. She will be frightened about her own fate. Against these risks, she balances a new intervention with as yet no visible impact. In this tragic calculus, not having a test may seem the better path.
It is clear that the involvement and support of men is crucial. The exclusion of men from reproductive health and pregnancy care is long-standing, and bringing men in now will not be simple. In fact, men generally have little contact with the health care system. Even finding ways to reach them is difficult. Addressing this issue will take time. Meanwhile, at the least, men need to hear a message along the lines of: “A man is responsible for looking after his family. He supports his wife in getting comprehensive pregnancy care.”
Male involvement is part of broader community involve-ment.21 In many settings, stigma and shame continue to be the dominant response to AIDS. Community involvement is a long-term and important process. One fairly straightforward activity is establishing community advisory boards.
Lack of Treatment for Mothers
Recently, Allan Rosenfield asked, “Where is the M in MTCT [mother-to-child transmission]?”22 Not surprisingly, women have been asking this question themselves. In a recent monograph on women's views in Botswana and Zambia, one woman said, “in the process pregnant woman will be thinking: I am going to die anyway. My baby might live but what is the point as there will be no mother to raise my baby.”20
Lack of treatment is an important barrier to the promotion of testing for both women and health workers. If we are committed not only to preventing HIV infection in infants but to ensuring child survival, we will have to think seriously about this call for attention to mothers. “MTCT plus”—treatment of the mother in addition to prevention of disease in the infant—also may make testing more acceptable. It is inevitable that women will begin to ask for treatment, and it is no longer so far from reach.
WHEN WOMEN DO NOT CHOOSE TESTING
At present, it is clear that having a test is difficult, although uptake is improving and probably will continue to improve as programs mature. Nonetheless, many HIV-positive women receive antenatal care services at our health care facilities and are not identified. Could we do better with VCT? Are we doing it “right”? Certainly there is room for improvement in the quality of counseling and in efforts to reach men and communities at large.
However, the fact that in such a wide range of settings we often fail to offer HIV-infected women anything because they have not been identified makes me ask, “Are we doing the right thing?”
HIV diagnosis differs from any other diagnostic process. This process emerged at a time when therapeutic intervention was uncertain.23 It stressed ensuring the patient's autonomy and asked the counselor to take a neutral stance—to be accepting of unwillingness to be tested and unwillingness to learn the result. This situation has changed with the advent of effective, available interventions. Should health workers—particularly in the developing world, where HIV is prevalent—remain neutral?
ALTERNATIVE PATHWAYS?
Current strategies depend on a woman's knowing and accepting her HIV status. This is certainly desirable, but it clearly is not always possible. Should it be a requirement? What other approaches might we take?
Universal Offer of HIV Testing
First, we might make universal the offer of HIV testing using the “opt out” approach.24 This would help normalize HIV testing as part of a comprehensive pregnancy care package, which includes screens for a number of conditions. If a woman does not wish to be tested, she should be allowed to opt out; however, the burden of taking the initial step is assumed by the health worker, who recommends the test.
In Britain, this approach increased uptake greatly. In Zimbabwe, the universal offer of HIV testing led to a doubling of uptake rates, which are now 80% to 90% (I. Chitsike, oral communication, September 2001).
Universal Treatment
With the universal treatment strategy, women who learned their HIV status through counseling and testing would receive antiretroviral drugs and infant feeding counseling if they tested positive for HIV.25 In addition, women who did not know their HIV status for whatever reason (not screened in antenatal care, never received antenatal care) would be offered nevirapine on a mass treatment basis without being tested. Women who decline HIV testing and whose HIV status is unknown may have assessed their own risk of HIV infection as high. In Kenya, unlinked anonymous surveillance of women who had not entered HIV counseling testing showed that HIV seroprevalence in this group was twice that of tested women (C. Wilfert, oral communication, September 2001).
There might be variations on this approach. We might offer nevirapine to all women of unknown HIV status. Staff might say, “There is a drug that when taken by the mother in labor and given to the baby after birth will reduce risk if the mother is HIV positive. Do you want to take this drug?” It might work to do rapid testing during labor or shortly after birth, so that the offer of testing could be made again at that time. All women offered mass treatment should have a subsequent offer of HIV counseling and testing.
Work by Stringer and colleagues in Zambia suggests that “mass treatment” will not be acceptable to all women and so will not result in perfect uptake.25 In their study, nevirapine levels suggested that adherence was lower in the mass treatment group than among women who were counseled, tested, and given nevirapine only if HIV positive. It makes sense that motivation for adherence might be higher if HIVpositive status is known.
Some work also suggests that not all women who present in labor accept nevirapine. A study in Zambia found that about one half accepted nevirapine.26 However, the use of short-course nevirapine was less effective, probably because women who presented in labor took their nevirapine dose much closer to the time of delivery.
Universal Testing, With “Opt Out” From Learning Results
In this approach, women would be tested, but we would allow them to “opt out” of being informed of the result. The Zvitambo study in Zimbabwe showed that many women were willing to be tested, but only 20% elected to receive results.27 Some women might prefer to have the health worker do the tests and prescribe the treatment.
Mass Treatment
Simply treating everyone on a mass treatment basis, without testing, remains an option in settings where infrastructure needs to be developed. This option allows us to reach women now while we work to put the support in place for counseling. It probably remains the lowest-cost option.
CONCLUSIONS
It is best that a woman knows and accepts her HIV status, but achieving this aim is not the immediate goal of programs to reduce mother-to-child transmission of HIV. Antenatal care aims to help women deliver healthy babies with healthy mothers. For many years, clinicians in Africa have been able to offer very little to the HIV infected. It is not appropriate to hold hostage a woman's ability to protect her infant to her ability to learn and accept her HIV status. I am confident that, over time, willingness to enter VCT will increase, but we need to act now. Reducing the risk of mother-to-child transmission is the right thing to do. There may be no single right way to do it.
Acknowledgments
I thank UNICEF and the Elizabeth Glaser Pediatric AIDS Foundation for sharing site data. The interpretation of these data is my own.
Ideas in this paper were presented at the 3rd Conference on Global Strategies for the Prevention of HIV Transmission From Mothers to Infants, Kampala, Uganda, September 9—Experience of UN-sponsored pilot projects to prevent mother-to-child transmission in subSaharan Africa.
Peer Reviewed
References
- 1.Shaffer N, Chuachoowong R, Mock PA, et al. Short-course zidovudine for perinatal HIV-1 transmission in Bangkok, Thailand: a randomized controlled trial. Lancet. 1999;353:773–780. [DOI] [PubMed] [Google Scholar]
- 2.Dabis F, Msellati P, Meda N, et al. Six-month efficacy, tolerance and acceptability of a short regimen of oral zidovudine to reduce vertical transmission of HIV in breastfed children in Côte d'Ivoire and Burkina Faso: a double blind placebo-controlled multicentre trial. Lancet. 1999;353:786–792. [DOI] [PubMed] [Google Scholar]
- 3.Guay L, Musoke P, Fleming T, et al. Intrapartum and neonatal single-dose nevirapine compared to zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda. HIVNET 012 randomised trial. Lancet. 1999;354:795–802. [DOI] [PubMed] [Google Scholar]
- 4.Gray G, for the PETRA Trial Management Committee. The PETRA study: early and late efficacy of three short ZDV/3TC combination regimens to prevent mother-to-child transmission of HIV-1. Paper presented at: 13th International AIDS Conference; July 9–14, 2000; Durban, South Africa. Abstract LbOr5.
- 5.Moodley D, on behalf of the SAINT investigators. The SAINT trial: nevirapine (NVP) versus zidovudine (ZDV) + lamivudine (3TC) in prevention of peripartum HIV transmission. Paper presented at: 13th International AIDS Conference; July 9–14, 2000; Durban, South Africa. Abstract LbOr2.
- 6.Lallemant M, Jourdain G, Le Coeur S, et al. A trial of shortened zidovudine regimens to prevent mother-to-child transmission of the human immunodeficiency virus type 1. Perinatal HIV Transmission Trial (Thailand) investigators. N Engl J Med. 2000;343:982–991. [DOI] [PubMed] [Google Scholar]
- 7.PMTCT News. New York, NY: UNICEF; 2001. Newsletter no. 2.
- 8.United Nations General Assembly. Declaration of Commitment on HIV/AIDS. New York, NY: United Nations; June 2001.
- 9.Dabis F, Leroy V, Castelbon K, Spira R, Newell ML, Salamon R. Preventing mother-to-child transmission of HIV-1 in Africa in the year 2000. AIDS. 2000;14:1017–1026. [DOI] [PubMed] [Google Scholar]
- 10.Marseille E, Kahn J, Mmiro F, et al. Cost effectiveness of single-dose nevirapine regimen for mothers and babies to decrease vertical HIV-1 transmission in sub-Saharan Africa. Lancet. 1999;354:1–12. [DOI] [PubMed] [Google Scholar]
- 11.Coates TJ. Efficacy of voluntary HIV-1 counseling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: a randomized trial. Lancet. 2000;356:103–112. [PubMed] [Google Scholar]
- 12.Downing RG, Otten RA, Marum E, et al. Optimizing the delivery of HIV counseling and testing services: the Uganda experience using rapid HIV antibody test algorithms. J Acquir Immune Defic Syndr. 1998;18:384–388. [DOI] [PubMed] [Google Scholar]
- 13.Kuhn L, Stein Z. Infant survival, HIV infection, and feeding alternatives in less-developed countries. Am J Public Health. 1997;87:926–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.PMTCT News. New York, NY: UNICEF; 2001. Newsletter no. 1.
- 15.Mhazo M, Moyo S, von Lieven A, Maponga C, Bassett MT. HIV counselling and testing amongst antenatal women using lay community volunteers: experience from urban Zimbabwe. Paper presented at: 13th International AIDS Conference; July 9–14, 2000; Durban, South Africa. Abstract TuOrC309.
- 16.Nywose GH, Myeni Z, Ngidi A, Van Rooyen H, Rollins NC. Lay counsellors for voluntary counselling and testing: experiences from rural South Africa. Paper presented at: 3rd Conference on Global Strategies for the Prevention of HIV Transmission From Mothers to Infants; September 9–13, 2001; Kampala, Uganda. Abstract 224.
- 17.Cartoux M, Sombie I, Van de Perre P, Meda N, Tiendrebeogo S, Dabis F. Evaluation of 2 techniques of HIV pre-test counseling for pregnant women in West Africa. Int J STD AIDS. 1999; 10:199–201. [DOI] [PubMed] [Google Scholar]
- 18.Mungherera M, van der Straten A, Hall TL, Faigeles B, Fowler G, Mandel JS. HIV/AIDS related attitudes and practices of hospital-based health workers in Kampala, Uganda. AIDS. 1997; 11(suppl 1):S79–S85. [PubMed] [Google Scholar]
- 19.Palmer DL, Mason PR, Pasi C, Tobaiwa O. Value of mandatory testing for human immunodeficiency virus in a sub-Saharan hospital population. Clin Infect Dis. 2000;31:1258–1265. [DOI] [PubMed] [Google Scholar]
- 20.Nyblade L, Field-Nguer ML. Women communities and the prevention of mother-to-child transmission of HIV: issues and findings from community research in Botswana and Zambia. In: Community Involvement in Initiatives to Prevent Mother-to-Child Transmission of HIV: A Collaborative Project. New York, NY: Population Council, International Center for Research on Women, and Positive Action; 2001.
- 21.Leonard A, Mane P, Rutenberg N. Evidence for the importance of community involvement: implications for initiatives to prevent mother-to-child transmission of HIV. In: Community Involvement in Initiatives to Prevent Mother-to-Child Transmission of HIV: A Collaborative Project. New York, NY: Population Council, International Center for Research on Women, and Positive Action; 2001.
- 22.Rosenfield A, Figdor E. Where is the M in MTCT? The broader issues in mother-to-child transmission of HIV. Am J Public Health. 2001;91:703–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Valdiserri RO. HIV counseling and testing: its evolving role in HIV prevention. AIDS Educ Prev. 1997;9(suppl 3): 2–13. [PubMed] [Google Scholar]
- 24.De Cock KM, Johnson AM. From exceptionalism to normalization: a reappraisal of attitudes and practice around HIV testing. BMJ. 1998;316:290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stringer JSA, Sinkala, M, Goldenberg RL, et al. A prospective comparison of two strategies for perinatal nevirapine administration in Zambia. University of Alabama at Birmingham, University Teaching Hospital and Central Board of Health, Lusaka, Zambia. Paper presented at: 3rd Conference on Global Strategies for the Prevention of HIV Transmission From Mothers to Infants; September 9–13, 2001; Kampala, Uganda. Abstract 58.
- 26.Stringer JSA, Sinkala M, Goldenberg RL, et al. A pilot study of nevirapine administered upon presentation in labour with HIV testing. University of Alabama at Birmingham, University Teaching Hospital and Central Board of Health, Lusaka, Zambia. Paper presented at: 3rd Conference on Global Strategies for the Prevention of HIV Transmission From Mothers to Infants; September 9–13, 2001; Kampala, Uganda. Abstract 300.
- 27.Piwoz E, Tavengwa N, Lunney K, et al. Women's perceived risk of HIV infection and mother-to-child transmission (MTCT) in the first 12 months post delivery. Paper presented at: 3rd Conference on Global Strategies for the Prevention of HIV Transmission From Mothers to Infants; September 9–13, 2001; Kampala, Uganda. Abstract 215.